As the world continues to become more connected, technology comfortably allows interactions between individuals to transcend social, cultural, and geographic barriers. Today’s society now promotes effortless video communication, seen as commonplace in routine office video conferences or on-the-go mobile phone video chatting. The breadth of coverage that this technology spans is virtually limitless, and its use in the scope of clinical health care delivery is encompassed by the term telemedicine, which enables health care to be carried out at a distance.1 Telemedicine is playing an even more important role in response to the COVID-19 pandemic.
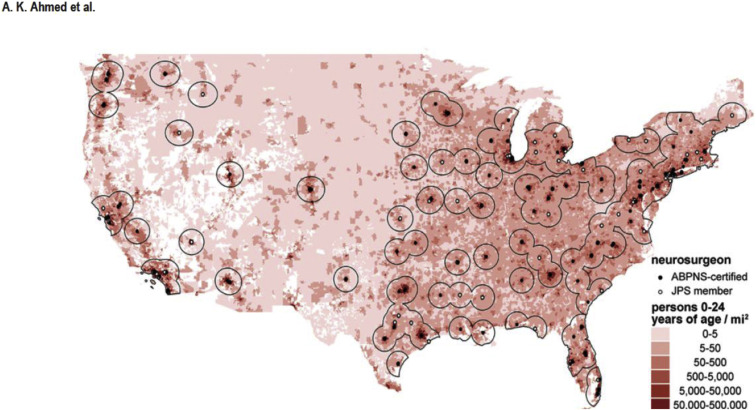
The benefit of this practice to rural communities is greater access to health care services. A dichotomy between massive metropolises and sprawling rural farmland creates an imbalance: accessible health care exists down the street for some and remains unattainable for others. In a surgical subspecialty such as pediatric neurosurgery, this dichotomy is even more apparent. The limited number of pediatric neurosurgeons in the United States results in coverage gaps, especially in sparsely populated areas. Over one fourth of children within the United States live farther than 96.56 kilometers (60 miles) from the nearest pediatric neurosurgeon (Figure 1 ), mirroring a disparity seen globally.2 , 3 Services and facilities are concentrated in urban centers, requiring patients in need to travel greater distances to receive care. In an age of booming information technology accessible globally at our fingertips, it is reasonable to want to adapt remote communication to help these patients.
Figure 1.
Radial boundaries represent a distance of 96.56 kilometers (60 miles) from a pediatric neurosurgeon. Neurosurgeons are designated by the American Board of Pediatric Neurological Surgery or as Joint Pediatric Section members, overlaying a population density map of persons 0–24 years of age per square mile. White spaces inland are areas without defined ZIP Code Tabulation Areas because of a minimal population. ABPNS, American Board of Pediatric Neurological Surgery; JPS, Joint Pediatric Section. (This image is used with permission from the Ahmed A.K., Duhaime A.C., Smith T.R. Geographic proximity to specialized pediatric neurosurgical care in the contiguous United States. J Neurosurg Pediatr. 2018;21:434–438).
Telemedicine at the Lucy Gooding Pediatric Neurosurgery Center
In 2009, coordination between Georgia Children’s Medical Services and the Lucy Gooding Pediatric Neurosurgery Center of the University of Florida College of Medicine-Jacksonville/Wolfson Children’s Hospital began as an effort to organize the Pediatric Neurosurgery Telemedicine Clinic (PNTMC). This clinic was designed to service an underserved Southeast Georgia Health District, centered in Waycross, with remote providers approximately 82 miles away in Jacksonville.4 The 2 areas involved in this partnership fit the 2 sides of the spectrum discussed previously. According to the 2018 U.S. Census data, Duval County, Florida, had 391.84 persons under the age of 24 years per square mile, whereas Ware County, Georgia, only had 12.79.
PNTMC began operation in 2011 and has served approximately 300 patients. The workflow is straightforward; referrals for patients in southeast Georgia with neurosurgical problems are evaluated at PNTMC. If they require an uncomplicated initial or follow-up pediatric neurosurgery appointment, they are scheduled for a remote visit to PNTMC. Otherwise, an in-person clinic visit at Lucy Gooding Pediatric Neurosurgery Center may be recommended to the patient. Within PNTMC operations, Georgia Children’s Medical Services nurses are on-site in Waycross and the pediatric neurosurgeon’s teleconference remotely from Jacksonville. Patient histories, prescriptions, consultations, and treatment options are presented from afar, and the next appointment can either occur in-person in Jacksonville or again remotely in Waycross as needed.
Our group has previously quantified the financial impact of the telemedicine practice for patients (with analysis of the health care system impact underway). We found that families attending PNTMC saved an average of 2.5 hours of travel time and $193.80 per visit.5 Considering that families within the region primarily come from a lower socioeconomic background, and some have multiple follow-up appointments, this amount saved is tremendous. Beyond financial data, there is an intrinsic value of access to care for these patients enabled via telemedicine, especially in an area where options are minimal. Put simply, they may not have care otherwise.
The New Barrier
To fully evaluate the potential of telemedicine, we must recognize its fundamental drawback. At its core, medicine is a field that is inherently human. The connection between a patient and provider is extraordinarily unique and surrounded by trust, connection, and oftentimes physical touch. Although telemedicine is able to remove social, cultural, and geographic barriers, another barrier takes its place. Physical touch and personal presence is lost, and the accuracy of the history and physical examination can suffer.
With this loss comes adaptation to the physical examination and the traditional patient-provider relationship. The accuracy of the examination can be maintained by peripheral devices that enhance visualization or auscultation, or by on-site allied health professionals to perform complex maneuvers such as manual muscle testing, but this is not always enough. For patients who are extremely sick, the physical presence of a physician is essential for thorough evaluation and, more importantly, to help comfort families and assuage their concerns. Ultimately, some appointments do not fit into the constraints of what telemedicine can offer.
The addition of technology into the humanistic practice of medicine should be undertaken with caution because we run the risk of creating an environment where health care is deeply impersonal. This potentially negative effect may be offset by the patient’s ready access to care. From the patient’s point of view, the overall impact of telemedicine has generally had favorable reviews.6 The prevalence of video communication elsewhere in today's society has no doubt acclimated patients and families to the idea of talking to a physician through the same technology. It is not out of the norm anymore, and culture overall is likely adjusting.
What Now?
Our experience is only one example of the health care system’s initiatives to meet the needs of the medically underserved through telemedicine. As telemedicine continues to grow inevitably, we must continue to guide it by optimizing its benefits and mitigating its pitfalls. Research continues to understand the immediate impact that telemedicine provides to patients and the health care system in fields such as pediatric neurosurgery, but it should begin to focus on longitudinal studies of patient outcomes and care differences. Once results of this nature come to fruition, we can more aptly determine the constraints on what type of visit fits the scope of telemedicine and what is more appropriate to have in person. The ability to provide care to patients in underserved regions as well as those in social isolation is a powerful aspect of telemedicine, and this should bring it to the forefront of consideration when designing new health care infrastructure in the United States and around the world.
Footnotes
Conflict of interest statement: The authors declare that the article content was composed in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
References
- 1.Darkins A.W., Cary M.A., editors. Telemedicine and Telehealth: Principles, Policies, Performance and Pitfalls. Springer; New York, NY: 2000. [Google Scholar]
- 2.Ahmed A.K., Duhaime A.C., Smith T.R. Geographic proximity to specialized pediatric neurosurgical care in the contiguous United States. J Neurosurg Pediatr. 2018;21:434–438. doi: 10.3171/2017.9.PEDS17436. [DOI] [PubMed] [Google Scholar]
- 3.Dewan M.C., Rattani A., Fieggen G. Global neurosurgery: the current capacity and deficit in the provision of essential neurosurgical care. J Neurosurg. 2018;130:1055–1064. doi: 10.3171/2017.11.JNS171500. [DOI] [PubMed] [Google Scholar]
- 4.James H.E. Pediatric neurosurgery telemedicine clinics: a model to provide care to geographically underserved areas of the United States and its territories. J Neurosurg Pediatr. 2016;25:753–757. doi: 10.3171/2016.6.PEDS16202. [DOI] [PubMed] [Google Scholar]
- 5.Hayward K., Han S.H., Simko A., James H.E., Aldana P.R. Socioeconomic patient benefits of a pediatric neurosurgery telemedicine clinic. J Neurosurg Pediatr. 2019;25:204–208. doi: 10.3171/2019.8.PEDS1925. [DOI] [PubMed] [Google Scholar]
- 6.Marcin J.P., Ellis J., Mawis R., Nagrampa E., Nesbitt T.S., Dimand R.J. Using telemedicine to provide pediatric subspecialty care to children with special health care needs in an underserved rural community. Pediatrics. 2004;113:1–6. doi: 10.1542/peds.113.1.1. [DOI] [PubMed] [Google Scholar]