Abstract
Background and Aim:
Desflurane and sevoflurane are the most common volatile anesthetics used during laparoscopic and hepatic surgery. The objective of the study was to evaluate the effect of desflurane and sevoflurane in patients with elevated preoperative liver functions undergoing laparoscopic cholecystectomy.
Methods:
The study was a randomized study and included 162 patients classified randomly into two groups: Desflurane group: The patients received desflurane (end-tidal concentration 4%–6%) as an inhalational agent during the whole procedure. Sevoflurane group: The patients received sevoflurane (end-tidal concentration 2%–4%) as an inhalational agent during the whole procedure. The investigations included serum level of aspartate aminotransferase (AST), alanine aminotransferase (ALT), alkaline phosphatase (ALP), gamma-glutamyltransferase (GGT), and total bilirubin. The values were serially collected at the following timepoints; T0:at the preoperative period, T1:directly after surgery, T2:1st postoperative day, T3:2nd postoperative day, T4:3rd postoperative day, T5:5th postoperative day, T6:7th postoperative day, and T7:10th postoperative day. The statistics were described in terms of mean ± standard deviation, frequencies, and percentages.
Results:
The preoperative liver enzymes and total bilirubin were higher than the normal range in patients of the two groups. Postoperatively, there was a decrease in the AST and ALT with desflurane more than sevoflurane from T1 to T6(P < 0.05). The ALP, GGT, and bilirubin decreased in patients of the two groups, but the comparison was insignificant (P > 0.05).
Conclusion:
The desflurane is a safe inhalational volatile for maintenance of anesthesia in patients with impaired liver function undergoing laparoscopic cholecystectomy. It was associated with a decrease in the liver enzymes more than the sevoflurane.
Key words: Desflurane, hepatic protection, laparoscopic cholecystectomy, liver enzymes, sevoflurane
INTRODUCTION
Laparoscopic cholecystectomy is considered the gold standard method to treat uncomplicated cholelithiasis. Many studies showed changes in the postoperative liver functions after laparoscopic procedures.[1,2,3] These changes may be related to hepatocellular damage secondary to the combination of carboxy pneumoperitoneum, liver manipulation, use of diathermy, general anesthesia, and hepatic artery injury.[4,5,6]
Desflurane and sevoflurane are the most common volatile anesthetics used during laparoscopic and hepatic surgery,[7,8,9,10] and we hypothesized that desflurane and sevoflurane provide equal hepatic protection in patients with acute cholecystitis and impaired preoperative liver functions undergoing laparoscopic cholecystectomy.
This study aimed to evaluate the effect of desflurane and sevoflurane in patients with acute cholecystitis and impaired preoperative liver functions undergoing laparoscopic cholecystectomy.
METHODS
After obtaining informed consent and approval of local ethics and research committee in the hospital (312016, 20/01/2016), a prospective randomized study included 162 patients (through 2016–2019) with ASA (American Society of Anesthesiologists) physical status I and II, acute cholecystitis, and elevated preoperative liver functions [higher than two times of the normal range: AST (5-34 U/L), ALT (7-55U/L), ALP (40-150U/L) GGT (12-64U/L), total bilirubin (3.4–20.5μmol/L), and direct bilirubin (<8.5μmol/L)].
Exclusion criteria of the study included patients with morbid obesity (body mass index > 35kg/m2), obstructive jaundice, fulminant hepatitis, significant severe cardiovascular, renal, respiratory, and neurological and psychiatric diseases. Preoperative magnetic resonance cholangiopancreatography (MRCP) was done for all patients to exclude obstructive jaundice and to provide detailed images of the hepatobiliary and pancreatic systems, including the liver, gallbladder, bile ducts, pancreas, and pancreatic duct. All the cases were anesthetized by the same anesthetic team and the same surgeon.
The patients were randomly allocated (the concealment of allocation was done by using random numbers generated through excel) into two equal groups (n = 81 each). Desflurane group: The patients received desflurane (end-tidal concentration 4%–6%) as an inhalational agent during the whole procedure. Sevoflurane group: The patients received sevoflurane (end-tidal concentration 2%–4%) as an inhalational agent during the whole procedure.
During the procedure, the dial concentration of desflurane and sevoflurane vaporizers was adjusted every 5 min to maintain the concentration around one MAC (minimum alveolar concentration) and to control the changes in the heart rate and blood pressure. The MAC of desflurane and sevoflurane were measured using Dräger infinity C700 (Dräger, Lübeck Germany). The age was not considered during adjustment of the MAC.
The carboxy pneumoperitoneum during laparoscopic cholecystectomy was maintained at a pressure of 10–15 mmHg.
For all patients, a peripheral venous line G18wasinserted and intravenous administration of 500 mL of crystalloids was administered before surgery. Premedication of two mg of midazolam was given intravenously 30 min before induction. After attaching the monitors (ECG, pulse oximeter, noninvasive arterial blood pressure), the induction of anesthesia was done for all patients by pre-oxygenation, intravenous propofol (1–2mg/kg) followed by fentanyl (1-2μg/kg) and atracurium 0.5mg/kg as a bolus dose over 30 s. After tracheal intubation, anesthesia was maintained with oxygen: air (concentration 50:50%, flow 2L: 2L constant with all patients) and desflurane or sevoflurane according to the study medication protocol. An additional dose of intravenous atracurium (0.08–0.1mg/kg) was given and guided by the peripheral nerve stimulator to provide a train-of-four count zero. The ventilation was adjusted to maintain the end-tidal PaCO2 within 30–35 mmHg (CO2 absorber was the same type for all patients and it was CLIC absorber 800+ Drägerwerk AG and Co. Lübeck Germany). Volatile anesthetic concentration adjusted to maintain the mean arterial blood pressure and heart rate within ± 20% of the preinduction baseline values. Intraoperative tachycardia (heart rate >100 bpm), and systemic hypertension (systolic arterial blood pressure >20% above baseline) was managed by increasing the concentration of desflurane or sevoflurane by increments of 1% and bolus doses of fentanyl (0.5–1μg/kg). Intraoperative hypotension (systolic arterial blood pressure < 20% below baseline) was managed by bolus doses of ephedrine 5–10mg and fluid administrations. Bradycardia (heart rate < 60 bpm) was managed by a bolus dose of atropine (0.02mg/kg). At the end of the surgery, the volatile agent was discontinued, and controlled ventilation with 100% oxygen was maintained until end-tidal volatile anesthetic concentration was less than 0.1%. Intravenous lidocaine 1mg/kg was given for all patients 2 min before removal of the endotracheal tube to provide smooth extubation. The residual neuromuscular blockade was reversed with a combination of neostigmine 0.05mg/kg mg and atropine 0.02mg/kg intravenously. Postoperative nausea and vomiting were managed by intravenous administration of ondansetron (0.1–0.15mg/kg).
At the end of anesthesia and after extubation, the patients were shifted to the post-anesthesia care unit and later to the ward. After discharge from the hospital, the patients were informed to repeat the liver function test as the scheduled plan in the study until postoperative day 10.
The variables used during the study included serum levels of aspartate aminotransferase (AST), alanine aminotransferase (ALT), alkaline phosphatase (ALP), gamma-glutamyltransferase (GGT), and total bilirubin. The blood samples were withdrawn in the main hospital laboratory either the preoperative or postoperative investigations which were done by using the resources of the hospital and not funded from any company. The values were serially collected at the following timepoints; T0:at the preoperative period, T1:directly after surgery, T2:1st postoperative day, T3:2nd postoperative day, T4:3rd postoperative day, T5:5th postoperative day, T6:7th postoperative day, T7:10th postoperative day. Also, the monitors included the heart rate, mean arterial blood pressure, arterial oxygen saturation, end-tidal PaCO2, end-tidal concentration of desflurane and sevoflurane, emergence and extubation time, the total dose of fentanyl, atracurium, ephedrine and atropine, duration of surgery and anesthesia, intraoperative fluids, blood loss, postoperative hematocrit values, and the renal functions tests.
The primary outcome was the hepatic protective effect as assessed by the decreased postoperative level of liver enzymes. Secondary outcomes were the safety of the study medications, as assessed by the incidence of adverse events such as arrhythmia, hypotension, hypertension, emergence cough, emergence agitation, postoperative nausea and vomiting.
Power analysis was performed using the Chi-square test for independent samples on the frequency of patients associated with decreased postoperative liver enzymes because it was the main outcome variable in this study. A pilot study was done before starting this study because there is no available data in the literature for the comparison of the hepatic protective effect in patients with impaired liver functions undergoing laparoscopic cholecystectomy. The results of the pilot study showed that the postoperative liver enzymes level decreased in 40% with desflurane and 20% with sevoflurane. Taking power 0.8, α error 0.05, β 0.2, and power 0.8, a minimum sample size of 81 patients was calculated for each group.
Data were statistically described in terms of mean ± standard deviation, frequencies, and percentages when appropriate. A comparison of numerical variables between the study groups was done using the Student's t test for independent samples. Repeated measure analysis of variance (ANOVA) was used to compare the liver function tests at different follow-up intervals. For comparing categorical data, Chi-square test was performed. An exact test was used instead when the expected frequency is less than 5. A value of P < 0.05 was considered statistically significant. All statistical calculations were done using Statistical Package for the Social Sciences (SPSS) software program, version 15.0 for Microsoft Windows (SPSS, Chicago, Illinois).
RESULTS
Figure 1 shows the CONSORT diagram for the flow of participants through each stage of this study. All patients in each group have been completed the study and included in the analysis of this study.
Figure 1.
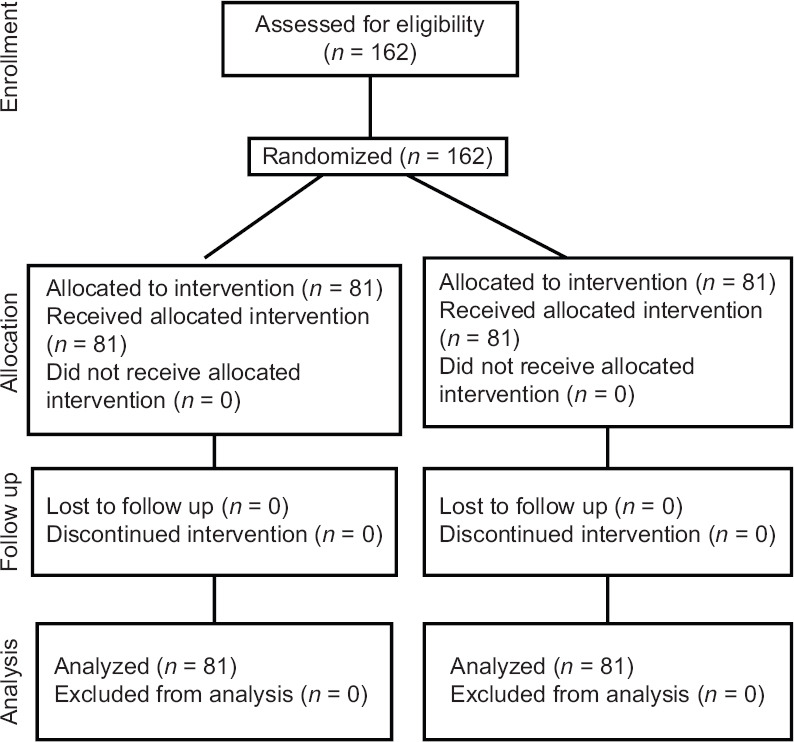
CONSORT diagram for the flow of participants through each stage of this study
Table 1 shows no significant difference regarding the demographic data, comorbidities, preoperative medications, ASA physical status score, and the hematocrit values (P > 0.05).
Table 1.
Preoperative data of patients
| Variable | Desflurane group (n=81) | Sevoflurane group (n=81) | P |
|---|---|---|---|
| Age (year) | 44.15±15.24 | 43.66±13.90 | 0.831 |
| Weight (kg) | 88.30±18.65 | 86.47±19.10 | 0.538 |
| Gender | |||
| Male:female | 38:43 | 36:45 | 0.8747 |
| Diabetes mellitus | 31 (38.27%) | 26 (32.09%) | 0.510 |
| Hypertension | 24 (29.62%) | 28 (34.56%) | 0.613 |
| ASA grade | |||
| Grade I:II | 55: 26 | 57: 24 | 0.865 |
| Anti-diabetic medications | |||
| Oral hypoglycemic drugs | 25 | 19 | 0.377 |
| Insulin | 6 | 7 | 0.953 |
| Antihypertensive drugs | |||
| Calcium channel blockers | 15 | 19 | 0.563 |
| blockers | 5 | 3 | 0.7196 |
| ACEI | 4 | 6 | 0.746 |
| Hematocrit (%) | 39.40±2.57 | 38.90±2.49 | 0.210 |
ASA – American Society of Anesthesiologists Physical Status Score, ACEI – Angiotensin-converting-enzyme inhibitor. Data are presented as mean±SD, number, %
Table 2 shows the changes in the liver function tests of patients. The preoperative levels of liver enzymes and bilirubin were higher than the normal range in the patients of the two groups, but the difference was insignificant between the two groups (P > 0.05). Postoperatively, there were changes in the liver enzymes and bilirubin in the two groups. There was a decrease in the AST and ALT from day 1 to day 7 in patients of the two groups, but it decreased significantly in desflurane group more than sevoflurane group (P < 0.05) and the levels become within the normal range at day 10 with insignificant difference between the two groups (P > 0.05). There was a decrease in the ALP and GGT from day 1 to day 3 in patients of the two groups, and the decrease was more in the desflurane group than the sevoflurane group, but the difference between the two groups was insignificant (P > 0.05). The levels become within the normal range on day 4, and the difference between the two groups was insignificant (P > 0.05). There was a decrease in the total bilirubin level from day 1 to day 7 in patients of the two groups, and the decrease was more in the desflurane group than the sevoflurane group, but the difference between the two groups was insignificant (P > 0.05). The levels become within the normal range on day 10.
Table 2.
Serum levels of aspartate aminotransferase (AST), alanine aminotransferase (ALT), alkaline phosphatase (ALP), gamma-glutamyltransferase (GGT), and total bilirubin
| Variable | Desflurane group (n=81) | Sevoflurane group (n=81) | P |
|---|---|---|---|
| Aspartate aminotransferase (U/L) | |||
| T0 | 257.43±89.14 | 248.12±85.37 | 0.498 |
| T1 | 164.15±30.70 | 201.92±41.37 | 0.001* |
| T2 | 103.54±19.40 | 159.11±29.80 | 0.001* |
| T3 | 72.34±10.25 | 111.56±17.59 | 0.001* |
| T4 | 55.20±8.04 | 79.40±11.38 | 0.001* |
| T5 | 32.70±7.25 | 45.20±9.34 | 0.001* |
| T6 | 25.70±5.40 | 29.38±7.50 | 0.001* |
| T7 | 23.90±4.51 | 25.11±5.50 | 0.127 |
| Alanine aminotransferase (U/L) | |||
| T0 | 235.22±66.45 | 227.63±58.70 | 0.442 |
| T1 | 180.35±44.80 | 198.56±56.68 | 0.024* |
| T2 | 157.43±33.72 | 170.18±42.08 | 0.034* |
| T3 | 129.10±22.60 | 140.32±37.70 | 0.020* |
| T4 | 98.99±10.43 | 107.39±21.30 | 0.002* |
| T5 | 67.15±9.90 | 80.25±13.40 | 0.006* |
| T6 | 44.52±7.18 | 52.76±10.03 | 0.001* |
| T7 | 26.26±6.30 | 28.10±8.70 | 0.125 |
| Alkaline phosphatase (U/L) | |||
| T0 | 182.65±16.73 | 179.15±15.36 | 0.167 |
| T1 | 172.90±10.43 | 175.27±12.50 | 0.192 |
| T2 | 162.80±8.50 | 164.45±9.30 | 0.082 |
| T3 | 152.40±7.10 | 153.28±7.34 | 0.439 |
| T4 | 143.50±6.28 | 145.10±5.05 | 0.075 |
| T5 | 134.95±4.85 | 136.40±5.90 | 0.089 |
| T6 | 124.70±4.14 | 125.86±±4.60 | 0.093 |
| T7 | 121.80±4.90 | 122.63±5.60 | 0.317 |
| Gamma-glutamyltransferase (U/L) | |||
| T0 | 82.54±7.13 | 81.59±6.80 | 0.386 |
| T1 | 75.30±6.50 | 75.40±6.13 | 0.919 |
| T2 | 68.90±5.20 | 70.12±5.70 | 0.156 |
| T3 | 63.96±4.90 | 65.19±5.10 | 0.119 |
| T4 | 58.80±4.47 | 60.13±5.23 | 0.083 |
| T5 | 52.40±4.52 | 53.25±4.75 | 0.245 |
| T6 | 50.21±5.47 | 51.29±5.63 | 0.217 |
| T7 | 47.80±4.60 | 48.11±5.52 | 0.698 |
| Bilirubin (µmol/L) | |||
| T0 | 42.18±6.40 | 43.46±7.30 | 0.237 |
| T1 | 38.24±6.38 | 40.04±6.55 | 0.078 |
| T2 | 35.77±5.90 | 37.20±6.10 | 0.131 |
| T3 | 31.20±7.50 | 33.04±6.36 | 0.094 |
| T4 | 28.80±7.41 | 30.14±7.11 | 0.155 |
| T5 | 23.96±6.30 | 26.01±7.92 | 0.069 |
| T6 | 21.60±6.19 | 23.20±7.16 | 0.130 |
| T7 | 16.84±5.33 | 18.53±6.40 | 0.165 |
*P<0.05 significant comparison between the two groups. T0 – at the preoperative period, T1 – Directly after surgery, T2 – 1st postoperative day, T3 – 2nd postoperative day, T4 – 3rd postoperative day, T5 – 5th postoperative day, T6 – 7th postoperative day, T7 – 10th postoperative day
There were minimal and insignificant changes in the perioperative heart rate and mean arterial blood pressure and the difference between the two groups was insignificant (P > 0.05) [Table 3].
Table 3.
Heart rate and mean arterial blood pressure
| Variable | Desflurane group (n=81) | Sevoflurane group (n=81) | P |
|---|---|---|---|
| Heart rate (bpm) | |||
| T0 | 79.53±12.15 | 77.34±10.28 | 0.217 |
| T1 | 77.93±11.11 | 76.65±10.31 | 0.448 |
| T2 | 78.63±9.82 | 76.46±9.35 | 0.151 |
| T3 | 79.10±10.38 | 78.55±11.05 | 0.744 |
| T4 | 76.38±11.86 | 75.32±9.53 | 0.531 |
| T5 | 78.02±8.80 | 76.89±10.35 | 0.455 |
| T6 | 77.27±9.18 | 79.46±10.65 | 0.162 |
| T7 | 76.42±10.33 | 77.74±12.09 | 0.456 |
| Mean arterial blood pressure (mmHg) | |||
| T0 | 103.17±15.87 | 104.75±16.35 | 0.533 |
| T1 | 105.06±13.79 | 106.15±14.63 | 0.6263 |
| T2 | 104.61±14.84 | 107.04±15.33 | 0.306 |
| T3 | 107.36±13.44 | 105.61±14.09 | 0.419 |
| T4 | 103.80±12.75 | 106.00±13.23 | 0.282 |
| T5 | 105.58±11.66 | 104.11±10.99 | 0.410 |
| T6 | 106.00±12.54 | 105.20±11.43 | 0.671 |
| T7 | 104.65±10.37 | 106.35±12.73 | 0.352 |
T0 – At the preoperative period, T1 – Directly after surgery, T2 – 1st postoperative day, T3 – 2nd postoperative day, T4 – 3rd postoperative day, T5 – 5thpostoperative day, T6 – 7th postoperative day, T7 – 10th postoperative day. Data are presented as mean±SD
Table 4 shows the intraoperative data and the outcomes of patients of the two groups. There were no significant differences regarding the duration of surgery and anesthesia, intraoperative fluids and blood loss, temperature, end-tidal PaCO2, the total dose of fentanyl and atracurium, postoperative hematocrit values and the renal functions tests (P > 0.05). The comparison of the end-tidal concentration of desflurane and sevoflurane was significant (P = 0.001). The required dose of ephedrine and atropine was lower with desflurane than the sevoflurane, but the difference was insignificant (P = 0.531 and 0.317, respectively). The incidence of hypotension and bradycardia was lower with desflurane than the sevoflurane, but the difference was insignificant (P = 0.054 and 0.077, respectively). The incidence of hypertension and tachycardia was higher in desflurane group than the sevoflurane group, but the difference was insignificant (P = 0.191 and 0.368, respectively). The emergence time (time from end of anesthesia to the time of opening the eyes spontaneously or the response to verbal commands) was shorter in the desflurane group than the sevoflurane group (P = 0.019). The extubation time (duration from the end of anesthesia until the patients become fully awake and removal of the endotracheal tube) was shorter with desflurane than the sevoflurane (P = 0.023). The incidence of emergence cough (coughing during emergence) was insignificant between the two groups (P = 0.587). The incidence of nausea and vomiting was significantly lower with desflurane than the sevoflurane (P = 0.015). The length of hospital stay was shorter with desflurane than the sevoflurane (P = 0.011). There was no incidence of emergence agitation, morbidity, or mortality in patients of the two groups.
Table 4.
Intraoperative data and outcome of patients
| Variable | Desflurane group (n=81) | Sevoflurane group (n=81) | P |
|---|---|---|---|
| Duration of procedure (min) | 49.27±5.75 | 47.94±4.80 | 0.112 |
| Duration of anesthesia (min) | 60.30±13.40 | 66.59±17.84 | 0.012* |
| Temperature (°C) | 36.30±0.50 | 36.20±0.48 | 0.196 |
| End-tidal CO2 (mmHg) | 35.86±2.28 | 36.17±2.40 | 0.400 |
| Total fentanyl dose (µg) | 136.25±27.80 | 130.90±23.63 | 0.188 |
| Total atracurium dose (mg) | 57.35±12.80 | 54.79±10.75 | 0.170 |
| End-tidal concentration (%) | 5.32±0.31 | 2.42±0.24 | 0.001* |
| Ephedrine | |||
| Number of patients | 9 (11.11%) | 17 (20.98%) | 0.054 |
| Dose (mg) | 6.85±2.57 | 7.15±3.45 | 0.531 |
| Atropine | |||
| Number of patients | 5 (6.7%) | 13 (16.04%) | 0.077 |
| Dose (mg) | 0.58±0.18 | 0.61±0.20 | 0.317 |
| Hypotension (SAP ≤20% below baseline) | 9 (11.11%) | 17 (20.98%) | 0.054 |
| Hypertension (SAP ≥20% above baseline) | 16 (19.95%) | 9 (11.11%) | 0.191 |
| Bradycardia (HR <60 bpm) | 5 (6.7%) | 13 (16.04%) | 0.077 |
| Tachycardia (HR >100 bpm) | 14 (17.28%) | 9 (11.11%) | 0.368 |
| Emergence cough | 9 (11.11%) | 6 (7.40%) | 0.587 |
| Emergence time (min) | 10.53±4.62 | 12.48±5.84 | 0.019* |
| Extubation time (min) | 7.87±3.37 | 9.18±3.90 | 0.023* |
| Emergence agitation | - | - | |
| Incidence of nausea and vomiting | 23 (28.39%) | 39 (48.14%) | 0.015* |
| Intraoperative fluids [only crystalloids] (mL) | 1873.30±314.80 | 1840.90±324.10 | 0.519 |
| Intraoperative blood loss (mL) | 73.15±10.54 | 70.75±9.71 | 0.133 |
| Hematocrit (%) | 35.54±2.15 | 36.00±2.23 | 0.183 |
| Renal functions tests | |||
| Serum creatinine (mg/dL) | 1.12±0.3 | 1.17±0.21 | 0.220 |
| Blood urea nitrogen (mg/dL) | 7.98±2.43 | 8.10±2.31 | 0.747 |
| Hospital length of stay (days) | 4.60±1.15 | 5.05±±1.10 | 0.011* |
| Postoperative morbidity or mortality | - | - |
*P<0.05 significant comparison between the two groups. SAP – Systolic arterial blood pressure, HR – Heart rate. Data are presented as mean±SD, number, %
DISCUSSION
This study showed that the desflurane has a hepatic protective effect in patients with elevated preoperative liver functions and undergoing laparoscopic cholecystectomy as assessed by the changes in levels of the liver enzymes, especially the AST and ALT that decreased significantly through the first three postoperative days, whereas in patients of sevoflurane group, there were minimal changes in liver enzymes that also increased significantly in some patients. This means that the sevoflurane has no hepatic protective effect in patients undergoing laparoscopic cholecystectomy. The findings in this study show that desflurane minimized the damage of the liver during laparoscopic cholecystectomy and also provided hepatic protection for the patients with preoperative elevated liver functions better than sevoflurane.
Desflurane showed better hepatic protection than sevoflurane and this may be supported by many factors: (1) the ability of desflurane to preserve the hepatic blood flow and cardiac output better than the sevoflurane[8,11]; (2) the desflurane has a lower degree of metabolism (0.02%) than sevoflurane (1%–5%), this means the sevoflurane metabolism is approximately 100 times greater than desflurane metabolism in humans[12]; (3) sevoflurane metabolism produces an extra metabolite, compound A through a chemical reaction with CO2 absorbents[13] and several studies have suggested that compound A has a hepatotoxic effect as shown by a transient increase in postoperative liver function tests[14,15]; (4) the desflurane is stable and resists degradation by standard carbon dioxide absorbents more than sevoflurane[16] and undergo minimal metabolism by the liver[17]; (5) many studies showed that hemodynamic stability during anesthesia was significantly better with desflurane than sevoflurane[18,19,20]; (6) the desflurane is rapidly excreted from the body.[8] These unique properties of desflurane lead to a better postoperative hepatic function.
Yontem et al.[17] reported that desflurane is less metabolized than sevoflurane, and desflurane is preferred for the patients with liver disorders and the same results were shown by other studies.[8,21,22] Chudasama et al.[18] concluded that desflurane provided better hemodynamic stability during the postoperative period compared to sevoflurane. Ko et al.[23] found that postoperative hepatic function tests were better with desflurane than the sevoflurane in living donors undergoing right hepatectomy at an equivalent dose of one MAC and there was a higher degree of liver damage after anesthesia in patients with sevoflurane than with desflurane. Abou Hussein et al.[7] reported that the hemodynamics was better with desflurane than sevoflurane in cirrhotic patients undergoing major liver resections. Kumari et al.[20] showed that desflurane is safe for the maintenance of hemodynamics in normotensive and hypertensive patients undergoing laparoscopic cholecystectomy.
Lin et al.[24] reported that sevoflurane was associated with a severe degree of liver damage than desflurane in prolonged surgery as shown by the elevated postoperative AST and ALT with sevoflurane than desflurane.
Contrary to the findings of this study, some studies showed that sevoflurane provided better hepatic protection than desflurane, as the sevoflurane increases significantly the blood levels of antioxidants (superoxide dismutase, catalase, glutathione peroxidase, and glutathione reductase) than desflurane,[25] in addition to the increased levels of free oxygen radicals with desflurane more than sevoflurane, especially the release of free oxygen radicals increases during laparoscopic surgery,[26,27] and other studies reported that sevoflurane is superior to other inhalational agents in patients with liver disease.[28,29] Some studies showed no difference between desflurane and sevoflurane regarding their effect on live enzymes.[30,31,32]
There are some limitations to this study, such as the study was not a blinded, small number of patients and there were no studies assessed the hepatic protective effect of desflurane and sevoflurane in patients with impaired liver functions undergoing laparoscopic cholecystectomy to compare the results of this study.
CONCLUSION
The desflurane is a safe inhalational volatile for maintenance of anesthesia in patients with impaired liver function undergoing laparoscopic cholecystectomy. It was associated with a decrease in the liver enzymes more than the sevoflurane.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Acknowledgements
The authors appreciate the help and support of the staff-nurses in the operative rooms and postoperative surgical wards to achieve this work.
REFERENCES
- 1.Cuschieri A. Laparoscopic cholecystectomy. J R Coll Surg Edinb. 1999;44:187–92. [PubMed] [Google Scholar]
- 2.Al-Luwalzi KR, Hamad SO. Changes of liver enzymes and serum bilirubin after laparoscopic cholecystectomy. Ann Coll Med Mosul. 2013;39:113–7. [Google Scholar]
- 3.Guven HE, Oral S. Liver enzyme alterations after laparoscopic cholecystectomy. J Gastrointestin Liver Dis. 2007;16:391–4. [PubMed] [Google Scholar]
- 4.Tan M, Xu FF, Peng JS, Li DM, Chen LH, Lv BJ, et al. Changes in the level of serum liver enzymes after laparoscopic surgery. World J Gstroenterol. 2003;9:364–7. doi: 10.3748/wjg.v9.i2.364. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Sakorafas G, Anagnostopoulos G, Stafyla V, Koletis T, Kotsifopoulos N, Tsiakos S, et al. Elevation of serum liver enzymes after laparoscopic cholecystectomy. N Z Med J. 2005;118:U1317. [PubMed] [Google Scholar]
- 6.Hasukic S. Postoperative changes in liver function tests: Randomized comparison of low and high-pressure laparoscopic cholecystectomy. Surg Endosc. 2005;19:1451–5. doi: 10.1007/s00464-005-0061-5. [DOI] [PubMed] [Google Scholar]
- 7.Abou Hussein M, Mahmoud F, Beltagy R, Hasanin A, Yassen K, Attar A. Desflurane in comparison to sevoflurane in cirrhotic patients undergoing major liver resection. Middle East J Anaesthesiol. 2015;23:213–23. [PubMed] [Google Scholar]
- 8.Vaja R, McNicol L, Sisley I. Anaesthesia for patients with liver disease. Contin Educ Anaesth Crit Care Pain. 2010;10:15–9. [Google Scholar]
- 9.Ozcan ATD, Doger C, Ozturk L, Yungul A, Kurtsahin M, Neselioglu S, et al. Comparison of the effects of sevoflurane and desflurane on thiol-disulfide homeostasis in patients undergoing laparoscopic cholecystectomy. Eurasian J Med. 2019;51:70–4. doi: 10.5152/eurasianjmed.2019.18299. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Fanelli G, Berti M, Casati A. Fast-track anaesthesia for laparoscopic cholecystectomy: A prospective, randomized, multicentre, blind comparison of desflurane-remifentanil or sevoflurane-remifentanil. Eur J Anaesthesiol. 2006;23:861–8. doi: 10.1017/S0265021506000718. [DOI] [PubMed] [Google Scholar]
- 11.Sivanna U, Joshi S, Babu B, Jagadeesh AM. A comparative study of pharmacological myocardial protection between sevoflurane and desflurane at anaesthestic doses in patients undergoing off pump coronary artery bypass grafting surgery. Indian J Anaesth. 2015;59:282–6. doi: 10.4103/0019-5049.156867. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Reichle FM, Conzen PF. Halogenated inhalational anaesthetics. Best Pract Res Clin Anesthesiol. 2003;17:29–46. doi: 10.1053/bean.2002.0265. [DOI] [PubMed] [Google Scholar]
- 13.Keller KA, Callan C, Prokocimer P, Delgado-Herrera L, Friedman MB, Hoffman GM, et al. Inhalation toxicity study of a haloalkene degradant of sevoflurane, compound A (PIFE), in Sprague-Dawley rats. Anesthesiology. 1995;83:1220–32. doi: 10.1097/00000542-199512000-00013. [DOI] [PubMed] [Google Scholar]
- 14.Obata R, Bito H, Ohmura M, Moriwaki G, Ikeuchi Y, Katoh T, et al. The effects of prolonged low-flow sevoflurane anesthesia on renal and hepatic function. Anesth Analg. 2000;91:1262–8. doi: 10.1097/00000539-200011000-00039. [DOI] [PubMed] [Google Scholar]
- 15.Eger EI, Koblin DD, Bowland T, Ionescu P, Laster MJ, Fang Z, et al. Nephrotoxicity of sevoflurane versus desflurane anesthesia in volunteers. Anesth Analg. 1997;84:160–8. doi: 10.1097/00000539-199701000-00029. [DOI] [PubMed] [Google Scholar]
- 16.Eger EI., 3rd Stability of I-653 in soda lime. Anesth Analg. 1987;66:983–5. [PubMed] [Google Scholar]
- 17.Yontem M, Akkaya A, Kaleli S, Erci F, Kocak FE. Effects of sevoflurane and desflurane on some biochemical parameters. Asian J Biomed Pharm Sci. 2015;5:1–5. [Google Scholar]
- 18.Chudasama PA, Mehta MV. Comparison of haemodynamic parameters and recovery characteristics between sevoflurane and desflurane in patients undergoing day-care surgical procedure. Adv Hum Biol. 2018;8:140–4. [Google Scholar]
- 19.Shan J, Sun L, Wang D, Li X. Comparison of the neuroprotective effects and recovery profiles of isoflurane, sevoflurane and desflurane as neurosurgical pre-conditioning on ischemia/reperfusion cerebral injury. Int J Clin Exp Pathol. 2015;8:2001–9. [PMC free article] [PubMed] [Google Scholar]
- 20.Kumari K, Samra T, Saini V, Sethi S, Banerjee N, Sharma S. Comparison of hemodynamic response to inhalational bolus with desflurane in normotensive and hypertensive patients undergoing laparoscopic cholecystectomy. Turk J Anesthesiol Reanim. 2019;47:165–72. doi: 10.5152/TJAR.2018.93457. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Suttner SW, Schmidt CC, Boldt J, Hüttner I, Kumle B, Piper SN. Low-flow desflurane and sevoflurane anesthesia minimally affect hepatic integrity and function in elderly patients. Anesth Analg. 2000;91:206–12. doi: 10.1097/00000539-200007000-00039. [DOI] [PubMed] [Google Scholar]
- 22.Abbas N, Makker J, Abbas H, Balar B. Perioperative care of patients with liver cirrhosis: A review. Health Serv Insights. 2017;10:1–12. doi: 10.1177/1178632917691270. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Ko JS, Gwak MS, Choi SJ, Sethi S, Banerjee N, Sharma S. The effects of desflurane and sevoflurane on hepatic and renal functions after right hepatectomy in living donors. Transpl Int. 2010;23:736–44. doi: 10.1111/j.1432-2277.2009.01050.x. [DOI] [PubMed] [Google Scholar]
- 24.Lin H, Fan SZ, Chen HM, JJ, Cheng SJ, Chang HH, et al. Changes in biomarkers of hepatic and renal function after prolonged general anesthesia for oral cancer surgery: A cohort comparison between desflurane and sevoflurane. J Dent Sci. 2013;8:385–91. [Google Scholar]
- 25.Luo C, Yuan D, Zhao W, Chen H, Luo G, Su G, et al. Sevoflurane ameliorates intestinal ischemia-reperfusion-induced lung injury by inhibiting the synergistic action between mast cell activation and oxidative stress. Mol Med Rep. 2015;12:1082–90. doi: 10.3892/mmr.2015.3527. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Sivaci R, Kahraman A, Serteser M, Sahin DA, Dilek ON. Cytotoxic effects of volatile anesthetics with free radicals undergoing laparoscopic surgery. Clin Biochem. 2006;39:293–8. doi: 10.1016/j.clinbiochem.2006.01.001. [DOI] [PubMed] [Google Scholar]
- 27.Erbas M, Demiraran Y, Yildirim HA, Sezen G, Iskender A, Karagoz I, et al. Comparison of effects on the oxidant/antioxidant system of sevoflurane, desflurane and propofol infusion during general anesthesia. Rev Bras Anestesiol. 2015;65:68–72. doi: 10.1016/j.bjan.2014.05.002. [DOI] [PubMed] [Google Scholar]
- 28.Nishiyama T, Yokoyama T, Hanaoka K. Liver function after sevoflurane or isoflurane anaesthesia in neurosurgical patients. Can J Anaesth. 1998;45:753–6. doi: 10.1007/BF03012146. [DOI] [PubMed] [Google Scholar]
- 29.Mohseni M, Safari S, Alavian SM. Volatile anesthetics in ischemic liver injury: Enemy or friend? Hepat Mon. 2014;14:e20153. doi: 10.5812/hepatmon.19880. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Yoon JH, Cho SH, Kim CS, Ahn KR, Kwon JH, Kang KS, et al. Comparisons of propofol, enflurane, sevoflurane, and desflurane anesthesia in laparoscopic cholecystectomy on postoperative liver enzyme levels. Korean J Anesthesiol. 2005;49:18–24. [Google Scholar]
- 31.Lee J, Kim MS, Lee HM, Lee JR, Park JH. The comparison of desflurane and sevoflurane on postoperative hepatic function of infant with biliary atresia undergoing Kasai operation. Anesth Pain Med. 2019;14:272–9. [Google Scholar]
- 32.Jacob R. Anaesthesia for biliary atresia and hepatectomy in paediatrics. Indian J Anaesth. 2012;56:479–84. doi: 10.4103/0019-5049.103965. [DOI] [PMC free article] [PubMed] [Google Scholar]


