Abstract
Background
The global spread of the 2019 novel coronavirus (COVID-19) has profoundly affected the way we conduct our health care practices. The goal of this paper is to report the outcomes of 11 patients who underwent humeral fracture surgery in the first few weeks of the COVID-19 outbreak in Spain.
Methods
This was a retrospective case series of 11 patients who underwent humeral fracture surgery during the first weeks of the COVID-19 outbreak in Spain, between March 10 and April 25, 2020. The clinical outcomes of these operative patients were monitored up to May 12, 2020, the final date of follow-up, a minimum of 15 days after all patients were discharged from the hospital. COVID-19 infection, mortality, demographic, clinical, and laboratory data were analyzed.
Results
Thirty-six humeral fractures were recorded between March 10 and April 25, 2020. During this period, humeral fracture fixation was the third most common surgery for fracture in our institution after hip fracture and ankle fracture surgery. Eleven patients underwent surgery (30.5%), of whom 7 were women (63.3%). The mean age was 64.8 years (standard deviation, 13.5). Nine operated cases had a proximal humerus fracture and 2 had a humeral shaft fracture. One of the 11 patients was positive for SARS-CoV-2 on the basis of the quantitative reverse transcription polymerase chain reaction of throat swab samples. The overall median surgical time was 101.2 minutes (standard deviation, 28.4). The overall median hospital length stay for the patient discharged was 2.2 days (range, 1-4 days). No COVID-19 nosocomial intrahospital infection occurred, and no patient reported COVID-19 infection during the 15 days after hospital discharge. No intrahospital mortality was recorded. Furthermore, no COVID-19 infection was reported in the shoulder surgeons who performed the surgeries.
Conclusions
Although humeral fractures were not the most frequent fractures during this outbreak, some required surgery. With good preoperative management that included reverse transcription polymerase chain reaction for COVID-19 and chest radiographs, protective measurements for the surgical team, and rapid discharge of the patients, we were able to operate on 11 humeral fractures with no COVID-19 nosocomial intrahospital infection in the patients or in the shoulder surgeons who performed the surgeries.
Keywords: Shoulder, humerus, fracture, coronavirus, pandemic
The global spread of the 2019 novel coronavirus (COVID-19) has profoundly affected the way we conduct our health care practices.1 On March 11, 2020, the World Health Organization (WHO) declared COVID-19 a pandemic. As of late June 2020, more than 10,000,000 people across all countries, territories, and regions have been infected by this virus, and over 400,000 people have died.18
Hospitals’ work regimes have been re-prioritized. However, even though coronavirus infection must be a priority, this pandemic does not cause other health injuries, including shoulder fractures, to disappear.14 Although most surgeons are not fighting on the front line, we must continue treatment for surgical patients and, in the meantime, protect health care workers and patients from COVID-19 infection.15 Current guidelines, based on expert opinion, suggest that operation may be performed on select closed shoulder fractures, which if left untreated for more than 30 days may lead to loss of function, permanent disability, and/or irreducible dislocation of major joints.17 However, outcomes reported during the pandemic have been less than optimal. Lei et al7 retrospectively analyzed 34 operative patients who underwent elective surgeries during the incubation of COVID-19 in Wuhan; they reported that all patients developed COVID-19, 44% required intensive care unit (ICU) admission, and 7 died after admission to the ICU. Aminian et al2 reported 4 surgical patients (cholecystectomy, hernia repair, gastric bypass, and hysterectomy) who developed perioperative complications in the first few weeks of COVID-19 outbreak in Tehran, Iran, with a mortality of 75%. Mi et al9 reported 7 cases of osteoporotic hip fractures with an intrahospital mortality of 42.9% (3 of 7); the other 4 remained in the hospital, with no one discharged home. Although many questions remain unanswered about COVID-19 and surgical practice, surgical teams should appropriately respond to this worldwide public health crisis to improve patient outcomes and minimize the burden on the health care systems and global society.
Despite shoulder fractures not being the most common fracture during this outbreak, most shoulder fractures occurred in the home, so the implementation of stringent lockdown measures for the population may not affect their incidence. Zhu et al20 in a retrospective multicenter study of the epidemiologic characteristics of traumatic fractures in elderly patients during the outbreak of coronavirus disease 2019 in China found that shoulder fractures were the third most common fracture after hip fractures and spine fractures. The goal of this paper is to report the outcomes of 11 patients who underwent humeral fracture surgery in the first weeks of the COVID-19 outbreak in Spain. Furthermore, we discuss our personal protective equipment (PPE) and recommendations in these cases.
Material and methods
Our experience comes from our work at a hospital within the Spanish National Health System, which is one of the orthopedic and trauma referral centers in Spain. This was a retrospective review of all humeral fractures between March 10 and April 25, 2020. We also analyzed a retrospective case series of all patients who underwent humeral fracture surgery. We monitored the clinical outcomes of these operative patients up to May 12, 2020, the final date of follow-up, a minimum of 15 days after all patients were discharged from the hospital.
Surgery protection measures
A description of our PPE is given in Table I and is also shown in Fig. 1 . In our institution, 2 different surgical areas were created, each on a different floor: one a COVID-positive surgical area and the other a COVID-negative surgical area. Reverse transcription polymerase chain reaction (RT-PCR) tests for COVID-19 and chest radiographs were performed before the patients underwent surgery.
Table I.
Description of personal protective equipment (PPE)
|
Figure 1.
Photographs of our personal protective equipment.
In the operating room, general anesthesia with endotracheal intubation was performed, with only the anesthesiologist and 1 surgical nurse in the room at that time. Only 1 surgeon performed patient positioning in the beach chair. In draping the surgical field, we started by draping and covering the head, instead of starting at the axilla, for further protection of the health care providers. A maximum of 3 surgeons were allowed during surgery, although most of the surgeries were performed by only 2 surgeons.
Follow-up and outcome measures
Primary data included demographics, clinical characteristics, laboratory findings, evidence of COVID-19 infection or lack thereof, surgical treatment, and clinical outcome. Data collected included patient’s age, gender, injury mechanism, American Society of Anesthesiologists score, fracture type (shoulder fracture using the Association for the Study of Internal Fixation [AO] classification), and complications. We also recorded the surgical duration and time from hospital admission to discharge. We monitored the status of any COVID-19-positive patients, to know if it was reasonable to operate on patients with fractures during this pandemic. A COVID-19 nosocomial infection was defined as one that was acquired in the hospital. We reviewed the electronic medical record to note if any symptoms of fever, dyspnea, or COVID-19 infection (RT-PCR for COVID-19 and chest radiographs) occurred up until May 12, 2020, a minimum of 15 days after surgery. We also directly communicated with the patients and their families for any missing information.
Statistical analysis
The results are presented as descriptive statistics, describing the categorical variables by absolute values and percentages. Quantitative variables were presented by their measures of central tendency (mean and standard deviation [SD]). We used SPSS software (version 23.0; IBM, Armonk, NY, USA) for statistical analysis of the data.
Results
Thirty-six humeral fractures presented between March 10 and April 25, 2020, of which 26 (72.2%) were female. The mean patient age was 71.4 years (SD, 15.2). Of these patients, 11 underwent surgery (30.5%) (Table II ), of whom 7 (63.6%) were women. The age range on surgical patients was 43-86 years, with a mean age of 64.8 years (SD, 13.5). A fall from standing height caused 10 (90.9%) of the fractures. One younger patient was involved in a high-velocity (traffic) accident, which caused his humeral fracture and also a thoracic vertebral fracture that required surgery and débridement.
Table II.
Demographic, clinical, and laboratory data for patients who underwent surgery in our study
| Case 1 | Case 2 | Case 3 | Case 4 | Case 5 | Case 6 | Case 7 | Case 8 | Case 9 | Case 10 | Case 11 | |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Sex | Female | Female | Female | Female | Male | Male | Female | Female | Male | Female | Male |
| Age (yr) | 86 | 74 | 64 | 58 | 55 | 43 | 84 | 73 | 50 | 60 | 66 |
| ASA score | II | II | II | II | II | II | II | II | II | II | II |
| Comorbidity | HBP, DLP, A-fib | HBP | DLP | Fibromyalgia | Diabetes, DLP, BPH | Polytrauma with thoracic vertebral fracture, pelvis fracture, PFF | Diabetes, hypothyroidism, DLP | Asthma, DLP, PFF | HBP | HBP | HBP |
| Orthopedic diagnosis | Proximal humerus fracture | Humerus shaft fracture | Proximal humerus fracture | Proximal humerus fracture | Proximal humerus fracture | Proximal humerus fracture | Humerus shaft fracture | Proximal humerus fracture | Proximal humerus fracture | Proximal humerus fracture | Proximal humerus fracture |
| Orthopedic procedure | rTSA | ORIF with humeral nail and cerclages | ORIF with proximal humeral plate | ORIF with proximal humeral plate | ORIF with proximal humeral plate | ORIF with proximal humeral plate | ORIF with humeral nail and cerclages | ORIF with proximal humeral plate | ORIF with proximal humeral plate | ORIF with proximal humeral plate | ORIF with proximal humeral plate |
| Date of fracture | March 4 | March 13 | March 14 | March 15 | March 21 | February 28 | April 2 | April 21 | April 22 | April 25 | April 22 |
| Date of admission | March 13 | March 17 | March 18 | March 18 | March 25 | February 28 | April 22 | April 21 | April 29 | April 29 | April 29 |
| Orthopedic operation | March 13 | March 17 | March 18 | March 18 | March 25 | March 27 | April 22 | April 24 | April 29 | April 29 | April 29 |
| Date of discharge | March 16 | March 20 | March 19 | March 20 | March 27 | Remained in hospital | April 25 | April 26 | April 30 | May 1 | May 7 |
| Surgical duration (min) | 80 | 110 | 84 | 80 | 75 | 150 | 100 | 90 | 95 | 160 | 90 |
| Hospital length stay (d) | 3 | 3 | 1 | 2 | 2 | Remained in hospital | 3 | 5 | 1 | 3 | 1 |
| Laboratory test results | |||||||||||
| Hemoglobin (g/dL) | 12.9 | 11.9 | 13 | 14.6 | 14 | 12 | 13.2 | 15.2 | 13.1 | 13.7 | 14.1 |
| White blood cell count (×109/L) | 17.2 | 12.2 | 10.62 | 6.97 | 15.63 | 10.78 | 5.79 | 13.2 | 10.9 | 17.66 | 7.4 |
| Neutrophil count (×109/L) | 14.4 | 7.9 | 6.9 | 4.1 | 12.3 | 8.2 | 3.4 | 9.4 | 8 | 15.6 | 5.6 |
| Lymphocyte count (×109/L) | 1.8 | 2.9 | 2.2 | 2 | 1.3 | 1.6 | 1.8 | 2.8 | 1.8 | 0.8 | 1.2 |
| Monocyte count (×109/L) | 0.9 | 1.1 | 1.5 | 0.7 | 1.5 | 0.6 | 0.5 | 0.7 | 1 | 1.3 | 0.5 |
| Platelet count (×109/L) | 264 | 256 | 288 | 253 | 189 | 647 | 249 | 269 | 298 | 258 | 250 |
| aPTT (s) | 26 | 26.4 | 31.1 | 27.8 | 26.6 | 28.3 | 28.8 | 22.9 | 34.3 | 29.7 | 30.1 |
| PT (s) | 16.1 | 11.9 | 11.3 | 10.9 | 12.8 | 14.6 | 13.1 | 11.5 | 12.2 | 13.1 | 13.1 |
| Albumin (g/L) | 3.3 | 3.7 | 3.2 | 3.7 | 3.7 | 2.7 | 4.1 | NA | 3.8 | NA | 4.7 |
| ALT (U/L) | 10 | 17 | 22 | 24 | 62 | 95 | 10 | 15 | 11 | 13 | 35 |
| AST (U/L) | 22 | 18 | 31 | 24 | 73 | 27 | 15 | 24 | 18 | 19 | 26 |
| Total bilirubin (mg/dL) | NA | 0.75 | 0.77 | 0.67 | 0.78 | 0.42 | NA | 0.68 | NA | 0.48 | NA |
| Blood urea nitrogen (mg/dL) | 56 | 47 | 44 | 51 | 32 | 28 | 33 | 54 | 15 | 35 | 46 |
| Creatinine (mg/dL) | 1.44 | 0.88 | 0.54 | 0.59 | 1.08 | 0.37 | 0.7 | 0.72 | 0.49 | 0.64 | 0.84 |
| C-reactive protein (mg/dL) | 0.70 | 1.45 | 0.75 | 0.39 | 1.41 | 2.76 | 0.24 | 0.27 | 0.75 | 0.24 | 0.39 |
| IL-6 (pg/mL) | NA | NA | NA | NA | NA | 17.1 | NA | 72.7 | NA | 25.23 | NA |
| D-dimer (ng/mL) | NA | NA | NA | NA | NA | 710 | NA | 7780 | NA | 4743 | NA |
| SARS-CoV-2 quantitative RT-PCR | NA | NA | NA | NA | Negative | Positive | Negative | Negative | Negative | Negative | Negative |
| Chest X-ray | Lungs and pleural spaces were clear | Lungs and pleural spaces were clear | Lungs and pleural spaces were clear | Lungs and pleural spaces were clear | Lungs and pleural spaces were clear | Unilateral patchy consolidation | Lungs and pleural spaces were clear | Lungs and pleural spaces were clear | Lungs and pleural spaces were clear | Lungs and pleural spaces were clear | Lungs and pleural spaces were clear |
ASA, American Society of Anesthesiologists; aPTT, activated partial thromboplastin time; PT, prothrombin time; ALT, alanine aminotransferase; AST, aspartate aminotransferase; IL, interleukin; RT-PCR, reverse transcription polymerase chain reaction; HBP, high blood pressure; DLP, dyslipidemia; A-fib, atrial fibrillation; rTSA, reverser total shoulder arthroplasty; ORIF, open reduction and internal fixation; BHP, benign prostatic hyperplasia; PFF, proximal femoral fracture. All dates listed are 2020.
Nine operated cases had a proximal humerus fracture and 2 had a humeral shaft fracture. The patients included in this study underwent 3 different surgical procedures. Eight underwent open reduction and internal fixation of a proximal humeral fracture with a proximal humeral plate, 2 underwent open reduction and internal fixation of a humeral shaft fracture with a humeral nail, and 1 underwent a reverse total shoulder arthroplasty.
At the time of surgery, 1 of the 11 patients was positive for SARS-CoV-2 on the basis of quantitative RT-PCR of throat swab samples. The overall median time between fracture and surgery was 9 days (SD, 8.7). All patients had an American Society of Anesthesiologists score of II. The overall median surgical time was 101.2 minutes (SD, 28.4), and the overall median hospital stay until discharge was 2.2 days (range, 1-4 days). No COVID-19 nosocomial intrahospital infections occurred, and no patient reported COVID-19 infection during the 15 days after hospital discharge. No intrahospital mortality was recorded. The 10 COVID-19-free patients were discharged, 9 to home and 1 to a nursing home. The patient with COVID-19 remained in the hospital for complications related to his spine surgery, but as of April 19, 2020, he was asymptomatic with a negative RT-PCR for COVID-19. Furthermore, no COVID-19 infection occurred in the shoulder surgeons who performed the surgeries.
Discussion
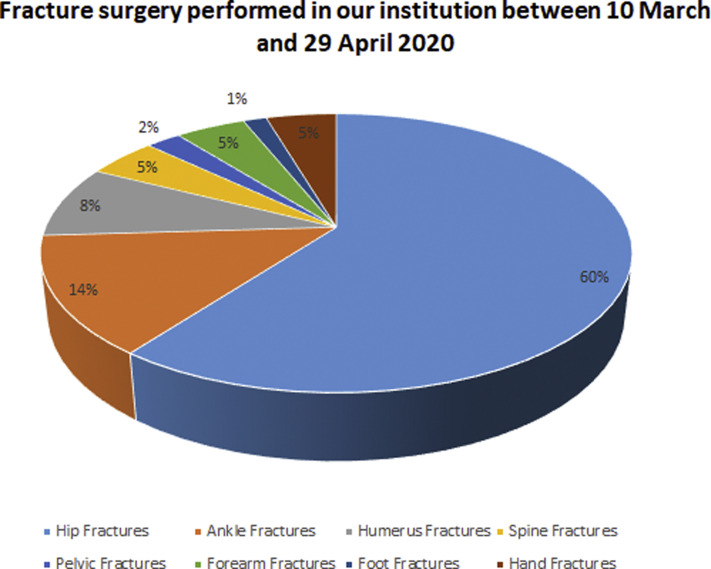
This report, to the best of our knowledge, is the first retrospective cohort study to describe the clinical characteristics and outcomes of shoulder surgery patients during the COVID-19 pandemic. Shoulder fractures are not the most frequent fracture during this outbreak, but their incidence is relatively constant despite the implementation of stringent lockdown measures for the population because, as with hip fractures, most shoulder fractures occur at home.12 Proximal humeral fractures account for 4%-5% of all fractures, with only hip and distal radial fractures being more common in the elderly.3 In our study, humeral fracture fixation was the third most common fracture surgery at our institution after hip and ankle fractures (Fig. 2 ). Using all the protective measurements described, we had no COVID-19 nosocomial intrahospital infection in the patients nor shoulder surgeons who performed the surgeries.
Figure 2.
Fracture surgery performed in our institution between March 10 and April 25, 2020. Humeral fracture fixation was the third most common surgery for fracture in our institution after hip fracture and ankle fractures during this period.
Unfortunately, this pandemic does not mean other medical emergencies disappear, including shoulder fractures requiring surgery. We recommend operation only when it is essential and realize that we put both ourselves and our team, which includes anesthesiologists and nurses, at risk. We must remember that intubation is considered one of the highest-risk procedures when dealing with patients with COVID-19.13 The majority of proximal humerus fractures and humerus shaft fractures can be treated nonoperatively. In a study evaluating the surgical management of proximal humerus fractures, it was found that the percentage of patients with proximal humerus fractures who underwent surgery ranged from 0% to 68%.3 A randomized clinical trial also found that in 2 years of follow-up, no significant differences were seen in patient-reported outcomes between surgical and nonsurgical management of displaced proximal humeral fractures of the surgical neck. However in that study, the patients who underwent nonoperative management underwent guided physiotherapy.16 In our study, only 30.5% of humerus fractures required surgery and were indicated only in complex and displaced fractures. Three cases were fracture dislocations of the proximal humerus, 6 cases were 3- and 4-part proximal humeral fractures, and the 2 humeral shaft fractures were severely displaced.
We note that in comparison with other studies, our patients had good outcomes with respect to COVID-19 infection or respiratory complications. Fifteen days after discharge, no patient was noted to have COVID-19 infection. We assessed the patients after 15 days because it has been estimated that 97.5% of COVID-19-infected cases will show symptoms within 11.5 days (95% CI, 8.2-15.6 days).6
One of the most important problems during the pandemic outbreak has been nosocomial COVID-19 infections. In our hospital, as of April 2, 2020, 707 patients with COVID-19 had been admitted, of whom 165 were considered critical, requiring ICU admission (Fig. 3 ).5
Figure 3.
Number of patients with COVID-19 admitted in our hospital per day and the day of surgery of the 11th patient. ICU, intensive care unit.
One point that differs from other studies is that we performed surgery on the day of the admission in 81.1% of our cases. Only 2 cases had a hospital admission before our surgery, one because of polytrauma in the COVID-19-positive patient and the other one because of a concomitant proximal femur fracture. The overall mean hospital length stay was 2.2 days (range, 1-4 days), although we excluded the polytrauma patient, because he was COVID-19 positive before surgery and stayed to the date of this paper due to his spinal surgery.
In the Spanish HIP-COVID Investigation Group study, the mean delay from presentation to the surgical procedure was 2.4 days. They did not report the overall median hospital length. In that study of 62 patients who were tested for COVID-19, 23 patients were positive.11 In a study of 305 patients admitted to gastrointestinal surgery services, Luong-Nguyen et al8 had 15 patients (4.9%) develop a nosocomial infection with SARS-Cov-2. In 12 patients (80%), the diagnosis was made after a hospital stay of more than 14 days (15-63 days).8 A report of 138 hospitalized patients from a single institution in Wuhan indicated that hospital-acquired transmission accounted for 41.3% of these admitted patients, thus implicating the hospital environment as a source of spread of the virus. Among those discharged alive, the median hospital stay was 10 days (interquartile range, 7.0-14.0).19
From an epidemiological perspective, nosocomial infection is a time-dependent event, although other factors can contribute to nosocomial infection.4 However, in our study with a mean hospital stay of 2.2 days, we had excellent outcomes with respect to a COVID-19 nosocomial infection. No COVID-19 infection was reported in the shoulder surgeons who performed the surgeries.
It is known that COVID-19 has forced thousands of health care workers out of action in Europe.10 As of April 25, 2020, more than 35,000 health care workers were infected in Spain.17 Every possible effort is important to create a feeling of health care provider protection. In our study, 3 patients had abnormal laboratory data with an increase in white blood cell count and D-dimer, despite having a negative RT-PCR for COVID-19 and normal chest radiographs.
We recommend that surgical draping start by covering the head, instead of starting at the axilla. With our protocol, no surgical wound infection developed in our patients at an early follow-up. Also, depending on the severity of the epidemic and available resources, the risk and benefits of performing shoulder surgical procedures should be carefully assessed. In locations with widespread infections and limited resources, the risk of shoulder surgical procedures for the patient and the community may outweigh the benefit. Hospital beds, surgical masks, and other PPE are in enormous demand around the world.
Our study has several notable limitations. The sample size of the present study was small with a short follow-up. However, this is understandable because all surgeries around the world have decreased because the COVID-19 pandemic. In addition, only 7 patients had RT-PCR for COVID-19 before surgery; however, none developed SARS-CoV-2 infection after surgery, and no respiratory symptoms were recorded during follow-up.
Conclusions
With good preoperative management that included RT-PCR for COVID-19 and chest radiographs, protective measures for the surgical team, and rapid patient discharge, we were able to operate on 11 humeral fractures with no COVID-19 nosocomial intrahospital infection in the patients or the shoulder surgeons who performed the surgeries.
Acknowledgment
We would like to thank all the healthcare workers of our department, especially Dr. Joan Minguell and Dr. Eric Montserrat and the trauma and orthopedic nurses of the University Hospital of Vall d'Hebron, Barcelona, Spain.
Disclaimer
The authors, their immediate families, and any research foundations with which they are affiliated have not received any financial payments or other benefits from any commercial entity related to the subject of this article.
Footnotes
Institutional review board approval was not required for this report.
References
- 1.Acter T., Uddin N., Das J., Akhter A., Choudhury T.R., Kim S. Evolution of severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) as coronavirus disease 2019 (COVID-19) pandemic: a global health emergency [Epub ahead of print] Sci Total Env. 2020 doi: 10.1016/j.scitotenv.2020.138996. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Aminian A., Safari S., Razeghian-Jahromi A., Ghorbani M., Delaney C.P. COVID-19 outbreak and surgical practice [Epub ahead of print] Ann Surg. 2020 doi: 10.1097/sla.0000000000003925. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Bell J.E., Leung B.C., Spratt K.F., Koval K.J., Weinstein J.D., Goodman D.C. Trends and variation in incidence, surgical treatment, and repeat surgery of proximal humeral fractures in the elderly. J Bone Joint Surg Am. 2011;93:121–131. doi: 10.2106/JBJS.I.01505. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Beyersmann J., Kneib T., Schumacher M., Gastmeier P. Nosocomial infection, length of stay, and time-dependent bias. Infect Control Hosp Epidemiol. 2009;30:273–276. doi: 10.1086/596020. [DOI] [PubMed] [Google Scholar]
- 5.Hospital Universitario Vall d' Hebron Dades actualització situació COVID-19—Evolució Ingressos i Altes Hospitalització. 2020. https://hospital.vallhebron.com/es/enfermedades/coronavirus-sars-cov-2/
- 6.Lauer S.A., Grantz K.H., Bi Q., Jones F.K., Zheng Q., Meredith H.R. The incubation period of coronavirus disease 2019 (COVID-19) from publicly reported confirmed cases: estimation and application. Ann Intern Med. 2020;172:577–582. doi: 10.7326/M20-0504. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Lei S., Jiang F., Su W., Chen C., Chen J., Mei W. Clinical characteristics and outcomes of patients undergoing surgeries during the incubation period of COVID-19 infection [Epub ahead of print] EClinicalMedicine. 2020;21:100331. doi: 10.1016/j.eclinm.2020.100331. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Luong-Nguyen M., Hermand H., Abdalla S., Cabrit N., Hobeika C., Brouquet A. Nosocomial infection with SARS-Cov-2 within Departments of Digestive Surgery [Epub ahead of print] J Visc Surg. 2020 doi: 10.1016/j.jviscsurg.2020.04.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Mi B., Chen L., Xiong Y., Xue H., Zhou W., Liu G. Characteristics and early prognosis of COVID-19 infection in fracture patients. J Bone Joint Surg Am. 2020;102:750–758. doi: 10.2106/jbjs.20.00390. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Minder R. Virus knocks thousands of health workers out of action in Europe. https://www.nytimes.com/2020/03/24/world/europe/coronavirus-europe-covid-19.html The New York Times.
- 11.Muñoz Vives J.M., Jornet-Gibert M., Cámara-Cabrera J., Esteban P.L., Brunet L., Delgado-Flores L. Mortality rates of patients with proximal femoral fracture in a worldwide pandemic preliminary results of the Spanish HIP-COVID observational study [Epub ahead of print] J Bone Joint Surg Am. 2020 doi: 10.2106/JBJS.20.00686. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Nuñez J.H., Sallent A., Lakhani K., Guerra-Farfan E., Vidal N., Ekhtiari S. Impact of the COVID-19 pandemic on an emergency traumatology service: experience at a tertiary trauma centre in Spain [Epub ahead of print] Injury. 2020 doi: 10.1016/j.injury.2020.05.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Orser B.A. Recommendations for endotracheal intubation of COVID-19 patients. Anesth Analg. 2020;130:1109–1110. doi: 10.1213/ANE.0000000000004803. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Prada C., Chang Y., Poolman R., Johal H., Bhandari M. Best practice for surgeons. COVID-19 evidence-based scoping review a unifying report of global recommendations. https://myorthoevidence.com/covid19
- 15.Ramanathan K., Antognini D., Combes A., Paden M., Zakhary B., Ogino M. Health-care Development Planning and provision of ECMO services for severe ARDS during the COVID-19 pandemic and other outbreaks of emerging infectious diseases. Lancet Respir. 2020;8:518–526. doi: 10.1016/S2213-2600(20)30121-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Rangan A., Handoll H., Brealey S., Jefferson L., Keding A., Martin B.C. Surgical vs nonsurgical treatment of adults with displaced fractures of the proximal humerus the PROFHER randomized clinical trial. JAMA. 2015;313:1037–1047. doi: 10.1001/jama.2015.1629. [DOI] [PubMed] [Google Scholar]
- 17.Urra S. Spain ranks first for Covid-19 infections among healthcare workers. El País. https://english.elpais.com/spanish_news/2020-04-25/spain-ranks-first-for-covid-19-infections-among-healthcare-workers.html
- 18.World Health Organization (WHO) https://ourworldindata.org/coronavirus/
- 19.Yu J., Ouyang W., Chua M.L.K., Xie C. SARS-CoV-2 transmission in patients with cancer at a tertiary care hospital in Wuhan, China [Epub ahead of print] JAMA Oncol. 2020 doi: 10.1001/jamaoncol.2020.0980. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Zhu Y., Chen W., Xin X., Yin Y., Hu J., Lv H. Epidemiologic characteristics of traumatic fractures in elderly patients during the outbreak of coronavirus disease 2019 in China [Epub ahead of print] Int Orthop. 2020 doi: 10.1007/s00264-020-04575-0. [DOI] [PMC free article] [PubMed] [Google Scholar]