To the Editor: Since the end of February 2020, when the first cases of coronavirus disease 2019 (COVID-19) caused by severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) were identified in Italy, the metropolitan area of Milan has been greatly affected by the spread of the disease. Individual case reports1 and studies of case series2, 3, 4, 5 have recently highlighted the presence of chilblain-like acral manifestations in young COVID-19 patients.
Between March 26 and April 26, 2020, 30 patients with a median age of 11 years (range 2-17 years) and chilblain-like acral lesions who had not started treatment with any new drug in the 15 days preceding lesion onset were referred to the Pediatric Dermatology Unit of the Fondazione IRCCS Ca' Granda in Milan, with the collaboration of the Italian Pediatric Primary Healthcare Society (SICuPP) Lombardy Section (Table I ). Seventeen (56.7%) were male patients.
Table I.
Demographic and clinical data of patients with chilblain-like lesions observed at the Pediatric Dermatology Unit of the University of Milan between March 26 and April 26, 2020
| ID | Sex | Age at diagnosis | Residence | Nasopharyngeal swab for SARS-CoV-2 | Cohabitants with systemic symptoms/COVID-19 in the 4 weeks preceding lesion onset | Systemic symptoms | Time between systemic symptoms and onset of lesions (days) | Duration of lesions (days) | Location of lesions | Distribution of lesions | Itching (visual analogue scale) | Local pain (visual analogue scale) |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 | F | 10 | Milan (province) | No | None | None | Not applicable | 23 | Feet (toes) | Bilateral | 0 | 0 |
| 2 | F | 17 | Milan (city) | Negative | Grandfather died of COVID-19 pneumonia | Fever | 13 | 12 (ongoing) | Hand (fingers) | Unilateral | 2 | 0 |
| 3 | F | 4 | Milan (city) | No | None | Fever | –1 | 3 | Feet (toes, dorsum) | Bilateral | 0 | 0 |
| 4 | M | 12 | Milan (province) | No | None | None | Not applicable | 9 (ongoing) | Feet (toes, soles) | Bilateral | 5 | 0 |
| 5 | F | 11 | Milan (province) | No | Both parents (fever); not tested for SARS-CoV-2 | Fever, coryza, cough, abdominal pain | 1 | 16 (ongoing) | Feet (toes) | Bilateral | 2 | 0 |
| 6 | F | 17 | Milan (province) | No | Two friends affected by COVID-19 (fever, cough) | None | Not applicable | 18 (ongoing) | Feet (soles) | Bilateral | 5 | 0 |
| 7 | M | 6 | Milan (province) | No | None | None | Not applicable | 10 (ongoing) | Hands (palms), feet (soles) | Bilateral | 6 | 0 |
| 8 | M | 17 | Milan (province) | No | None | None | Not applicable | 25 (ongoing) | Feet (toes) | Bilateral | 0 | 3 |
| 9 | M | 16 | Milan (province) | No | None | None | Not applicable | 24 (ongoing) | Feet (toes) | Bilateral | 0 | 4 |
| 10∗ | F | 11 | Milan (province) | Negative | Mother (cough); tested negative for COVID-19 | Fever, headache | 1 | 32 (ongoing) | Feet (soles, dorsum) | Bilateral | 1 | 0 |
| 11 | F | 11 | Milan (province) | No | None | Cough, dyspnea | 30 | 18 (ongoing) | Feet (toes) | Bilateral | 0 | 0 |
| 12 | M | 17 | Milan (province) | No | None | None | Not applicable | 24 (ongoing) | Feet (dorsum) | Bilateral | 0 | 2 |
| 13 | M | 11 | Milan (city) | No | None | None | Not applicable | 39 (ongoing) | Foot (toes) | Unilateral | 0 | 0 |
| 14 | F | 13 | Milan (province) | No | Father (fever, cough); not tested for SARS-CoV-2 | None | Not applicable | 13 (ongoing) | Feet (toes) | Bilateral | 0 | 0 |
| 15 | M | 10 | Milan (province) | No | None | None | Not applicable | 21 (ongoing) | Foot (toe) | Unilateral | 0 | 0 |
| 16 | M | 14 | Milan (province) | No | None | Coryza, weakness | 2 | 17 (ongoing) | Foot (sole) | Unilateral | 0 | 0 |
| 17 | M | 11 | Milan (province) | No | None | None | Not applicable | 1 | Ankles | Bilateral | 0 | 0 |
| 18 | M | 2 | Milan (province) | No | Mother (cough and coryza); not tested for SARS-CoV-2 | Cough, coryza | 5 | 5 | Hands (palms) | Bilateral | 0 | 0 |
| 19 | M | 4 | Milan (province) | No | None | None | Not applicable | 7 | Feet (soles) | Bilateral | 0 | 0 |
| 20∗ | F | 11 | Milan (city) | Negative | Both parents (cough); father tested negative for SARS-CoV-2 | Fever, cough | 6 | 19 | Feet (toes, dorsum) | Bilateral | 2 | 0 |
| 21∗ | F | 6 | Milan (province) | Negative | Mother (fever); tested negative for SARS-CoV-2 | Fever | 10 | 7 | Feet (toes, soles) | Bilateral | 0 | 3 |
| 22∗ | M | 5 | Milan (city) | Negative | Grandfather with bilateral pneumonia (not tested for SARS-CoV-2); mother tested negative for SARS-CoV-2 | Cough, dyspnea | 35 | 24 | Feet (toes, soles), hand (palm) | Bilateral | 1 | 5 |
| 23 | F | 6 | Milan (city) | No | None | None | Not applicable | 14 (ongoing) | Feet (toes, soles) | Bilateral | 0 | 0 |
| 24 | M | 14 | Milan (city) | Negative | None | None | Not applicable | 19 (ongoing) | Feet (toes) | Bilateral | 5 | 0 |
| 25 | M | 4 | Milan (province) | No | Mother with COVID-19 (presenting with fever and cough) | Fever, pharyngodynia | 2 | 8 (ongoing) | Ankles | Bilateral | 3 | 0 |
| 26 | M | 14 | Milan (province) | No | Father (fever, cough, dyspnea); not tested for SARS-CoV-2 | None | Not applicable | 24 (ongoing) | Feet (toes) | Bilateral | 0 | 0 |
| 27 | M | 13 | Milan (province) | No | None | None | Not applicable | 6 (ongoing) | Feet (toes, soles) | Bilateral | 4 | 0 |
| 28 | M | 16 | Milan (province) | No | Sister (fever); not tested for SARS-CoV-2 | Fever | 21 | 9 (ongoing) | Feet (toes) | Bilateral | 5 | 0 |
| 29 | F | 10 | Milan (province) | No | None | Fever, cough, weakness, pharyngodynia | 30 | 20 (ongoing) | Feet (toes) | Bilateral | 5 | 0 |
| 30 | F | 14 | Milan (province) | No | Sister (fever, cough, pharyngodynia, weakness) | None | Not applicable | 3 | Feet (toes) | Bilateral | 5 | 0 |
COVID-19, Coronavirus disease 2019; F, female patient; ID, identification; M, male patient; SARS-CoV-2, severe acute respiratory syndrome coronavirus 2.
Described in a previous article (Colonna C et al. Chilblain-like lesions in children following suspected COVID-19 infection. Pediatr Dermatol. 2020;37(3):437-440).
Thirteen patients (43.3%) experienced systemic symptoms a median of 6 days (range −1 to 35 days) before skin lesion onset, the most frequent being fever (n = 9/13; 69.2%), followed by cough (n = 6/13; 46.2%), coryza (n = 3/13; 23.1%), pharyngodynia (n = 2/13; 15.4%), weakness (n = 2/13; 15.4%), dyspnea (n = 2/13; 15.4%), abdominal pain (n = 1/13; 7.7%), and headache (n = 1/13; 7.7%).
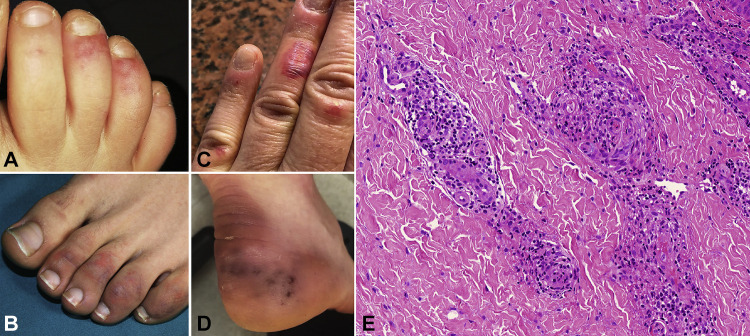
In all cases, the lesions were erythematous-violaceous patches or slightly infiltrated plaques, associated with edema in 3 cases (Fig 1, A-D ). No blisters, crusts, or ulcers were observed. Twenty-six patients (86.7%) had foot lesions, 2 involving only the ankle, and 4 had hand lesions, including 2 with foot involvement. Lesion distribution was unilateral in 4 cases (13.3%). Usually moderate itching (median visual analog scale score 4.5) was recorded in 14 patients (46.7%), and pain in 5 (16.7%; median visual analog scale score 3). The median duration of the lesions in the 9 patients whose lesions healed was 7 days (range 1-23 days). Two patients underwent a skin biopsy, and histology showed perivascular and periadnexal dermal lymphocytic infiltrates suggesting chilblains (Fig 1, E). Polymerase chain reaction–based testing result of nasopharyngeal swabs for SARS-CoV-2 was negative in all 6 patients tested.
Fig 1.
Chilblain-like acral lesions in 4 patients. A, Erythematous-violaceous noninfiltrated patches on the toes of a 10-year-old girl (patient 1). B, Violaceous noninfiltrated patches on the toes of a 16-year-old boy (patient 28). C, Violaceous slightly infiltrated plaques on the fingers of a 17-year-old girl (patient 2). D, Violaceous lesions on the heel of an 11-year-old girl (patient 11). E, Case 10. Histology revealed dense perivascular cuffs of lymphocytes and periadnexal lymphocytic infiltrates in the dermis. (Hematoxylin-eosin stain; original magnification: ×20.)
Like other centers,2 , 5 our Pediatric Dermatology Unit, which has a catchment area of approximately 3,000,000 people, has recently experienced an “outbreak” of 30 cases of chilblain-like lesions in comparison with only 3 cases of authentic chilblains in the corresponding period of 2019. The lesions are probably vasculopathic, and although their etiopathogenesis is still unclear, it seems to be related to SARS-CoV-2 infection. Median latency in our cohort was shorter than that reported in previous series2 , 4 and was slightly longer in the patients younger than 10 years (7.5 vs 6 days). This manifestation usually appears in asymptomatic or paucisymptomatic children, who do not often undergo SARS-CoV-2 testing in Italy for economic reasons. The recognition of chilblain-like lesions may facilitate a diagnosis of COVID-19 in asymptomatic or paucisymptomatic pediatric patients.
Acknowledgments
The authors would like to thank the following collaborators for their help in data collection and patient management: Elena Baggi, Cristina Bertanza, Giancarlo Brandolini, Luisa Callegaro, Valentina Cammareri, Marialuisa Cappuccilli, Elena Centimerio, Massimo Cordini, Elena Decet, Serena De Trane, Chiara Di Francesco, Maurizio Galea, Marco Giussani, Fabiana Lanfranchi, Roberto Marinello, Anna Maria Mazzei, Antonella Mezzopane, Daniela Moscatelli, Anna Maria Palmieri, Cristina Perfetti, and Patrizia Rogari.
Footnotes
Funding sources: None.
Conflicts of interest: None disclosed.
References
- 1.Kolivras A., Dehavay F., Delplace D. Coronavirus (COVID-19) infection-induced chilblains: a case report with histopathologic findings. JAAD Case Rep. 2020;6(6):489–492. doi: 10.1016/j.jdcr.2020.04.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Piccolo V., Neri I., Filippeschi C. Chilblain-like lesions during COVID-19 epidemic: a preliminary study on 63 patients. J Eur Acad Dermatol Venereol. 2020 doi: 10.1111/jdv.16526. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Fernandez-Nieto D., Jimenez-Cauhe J., Suarez-Valle A. Characterization of acute acro-ischemic lesions in non-hospitalized patients: a case series of 132 patients during the COVID-19 outbreak. J Am Acad Dermatol. 2020;83(1):e61–e63. doi: 10.1016/j.jaad.2020.04.093. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Andina D., Noguera-Morel L., Bascuas-Arribas M. Chilblains in children in the setting of COVID-19 pandemic. Pediatr Dermatol. 2020;37(3):406–411. doi: 10.1111/pde.14215. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.de Masson A., Bouaziz J.D., Sulimovic L., SNDV (French Union of Dermatologists-Venereologists) Chilblains are a common cutaneous finding during the COVID-19 pandemic: a retrospective nationwide study from France. J Am Acad Dermatol. 2020;83(2):667–670. doi: 10.1016/j.jaad.2020.04.161. [DOI] [PMC free article] [PubMed] [Google Scholar]