Coronavirus disease 2019 (COVID-19), caused by the severe acute respiratory syndrome coronavirus-2 (SARS-CoV-2), is marked by a wide range and severity of symptoms. Most patients have mild to moderate symptoms, whereas 10%–15% require hospitalization. Mortality is higher with cardiovascular disorders, diabetes, and older age.1
Little is known about the clinical features of COVID-19 in the context of multiple sclerosis (MS), where some disease-modifying therapies (DMTs) may lead to immunocompromised state. Regarding the use of MS DMTs in the context of the COVID-19 pandemic, clinicians have had to make inferences, based on the DMT's mechanism of action and clinical trial data on infections, whether to continue, stop, or change the therapy in their patients with MS.2
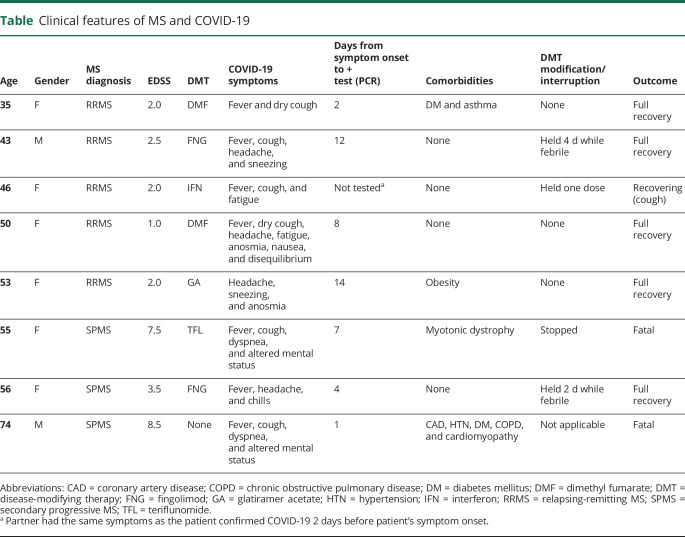
Here, we report our initial experience with COVID-19 among 8 patients with MS (table). The earliest case in our series occurred abroad in the early days of the COVID-19 outbreak. Other infections occurred locally in Washington and Oregon. The source of infection was a close contact in 2 cases, residential nursing facility in 2 cases, travel in 1, but not identified in 3 cases. Our case series consists mostly of female patients (6 of 8), aged 35–74, and most of whom had relapsing-remitting MS (5 of 8). Most of the patients had lower disability (Expanded Disability Status Scale [EDSS] score 1–3.5), with 2 exceptions (EDSS 7.5 and 8.5). Two patients were on injectable agents (1 interferon and 1 glatiramer), 2 on dimethyl fumarate (DMF), 1 on teriflunomide (TFL), and 2 on fingolimod (FNG), whereas 1 patient was not on DMT. None had a relapse or systemic corticosteroids recently. Neither of the patients on DMF had lymphopenia at baseline. Patients with FNG had lymphopenia (0.8 and 0.6 K/ul) at presentation and 6 months before COVID-19 infection, respectively.
Table.
Clinical features of MS and COVID-19
The most common presenting symptoms of COVID-19 in this cohort were fever (7 of 8), cough (6 of 8), and headache (4 of 8). Less common symptoms were sneezing (2), anosmia (2), fatigue (2), nausea (1), chills (1), and disequilibrium (1). One patient never developed fever. Two patient had dyspnea and altered mental status. We suspect that their altered mental status was probably due to hypoxia, although direct effect of SARS-CoV-2 on CNS could not be excluded.
COVID-19 diagnosis was confirmed by RT-PCR on a sample obtained by nasopharyngeal swab between 1 and 14 days after symptom onset, reflecting the challenges with laboratory testing at the time. One patient's diagnosis was not confirmed by RT-PCR, but her spouse, who had the same symptoms, tested positive 2 days earlier, so we believe that COVID-19 diagnosis is most likely accurate.
COVID-19 symptoms lasted 6–28 days. Three patients were hospitalized, one of them primarily for observation. Although symptomatic, 2 patients on FNG stopped taking their medication for 2 and 4 days (while febrile). The patient on interferon missed 1 dose. Patients on glatiramer acetate and DMF continued their treatment without interruption.
Two patients died. Both of these patients were severely affected by both MS (EDSS 7.5 17 and 8.5) and COVID-19 (hypoxia, fever, and altered mental status), in addition to having significant comorbidities. On admission, both patients had low absolute lymphocyte counts (0.6 and 0.58 K/uL) and one had increased liver function tests (AST 93 and ALT 66), probably because of the COVID-19 infection1 because laboratory test results were in the normal range 10 months before for the TFL-treated patient. Both patients were placed on supplemental oxygen, but continued to deteriorate. As per advanced directive of both patients, they were not intubated, and they died 3 and 4 days after the admission, respectively. Autopsy was not performed.
The full scope of COVID-19 manifestations in the MS population remains to be defined. To that end, we encourage all clinicians to follow our example and report their cases of COVID-19 in MS and related disorders in North America (covims.org) and elsewhere (msdataalliance.com). In publishing this initial report, we wanted to share our experiences and observations among patients from a region with early community spread of SARS-CoV-2 in the United States.3 We were relieved that most of these infections were mild and in line with observations in general (non-MS) population. At the same time, the fatal outcome in our most disabled patients portends significant risks for patients with advanced MS. Most of our patients remained on their DMTs with no interruption during the COVID-19 infection. However, the generalizability of this finding is limited because none of these were cell-depleting therapies, and most infections were mild. We hope that larger studies will provide more definitive information on additional risks associated with MS DMTs in COVID-19 and hospitalization outcomes to better inform our care for this population.
Appendix. Authors
Study funding
No targeted funding reported.
Disclosure
J.D. Bowen, J. Brink, T. Brown, E.B. Lucassen, K. Smoot, A. Wundes, and P. Repovic report no financial disclosures relevant to the topic of this manuscript. Go to Neurology.org/NN for full disclosures.
References
- 1.Guan WJ, Ni ZY, Hu Y, et al. Clinical characteristics of coronavirus disease 2019 in China. N Engl J Med 2020;382:1708–1720. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Giovannoni G, Hawkes C, Lechner-Scott J, Levy M, Waubant E, Gold J. The COVID-19 pandemic and the use of MS disease-modifying therapies. Mult Scler Relat Disord 2020;39:102073. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Bhatraju PK, Ghassemieh BJ, Nichols M, et al. Covid-19 in critically ill patients in the Seattle region—case series. N Engl J Med 2020;382:2012–2022. [DOI] [PMC free article] [PubMed] [Google Scholar]