Abstract
Background and Aim:
There is a paucity of regional data on acute postoperative pain. The present study was conducted with an aim to assess the acute postoperative pain experiences, its interference with ADLs, emotions, sleep, IPR and satisfaction with pain management among patients who had undergone elective surgeries.
Methods:
In this observational study, 200 postoperative adult patients; who had undergone elective surgery were interviewed using American Pain Society's Patient Outcome and Satisfaction Survey Questionnaire. Pain perception and interference of pain with ADLs, emotions, sleep, and IPR was measured on 0–10 numerical scale and satisfaction on 6 point Likert scale, i.e., very satisfied to very dissatisfied.
Results:
There was high incidence (82.5%) of acute postoperative pain experience and mean score for worst episodes of pain was significantly high, i.e., 7.6 ± 1.5, which had significant interference with ADLs (5.6 ± 2.1), sleep (3.6 ± 1.7), and emotions (3.6 ± 1.6). Majority of patients reported that pain was assessed only once (17%) or twice (48.5%) in each shift. Despite of poor pain control, a large number of patients were satisfied with overall pain treatment (69%), and response of physicians (81%) and nurses (62%) for their pain complaints. Acute pain score was directly associated with the duration of postoperative hospital stay (P = 0.001).
Conclusion:
Acute postoperative pain was inadequately assessed and undertreated but still a large number of participants were satisfied with acute postoperative pain management probably because patients expects that pain is inevitable after surgery. Postoperative pain had significant interference with ADLs, emotions and sleep of patients, which may affect postoperative comfort and recovery.
Key words: Interference of pain, pain perception, postoperative pain, satisfaction
INTRODUCTION
Acute pain is an invariable phenomenon in the postoperative period and is still considered to be a great challenge in developing countries like India. Poorly managed pain during postoperative period not only results in discomfort and suffering of patients, but also associated with many complications.[1,2]
Despite the latest advancement in pain management, postoperative pain still remains undertreated.[3,4] A national survey highlighted that even in specialized centres of acute pain services, patients were undertreated for pain and even assessment of pain was not done routinely.[5] Several studies have been conducted in India on incidence of pain in different conditions; however in a questionnaire based survey it was reported that 70% patients suffer from inadequate pain management in India.[6] There is a paucity of data about the incidence of acute postoperative pain in tertiary care public hospitals, its interference with patient's activities of daily living (ADLs), sleep, emotions and interpersonal relationship (IPR), and patients' satisfaction with the pain management practices. Therefore, this present study was planned to assess the incidence of acute postoperative pain, its interference with ADLs, sleep, emotions and IPR, as well as patients' satisfaction with overall acute postoperative pain treatment and response of physicians and nurses for their pain complaints.
METHODS
This observational study was conducted at a tertiary care teaching public hospital in Uttarakhand to assess the patients' acute postoperative pain experience, its interference with ADLs, sleep, emotions, IPR, and patients' satisfaction with acute postoperative pain management.
Total 200 postoperative patients underwent elective surgeries in the departments of orthopaedics, general surgery, and obstetrics and gynaecology during month of March–August, 2019 and were admitted in recovery room were recruited in the study. Postoperative patients aged 18 years and above who underwent elective surgeries and patients who received intravenous postoperative analgesia were included in the present study. However, patients with emergency surgeries, impaired cognition, serious/life threatening illness, history of substance abuse, and antiepileptic medications use were excluded from the study.
Ethical permission was obtained from institution ethics committee vide letter no. ECR/736/Inst/UK/2015/RR-18. Participants were informed about the purpose of research and ensured about anonymity and confidentiality of the information. A written informed voluntary participation consent was taken from each study participant.
Data were collected through a 15–20-min face-to-face interview with each participant using standardized and reliable (r = 0.75)[7] tool, i.e., American Pain Society Patient Outcome Questionnaire (APS-POQ). Questionnaire consisted two sections; Section-I: 15 items related to socio-demographic characteristics and clinical profile of participants (duration of hospitalization, diagnosis, type of surgery, type of analgesics used and assessment of pain); Section-II: APS-POQ; to assess patients' pain experience (the presence of pain in last 24-h on yes/no response; average pain, worst episodes of pain in first 24-h and pain at 24-h postoperatively was assessed on 0 (no pain) to 10 (worst pain), numerical scale); pain's interference on patients' ADLs, sleep, emotions, IPR was assessed on 0 (no interfere) to 10 (completely interfere) numerical scale; patients' satisfaction with overall pain treatment, and response of physicians and nurses for the postoperative pain complaints was measured on 6 point Likert scale, i.e., very dissatisfied, slightly dissatisfied, dissatisfied, slightly satisfied, satisfied, and very satisfied. Further, it included items related to nurses' use of non-pharmacological methods for pain relief (yes/no, with details about types of methods) and degree to which doctors and nurses encouraged them to use non-pharmacological methods for pain relief on three-point scale, i.e., never, sometimes and often. An item was also included to rate patient involvement in decision for pain management on 0 (not at all) to 10 (very much) numerical scale.
Sample size was estimated by using formula (Z1− a/2)2 (p) (q)/d28 with absolute error of 5%, confidence interval 95% and minimum estimated sample size was 178 participants, while considering 10% non-response rate, total 200 sample size was considered for the present study. A sample of 200 eligible participants, who met the inclusion and exclusion criteria were selected using consecutive sampling technique.
Data were coded and then entered to excel sheets and Statistical Package for the Social Sciences (SPSS 21.0) was used for statistical analysis. Descriptive and inferential statistics were used for data analysis. Socio-demographic characteristics, patients' clinical variables, pain assessment frequency, pain management interventions, and patient satisfaction with overall pain treatment, and response of physicians and nurses for the postoperative pain complaints were presented using frequency and percentage. While pain perception and its interference with ADLs, emotions, IPR was analyzed and presented by using mean, standards deviation, as well as frequency and percentage. One-way ANOVA was used to determine association of average pain during 24-h postoperatively with selected clinical variables of participants at 0.05 level of significance.
RESULTS
Average age of participants in years was 36.1 ± 13.1, where more than one third of them (38.5%) were in the age group of 18–28 years; followed by 25.5% were in the age group of 40–50 years. Majority of the participants (142, 71%) were female and a significant number of them were educated either up to secondary (27%) or not formally educated (25.5%).
Majority of the participants (91.5%) stayed in hospitals for < 2 weeks for orthopaedics (34.5%), general surgery (21%), obstetrics (29%), and gynaecological (15.5%) surgeries. The commonest site of pain was abdomen (56.5%), followed by lower limb (18.5%), back (7%), upper limb (4.5%), and other areas (13.5%), such as perineum, neck, breast, and groin [Table 1].
Table 1.
Clinical profile, pain assessment and management of participants n=200
| Variables | f (%) |
|---|---|
| Duration of hospitalization | |
| <2 Weeks | 183 (91.5) |
| 2-4 Weeks | 14 (7.0) |
| >4 Weeks | 03 (1.5) |
| Location of pain | |
| Abdomen | 113 (56.5) |
| Lower limbs | 37 (18.5) |
| Upper limbs | 09 (4.5) |
| Back | 14 (7.0) |
| Perineum/neck/breast/groin | 27 (13.5) |
| Frequency of pain assessment | |
| Never | 24 (12.0) |
| Once | 34 (17.0) |
| Twice | 97 (48.5) |
| Thrice | 45 (22.5) |
| Did nurses use non-pharmacological method to relieve pain? | 161 (80.5) |
| No | 39 (19.5) |
| Yes | |
| Type of surgery | |
| Orthopaedics | 69 (34.5) |
| General surgery | 42 (21.0) |
| Obstetrics | 58 (29.0) |
| Gynaecology | 31 (15.5) |
| Type of analgesics | |
| NSAIDs | 118 (59.0) |
| Opioids + NSAIDs | 60 (30.0) |
| Opioids | 10 (5.0) |
| Opioids + NSAIDs + Muscle relaxant | 12 (6.0) |
| Experience of pain in past 24 h | |
| Yes | 200 (100) |
| No | 00 (00) |
| Did Nurse or Doctor encourage to use non-pharmacological methods? | |
| Never | 162 (81.0) |
| Sometimes | 37 (18.5) |
| Often | 01 (0.5) |
Majority of participants reported that pain was assessed only once (17%) or twice (48.5%) during each shift; while even few of them (12%) mentioned that it was never done until they reported it. All the study participants (100%) reported pain during first 24 h postoperatively. Majority of patients were treated with non-steroidal anti-inflammatory drugs (NSAIDs) alone (59.0%) or in combination with opioids (30%); while very few of them received only opioids (5%) or opioids in combination with NSAIDs and muscle relaxants (6%) for pain management. Surprisingly, majority of participants (80.5%) reported that nurses did not use any non-pharmacological methods to relieve their pain. Similarly, majority of them (81%) reported that doctors or nurses never encouraged them to use non-pharmacological interventions for acute postoperative pain relief [Table 1].
Subjective postoperative pain perception of participant was assessed using 0 to 10 numerical rating scale (where '0' means no pain and '10' indicates worst pain). Pain was assessed for three categories, i.e., average pain during first 24-h postoperatively, episodes of worst pain during first 24-h after surgery and level of pain at 24-h postoperatively. Mean worst pain experienced during first 24-h after surgery was alarmingly high, i.e., 7.6 ± 1.5. Similarly, mean pain score for the average pain during first 24-h and at 24-h postoperatively was also reasonably high, i.e., 4.9 ± 1.5 and 4.6 ± 1.8, respectively. Incidence of moderate-to-severe level of acute postoperative pain was also significantly high; where 82.5% of participants experienced moderate-to-severe level of average pain during first 24-h of surgery.
Data regarding interference of postoperative pain with participants' ADLs, emotions, IPR, and sleep revealed that majority of participants (85.5%) had moderate-to-severe level of interference with their ADLs and more than half of the participants also reported moderate-to-severe level of interference with emotions (54.5%) and sleep (51%) [Table 2].
Table 2.
Acute postoperative pain perception and it impact on ADLs, emotions, IPR and sleep of participants n=200
| Pain perception during first 24-h postoperatively | ||||
|---|---|---|---|---|
| Pain perception | Mean±SD | Perceived level of pain |
||
| Mild f (%) | Moderate f (%) | Severe f (%) | ||
| Average pain | 4.9±1.5 | 35 (17.5) | 134 (67.0) | 31 (15.5) |
| Worst episodes of pain | 7.6±1.5 | 01 (0.5) | 44 (22.0) | 155 (77.5) |
| Pain at 24 h | 4.6±1.8 | 61 (30.5) | 103 (51.5) | 36 (18.0) |
| Impact on patients’ ADLs, sleep, emotions and IPR | ||||
| Domains of impact | Mean±SD | Level of impact |
||
| Slight f (%) | Moderate f (%) | Severe f (%) | ||
| Activities of daily living (ADLs) | 5.6±2.1 | 29 (14.5) | 111 (55.5) | 60 (30.0) |
| Sleep | 3.6±1.7 | 98 (49.0) | 64 (32.0) | 38 (19.0) |
| Emotions | 3.6±1.6 | 91 (45.5) | 76 (38.0) | 33 (16.5) |
| Interpersonal relationships (IPR) | 1.9±2.2 | 161 (80.5) | 29 (14.5) | 10 (05.0) |
Scoring of pain on 0-10 scale: Mild: 1-3; Moderate: 4-6; Sever: 7-10. Scoring of impact on 0-10 scale: Slight: 1-3; Moderate: 4-6; Sever: 7-10
Surprisingly, significantly large number of participants were satisfied with overall postoperative acute pain treatment (69%) and response of physician (81%) and nurses (62%) for their postoperative acute pain complaints. However, 15% participants physician (81%) and nurses (62%) for their postoperative their postoperative pain complaints [Figure 1].
Figure 1.
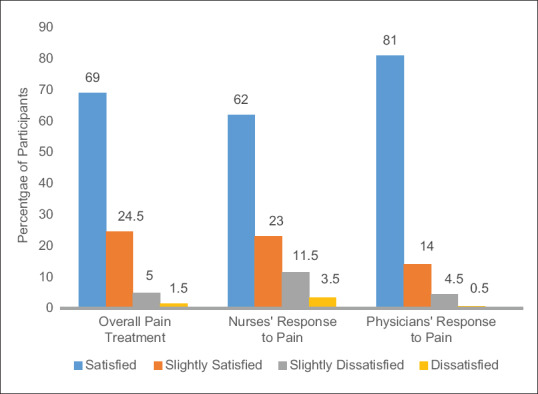
Patient's satisfaction with overall pain treatment, response of physician and nurses to pain
One-way ANOVA was used to determine the association of acute postoperative pain perception with length of hospital stay and type of analgesia. It was found that mean acute postoperative pain perception score was directly associated with longer postoperative stay of patients in hospitals (P = 0.001). Furthermore, mean pain score was high in participants treated with either opioid alone (5.4 ± 1.8) and in combination with NASIDs (5.3 ± 1.6) as compared to patients treated with NSAIDs (4.7 ± 1.4); which could be because of inadequate dose of opioids (P = 0.04) [Table 3].
Table 3.
Association of average pain during first 24 h postoperatively with selected clinical variable of participants n=200
| Clinical variables | Average pain perception during first 24 h postoperatively |
|
|---|---|---|
| Mean±SD | P | |
| Duration of hospitalization | ||
| <2 weeks | 4.79±1.45 | 0.00* |
| 2-4 weeks | 6.07±1.43 | |
| >4 weeks | 7.00±1.73 | |
| Types of analgesics | ||
| NSAIDs | 4.72±1.38 | 0.04* |
| Opioids + NSAIDs | 5.31±1.59 | |
| Opioids | 5.40±1.83 | |
| Opioids + NSAIDs + Muscle relaxant | 4.50±1.50 | |
*Significant (P<0.05)
DISCUSSION
Acute postoperative pain assessment must be done frequently, preferably every hour when complex analgesia is used.[9] American Society of Anesthesiologists recommends that postoperative pain assessment must be performed regularly to reduce adverse outcomes of postoperative pain.[10] However, in present study 12% patient reported that their pain was never assessed until they reported it and majority of them verbalized that it was assessed only once (17%) or twice (48.5%) during each shift. Inadequate assessment of postoperative pain is a serious challenge and barrier for effective pain management.[11]
In the present study, all the patients (100%) experienced postoperative pain during first 24-h of the surgery, where average mean pain during first 24-h postoperatively was 4.9 ± 1.5 and mean worst pain score of first 24-h after surgery was 7.6 ± 1.5. Furthermore, the incidence of moderate-to-severe level of average pain experienced during first 24-h after surgery was significantly high (82.5%). This signifies that acute postoperative pain was undertreated in present study, which may have serious adverse effects such as discomfort, delayed wound healing, increased risk of cardiovascular, pulmonary complications, decreased gastrointestinal activity, prolonged hospital stay, and poor patient satisfaction.[1,2]
In the present study, postoperative pain mainly treated by using NSAIDs alone (59%) or in combination with opioids (30%); while sole use of opioids was very low (5%). Opioids are more liberally used in the West may be because of easy accessibility and better training of health care professionals.[12] Opioids are found more effective in the management of acute pain but they are restrictively used in countries like India because of rigid regulations,[13] fear of addiction,[14] and poor training of healthcare professionals.[15]
Surprisingly, there was negligible use of non-pharmacological intervention for the pain management in the present study, where the majority of patients reported that neither nurses use any non-pharmacological interventions for the pain management (80.5%) nor any health care professional encouraged for the use of non-pharmacological pain relieving methods (81.0%). These results were consistent with another study, where only a few patients reported that nurses taken additional actions to manage their pain.[16] Non-pharmacological therapies alone are not efficacious for the treatment of acute postoperative pain but they may act as good adjunct.[17]
Present study findings demonstrated that postoperative pain has significant interference with ADLs, sleep and emotions of the patients, where mean interference score for ADLs was 5.6 ± 2.1 followed by sleep (3.6 ± 2.7) and emotions (3.6 ± 2.6). Further, a significant number of patients have moderate-to-several level of interference with ADLs (85.5%), emotions (54.5%) and sleep (51%) due to their acute postoperative pain. Subramanianet al.[18] also reported that the majority of participants (97%) with postoperative pain experienced difficulty in activities in bed and 78.4% verbalized feelings of depression. Interference in ADLs, emotions and sleep may have direct effect on the early postoperative mobilization, recover and wound healing.[19] The current study found that higher the acute postoperative pain score, longer the postoperative stay of patients in the hospital (>4 week of stay who had mean pain score 7.0 ± 1.7 vs. < 2 weeks who had mean pain score 4.79 ± 1.6; P = 0.001). Garimella and Cellini (2013)[20] concluded that effective management of postoperative pain in colorectal surgeries may reduce the duration of hospital stay. It was evident from our study findings that the mean score of acute pain was highest among patients treated with opioids (5.4 ± 1.8), followed by opioids in combination with NSIADs (5.3 ± 1.6); as compared to patients treated with only NSAIDs (4.7 ± 1.4) and with combination therapy (4.5 ± 1.5), which could be due to inadequate doses of opioids for the management of acute postoperative pain (P = 0.04), which may be due to the fear of side effect, addiction and poor pain management training for health care professionals.[15,21]
Surprisingly, despite the fact that the majority of patients experienced moderate to severe level of acute postoperative pain, significant number of them were satisfied with overall pain treatment (69%) and response of physician (81%) and nurses (62%) for their pain complaints. This may be due to the fact that patients expect pain as an inevitable phenomenon after surgery and nothing much can be done about it. Such attitude characterized by low expectations of postoperative pain relief encourage the persistence of poor standards for analgesia. Patients are satisfied even though they suffer from moderate-to-severe pain and had to wait for a relatively longer time for pain medication.[16] This issue could only be handled through patient education for adequate reporting the postoperative pain and active patient participation in pain management.
Patients' involvement in pain management in our study was assessed on 0 (not at all) to 10 (very much) scale and found that the mean score of their involvement was surprisingly very low i.e., 0.9 ± 1.7. Similar findings have been reported by McTier et al. (2013).[22] While, Schwenkglenks et al. (2014)[23] conducted an extensive multi-national study and concluded that patients actively involved in their pain treatment report better pain control and higher levels of satisfaction. Studies have also reported that constant monitoring of patients acts as a preventive strategy to minimize post-operative complication related to pain.[24,25]
CONCLUSION
The incidence of moderate-to-severe level of acute postoperative pain was alarmingly high and pain assessment was significantly inadequate. Acute postoperative pain has significant interference with ADLs, sleep and emotions. Patient participation in acute postoperative pain management was nearly non-existent and was seriously undertreated, which had significant effect on patient's duration of postoperative stay in hospital. Surprisingly, despite poor pain management, patient's satisfaction with pain management was quite high, which could be because patients expect that pain is inevitable after surgery. Therefore, it is recommended that tertiary care centres or such organizations must have acute pain services (APS) for the management of acute pain in surgical patients. The quality criteria for APS should be evidence based written pain management protocol which is feasible in the Indian scenario, adequate manpower deployment, training and motivation of health care professionals, patient education and participation in pain management and regular audit for effective implementation of APS.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest
Acknowledgements
The authors thank All India Institute of Medical Sciences, Rishikesh for providing library facility which was helpful in literature search.
REFERENCES
- 1.Ncbi.nlm.nih.gov. 2019. [cited 2019 Dec 30]. Available from: https://www.ncbi.nlm.nih.gov/pubmed/16357114 .
- 2.PMC E. Europe PMC [Internet] Europepmc.org. 2019. [cited 2019 Dec 30]. Available from: https://europepmc.org/abstract/MED/12271555 .
- 3.Bhakta H, Marco C. Pain management: Association with patient satisfaction among emergency department patients. J Emerg Med. 2014;46:456–64. doi: 10.1016/j.jemermed.2013.04.018. [DOI] [PubMed] [Google Scholar]
- 4.Brown C, Constance K, Bédard D, Purden M. Colorectal surgery patients' pain status, activities, satisfaction, and beliefs about pain and pain management. PainManag Nurs. 2013;14:184–92. doi: 10.1016/j.pmn.2010.12.002. [DOI] [PubMed] [Google Scholar]
- 5.Jain P, Bakshi S, Thota R. Acute pain services in India: A glimpse of the current scenario. 2019. [cited 2019 Dec 31]. Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4676250/ [DOI] [PMC free article] [PubMed]
- 6.Vijayan R. Managing Acute Pain in the Developing World-IASP [Internet] Iasp-pain.org. 2019. [cited 2019 Dec 30]. Available from: https://www.iasp-pain.org/PublicationsNews/NewsletterIssue.aspx?ItemNumber=2078 .
- 7.Gordon DB, Polomano RC, Pellino TA, Turk DC, McCracken LM, Sherwood G, et al. Revised American pain society patient outcome questionnaire (APS-POQ-R) for quality improvement of pain management in hospitalized adults: Preliminary psychometric evaluation. J Pain. 2019;11:1172–86. doi: 10.1016/j.jpain.2010.02.012. [DOI] [PubMed] [Google Scholar]
- 8.Sharma SK, Mudgal SK, Thakur K, Gaur R. How to calculate sample size for observational and experimental nursing research studies? Natl J Physiol Pharm Pharmacol. 2020;10:1–8. [Google Scholar]
- 9.Melbourne T. Clinical Guidelines (Nursing): Pain assessment and measurement [Internet] Rch.org.au. 2020. [cited 2020 Jan 04]. Available from: https://www.rch.org.au/rchcpg/hospital_clinical_guideline_index/Pain_Assessment_and_Measureme .
- 10.Apfelbaum J, Silverstein J, Chung F, Connis R, Fillmore R, Hunt S, et al. Practice Guidelines for Postanesthetic Care [Internet] 2020. [cited 2020 Jan 04]. Available from: https://anesthesiology.pubs.asahq.org/article.aspx?articleid=1918686 .
- 11.Herr K, Coyne P, McCaffery M, Manworren R, Merkel S. Pain assessment in the patient unable to self-report: Position statement with clinical practice recommendations. Pain Manag Nurs. 2011;12:230–50. doi: 10.1016/j.pmn.2011.10.002. [DOI] [PubMed] [Google Scholar]
- 12.Nawar EW, Niska RW, Xu J. [cited 2019 Aug01];National Hospital Ambulatory Medical Care Survey: 2005 emergency department summary. [Internet] 2016 389:1–34. Available from: https://www.ncbi.nlm.nih.gov/pubmed/17703794 . [PubMed] [Google Scholar]
- 13.Khatib SK, Kulkarni SS, Razvi SS. Acute pain services in India: A long and challenging ahead. Indian J Pain. 2016;30:83–9. [Google Scholar]
- 14.Rajagopal M, Joranson D. India: Opioid Availability—An Update [Internet] 2020. [cited 2020 Jan04]. Available from: https://www.ncbi.nlm.nih.gov/pubmed/17482057 . [DOI] [PubMed]
- 15.Vadivelu N, Mitra S, Hines RL. Acute pain in undergraduate medical education: An unfinished chapter!-PubMed-NCBI [Internet] Ncbi.nlm.nih.gov. 2020. [cited 2020 Jan04]. Available from: https://www.ncbi.nlm.nih.gov/pubmed/22712557 .
- 16.Tawil S, Iskandar K, Salameh P. Pain management in hospitals: Patients' satisfaction and related barriers. Pharm Pract. 2018;16:1268. doi: 10.18549/PharmPract.2018.03.1268. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Van der Wal-Huisman H, Dons KSK, Smilde R, Heineman E, van Leeuwen BL. The effect of music on postoperative recovery in older patients: A systematic review. J Geriatr Oncol. 2018;9:550–9. doi: 10.1016/j.jgo.2018.03.010. [DOI] [PubMed] [Google Scholar]
- 18.Subramanian P, Ramasamy S, Ng K, Chinna K, Rosli R. Pain experience and satisfaction with postoperative pain control among surgical patients. Int J Nurs Pract. 2014;22:232–8. doi: 10.1111/ijn.12363. [DOI] [PubMed] [Google Scholar]
- 19.Mclain JM, Alami WH, Glovak ZT, Cooley CR, Burke SJ, Collier JJ, et al. Sleep fragmentation delays wound healing in a mouse model of type 2 diabetes. Sleep. 2018 doi: 10.1093/sleep/zsy156. doi: 10.1093/sleep/zsy156. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Garimella V, Cellini C. Postoperative pain control. Clin Colon Rectal Surg. 2013;26:191–6. doi: 10.1055/s-0033-1351138. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.De Lima L, Sweeney C, Palmer J, Bruera E. Potent Analgesics Are More Expensive for Patients in Developing Countries [Internet] 2020. [cited 2020Jan 04]. Available from: https://www.ncbi.nlm.nih.gov/pubmed/15148009 . [PubMed]
- 22.McTier L, Botti M, Duke M. Patient Participation in Quality Pain Management During an Acute Care Admission [Internet] 2020. [cited 2020 Jan05]. Available from: https://www.ncbi.nlm.nih.gov/pubmed/23727655 . [DOI] [PubMed]
- 23.Schwenkglenks M, Gerbershagen H, Taylor R, Pogatzki-Zahn E, Komann M, Rothaug J, et al. Correlates of satisfaction with pain treatment in the acute postoperative period: Results from the international PAIN OUT registry [Internet] 2020. [cited 2020 Jan05]. Available from: https://www.ncbi.nlm.nih.gov/pubmed/24785269 . [DOI] [PubMed]
- 24.Jain PN. Acute pain service: Round the clock vigilance. Indian J Anaesth. 2018;62:491–2. doi: 10.4103/ija.IJA_471_18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Mehrotra S. Postoperative anaesthetic concerns in children: Postoperative pain, emergence delirium and postoperative nausea and vomiting. Indian J Anaesth. 2019;63:763–70. doi: 10.4103/ija.IJA_391_19. [DOI] [PMC free article] [PubMed] [Google Scholar]


