Abstract
Introduction
Drug-induced QT prolongation is associated with higher cardiovascular mortality.
Material and methods
We conducted a protocol-based comprehensive review of antidepressant-induced QT prolongation in people with mental disorders.
Results
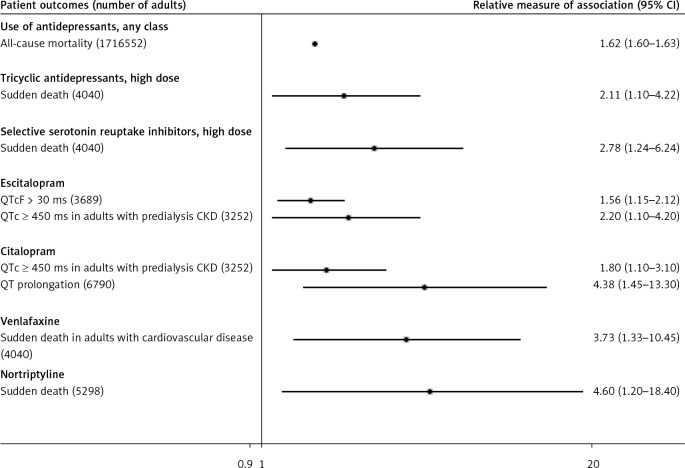
Based on findings from 47 published randomized controlled trials (RCTs), 3 unpublished RCTs, 14 observational studies, 662 case reports of torsades de pointes, and 168 cases of QT prolongation, we conclude that all antidepressants should be used only with licensed doses, and that all patients receiving antidepressants require monitoring of QT prolongation and clinical symptoms of cardiac arrhythmias. Large observational studies suggest increased mortality associated with all antidepressants (RR = 1.62, 95% CI: 1.60–1.63, number of adults: 1,716,552), high doses of tricyclic antidepressants (OR = 2.11, 85% CI 1.10–4.22), selective serotonin reuptake inhibitors (OR = 2.78, 95% CI: 1.24–6.24), venlafaxine (OR = 3.73, 95% CI: 1.33–10.45, number of adults: 4,040), and nortriptyline (OR = 4.60, 95% CI: 1.20–18.40, number of adults: 5,298).
Conclusions
Evidence regarding the risk of QT prolongation in children is sparse.
Keywords: quality of evidence, cardiovascular morbidity, drug-induced QT prolongation, antidepressants
Introduction
Observational studies provide consistent evidence that prolonged QT interval is associated with higher risk of all-cause and cardiovascular mortality [1]. Drug-induced prolongation of QT contributes to higher mortality [2, 3]. The risk of drug-induced prolongation of QT is much higher in older adults and people with multiple chronic conditions [4]. Doctors often prescribe antidepressants for licensed and off-label indications without careful assessment of baseline risk for drug-induced prolongation of QT [5, 6]. The U.S. Food and Drug Administration released several warning statements concerning the elevated risk of prolonged QT interval and potentially fatal torsades de pointes arrhythmia associated with a higher dose of citalopram during post-marketing surveillance [7, 8]. Safety of other antidepressants with respect to QT interval has been examined in cross-over trials on healthy volunteers (Supplementary Table SI) [9–21]. This rapid review focuses on all available evidence regarding the effects of antidepressants on the QT interval in children and adults with mental disorders.
Supplementary Tables
Material and methods
We used a standard recommended methodology in conducting systematic literature reviews and meta-analyses from the Cochrane Collaboration and the Agency for Healthcare Research and Quality [22, 23]. We developed an a priori protocol for a systematic literature review to answer the clinical question about the safety of antidepressants with respect to QT interval in children and adults with mental disorders.
We defined the target population as people with mental disorders treated with antidepressants. We excluded studies of healthy volunteers. Eligible interventions included antidepressants when compared with placebo or other psychotropic medications. Eligible outcomes included change in QT interval, prolongation of QT interval as reported in the studies including QT interval corrected to RR interval (QTc) ≥ 450 ms, QTc ≥ 480 ms, QTc ≥ 500 ms [24], torsades de pointes ventricular tachycardia, and sudden death.
We conducted a comprehensive search in PubMed, EMBASE, the Cochrane Library, www.clinicaltrials.gov, PharmaPendium (www.pharmapendium.com), and https://crediblemeds.org/ up to January 2018 to find systematic reviews, published and unpublished RCTs, and nationally representative controlled observational studies that reported adjusted effect estimates [22, 23]. All of the authors determined the studies’ eligibility. All citations found during the searches are stored in a reference database.
The data were extracted from the Clinical Trials Transformation Initiative (CTTI) (https://www.ctti-clinicaltrials.org/aact-database), checked for quality, and stored in the HPCC platform (High-Performance Computing Cluster, https://hpccsystems.com/).
We performed direct frequentist meta-analyses of aggregate data when definitions of the active and control intervention and patient outcomes were deemed similar for pooling [25]. We used random effects models to address inevitable differences in patient characteristics across primary RCTs. For each abstracted hypothesis, we calculated absolute risk difference and relative risk with 95% CI. We calculated number needed to treat and number of attributable events per 1000 treated with 95% CI based on statistically significant differences in absolute risks of the outcomes. We examined consistency in results across studies with χ2 tests and I2 statistics and concluded statistically significant heterogeneity if I2 was > 50% [22]. Statistically significant heterogeneity did not preclude statistical pooling [25]. However, we planned exploring heterogeneity with a priori defined patient characteristics, drug doses, and study quality if this information was available in the studies [25].
We used consensus method guidelines for systematic review and meta-analyses that do not recommend conducting post hoc analyses of statistical power [26–29]. Instead, we downgraded our confidence in true treatment effects based on calculated optimal information size as the number of patients required for an adequately powered individual trial [30]. Since power is more closely related to number of events than to sample size, we concluded imprecision in treatment effects if fewer than 250 patients experienced the event [30].
We used Statistics/Data Analysis, Stata software (StataCorp LP, College Station, Texas). Statistical significance was evaluated at a 95% confidence level.
We evaluated the quality of systematic reviews using the Assessment of Multiple Systematic Reviews (AMSTAR) [31]. For primary RCTs, we used the Cochrane risk-of-bias tool on a three-point scale: high bias, low bias, and unclear [32, 33]. A low risk of bias was assumed when RCTs met all the risk-of-bias criteria and a high risk of bias if one or more risk-of-bias criteria were not met. An unknown risk of bias was assigned for the studies with poorly reported risk-of-bias criteria. We assigned a high risk of bias to all observational studies.
The authors assigned the quality-of-evidence ratings as high, moderate, low, or very low, according to risk of bias in the body of evidence, directness of comparisons, precision and consistency in treatment effects, and evidence of reporting bias, using Grading of Recommendations Assessment, Development and Evaluation (GRADE) methodology [34].
A high quality of evidence was assigned to well-designed RCTs with consistent findings. The quality of evidence was downgraded to moderate if at least one of four quality-of-evidence criteria was not met; for example, moderate quality of evidence was assigned if there was a high risk of bias in the body of evidence or if the results were not consistent or precise. The quality of evidence was downgraded to low if two or more criteria were not met. We concluded a high risk of bias in the body of evidence if at least one RCT had high risk of bias. We downgraded the quality of evidence when we suspected high risk of publication bias due to unavailability of the results in clinicaltrials.gov or in journal articles.
A low quality of evidence was assigned to nonrandomized studies, but the rating was upgraded if there was a strong or dose-response association [35]. Evidence was defined as insufficient when no studies provided valid information about treatment effects. This approach was applied regardless of whether the results were statistically significant.
Results
Our comprehensive search in PubMed, EMBASE, the Cochrane Library, and clinicaltrials.gov up to January 2018 identified 2 individual patient data and one aggregate data meta-analysis, 8 reviews, 47 publications of RCTs, 3 unpublished RCTs, 14 observational studies, and 4 publications of case reports [7, 36–114]. We present the results from antidepressants with known and probable risk of QT prolongation.
Citalopram and escitalopram
Low-quality evidence suggests that escitalopram, when compared with placebo, increases the risk of QT prolongation (> 30 ms) in adults with mental disorders (Table I). Escitalopram prolongs the QT interval in adults hospitalized for acute coronary syndrome (Table I). Escitalopram does not increase the risk of clinically important prolongation of QT > 400 ms in RCTs (Table I). However, observational data suggest that escitalopram is associated with higher risk of clinically important prolongation of QT (≥ 450 ms) when compared with no antidepressant use in adults undergoing dialysis for chronic kidney disease (Table I). Observational studies also suggest a positive dose-response association between the larger doses of escitalopram and longer QT interval (Table I). Post-marketing surveillance detected 19 cases of prolonged QT interval and 76 cases of torsades de pointes tachycardia in people treated with escitalopram, among other medications, for various mental disorders (Supplementary Table SI).
Table I.
GRADE summary of findings: effect of escitalopram on QT interval in adults with mental disorders
| Outcome | Risk with intervention per 1000 | Risk with comparator per 1000 | Relative measure of association | No. of participants (studies) | Quality (GRADE) | Comments† |
|---|---|---|---|---|---|---|
| QTcF > 30 ms, 8 weeks | 48 | 33 Attributable events per 1000 treated 15 (2;27) |
RR = 1.45 (1.05–2.00) NNT = 68 (36–474) |
3689 (14 RCTs)[48, 52–55, 57, 58, 62–67, 72–74, 91] | Low | Favors placebo |
| QTcF > 30 ms, last assessment | 55 | 35 Attributable events per 1000 treated 20 (7;33) |
RR = 1.56 (1.15–2.12) NNT = 50 (30;153) |
3689 (14 RCTs) [48, 52–55, 57, 58, 62–67, 72–74, 91] | Low | Favors placebo |
| QTcF > 30 ms, last assessment, elderly | 56 | 42 | RR = 1.35 (0.67–2.73) | 612 (2 RCTs) [48, 52–55, 57, 58, 62–67, 72–74, 91] | Low | No difference |
| QTcF > 60 ms, last assessment, 12 weeks | 2 | 0 | RR = 0.99 (0.04–24.24) | 670 (3 RCTs) [48, 52–55, 57, 58, 62–67, 72–74, 91] | Low | No difference |
| QTcF > 60 ms, last assessment, elderly | 7 | 0 | RR = 5.17 (0.25–107.15) | 612 (2 RCTs) [48, 52–55, 57, 58, 62–67, 72–74, 91] | Low | No difference |
| QTcF > 450 ms, end, 8 weeks | 17 | 11 | RR = 1.50 (0.86–2.62) | 3689 (14 RCTs) [48, 52–55, 57, 58, 62–67, 72–74, 91] | Low | No difference |
| QTcF > 450 ms, last assessment, elderly | 56 | 26 | RR = 2.20 (0.96–5.01) | 612 (2 RCTs) [48, 52–55, 57, 58, 62–67, 72–74, 91] | Low | No difference |
| QTcF > 480 ms, last assessment, 8 weeks | 2 | 0 | RR = 6.57 (0.34–127.10) | 3689 (14 RCTs) [48, 52–55, 57, 58, 62–67, 72–74, 91] | Low | No difference |
| QTcF > 480 ms, last assessment, elderly | 3 | 0 | RR = 3.10 (0.13–75.78) | 612 (2 RCTs) [48, 52–55, 57, 58, 62–67, 72–74, 91] | Low | No difference |
| QTcF > 500 ms, last assessment, 8 weeks | 1 | 0 | RR = 4.69 (0.23–97.68) | 3689 (14 RCTs) [48, 52–55, 57, 58, 62–67, 72–74, 91] | Low | No difference |
| QTcF > 500 ms, last assessment, elderly | 3 | 0 | RR = 3.10 (0.13–75.78) | 612 (2 RCTs) [48, 52–55, 57, 58, 62–67, 72–74, 91] | Low | No difference |
| QTc (ms), adults hospitalized for acute coronary syndrome | NR | NR | MD = 0.33 (0.07–0.58) SMD = 8.00 (1.79–14.21) |
239 (1 RCT) [81] | Very low | Favors placebo |
| QTc > 450 ms, adults hospitalized for acute coronary syndrome | 17 | 0 | RR = 4.96 (0.24–102.21) | 239 (1 RCT) [81] | Very low | No difference |
| QTc ≥ 450 ms, adults with predialysis CKD | NR | NR | Adjusted OR = 2.20 (1.10–4.20) | 3252 (1 observational study) [112] | Low | Favors control (no antidepressants) |
| QT prolongation, adults with an ECG recorded after prescription of antidepressant or methadone | NR | NR | Adjusted MD = 0.58 (0.29–0.87) | 38397 (1 observational study) [86] | Low | Favors control (no antidepressants) |
| QT prolongation, escitalopram, 10 mg vs. escitalopram, 5 mg | NR | NR | Adjusted MD = 11.00 (2.18–19.82) | 38397 (1 observational study) [86] | Low | Favors lower dose |
| QT prolongation, escitalopram, 20 mg vs. escitalopram, 10 mg | NR | NR | Adjusted MD = 4.70 (1.56–7.84) | 38397 (1 observational study) [86] | Low | Favors lower dose |
Population: adults with mental disorders; Settings: any; Intervention: escitalopram at doses between 5 and 20 mg/day; Comparator: placebo or no active drug. Boldface indicates statistically significant differences at 95% CI. †We concluded that there is no difference in outcomes between active and control interventions based on p-value > 0.05 and inability to reject null hypotheses but without post hoc analysis of the statistical power to detect true differences. GRADE – Grading of Recommendations Assessment, Development and Evaluation, NNT – number needed to treat, NNTp – number needed to treat to prevent an outcome in one patient (when the outcome is more probable with control intervention), NR – not reported, OR – odds ratio, RCT – randomized controlled trial, RR – relative risk. Between studies differences in continuous outcomes: MD – mean difference in absolute values of continuous outcomes between intervention and comparator, SMD – standardized mean difference between intervention and comparator where the magnitude of the effect is defined as small (SMD, 0–0.5 standard deviations), moderate (SMD, 0.5–0.8 standard deviations), and large (SMD > 0.8 standard deviations).
Moderate-quality evidence suggests that citalopram prolongs the QT interval compared with placebo in adults with mental disorders (Table II). Citalopram does not increase the risk of clinically important prolongation of QT > 400 ms in RCTs (Table II). In contrast with RCTs, observational data suggest that citalopram is associated with higher risk of clinically important prolongation of QT (≥ 450 ms) compared with no antidepressant use in adults undergoing dialysis for chronic kidney disease (Table II). Observational studies also suggest a positive dose-response association between the larger doses of citalopram and longer QT intervals (Supplementary Table SII). Much less expected is the evidence from observational studies that a citalopram dose reduction to < 40 mg following the FDA warning is associated with a higher risk of all-cause mortality, arrhythmias, and CVD-related hospitalizations (Supplementary Table SII). Post-marketing surveillance detected 36 cases of prolonged QT intervals and 196 cases of torsades de pointes tachycardia in people treated with citalopram, among other medications, for various mental disorders (Supplementary Table SI).
Table II.
GRADE Summary of findings: effect of citalopram on QT interval in adults with mental disorders
| Outcome | Risk with intervention per 1000 | Risk with comparator per 1000 | Relative measure of association | No. of participants (studies) | Quality (GRADE) | Comments† |
|---|---|---|---|---|---|---|
| QTc > 30 ms, 3 weeks | 74 | 11 | RR = 6.85 (0.86–54.59) | 186 (1 RCT) [96] | Very low | No difference |
| QTc > 60 ms | 33 | 0 | RR = 3.19 (0.14–75.49) | 62 (1 RCT) [107] | Very low | No difference |
| QTc > 450 ms for men or > 470 ms for women, 3 weeks | 32 | 11 | RR = 2.94 (0.31–27.71) | 186 (1 RCT) [96] | Very low | No difference |
| QTc > 500 ms | 0 | 0 | RR inestimable | 62 (1 RCT) [107] | Very low | No difference |
| QTC [ms] | NR | NR | MD = 6.56 (0.07–13.04) | 892 (6 RCTs) [7, 71, 94, 96, 107] | Moderate | Favors control |
| QTc ≥ 450 ms, adults with predialysis CKD | NR | NR | Adjusted OR = 1.80 (1.00–3.10) | 3252 (1 observational study) [112] | Low | Favors control |
| QT prolongation | NR | NR | Adjusted MD = 0.10 (0.02–0.18) | 38397 (1 observational study) [86] | Low | Favors control |
| QT prolongation | NR | NR | Adjusted OR = 4.38 (1.45–13.30) | 6790 (1 observational study) [87] | Low | Favors control |
| Sudden death with cardiovascular disease | NR | NR | Adjusted OR = 1.81 (0.81–4.03) | 4040 (1 observational study) [76] | Low | No difference |
| Sudden death without cardiovascular disease | NR | NR | Adjusted OR = 1.70 (0.50–5.99) | 4040 (1 observational study) [76] | Low | No difference |
Population: adults with mental disorders, Settings: any, Intervention: citalopram, any dose, Comparator: placebo or no active drug. Boldface indicates statistically significant differences at 95% CI. †We concluded that there is no difference in outcomes between active and control interventions based on p-value > 0.05 and inability to reject null hypotheses but without post hoc analysis of the statistical power to detect true differences. GRADE – Grading of Recommendations Assessment, Development and Evaluation, NR – not reported, OR – odds ratio, RCT – randomized controlled trial, RR – relative risk. Between studies differences in continuous outcomes: MD – mean difference in absolute values of continuous outcomes between intervention and comparator, SMD – standardized mean difference between intervention and comparator where the magnitude of the effect is defined as small (SMD, 0–0.5 standard deviations), moderate (SMD, 0.5–0.8 standard deviations), and large (SMD > 0.8 standard deviations).
Systematic reviews of published case reports found only a few cases of QT prolongation and torsades de pointes tachycardia in adults taking citalopram in doses between 20 and 60 mg/day [83, 88, 106]. The authors concluded that reporting of citalopram-induced adverse effects was incomplete and monitoring of the safety outcomes for citalopram and other antidepressants was inadequate [83, 88, 106].
We found no pediatric RCTs or high-quality observational studies that examined the effects from escitalopram or citalopram on QT interval.
Desvenlafaxine and venlafaxine
Low-quality evidence from RCTs suggests that desvenlafaxine does not increase the QT interval in adults with various mental disorders (Table III). Post-marketing surveillance detected two cases of torsades de pointes tachycardia in adult women treated with desvenlafaxine among other medications (Supplementary Table SI). Post-approval studies conducted by the pharmaceutical company suggest an association between desvenlafaxine overdose and QT prolongation in adults with concurrent alcohol and drug consumption [115]. The evidence regarding the effects of desvenlafaxine on the QT interval in children is insufficient [113].
Table III.
GRADE summary of findings: effect of desvenlafaxine on QT interval in adults with mental disorders
| Outcome | Risk with intervention per 1000 | Risk with comparator per 1000 | Relative measure of association | No. of participants (studies) | Quality (GRADE) | Comments† | |
|---|---|---|---|---|---|---|---|
| Adults with major depressive disorder: | |||||||
| QT prolonged, desvenlafaxine 50 mg/day | 0 | 7 | RR = 0.17 (0.01–4.07) | 427 (1 RCT) [110] | Very low | No difference | |
| QTcF change, desvenlafaxine 200 mg/day | NR | NR | MD = 1.50 (–0.88 – 3.88) | 2476 (4 RCTs) [115] | Low | No difference | |
| QTcF change, desvenlafaxine 600 mg/day | NR | NR | MD = –2.43 (–4.90 – 0.04) | 2476 (4 RCTs) [115] | Low | No difference | |
| Postmenopausal women with moderate to severe vasomotor symptoms: | |||||||
| QT prolonged | 1 | 0 | RR = 2.96 (0.12–72.59) | 2118 (1 RCT) [90] | Very low | No difference | |
| Adults with painful diabetic peripheral neuropathy: | |||||||
| Ventricular tachycardia | 3 | 0 | RR = 0.85 (0.03–20.57) | 412 (2 RCTs) [93] | Low | No difference | |
Population: adults with mental disorders, Settings: any, Intervention: desvenlafaxine, Comparator: placebo or no active drug. †We concluded that there is no difference in outcomes between active and control interventions based on p-value > 0.05 and inability to reject null hypotheses but without post hoc analysis of the statistical power to detect true differences.
Low-quality evidence from observational studies suggests that venlafaxine is associated with increased risk of sudden death in adults with cardiovascular diseases (Table IV). Observational studies suggest no association between venlafaxine and QT prolongation in adults without cardiovascular disease, in adults undergoing hemodialysis for chronic kidney failure, or in adults with deliberate overdosing of this drug (Table IV). Published case reports also suggest the association between therapeutic doses of venlafaxine and QT prolongation in older adults taking concomitant drugs [37, 105, 116]. Post-approval studies conducted by the pharmaceutical company suggest the association between venlafaxine overdose and QT prolongation in adults with concurrent alcohol and drug consumption [117]. Post-marketing surveillance detected 7 cases of prolonged QT interval and 58 cases of torsades de pointes tachycardia in people treated with venlafaxine among other medications (Supplementary Table SI). The evidence regarding the effects of venlafaxine on the QT interval in children is insufficient.
Table IV.
GRADE summary of findings: effect of venlafaxine on QT interval in adults with mental disorders
| Outcome | Risk with intervention per 1000 | Risk with comparator per 1000 | Relative measure of association | No. of participants (studies) | Quality (GRADE) | Comments† |
|---|---|---|---|---|---|---|
| QT change | NR | NR | Adjusted MD = 0.01 (–0.01 – 0.03) | 38397 (1 observational study) [86] | Low | No difference |
| Sudden death with cardiovascular disease | NR | NR | Adjusted OR = 3.73 (1.33–10.45) | 4040 (1 observational study) [76] | Low | Favors control, drugs without known effects on QT |
| Sudden death without cardiovascular disease | NR | NR | Adjusted OR = 0.67 (0.07–6.19) | 4040 (1 observational study) [76] |
Low | No difference |
| QRS > 100 ms, venlafaxine deliberate self-poisoning (DSP) vs. tricyclic antidepressant overdose | NR | NR | Adjusted OR = 0.60 (0.20–1.20) | 538 (1 observational study) [56] | Very low | No difference |
| QTc ≥ 450 ms, adults with predialysis chronic kidney disease | NR | NR | Adjusted OR = 1.10 (0.50–2.70) | 3252 (1 observational study) [112] | Low | No difference |
Population: adults with mental disorders; Settings: any; Intervention: venlafaxine; Comparator: placebo or no active drug. Boldface indicates statistically significant differences at 95% CI. †We concluded that there is no difference in outcomes between active and control interventions based on p-value > 0.05 and inability to reject null hypotheses but without post hoc analysis of the statistical power to detect true differences.
Fluoxetine
Very low-quality evidence suggests that fluoxetine does not cause QT prolongation when compared with placebo in adults with mental disorders (Supplementary Table SIII). Low-quality evidence suggests that fluoxetine is not associated with increased risk of cardiac death in adults with or without concurrent cardiovascular disease (Supplementary Table SIII).
Paroxetine
Moderate-quality evidence suggests that paroxetine does not increase the QT interval in adults with mental disorders (Supplementary Table SIV). Low-quality evidence suggests that paroxetine administration is not associated with higher risk of sudden death in adults with mental disorders, with or without comorbid cardiovascular disease (Supplementary Table SIV).
Very low-quality evidence from a single RCT suggests that paroxetine decreases the length of the QT interval when compared with placebo or with imipramine in children with depression or obsessive-compulsive disorder (Supplementary Table SV).
Bupropion
Low-quality evidence suggests that bupropion, 75–300 mg/day, is not associated with QT prolongation in adults with mental disorders (Supplementary Table SVI).
Duloxetine
Very low-quality evidence suggests that duloxetine, 80–120 mg/day, does not prolong QT in adults with mental disorders (Supplementary Table SVII).
Fluvoxamine
Very low-quality evidence from a small single RCT suggests that fluvoxamine decreases the QT interval when compared with placebo in adults with mental disorders (Supplementary Table SVIII).
Sertraline
Low-quality evidence suggests that sertraline prolongs the QT interval but is not associated with higher risk of sudden death (Supplementary Table SVIII).
Trazodone
Low-quality evidence suggests that trazodone is not associated with clinically important QT prolongation in adults with mental disorders and comorbid renal failure undergoing dialysis (Supplementary Table SVIII).
Amitriptyline
Very low-quality evidence from a small single RCT suggests that amitriptyline does not cause QT prolongation in children with functional gastrointestinal disorders (Supplementary Table SIX). Very low-quality evidence from a single RCT suggests that amitriptyline cream does not cause QT prolongation in adults with diabetic peripheral neuropathy (Supplementary Table SIX). Low-quality evidence from observational studies suggests that amitriptyline is associated with longer QT interval in adults with mental disorders in a dose-dependent manner (Supplementary Table SIX). Observational studies suggest no association between amitriptyline with clinically important QT prolongation or sudden death (Supplementary Table SIX).
Imipramine
Very low-quality evidence from a small single RCT suggests that imipramine increases the risk of clinically important QT prolongation compared with placebo in children with depression or obsessive-compulsive disorder (Supplementary Table SX).
Clomipramine
Low-quality evidence suggests that clomipramine is not associated with higher risk of sudden death in adults with mental disorders, with or without cardiovascular disease (Supplementary Table SXI).
Dosulepin
Low-quality evidence suggests that dosulepin is not associated with higher risk of sudden death in adults with mental disorders, with or without cardiovascular disease (Supplementary Table SXI).
Mirtazapine
Low-quality evidence suggests that mirtazapine is not associated with QT prolongation (Supplementary Table SXI).
Nortriptyline
Low-quality evidence suggests that nortriptyline is not associated with QT prolongation (Supplementary Table SXI). However, nortriptyline is associated with higher risk of sudden death (Supplementary Table SXI).
Drug class effect
The evidence from large observational studies suggests that antidepressants with conditional possible or known risk of torsades de pointes are associated with higher odds of all-cause mortality after adjustment for other confounding factors in adults with mental disorders. Tricyclic antidepressants are not associated with higher risk of sudden death except at higher doses. Selective serotonin reuptake inhibitors are associated with higher risk of sudden death specifically in adults with comorbid cardiovascular disease. The adjusted odds of sudden death are the highest after high doses of selective serotonin reuptake inhibitors. However, the adjusted odds of clinically important QT prolongation are lower after overdose of selective serotonin reuptake inhibitors when compared with overdose of tricyclic antidepressants (Table V).
Table V.
GRADE summary of findings: association between antidepressant classes and QT interval and sudden death in adults with mental disorders
| Outcome | Risk with intervention per 1000 | Risk with comparator per 1000 | Relative measure of association | No. of participants (studies) | Quality (GRADE) | Comments† | |
|---|---|---|---|---|---|---|---|
| Use of antidepressants, any class vs. no antidepressants: | |||||||
| All-cause mortality, 5 years | NR | NR | Adjusted RR = 1.62 (1.60–1.63) | 1,716,552 (1 observational study) [108] | Low | Favors control | |
| Antidepressants without known risk for torsades de pointes: | |||||||
| All-cause mortality, 5 years | NR | NR | Adjusted RR = 0.99 (0.94–1.05) | 1,716,552 (1 observational study) [108] | Low | No difference | |
| Antidepressants with conditional risk for torsades de pointes: | |||||||
| All-cause mortality, 5 years | NR | NR | Adjusted RR = 1.25 (1.22–1.28) | 1,716,552 (1 observational study) [108] | Low | Favors control | |
| Antidepressants with possible risk for torsades de pointes: | |||||||
| All-cause mortality, 5 years | NR | NR | Adjusted RR = 1.63 (1.61–1.67) | 1,716,552 (1 observational study) [108] | Low | Favors control | |
| Antidepressants with known risk for torsades de pointes: | |||||||
| All-cause mortality, 5 years | NR | NR | Adjusted RR = 1.53 (1.51–1.56) | 1,716,552 (1 observational study) [108] | Low | Favors control | |
| Tricyclic antidepressants: | |||||||
| Sudden death | NR | NR | Adjusted OR for other drugs with known QT effect = 1.28 (0.84–1.96) | 4040 (1 observational study) [76] | Low | No difference | |
| Sudden death | NR | NR | Adjusted OR = 1.41 (0.93–2.13) | 4040 (1 observational study) [76] | Low | No difference | |
| Sudden death with cardiovascular disease | NR | NR | Adjusted OR = 1.34 (0.79–2.28) | 4040 (1 observational study) [76] | Low | No difference | |
| Sudden death without cardiovascular disease | NR | NR | Adjusted OR = 1.61 (0.83–3.13) | 4040 (1 observational study) [76] | Low | No difference | |
| Sudden death, high-dose antidepressants | NR | NR | Adjusted OR = 2.11 (1.10–4.22) | 4040 (1 observational study) [76] | Low | Favors control | |
| Sudden death, moderate-dose antidepressants | NR | NR | Adjusted OR = 0.85 (0.42–1.73) | 4040 (1 observational study) [76] | Low | No difference | |
| Sudden death, low-dose antidepressants | NR | NR | Adjusted OR = 1.60 (0.72–3.56) | 4040 (1 observational study) [76] | Low | No difference | |
| Selective serotonin reuptake inhibitors: | |||||||
| QTc interval prolongation | NR | NR | Adjusted OR = 1.10 (0.50–2.00) | 794 (1 observational study) [104] | Very low | No difference | |
| Sudden death | NR | NR | Adjusted OR for other drugs with known QT effect = 1.78 (1.24–2.55) | 4040 (1 observational study) [76] | Low | Favors control | |
| Sudden death | NR | NR | Adjusted OR = 1.89 (1.34–2.69) | 4040 (1 observational study) [76] | Low | Favors control | |
| Sudden death with cardiovascular disease | NR | NR | Adjusted OR = 2.04 (1.33–3.13) | 4040 (1 observational study) [76] | Low | Favors control | |
| Sudden death without cardiovascular disease | NR | NR | Adjusted OR = 1.63 (0.86–3.10) | 4040 (1 observational study) [76] | Low | No difference | |
| Sudden death, high antidepressant dose | NR | NR | Adjusted OR = 2.78 (1.24–6.24) | 4040 (1 observational study) [76] | Low | Favors control | |
| Sudden death, moderate antidepressant dose | NR | NR | Adjusted OR = 1.55 (0.96–2.49) | 4040 (1 observational study) [76] | Low | No difference | |
| Sudden death, low antidepressant dose | NR | NR | Adjusted OR = 1.83 (0.70–4.78) | 4040 (1 observational study) [76] | Low | No difference | |
| Selective serotonin reuptake inhibitor overdose vs. tricyclic antidepressant overdose: | |||||||
| QRS > 100 | NR | NR | Adjusted OR = 0.20 (0.10–0.40) | 538 (1 observational study) [56] | Very low | Favors selective serotonin reuptake inhibitors | |
Population: adults with mental disorders; Settings: any; Intervention: tricyclic antidepressants or selective serotonin reuptake inhibitors; comparator: no active drug class. Boldface indicates statistically significant differences at 95% CI. †We concluded that there is no difference in outcomes between active and control interventions based on p-value > 0.05 and inability to reject null hypotheses but without post hoc analysis of the statistical power to detect true differences.
Discussion
Our review of clinical trials found mostly low quality of evidence that escitalopram and citalopram are associated with higher risk of QT prolongation in adults, and imipramine increases the risk of QT prolongation in children. Observational studies demonstrate that selective serotonin reuptake inhibitors (specifically venlafaxine and nortriptyline) and high doses of tricyclic antidepressants are associated with higher risk of sudden death specifically in adults with comorbid cardiovascular disease (Figure 1).
Figure 1.
Increased risk of patient outcomes in association with antidepressants in adults with mental disorders
Post-marketing surveillance suggests that serotonin reuptake inhibitors and tricyclic antidepressants are associated with torsades de pointes (total of 662 cases) and QT prolongation (168 cases) in people taking antidepressants among other drugs. The direct evidence regarding comparative safety of antidepressants is insufficient.
We downgraded the quality of evidence due to the high risk of bias and small number of events in the RCTs. Most clinical studies did not have statistical power to detect higher risk of ventricular tachycardia. We further downgraded the quality of evidence due to reporting bias, because only a very small proportion of primary studies that examined benefits of antidepressants also examined drug-induced QT prolongation. Post-marketing surveillance is the major safety source, but case reporting depends on clinician opinion regarding the association between ventricular tachycardia and administration of antidepressants.
Differences in the definition of QT prolongation and correction methods precluded indirect analysis of comparative safety between antidepressants. Primary studies did not evaluate factors that increase susceptibility to QT prolongation and torsades de pointes, including electrolyte disorders, chronic inflammation, baseline cardiovascular disease, comorbidities, or concomitant medications [118–120]. The evidence is lacking regarding interaction between antidepressant use with clinical and genetic risk factors for torsade de pointes [121]. Evolving research suggests genetic predisposition associated with QT prolongation and torsades de pointes [121–124]. Stratification algorithms predicting the risk of acquired QT prolongation have been proposed [122, 123, 125]. Larger sample size and longitudinal modeling with multivariate analyses are required to develop valid prediction pharmacogenomic algorithms of acquired QT prolongation for individual patients taking antidepressants and other proarrhythmic drugs [121, 124]. Genetic mutations in hERG (human-ether-a-go-go-related gene) potassium channel kinetic abnormalities and other genes responsible for cardiac function and repolarization may contribute to complex mechanisms of antidepressant-induced QT prolongation [126–128]. Valid prediction algorithms should also address factors affecting drug clearance, thereby resulting in a relative overdose and an associated increased risk of proarrhythmia [129].
Available guidelines emphasize the importance of individual assessment of probable benefits and harms, including QT prolongation, when selecting antidepressants for people with high risk of QT prolongation and cardiac arrhythmias [130, 131]. Guidelines recommend standardized assessment of QT interval in patients who need antidepressants and are at high risk of QT prolongation and cardiac arrhythmias [131–133]. Guidelines recommend therapeutic drug monitoring of antidepressants to prevent overdose and consequential adverse effects, including QT prolongation [134]. Guidelines do not address optimal risk mitigation that may include drug dose reduction or switching as well as individualized assessment and management of comorbidities and concomitant drugs [135]. For instance, the evidence suggests that a simple adjustment of escitalopram or citalopram administration is not enough to ensure better patient outcomes [92, 109, 135]. Drug labels recommend against administration of antidepressants in combination with other drugs that are known to prolong QT interval and in people with bradycardia, hypokalemia or hypomagnesemia, or congenital prolongation of the QT interval [9, 11–21, 115, 117]. Despite these recommendations, the prevalence of polypharmacy with multiple proarrhythmic drugs is high [2, 4, 136].
Our review has limitations. Our analyses are based only on the available evidence. Despite our efforts to include all published and unpublished clinical trials, observational studies, and post-marketing data, we do not know how many unregistered and unpublished studies have been conducted. We detected a substantial reporting bias but did not contact principal investigators of all studies of antidepressants that did not report QT prolongation. Analyzing aggregate data, we could not overcome differences in outcome definitions. Despite all these limitations, we attempted a comprehensive review of all available evidence and consistent appraisal of the quality of evidence with a conservative GRADE approach.
Our review has implications for clinical practice. Baseline risk of cardiac arrhythmias should be assessed in all patients treated with antidepressants [137]. High-risk patients should be monitored for clinical symptoms indicating the occurrence of cardiac arrhythmias (e.g., dizziness, palpitations, or syncope) and should receive ECG monitoring for the prolongation of QT interval [138, 139]. Multidisciplinary coordinated care should be implemented to avoid polypharmacy with antidepressants and other proarrhythmic drugs [137, 140].
Our review has policy implications. Prescriber compliance with the licensed drug use should be routinely evaluated using electronic health records [141–143]. Proactive post-marketing pharmacovigilance applications should be implemented to decrease the risk of drug-induced QT prolongation and cardiac arrhythmias [144–149].
Our review has research implications. Future research should examine long-term comparative safety of antidepressant drugs in patients of different ages as well as those with baseline cardiovascular risk, multiple comorbidities, and concomitant drug use [118]. Future research is needed to develop a valid risk stratification algorithm that includes pharmacokinetic factors (e.g., old age and renal impairment) and pharmacodynamic factors that modulate repolarization (e.g., potassium level, genetic mutations, hypertrophy and heart failure, and concomitant use of proarrhythmic drugs) [118, 122, 125].
In conclusion, in adults with indications for antidepressants and elevated risk of QT prolongation, in order to avoid prolongation of the QT interval and reduce the risk of ventricular tachycardia, clinicians should not recommend citalopram or escitalopram,
In adults with indications for antidepressants and low baseline risk of QT prolongation, clinicians may recommend licensed doses of antidepressants in addition to close monitoring of QT interval and clinical symptoms indicating occurrence of cardiac arrhythmias (e.g., dizziness, palpitations, or syncope) to avoid prolongation of QT interval and reduce the risk of ventricular tachycardia.
Conflict of interest
The authors declare no conflict of interest.
References
- 1.Zhang Y, Post WS, Blasco-Colmenares E, Dalal D, Tomaselli GF, Guallar E. Electrocardiographic QT interval and mortality: a meta-analysis. Epidemiology 2011; 22: 660-70. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Jackobson G, Carmel NN, Lotan D, Kremer A, Justo D. Reckless administration of QT interval-prolonging agents in elderly patients with drug-induced torsades de pointes. Z Gerontol Geriatr 2018; 51: 41-7. [DOI] [PubMed] [Google Scholar]
- 3.Schachtele S, Tumena T, Gassmann KG, Fromm MF, Maas R. Co-prescription of QT-interval prolonging drugs: an analysis in a large cohort of geriatric patients. PloS One 2016; 11: e0155649. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Franchi C, Ardoino I, Rossio R, et al. . Prevalence and risk factors associated with use of QT-prolonging drugs in hospitalized older people. Drugs Aging 2016; 33: 53-61. [DOI] [PubMed] [Google Scholar]
- 5.Wong J, Motulsky A, Abrahamowicz M, Eguale T, Buckeridge DL, Tamblyn R. Off-label indications for antidepressants in primary care: descriptive study of prescriptions from an indication based electronic prescribing system. BMJ 2017; 356: j603. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Schroder C, Dorks M, Kollhorst B, et al. . Outpatient antidepressant drug use in children and adolescents in Germany between 2004 and 2011. Pharmacoepidemiol Drug Saf 2017; 26: 170-9. [DOI] [PubMed] [Google Scholar]
- 7.U.S. Food and Drug Administration. Abnormal heart arrhythmias associated with high foses of Celexa (citalopram hydrobromide). FDA Safety Communication 2011; https://www.fda.gov/Drugs/DrugSafety/ucm269086.htm#data.
- 8.U.S. Food and Drug Administration. FDA Drug Safety Communication: Revised recommendations for Celexa (citalopram hydrobromide) related to a potential risk of abnormal heart rhythms with high doses. Drug Safety and Availability 2012; https://www.fda.gov/Drugs/DrugSafety/ucm297391.htm.
- 9.Remeron (mirtazapine tablets) package insert 2016; https://www.accessdata.fda.gov/drugsatfda_docs/label/2016/020415s030lbl.pdf.
- 10.Anafranil (clomipramine capsules). Package insert 2017; https://www.accessdata.fda.gov/drugsatfda_docs/label/2017/019906s040lbl.pdf.
- 11.Norpramin (desipramine). Package insert 2014; https://www.accessdata.fda.gov/drugsatfda_docs/label/2014/014399s069lbl.pdf.
- 12.Tofranil (imipramine). Package insert 2017; https://www.accessdata.fda.gov/drugsatfda_docs/label/2012/040903lbl.pdf.
- 13.Pamelor (nortriptyline HCl capsules). Package insert 2016; https://www.accessdata.fda.gov/drugsatfda_docs/label/2014/018013s063lbl.pdf.
- 14.Trazodone HCl tablets. Package insert 2016; https://www.accessdata.fda.gov/drugsatfda_docs/label/2015/071196s062lbl.pdf.
- 15.Prozac (fluoxetine hydrochloride). Package insert 2017; https://www.accessdata.fda.gov/drugsatfda_docs/label/2017/018936s103,021235s023lbl.pdf.
- 16.Paxil (paroxetine) tablet. Package insert 2017; https://www.accessdata.fda.gov/drugsatfda_docs/label/2017/020031s074lbl.pdf.
- 17.Zoloft (sertraline). Package insert 2017; https://www.accessdata.fda.gov/drugsatfda_docs/label/2017/019839s091lbl.pdf.
- 18.Amitriptyline tablets. Package insert 2014; https://www.accessdata.fda.gov/drugsatfda_docs/label/2017/019839s091lbl.pdf.
- 19.Sinequan (doxepin). Package insert 2014; https://www.accessdata.fda.gov/drugsatfda_docs/label/2010/022036lbl.pdf.
- 20.Luvox (fluvoxamine). Package insert 2014; https://www.accessdata.fda.gov/drugsatfda_docs/label/2017/021519s009lbl.pdf.
- 21.Wellbutrin SR (bupropion). Package insert 2017; https://www.accessdata.fda.gov/drugsatfda_docs/label/2009/018644s039s040.pdf.
- 22.Higgins J, Green S (eds). Cochrane handbook for systematic reviews of interventions. Version 5.1.0. The Cochrane Collaboration, 2011. Available from http://handbook.cochrane.org.
- 23.Slutsky J, Atkins D, Chang S, Sharp BA. AHRQ series paper 1: comparing medical interventions: AHRQ and the effective health-care program. J Clin Epidemiol 2010; 63: 481-3. [DOI] [PubMed] [Google Scholar]
- 24.Rabkin SW, Cheng XB. Nomenclature, categorization and usage of formulae to adjust QT interval for heart rate. World J Cardiol 2015; 7: 315-25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Fu R, Gartlehner G, Grant M, et al. . Conducting quantitative synthesis when comparing medical interventions: AHRQ and the Effective Health Care Program. J Clin Epidemiol 2011; 64: 1187-97. [DOI] [PubMed] [Google Scholar]
- 26.Levine M, Ensom MH. Post hoc power analysis: an idea whose time has passed? Pharmacotherapy 2001; 21: 405-9. [DOI] [PubMed] [Google Scholar]
- 27.Goodman SN, Berlin JA. The use of predicted confidence intervals when planning experiments and the misuse of power when interpreting results. Ann Inter Med 1994; 121: 200-6. [DOI] [PubMed] [Google Scholar]
- 28.Yuan KH, Maxwell S. On the post hoc power in testing mean differences. J Educ Beha Stat 2005; 30: 141-67. [Google Scholar]
- 29.Agency for Healthcare Research and Quality: Methods Guide for Effectiveness and Comparative Effectiveness Reviews. AHRQ Publication No. 10(14)-EHC063-EF 2014; Rockville, MD: https://effectivehealthcare.ahrq.gov/index.cfm/search-for-guides-reviews-and-reports/?pageaction=displayproduct&productid=318. [PubMed] [Google Scholar]
- 30.Guyatt GH, Oxman AD, Kunz R, et al. . GRADE guidelines 6. Rating the quality of evidence--imprecision. J Clin Epidemiol 2011; 64: 1283-93. [DOI] [PubMed] [Google Scholar]
- 31.Shea BJ, Hamel C, Wells GA, et al. . AMSTAR is a reliable and valid measurement tool to assess the methodological quality of systematic reviews. J Clin Epidemiol 2009; 62: 1013-20. [DOI] [PubMed] [Google Scholar]
- 32.Viswanathan M, Berkman ND, Dryden DM, Hartling L. Assessing risk of bias and confounding in observational studies of interventions or exposures: further development of the RTI Item Bank. AHRQ Methods for Effective Health Care 2013; Contract No. 290-2007-10056-I. [PubMed] [Google Scholar]
- 33.Higgins JP, Altman DG, Gotzsche PC, et al. . The Cochrane Collaboration’s tool for assessing risk of bias in randomised trials. BMJ 2011; 343: d5928. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Grading of Recommendations Assessment Development and Evaluation (GRADE) Workgin Group. GRADE Handbook. http://gdt.guidelinedevelopment.org/central_prod/_design/client/handbook/handbook.html#h.fueh5iz0cor4.
- 35.Guyatt GH, Oxman AD, Sultan S, et al.; Group GW: GRADE guidelines: 9 . Rating up the quality of evidence. J Clin Epidemiol 2011; 64: 1311-6. [DOI] [PubMed] [Google Scholar]
- 36.Beach SR, Celano CM, Sugrue AM, et al. . QT Prolongation, torsades de pointes, and psychotropic medications: a 5-year update. Psychosomatics 2018; 59: 105-22. [DOI] [PubMed] [Google Scholar]
- 37.Kok R, Nolen W, Heeren T. Cardiovascular changes associated with venlafaxine in the treatment of late-life depression. Am J Geriatr Psychiatr 2007; 15: 725. [DOI] [PubMed] [Google Scholar]
- 38.Upward J, Edwards J, Goldie A, Waller D. Comparative effects of fluoxetine and amitriptyline on cardiac function. Br J Clin Pharmacol 1988; 26: 399-402. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Edwards JG, Goldie A, Papayanni-Papasthatis S. Effect of paroxetine on the electrocardiogram. Psychopharmacology 1989; 97: 96-8. [DOI] [PubMed] [Google Scholar]
- 40.Kuhs H, Rudolf GAE. Cardiovascular effects of paroxetine. Psychopharmacology 1990; 102: 379-82. [DOI] [PubMed] [Google Scholar]
- 41.Fisch C, Knoebel SB. Electrocardiographic findings in sertraline depression trials. Drug Invest 1992; 4: 305-12. [Google Scholar]
- 42.Baker B, Dorian P, Sandor P, et al. . Electrocardiographic effects of fluoxetine and doxepin in patients with major depressive disorder. J Clin Psychopharmacol 1997; 17: 15-21. [DOI] [PubMed] [Google Scholar]
- 43.Roose SP, Glassman AH, Attia E, Woodring S, Giardina EGV, Bigger JT Jr. Cardiovascular effects of fluoxetine in depressed patients with heart disease. Am J Psychiatry 1998; 155: 660-5. [DOI] [PubMed] [Google Scholar]
- 44.Roose SP, Laghrissi-Thode F, Kennedy JS, et al. . Comparison of paroxetine and nortriptyline in depressed patients with ischemic heart disease. JAMA 1998; 279: 287-91. [DOI] [PubMed] [Google Scholar]
- 45.Slavíček J, Paclt I, Hamplová J, Kittnar O, Trefný Z, Horáček BM. Antidepressant drugs and heart electrical field. Physiol Res 1998; 47: 297-300. [PubMed] [Google Scholar]
- 46.Strik JJMH, Honig A, Lousberg R, et al. . Efficacy and safety of fluoxetine in the treatment of patients with major depression after first myocardial infarction: findings from a double-blind, placebo-controlled trial. Psychosomat Med 2000; 62: 783-9. [DOI] [PubMed] [Google Scholar]
- 47.Yeragani VK, Pohl R, Jampala VC, Balon R, Ramesh C, Srinivasan K. Effects of nortriptyline and paroxetine on QT variability in patients with panic disorder. Depression Anxiety 2000; 11: 126-30. [PubMed] [Google Scholar]
- 48.Burke WJ, Gergel I, Bose A. Fixed-dose trial of the single isomer SSRI escitalopram in depressed outpatients. J Clinl Psychiatry 2002; 63: 331-6. [DOI] [PubMed] [Google Scholar]
- 49.Detke MJ, Lu Y, Goldstein DJ, Hayes JR, Demitrack MA. Duloxetine, 60 mg once daily, for major depressive disorder: a randomized double-blind placebo-controlled trial. J Clin Psychiatry 2002; 63: 308-15. [DOI] [PubMed] [Google Scholar]
- 50.Glassman AH, O’Connor CM, Califf RM, et al. . Sertraline treatment of major depression in patients with acute MI or unstable angina. JAMA 2002; 288: 701-9. [DOI] [PubMed] [Google Scholar]
- 51.Goldstein DJ, Mallinckrodt C, Lu Y, Demitrack MA. Duloxetine in the treatment of major depressive disorder: a double-blind clinical trial. J Clin Psychiatry 2002; 63: 225-31. [DOI] [PubMed] [Google Scholar]
- 52.Wade A, Michael Lemming O, Bang Hedegaard K. Escitalopram 10 mg/day is effective and well tolerated in a placebo-controlled study in depression in primary care. Int Clin Psychopharmacol 2002; 17: 95-102. [DOI] [PubMed] [Google Scholar]
- 53.Lepola UM, Loft H, Reines EH. Escitalopram (10-20 mg/day) is effective and well tolerated in a placebo-controlled study in depression in primary care. Int Clin Psychopharmacol 2003; 18: 211-7. [DOI] [PubMed] [Google Scholar]
- 54.Ninan PT, Ventura D, Wang J. Escitalopram is effective and well tolerated in the treatment of severe depression. Poster presented at the Congress of the American Psychiatric Association, May 17-22, 2003, San Francisco. [Google Scholar]
- 55.Stahl SM, Gergel I, Li D. Escitalopram in the treatment of panic disorder: a randomized, double-blind, placebo-controlled trial. J Clin Psychiatry 2003; 64: 1322-7. [DOI] [PubMed] [Google Scholar]
- 56.Whyte IM, Dawson AH, Buckley NA. Relative toxicity of venlafaxine and selective serotonin reuptake inhibitors in overdose compared to tricyclic antidepressants. Q J Med 2003; 96: 369-74. [DOI] [PubMed] [Google Scholar]
- 57.Alexopoulos GS, Gordon J, Zhang D. A placebo-controlled trial of escitalopram and sertraline in the treatment of major depressive disorder. Neuropsychopharmacology 2004; 29 (Suppl): S87. [Google Scholar]
- 58.Davidson JRT, Bose A, Korotzer A, Zheng H. Escitalopram in the treatment of generalized anxiety disorder: double-blind, placebo controlled, flexible-dose study. Depression Anxiety 2004; 19: 234-40. [DOI] [PubMed] [Google Scholar]
- 59.Detke MJ, Wiltse CG, Mallinckrodt CH, McNamara RK, Demitrack MA, Bitter I. Duloxetine in the acute and long-term treatment of major depressive disorder: a placebo-and paroxetine-controlled trial. Eur Neuropsychopharmacol 2004; 14: 457-70. [DOI] [PubMed] [Google Scholar]
- 60.Goldstein DJ, Lu Y, Detke MJ, Wiltse C, Mallinckrodt C, Demitrack MA. Duloxetine in the treatment of depression: a double-blind placebo-controlled comparison with paroxetine. J Clin Psychopharmacol 2004; 24: 389-99. [DOI] [PubMed] [Google Scholar]
- 61.Isbister GK, Bowe SJ, Dawson A, Whyte IM. Relative toxicity of selective serotonin reuptake inhibitors (SSRIs) in overdose. J Toxicol Clin Toxicol 2004; 42: 277-85. [DOI] [PubMed] [Google Scholar]
- 62.Lader M, Stender K, Bürger V, Nil R. Efficacy and tolerability of escitalopram in 12-and 24-week treatment of social anxiety disorder: randomised, double-blind, placebo-controlled, fixed-dose study. Depression Anxiety 2004; 19: 241-8. [DOI] [PubMed] [Google Scholar]
- 63.Rapaport MH, Bose A, Zheng H. Escitalopram continuation treatment prevents relapse of depressive episodes. J Clin Psychiatry 2004; 65: 44-9. [DOI] [PubMed] [Google Scholar]
- 64.Goodman WK, Bose A, Wang Q. Treatment of generalized anxiety disorder with escitalopram: pooled results from double-blind, placebo-controlled trials. J Affect Dis 2005; 87: 161-7. [DOI] [PubMed] [Google Scholar]
- 65.Kasper S, De Swart H, Andersen HF. Escitalopram in the treatment of depressed elderly patients. Am J Geriatr Psychiatry 2005; 13: 884-91. [DOI] [PubMed] [Google Scholar]
- 66.Kasper S, Stein DJ, Loft H, Nil R. Escitalopram in the treatment of social anxiety disorder: randomised, placebo-controlled, flexible-dosage study. Br J Psychiatry 2005; 186: 222-6. [DOI] [PubMed] [Google Scholar]
- 67.Baldwin DS, Huusom AKT, Mæhlum E. Escitalopram and paroxetine in the treatment of generalised anxiety disorder: randomised, placebo-controlled, double-blind study. Br J Psychiatry 2006; 189: 264-72. [DOI] [PubMed] [Google Scholar]
- 68.Krulewicz S, Carpenter DJ, Fong R, et al. . Analysis of electrocardiographic data following use of paroxetine in pediatric depression and obsessive-compulsive disorder. J Am Acad Child Adolesc Psychiatry 2006; 45: 422-30. [DOI] [PubMed] [Google Scholar]
- 69.Nelson JC, Lu Pritchett Y, Martynov O, Yu JY, Mallinckrodt CH, Detke MJ. The safety and tolerability of duloxetine compared with paroxetine and placebo: a pooled analysis of 4 clinical trials. Prim Care Companion J Clin Psychiatry 2006; 8: 212-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Goldstein DJ. Duloxetine in the treatment of major depressive disorder. Neuropsychiatr Dis Treatment 2007; 3: 193-209. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Lespérance F, Frasure-Smith N, Koszycki D, et al. . Effects of citalopram and interpersonal psychotherapy on depression in patients with coronary artery disease. The Canadian Cardiac Randomized Evaluation of Antidepressant and Psychotherapy Efficacy (CREATE) trial. JAMA 2007; 297: 367-79. [DOI] [PubMed] [Google Scholar]
- 72.Stein DJ, Andersen EW, Tonnoir B, Fineberg N. Escitalopram in obsessive-compulsive disorder: a randomized, placebo-controlled, paroxetine-referenced, fixed-dose, 24-week study. Curr Med Res Opin 2007; 23: 701-11. [DOI] [PubMed] [Google Scholar]
- 73.Bose A, Korotzer A, Gommoll C, Li D. Randomized placebo-controlled trial of escitalopram and venlafaxine XR in the treatment of generalized anxiety disorder. Depression Anxiety 2008; 25: 854-61. [DOI] [PubMed] [Google Scholar]
- 74.Bose A, Li D, Gandhi C. Escitalopram in the acute treatment of depressed patients aged 60 years or older. Am J Geriatr Psychiatry 2008; 16: 14-20. [DOI] [PubMed] [Google Scholar]
- 75.Brzozowska A, Werner B. Observation of QTc prolongation in an adolescent girl during fluvoxamine pharmacotherapy. J Child Adolesc Psychopharmacol 2009; 19: 591-2. [DOI] [PubMed] [Google Scholar]
- 76.Jolly K, Gammage MD, Cheng KK, Bradburn P, Banting MV, Langman MJ. Sudden death in patients receiving drugs tending to prolong the QT interval. Br J Clin Pharmacol 2009; 68: 743-51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Study Evaluating the Safety and Efficacy of Desvenlafaxine Succinate for Vasomotor Symptoms in Menopausal Women. https://clinicaltrials.gov/ct2/show/NCT00683800, 2010.
- 78.EpiCept Corporation. A Study of the Efficacy and Safety of Amitriptyline/Ketamine Topical Cream in Patients With Diabetic Peripheral Neuropathy. https://clinicaltrialsgov/ct2/show/NCT00476151, 2011.
- 79.A Study in Relapse Prevention of Treatment-Resistant Depression. https://clinicaltrials.gov/ct2/show/NCT00958568, 2012.
- 80.Fagiolini A, Comandini A, Catena Dell’Osso M, Kasper S. Rediscovering trazodone for the treatment of major depressive disorder. CNS Drugs 2012; 26: 1033-49. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Hanash JA, Hansen BH, Hansen JF, Nielsen OW, Rasmussen A, Birket-Smith M. Cardiovascular safety of one-year escitalopram therapy in clinically nondepressed patients with acute coronary syndrome: results from the DEpression in patients with Coronary ARtery Disease (DECARD) trial. J Cardiovasc Pharmacol 2012; 60: 397-405. [DOI] [PubMed] [Google Scholar]
- 82.NCT01598324: Functional and Neurochemical Correlates of Treatment Response in Major Depressive Disorder: https://clinicaltrials.gov/ct2/show/NCT01598324, 2012.
- 83.Vieweg WV, Hasnain M, Howland RH, et al. . Citalopram, QTc interval prolongation, and torsades de pointes. How should we apply the recent FDA ruling? Am J Med 2012; 125: 859-68. [DOI] [PubMed] [Google Scholar]
- 84.Archer DF, Pinkerton JV, Guico-Pabia CJ, Hwang E, Cheng RF. Cardiovascular, cerebrovascular, and hepatic safety of desvenlafaxine for 1 year in women with vasomotor symptoms associated with menopause. Menopause 2013; 20: 47-56. [DOI] [PubMed] [Google Scholar]
- 85.Bardai A, Amin AS, Blom MT, et al. . Sudden cardiac arrest associated with use of a non-cardiac drug that reduces cardiac excitability: evidence from bench, bedside, and community. Eur Heart J 2013; 34: 1506-16. [DOI] [PubMed] [Google Scholar]
- 86.Castro VM, Clements CC, Murphy SN, et al. . QT interval and antidepressant use: a cross sectional study of electronic health records. BMJ 2013; 346: f288. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Girardin FR, Gex-Fabry M, Berney P, Shah D, Gaspoz JM, Dayer P. Drug-induced long QT in adult psychiatric inpatients: the 5-year cross-sectional ECG screening outcome in psychiatry study. Am J Psychiatry 2013; 170: 1468-76. [DOI] [PubMed] [Google Scholar]
- 88.Kogut C, Crouse EB, Vieweg WV, et al. . Selective serotonin reuptake inhibitors and torsades de pointes: new concepts and new directions derived from a systematic review of case reports. Therap Adv Drug Safe 2013; 4: 189-98. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Pinkerton JV, Archer DF, Guico-Pabia CJ, Hwang E, Cheng RF. Maintenance of the efficacy of desvenlafaxine in menopausal vasomotor symptoms: a 1-year randomized controlled trial. Menopause 2013; 20: 38-46. [DOI] [PubMed] [Google Scholar]
- 90.Pinkerton JV, Constantine G, Hwang E, Cheng RF. Desvenlafaxine compared with placebo for treatment of menopausal vasomotor symptoms: a 12-week, multicenter, parallel-group, randomized, double-blind, placebo-controlled efficacy trial. Menopause 2013; 20: 28-37. [DOI] [PubMed] [Google Scholar]
- 91.Thase ME, Larsen KG, Reines E, Kennedy SH. The cardiovascular safety profile of escitalopram. Eur Neuropsychopharmacol 2013; 23: 1391-400. [DOI] [PubMed] [Google Scholar]
- 92.Zivin K, Pfeiffer PN, Bohnert AS, et al. . Evaluation of the FDA warning against prescribing citalopram at doses exceeding 40 mg. Am J Psychiatry 2013; 170: 642-50. [DOI] [PubMed] [Google Scholar]
- 93.Allen R, Sharma U, Barlas S. Clinical experience with desvenlafaxine in treatment of pain associated with diabetic peripheral neuropathy. J Pain Res 2014; 7: 339-51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Beach SR, Kostis WJ, Celano CM, et al. . Meta-analysis of selective serotonin reuptake inhibitor-associated QTc prolongation. J Clinic Psychiatry 2014; 75: e441-9. [DOI] [PubMed] [Google Scholar]
- 95.Chogle A, Saps M. Electrocardiograms changes in children with functional gastrointestinal disorders on low dose amitriptyline. World J Gastroenterol 2014; 20: 11321-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Drye LT, Spragg D, Devanand DP, et al. . Changes in QTc interval in the citalopram for agitation in Alzheimer’s disease (CitAD) randomized trial. PLoS One 2014; 9: e98426. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Endicott J, Lam RW, Hsu MA, Fayyad R, Boucher M, Guico-Pabia CJ. Improvements in quality of life with desvenlafaxine 50 mg/d vs placebo in employed adults with major depressive disorder. J Affect Disord 2014; 166: 307-14. [DOI] [PubMed] [Google Scholar]
- 98.Jasiak NM, Bostwick JR. Risk of QT/QTc prolongation among newer non-SSRI antidepressants. Ann Pharmacother 2014; 48: 1620-8. [DOI] [PubMed] [Google Scholar]
- 99.Lam RW, Endicott J, Hsu MA, Fayyad R, Guico-Pabia C, Boucher M. Predictors of functional improvement in employed adults with major depressive disorder treated with desvenlafaxine. Int Clin Psychopharmacol 2014; 29: 239-51. [DOI] [PubMed] [Google Scholar]
- 100.Porsteinsson AP, Drye LT, Pollock BG, et al. . Effect of citalopram on agitation in Alzheimer disease: the CitAD randomized clinical trial. JAMA 2014; 311: 682-91. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Portman DJ, Kaunitz AM, Kazempour K, Mekonnen H, Bhaskar S, Lippman J. Effects of low-dose paroxetine 7.5 mg on weight and sexual function during treatment of vasomotor symptoms associated with menopause. Menopause 2014; 21: 1082-90. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Ries R, Sayadipour A. Management of psychosis and agitation in medical-surgical patients who have or are at risk for prolonged QT interval. J Psychiatr Pract 2014; 20: 338-44. [DOI] [PubMed] [Google Scholar]
- 103.Spindelegger CJ, Papageorgiou K, Grohmann R, et al. . Cardiovascular adverse reactions during antidepressant treatment: a drug surveillance report of German-speaking countries between 1993 and 2010. Int J Neuropsychopharmacol 2018; 4: 18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.van Haelst IM, van Klei WA, Doodeman HJ, et al. . QT interval prolongation in users of selective serotonin reuptake inhibitors in an elderly surgical population: a cross-sectional study. J Clin Psychiatry 2014; 75: 15-21. [DOI] [PubMed] [Google Scholar]
- 105.Bavle A. Venlafaxine induced QTc interval prolongation in a therapeutic dose. Asian J Psychiatr 2015; 16: 63-4. [DOI] [PubMed] [Google Scholar]
- 106.Tampi RR, Balderas M, Carter KV, et al. . Citalopram, QTc prolongation, and torsades de pointes. Psychosomatics 2015; 56: 36-43. [DOI] [PubMed] [Google Scholar]
- 107.Barnes TR, Leeson VC, Paton C, et al. . Antidepressant Controlled Trial For Negative Symptoms In Schizophrenia (ACTIONS): a double-blind, placebo-controlled, randomised clinical trial. Health Tech Assess 2016; 20: 1-46. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.Danielsson B, Collin J, Jonasdottir Bergman G, Borg N, Salmi P, Fastbom J. Antidepressants and antipsychotics classified with torsades de pointes arrhythmia risk and mortality in older adults: a Swedish nationwide study. Br J Clin Pharmacol 2016; 81: 773-83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Rector TS, Adabag S, Cunningham F, Nelson D, Dieperink E. Outcomes of citalopram dosage risk mitigation in a veteran population. Am J Psychiatry 2016; 173: 896-902. [DOI] [PubMed] [Google Scholar]
- 110.Reddy S, Fayyad R, Edgar CJ, Guico-Pabia CJ, Wesnes K. The effect of desvenlafaxine on cognitive functioning in employed outpatients with major depressive disorder: a substudy of a randomized, double-blind, placebo-controlled trial. J Psychopharmacol 2016; 30: 559-67. [DOI] [PubMed] [Google Scholar]
- 111.Ray WA, Chung CP, Murray KT, Hall K, Stein CM. High-dose citalopram and escitalopram and the risk of out-of-hospital death. J Clin Psychiatry 2017; 78: 190-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112.Snitker S, Doerfler RM, Soliman EZ, et al. ; CSI. Association of QT-prolonging medication use in CKD with electrocardiographic manifestations. Clin J Am Soc Nephrol 2017; 12: pii: . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113.Uchida M, Spencer AE, Kenworthy T, et al. . A pilot study: cardiac parameters in children receiving new-generation antidepressants. J Clin Psychopharmacol 2017; 37: 359-62. [DOI] [PubMed] [Google Scholar]
- 114.Eli Lilly and Company. A Study of Fluoxetine in Major Depressive Disorder (MDD) Short-Term Dosing. https://clinicaltrials.gov/ct2/show/NCT01808612, 2015.
- 115.Pristiq (desvenlafaxine) extended-release tablets. Package insert 2018; https://www.accessdata.fda.gov/drugsatfda_docs/label/2018/021992s042lbl.pdf.
- 116.Letsas K, Korantzopoulos P, Pappas L, Evangelou D, Efremidis M, Kardaras F. QT interval prolongation associated with venlafaxine administration. Int J Cardiol 2006; 109: 116-7. [DOI] [PubMed] [Google Scholar]
- 117.Effexor XR (venlafaxine extended-release capsules). Package insert 2017; https://www.accessdata.fda.gov/drugsatfda_docs/label/2017/020699s110s111lbl.pdf.
- 118.Haverkamp W, Breithardt G, Camm AJ, et al. . The potential for QT prolongation and pro-arrhythmia by non-anti-arrhythmic drugs: clinical and regulatory implications: report on a Policy Conference of the European Society of Cardiology. Cardiovasc Res 2000; 47: 219-33. [DOI] [PubMed] [Google Scholar]
- 119.Lazzerini PE, Laghi-Pasini F, Bertolozzi I, et al. . Systemic inflammation as a novel QT-prolonging risk factor in patients with torsades de pointes. Heart 2017; 103: 1821-9. [DOI] [PubMed] [Google Scholar]
- 120.Chu T, Azevedo K, Ernst AA, Sarangarm D, Weiss SJ. A comparison of QTc intervals in alcohol withdrawal patients versus acute coronary syndrome patients. South Med J 2017; 110: 475-9. [DOI] [PubMed] [Google Scholar]
- 121.Sauer AJ, Newton-Cheh C. Clinical and genetic determinants of torsade de pointes risk. Circulation 2012; 125: 1684-94. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 122.Itoh H, Crotti L, Aiba T, et al. . The genetics underlying acquired long QT syndrome: impact for genetic screening. Eur Heart J 2016; 37: 1456-64. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 123.Duchatelet S, Crotti L, Peat RA, et al. . Identification of a KCNQ1 polymorphism acting as a protective modifier against arrhythmic risk in long-QT syndrome. Circ Cardiovasc Genetics 2013; 6: 354-61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 124.Avery CL, Sitlani CM, Arking DE, et al. . Drug-gene interactions and the search for missing heritability: a cross-sectional pharmacogenomics study of the QT interval. Pharmacogenom J 2014; 14: 6-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 125.Lavedan C, Volpi S, Licamele L. Method of predicting a predisposition to qt prolongation. 2018; http://www.freepatentsonline.com/y2018/0002759.html.
- 126.Romero L, Trenor B, Yang PC, Saiz J, Clancy CE. In silico screening of the impact of hERG channel kinetic abnormalities on channel block and susceptibility to acquired long QT syndrome. J Mol Cell Cardiol 2015; 87: 271-82. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 127.Shieh CC, Coghlan M, Sullivan JP, Gopalakrishnan M. Potassium channels: molecular defects, diseases, and therapeutic opportunities. Pharmacol Rev 2000; 52: 557-94. [PubMed] [Google Scholar]
- 128.Boutjdir M, Lazzerini PE, Capecchi PL, Laghi-Pasini F, El-Sherif N. Potassium channel block and novel autoimmune-associated long QT syndrome. Card Electrophysiol Clin 2016; 8: 373-84. [DOI] [PubMed] [Google Scholar]
- 129.Turner JR, Karnad DR, Kothari S. Cardiovascular Safety in Drug Development and Therapeutic Use: New Methodologies and Evolving Regulatory Landscapes. 2016, Springer, eBook, doi 10.1007/978-3-319-40347-2. [DOI] [Google Scholar]
- 130.U.S. Department of Health and Human Services FaDA, Center for Drug Evaluation and Research (CDER), Center for Biologics Evaluation and Research (CBER). E14 Clinical Evaluation of QT/QTc Interval Prolongation and Proarrhythmic Potential for Non-Antiarrhythmic Drugs. Guidance for Industry 2017; http://www.fda.gov/Drugs/GuidanceComplianceRegulatoryInformation/Guidances/default.htm.
- 131.Drew BJ, Ackerman MJ, Funk M, et al. ; the American Heart Association Acute Cardiac Care Committee of the Council on Clinical Cardiology, the Council on Cardiovascular Nursing, and the American College of Cardiology Foundation. Prevention of torsades de pointes in hospital settings: a scientific statement from the American Heart Association and the American College of Cardiology Foundation. Circulation 2010; 121: 1047-60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 132.Rautaharju PM, Surawicz B, Gettes LS. AHA/ACCF/HRS recommendations for the standardization and interpretation of the electrocardiogram: IV. The ST segment, T and U waves, and the QT interval a scientific statement from the American Heart Association Electrocardiography and Arrhythmias Committee, Council on Clinical Cardiology; the American College of Cardiology Foundation; and the Heart Rhythm Society Endorsed by the International Society for Computerized Electrocardiology. J Am Coll Cardiol 2009; 53: 982-91. [DOI] [PubMed] [Google Scholar]
- 133.Goldberger JJ, Cain ME, Hohnloser SH, et al. . ; American Heart Association/American College of Cardiology Foundation/Heart Rhythm Society scientific statement on noninvasive risk stratification techniques for identifying patients at risk for sudden cardiac death: a scientific statement from the American Heart Association Council on Clinical Cardiology Committee on Electrocardiography and Arrhythmias and Council on Epidemiology and Prevention. Circulation 2008; 118: 1497-518. [PubMed] [Google Scholar]
- 134.Hiemke C, Baumann P, Bergemann N, et al. . AGNP consensus guidelines for therapeutic drug monitoring in psychiatry: update 2011. Pharmacopsychiatry 2011; 21: 195-235. [DOI] [PubMed] [Google Scholar]
- 135.Gerlach LB, Kales HC, Maust DT, et al. . Unintended consequences of adjusting citalopram prescriptions following the 2011 FDA warning. Am J Geriatr Psychiatry 2017; 25: 407-14. [DOI] [PubMed] [Google Scholar]
- 136.Rodday AM, Triedman JK, Alexander ME, et al. . Electrocardiogram screening for disorders that cause sudden cardiac death in asymptomatic children: a meta-analysis. Pediatrics 2012; 129: e999-1010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 137.Shulman M, Miller A, Misher J, Tentler A. Managing cardiovascular disease risk in patients treated with antipsychotics: a multidisciplinary approach. J Multidiscip Healthcare 2014; 7: 489-501. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 138.Shah AA, Aftab A, Coverdale J. QTc prolongation with antipsychotics: is routine ECG monitoring recommended? J Psychiatr Pract 2014; 20: 196-206. [DOI] [PubMed] [Google Scholar]
- 139.Shen WK, Sheldon RS, Benditt DG, et al. . 2017 ACC/AHA/HRS Guideline for the Evaluation and Management of Patients With Syncope: Executive Summary: A Report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines and the Heart Rhythm Society. Circulation 2017; 136: e25-59. [DOI] [PubMed] [Google Scholar]
- 140.Hashimoto Y, Tensho M. Effect of pharmacist intervention on physician prescribing in patients with chronic schizophrenia: a descriptive pre/post study. BMC Health Serv Res 2016; 16: 150. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 141.Seroquel XR (quetiapine fumarate extended-release tablets) package insert. 2017; Wilmington, DE: https://www.accessdata.fda.gov/drugsatfda_docs/label/2017/020639s020065lbl.pdf. [Google Scholar]
- 142.Geodon (ziprasidone) package insert. New York, NY: 2017. https://www.accessdata.fda.gov/drugsatfda_docs/label/2009/020825s035,020919s023lbl.pdf [Google Scholar]
- 143.Bouvy JC, Koopmanschap MA, Shah RR, Schellekens H. The cost-effectiveness of drug regulation: the example of thorough QT/QTc studies. Clin Pharmacol Ther 2012; 91: 281-8. [DOI] [PubMed] [Google Scholar]
- 144.Beninger P, Ibara MA. Pharmacovigilance and biomedical informatics: a model for future development. Clin Therap 2016; 38: 2514-25. [DOI] [PubMed] [Google Scholar]
- 145.Black C, Tagiyeva-Milne N, Helms P, Moir D. Pharmacovigilance in children: detecting adverse drug reactions in routine electronic healthcare records. A systematic review. Br J Clin Pharmacol 2015; 80: 844-54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 146.Sarker A, Ginn R, Nikfarjam A, et al. . Utilizing social media data for pharmacovigilance: a review. J Biomed Informat 2015; 54: 202-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 147.Dias P, Penedones A, Alves C, Ribeiro CF, Marques FB. The role of disproportionality analysis of Pharmacovigilance databases in safety regulatory actions: a systematic review. Curr Drug Safety 2015; 10: 234-50. [DOI] [PubMed] [Google Scholar]
- 148.Raschi E, Poluzzi E, Salvo F, et al. . The contribution of national spontaneous reporting systems to detect signals of torsadogenicity: issues emerging from the ARITMO Project. Drug Safety 2016; 39: 59-68. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 149.Robinson J, Doogan D. A placebo controlled study of the cardiovascular effects of fluvoxamine and clovoxamine in human volunteers. Br J Clin Pharmacol 1982; 14: 805-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplementary Tables