Abstract
The Ministry of Health, Labor, and Welfare of Japan recommends that an occupational physician (OP) play an important role in implementing the stress-check program since 2015. This study aimed to compare the activities and encountered difficulties of Japanese part-time OPs in 2008 and 2016, and to investigate the effects of the stress-check program. Questionnaires were sent via mail to 946 part-time OPs in Kyoto prefecture in 2016. Completed questionnaires were returned by 181 OPs who were private practitioners or physicians in hospitals, and served as OPs on a part-time basis. In 2016, OPs utilized long hours for activities related to general health examination and to stress-check. Hours for specific health examination, health and hygiene education, health promotion activity, development of a comfortable workplace, and guidance of workers on sick leave reduced from 2008 to 2016. A total of 62% OPs frequently encountered difficulties in the stress-check-related activities in 2016. Many OPs also reported difficulties in the mental health care and the prevention of health hazard due to overwork both in 2008 and 2016. Enforcement of the stress-check program in 2015 changed the activities of part-time OPs in Japan. OPs should be given opportunities to gain more information in this area.
Keywords: Difficulties in occupational health service, Enterprise size, Japan, Part-time, Occupational physician, Stress-check program
Introduction
Occupational physicians (OPs) in Japan are responsible not only for the maintenance of the health of employees through regular health examinations, health guidance and consultation, but also for the maintenance and management of work conditions and the work environments. The responsibility of OPs also includes contribution to the prevention of overwork and mental health problems1). The overwork and mental health are especially important because cases of mental ill health possibly due to overwork are increasing and currently represent a pressing problem in Japan2, 3).
The Japan Society for Occupational Health (JSOH) provides course to train up specialist occupational physicians (OPs), but the number of JSOH-qualified OPs is still limited4). Thus, a majority of OPs in Japan are trained by the Japan Medical Association (JMA) through its training course5); according to JMA statistics, such certifications were given to 99,170 doctors in 2018 and earlier6).
Of the JMA-certified OPs, 40% were private practitioners and 57% were based in hospitals6), and mostly served on a part-time basis (to be called part-time OPs in this article). As their large number suggests, the JMA-certified part-time OPs are indeed core forces in occupational health services (OHS), especially in small- (with <50 employees) and medium-scale (with 50 to 999 employees) enterprises. The number of currently active JSOH-qualified OPs is estimated to be about 6684); these OPs mostly serve in large-scale (with ≥1,000 employees) enterprises or occupational health organizations, or have their own independent offices on a full-time basis (to be called specialist OPs); OPs who serve in large-scale enterprises or occupational health organizations are not always JSOH-qualified but they are very much specialized through practice.
A nation-wide survey conducted by the Ministry of Health, Labour and Welfare, Japan7) revealed that 86.0% of enterprises with ≥50 employees had OPs (either with a full-time or part-time contract). As expected, the percentage was higher (99.4%) for enterprises with ≥1,000 employees and lower (79.9%) for enterprises with 50 to 99 employees. The percentage for even smaller enterprises (so-called micro-enterprises) is not known as there was no legal stipulation that the micro-enterprises have OPs.
Reports on the activities and job demand of OPs have been published by several research groups8,9,10,11,12,13,14,15) as well as by a number of regional occupational health promotion centers16,17,18). Nevertheless, there are no currently available reports on the difficulties experienced by private clinic- or hospital-based part-time OPs in their daily OHS or that evaluate the time spent by OPs in various OHS activities except for Moriguchi et al19).
In 2015, the Ministry of Health, Labour and Welfare (MHLW), Japan launched the Stress Check Program (SC) that makes annual questionnaire survey to screen employees with high psychosocial stress in all workplaces with 50 or more employees20). The following two components of SC are enforced: (1) decreasing the risk of mental health problems through annual survey results to employees, and (2) prevention of mental health problems by screening high-risk employees and giving them an opportunity to consult with a physician. The MHLW recommends that this consultation should be conducted by an OP of the workplace. The MHLW also recommends that OPs should be in charge of planning of SC in enterprises and evaluation of their results. Therefore the load of OPs might be increased by enforcement of SC.
The purpose of the present study was to characterize the OHS performed by active part-time OPs in Kyoto Prefecture, Japan after the enforcement of SC. The survey focused on the current and desired length of time spent by OPs in major OHS activities. The survey targets were further extended to identify difficulties the OPs had encountered during their OHS. The results of the survey on part-time OPs in 2016 were compared with the findings on part-time OPs in 2008 to investigate the effects of SC19).
Materials and Methods
For the questionnaire survey, the List of OPs prepared by the Kyoto Medical Association, Kyoto, Japan was employed. The list was continually up-dated by the Association taking advantage of additional available information for effectiveness of communication with the OPs. In 2016, the list contained the names and postal addresses of 946 OPs.
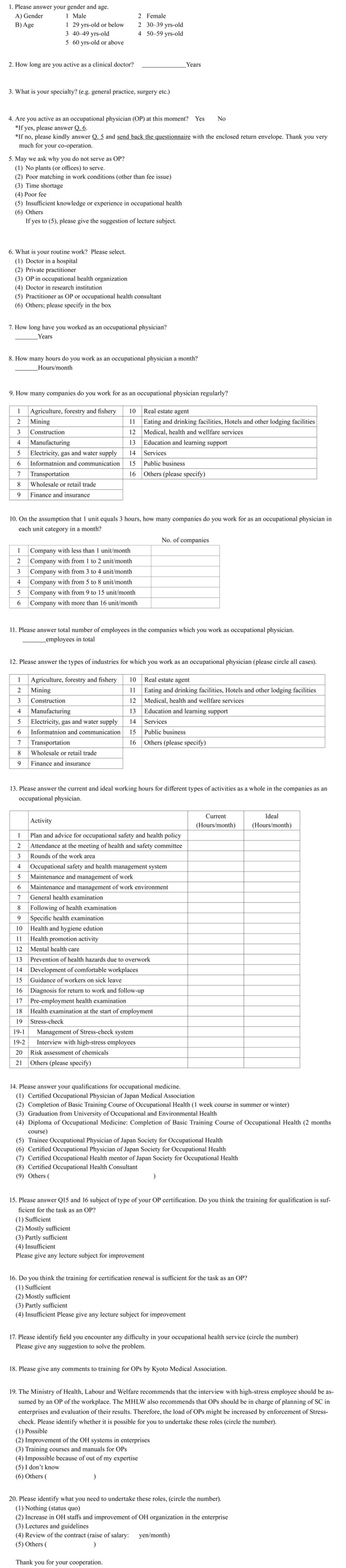
The questionnaires (in Japanese; for details, see Appendix quoted from Moriguchi et al.19)) was sent by mail to the 946 OPs in the registry early in October, 2016. The completed questionnaires were collected at the end of November. Responses were received from 363 OPs (response rate: 38%); of these, 139 physicians stated that they were no longer active as OPs. Thus, the usable answers (excluding those from 34 cases of industrial health organization-based specialist OPs and 9 invalid answers) were obtained from 181 OPs (50% of the 363 respondents, or 19% of the original 946 mail addressees), who were either private clinic-based or hospital-based (131 and 50 OPs, respectively). The present analyses were conducted based on the 181 effective answers. The data of the study were compared with the data of similar survey implemented in 200819), if necessary.
To compare the current and desired hours for each service field of OPs, the database of the subjects who answered both current and desired hours was conducted (n=102). The database was applied to Table 4, as to be discussed later.
Table 4. Comparison of time allocation by fields of service of the occupational physicians in 2016: current versus desired allocation.
| Field of services | Time allocation (hr) | |||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Current | Desired | Desired/current | Differencea | Wilcoxon test | ||||||||||
| N | AM ± ASD | Min | Med | Max | N | AM ± ASD | Min | Med | Max | % | p-value | |||
| 1 | Plan and advice for OSH policy | 46 | 1.3 ± 2.0 | 1 | 1 | 12 | 46 | 1.4 ± 1.8 | 0 | 1 | 10 | 109 | 0.1 | <0.05 |
| 2 | Attendance at the meeting of HS committee | 78 | 1.4 ± 1.2 | 0 | 1 | 7 | 78 | 1.6 ± 1.3 | 0 | 1 | 6 | 115 | 0.2 | <0.01 |
| 3 | Rounds of the work area | 78 | 1.2 ± 1.4 | 0 | 1 | 10 | 78 | 1.8 ± 3.4 | 0 | 1 | 30 | 151 | 0.6 | <0.01 |
| 4 | Occupational safety and health management system | 30 | 0.4 ± 0.6 | 0 | 0 | 3 | 30 | 0.7 ± 0.8 | 0 | 1 | 4 | 176 | 0.3 | <0.01 |
| 5 | Maintenance and management of work | 29 | 0.4 ± 0.6 | 0 | 0 | 3 | 29 | 0.8 ± 0.9 | 0 | 1 | 4 | 194 | 0.4 | <0.01 |
| 6 | Maintenance and management of work environment | 33 | 0.4 ± 0.6 | 0 | 0 | 3 | 33 | 0.9 ± 1.2 | 0 | 1 | 6 | 206 | 0.5 | <0.01 |
| 7 | General health examination | 52 | 2.1 ± 5.7 | 0 | 1 | 40 | 52 | 2.1 ± 5.6 | 0 | 1 | 40 | 100 | 0.0 | NS |
| 8 | Follow-up of examination | 64 | 1.9 ± 2.6 | 0 | 1 | 20 | 64 | 1.9 ± 2.0 | 0 | 1 | 10 | 100 | 0.0 | NS |
| 9 | Specific health examination | 30 | 0.3 ± 0.5 | 0 | 0 | 20 | 30 | 0.5 ± 0.5 | 0 | 1 | 2 | 186 | 0.2 | <0.01 |
| 10 | Health and hygiene education | 34 | 0.4 ± 0.6 | 0 | 0 | 3 | 34 | 0.9 ± 1.3 | 0 | 1 | 6 | 267 | 0.6 | <0.01 |
| 11 | Health promotion activity | 33 | 0.3 ± 0.6 | 0 | 0 | 4 | 33 | 0.9 ± 1.1 | 0 | 1 | 5 | 271 | 0.6 | <0.01 |
| 12 | Mental health care | 57 | 1.4 ± 2.5 | 0 | 1 | 15 | 57 | 1.6 ± 2.1 | 0 | 1 | 12 | 115 | 0.2 | <0.01 |
| 13 | Prevention of health hazards due to overwork | 44 | 1.8 ± 3.3 | 0 | 1 | 16 | 44 | 2.3 ± 3.1 | 0 | 1 | 16 | 123 | 0.4 | <0.01 |
| 14 | Development of comfortable workplaces | 29 | 0.2 ± 0.6 | 0 | 0 | 3 | 29 | 0.7 ± 1.0 | 0 | 1 | 4 | 332 | 0.5 | <0.01 |
| 15 | Guidance of workers on sick leave | 42 | 0.6 ± 1.0 | 0 | 1 | 8 | 42 | 0.9 ± 1.0 | 0 | 1 | 6 | 156 | 0.3 | <0.01 |
| 16 | Diagnosis for return to work and follow-up | 45 | 0.7 ± 0.8 | 0 | 1 | 4 | 45 | 1.0 ± 0.9 | 0 | 1 | 4 | 132 | 0.2 | <0.01 |
| 17 | Pre-employment health examination | 31 | 0.5 ± 0.9 | 0 | 0 | 20 | 31 | 1.0 ± 1.8 | 0 | 1 | 10 | 174 | 0.4 | <0.01 |
| 18 | Health examination at the start of employment | 37 | 0.6 ± 0.7 | 0 | 0 | 20 | 37 | 0.8 ± 1.0 | 0 | 1 | 5 | 142 | 0.2 | <0.05 |
| 19 | Stress-check | 59 | 1.6 ± 1.7 | 0 | 1 | 35 | 59 | 2.1 ± 2.4 | 0 | 1 | 13 | 130 | 0.5 | <0.05 |
| 19-1 | Management of Stress-check system | 42 | 0.9 ± 1.2 | 0 | 1 | 35 | 42 | 1.2 ± 1.7 | 0 | 1 | 10 | 137 | 0.3 | <0.05 |
| 19-2 | Interview with high-stress employees | 49 | 1.2 ± 1.2 | 0 | 1 | 4 | 49 | 1.4 ± 1.2 | 0 | 1 | 5 | 126 | 0.3 | <0.05 |
| 20 | Risk assessment of chemicals | 27 | 0.2 ± 0.4 | 0 | 0 | 3 | 27 | 0.4 ± 0.6 | 0 | 0 | 2 | 232 | 0.2 | <0.01 |
| 21 | Others | valign="top"5 | 0.2 ± 0.4 | 0 | 0 | 1 | 5 | 0.2 ± 0.4 | 0 | 0 | 1 | 100 | 0.0 | NA |
| Total (divided by answered subjects) | 102 | 9.1 ± 12.1 | 102 | 11.8 ± 15.9 | 130 | 2.7 | <0.01 | |||||||
OSH: Occupational safety and health; HS: Health and safety; AM: Arithmetic mean; ASD: Arithmetic standard deviation; Med: Median; Min: Minimum; Max: Maximum; NS: Not significant; NA: Not assessable due to insufficient number of data. aAM of Desired time − AM of Current time.
With regard to the enterprises served, a single enterprise may, depending on its scale, have more than one business office or production plant, e.g., a head office and several production plants. In the present study, both offices and plants are referred to as ‘plants’.
A normal distribution of the data was assumed, and the arithmetic mean (AM) and arithmetic standard deviation (ASD) of the data were calculated. However, because a normal distribution of the data was not always confirmed, Mann-Whitney test and Wilcoxon test were employed to detect possible difference. The χ2 test was also applied when appropriate. For evaluation of statistical significance, p<0.05 was employed as the cut-off point.
The research procedures were approved the board meeting of Kyoto Medical Association. As mentioned above, the questionnaires were sent by mail to the OPs from the Kyoto Medical Association. Participants were informed in advance that their participation was voluntary and that all information provided would handle confidentially. Only those who consented to participate answered the questionnaire. The questionnaire was conducted as an anonymous self-administrated style. No respondent could not be identified based on the presented procedure.
Results
Demographic and other characteristics of the 86 active OPs in 2008 and 181 active OPs in 2016
Of the 181 OPs in 2016 who completed the questionnaires, 153 and 23 (87 and 13%) were men and women, respectively; genders were not made clear in 5 cases. One hundred and thirty one physicians were private practitioners and 50 others were physicians in hospitals. The proportion of physicians in their 30’s, 40’s, and 50’s and those who were 60 yrs of age and over were 3%, 10%, 31% and 57%, respectively; a majority being over 50 yrs of age. The length of clinical practice experience was 32.3 ± 10.8 yr (AM ± ASD; median=32 yr), and most of the respondents specialized in general practice or internal medicine. All of OPs in 2016 were certified OP of JMA, and 6 of them had certification of the occupational health consultant. There were no OPs with JSOH certification.
There was essentially no difference between active OPs in 2008 and those in 2016 in demographic and other patterns (Table 1).
Table 1. Demographic and other characteristics of occupational physicians in 2008 and 2016.
| Elements | 2008 | 2016 | p-value | |||||
|---|---|---|---|---|---|---|---|---|
| N | Number | %a | N | Number | %a | |||
| Sex (men/women) | 86 | 77/9 | 90/10 | 176 | 153/23 | 87/13 | NSb | |
| Main line of businness | Private practitioners | 86 | 64 | 74.4 | 181 | 131 | 72.4 | NSb |
| Physicians in hospitals | 22 | 25.6 | 50 | 27.6 | ||||
| Age group | 30’s | 86 | 3 | 3.5 | 181 | 5 | 2.8 | NSb |
| 40’s | 13 | 15.1 | 17 | 9.4 | ||||
| 50’s | 22 | 25.6 | 56 | 30.9 | ||||
| 60’s and over | 48 | 55.8 | 103 | 56.9 | ||||
| Length of clinical experience (AM ± ASD) | 86 | 33.4 ± 9.7 | 181 | 32.3 ± 10.8 | NSc | |||
| Experiences as an OP (AM ± ASD) | 86 | 13.4 ± 8.3 | 177 | 13.3 ± 8.4 | NSc | |||
| Monthly service hours as an OP (AM ± ASD) | 86 | 6.2 ± 8.1 | 179 | 6.9 ± 12.4 | NSc | |||
aPercentage in total number of answers. bNot significant by χ2 test, cNot significant by Mann-Whitney test. AM: arithmetric mean; ASD: arithmetric standard deviation; OP: occupational physician.
Services as OPs
The 177 of 181 respondents had experiences as OPs of 13.3 ± 8.4 yr (median=11 yr). They served in plants 6.9 ± 12.4 h/month (median=4 h); the monthly service hours showed a remarkable skewness.
In total, the 181 OPs in 2016 served in 423 plants. Similar to the OPs in 2006, of these plants, the majority (356 plants or 84%) had less than 300 employees (Table 2). One OP served in 1 to 18 plants with an average of 2.3 (± 1.9 as AM ± ASD; median=2 plants).
Table 2. Number of plants classified by number of employees.
| No. of employees | 2008 | 2016 | χ2 test |
|---|---|---|---|
| No. of plants served by OPs (%) | No. of plants served by OPs (%) | p-value | |
| <50 | 39 (19.6) | 51 (12.1) | NS (2 × 6) |
| 50–99 | 77 (38.7) | 180 (42.6) | |
| 100–299 | 58 (29.1) | 125 (29.6) | |
| 300–499 | 15 (7.5) | 32 (7.6) | |
| 500–999 | 5 (2.5) | 21 (5.0) | |
| ≥1,000 | 5 (2.5) | 14 (3.3) | |
| Total | 199 (100.0) | 423 (100.0) | |
OP: occupational physician; NS: Not significant.
Considering 3 h as a unit of service, a majority (93%) served <1 to 2 units/month; of these, most served less than 1 unit/month (Fig. 1). When asked the number of employees treated by an individual OP, 12 of the 181 OPs gave no answer. An analysis of the remaining 169 cases showed that each OP served between 15 and 10,000 employees (AM ± ASD, 618 ± 1,396; median, 250). As shown in >Fig. 2, there was a remarkable skewness in the distribution. The skewness was approximately same as the distribution of Moriguchi et al19). Classification by type of business of enterprises showed that 69 OPs (38%) served in clinical or health and welfare-related enterprises, while 59 OPs (33%) served in manufacturing industries. Proportion of clinical or health and welfare-related enterprises increased from 26% in 2008 to 38% in 2016 significantly (p-value<0.05).
Fig. 1.
Number of units served by occupational physicians in enterprises.
Fig. 2.
Number of employees served by one occupational physician.
Time allocation for activities; comparison between the current and desired allocations
The leading fields of service in which the OPs in 2016 spent their times were [7. General health examination] (1.9 h/month; Table 3), [19. Stress-Check] (1.9 h/month), [8. Follow-up of health examination] (1.8 h/month), [13. Prevention of health hazards due to overwork] (1.7 h/month), [2. Attendance at the meeting of Health and safety (HS) committee] (1.5 h/month), and [12. Mental health care] (1.5 h/month). Hours for [9. Specific health examination], [10. Health and hygiene education, [11. Health promotion activity], [14. Development of a comfortable workplace], and [15. Guidance of employees on sick leave] reduced from 2008 to 2016 significantly (p-value<0.01 in most cases; Tables 3). The total working hours appeared to be increased from 2008 to 2016 (7.4 h/month to 9.9 h/month), although the difference was not statistically significant (p=0.24).
Table 3. Comparison of time allocation by fields of service between the occupational physicians in 2008 and in 2016.
| Field of services | Time allocation (hr) | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 2008 | 2016 | Mann-Whitney test | ||||||||||
| N | AM ± ASD | Min | Med | Max | N | AM ± ASD | Min | Med | Max | p-value | ||
| 1 | Plan and advice for OSH policy | 34 | 1.0 ± 0.7 | 0.1 | 1 | 4 | 71 | 1.3 ± 2.0 | 1 | 1 | 12 | NS |
| 2 | Attendance at the meeting of HS committee | 53 | 1.4 ± 1.4 | 0.1 | 1 | 7 | 121 | 1.5 ± 1.4 | 0 | 1 | 7 | NS |
| 3 | Rounds of the work area | 56 | 1.2 ± 0.9 | 0.1 | 1 | 4 | 124 | 1.3 ± 1.7 | 0 | 1 | 10 | NS |
| 4 | Occupational safety and health management system | 8 | 0.6 ± 0.4 | 0.1 | 0.5 | 1 | 44 | 0.5 ± 0.8 | 0 | 0 | 3 | NS |
| 5 | Maintenance and management of work | 10 | 0.6 ± 0.4 | 0.1 | 0.5 | 1 | 41 | 0.5 ± 0.7 | 0 | 0 | 3 | NS |
| 6 | Maintenance and management of work environment | 13 | 0.6 ± 0.4 | 0.1 | 0.5 | 1 | 51 | 0.5 ± 0.7 | 0 | 0 | 3 | NS |
| 7 | General health examination | 33 | 2.2 ± 2.9 | 0.2 | 1 | 12 | 75 | 1.9 ± 4.8 | 0 | 1 | 40 | NS |
| 8 | Follow-up of examination | 50 | 1.9 ± 2.3 | 0.1 | 1 | 10 | 112 | 1.8 ± 2.7 | 0 | 1 | 20 | NS |
| 9 | Specific health examination | 11 | 1.1 ± 1.2 | 0.1 | 1 | 4 | 43 | 0.8 ± 3.1 | 0 | 0 | 20 | −0.01 |
| 10 | Health and hygiene education | 7 | 1.2 ± 0.9 | 0.1 | 1 | 2 | 45 | 0.4 ± 0.7 | 0 | 0 | 3 | −0.01 |
| 11 | Health promotion activity | 12 | 1.3 ± 1.4 | 0.1 | 1 | 4 | 49 | 0.5 ± 0.8 | 0 | 0 | 4 | −0.01 |
| 12 | Mental health care | 24 | 1.5 ± 1.2 | 0.1 | 1 | 5 | 92 | 1.5 ± 2.7 | 0 | 1 | 15 | NS |
| 13 | Prevention of health hazards due to overwork | 25 | 1.7 ± 1.8 | 0.2 | 1 | 8 | 68 | 1.7 ± 2.9 | 0 | 1 | 16 | NS |
| 14 | Development of comfortable workplaces | 6 | 1.1 ± 1.0 | 0.3 | 1 | 3 | 44 | 0.3 ± 0.7 | 0 | 0 | 3 | −0.01 |
| 15 | Guidance of workers on sick leave | 13 | 1.2 ± 0.9 | 0.2 | 1 | 3 | 61 | 0.8 ± 1.3 | 0 | 1 | 8 | −0.05 |
| 16 | Diagnosis for return to work and follow-up | 19 | 1.2 ± 0.8 | 0.2 | 1 | 3 | 67 | 0.9 ± 1.0 | 0 | 1 | 4 | NS |
| 17 | Pre-employment health examination | 15 | 0.9 ± 0.5 | 0.1 | 1 | 2 | 48 | 1.1 ± 3.2 | 0 | 0 | 20 | −0.01 |
| 18 | Health examination at the start of employment | 15 | 1.0 ± 0.8 | 0.1 | 1 | 3 | 52 | 1.0 ± 2.8 | 0 | 0 | 20 | NS |
| 19 | Stress-check | - | - | - | - | 92 | 1.9 ± 4.0 | 0 | 1 | 35 | - | |
| 20 | Risk assessment of chemicals | - | - | - | - | 37 | 0.3 ± 0.6 | 0 | 0 | 3 | - | |
| 21 | Others | 3 | 1.8 ± 0.3 | 1.5 | 2 | 2 | 7 | 0.3 ± 0.4 | 0 | 0 | 1 | NA |
| Total (divided by answered subjects) | 75 | 7.4 ± 8.7 | 161 | 9.9 ± 15.3 | NS | |||||||
| Total hours divided by total subjects | 86 | 6.5 ± 8.5 | 181 | 8.8 ± 14.8 | NS | |||||||
OSH: Occupational safety and health; HS: Health and safety; AM: Arithmetic mean; ASD: Arithmetic standard deviation; Med: Median; Min: Minimum; Max: Maximum; NS: Not significant; NA: Not assessable.
OPs wished to allocate more time for [13. Prevention of overwork] (2.3 h/month, Table 4), [7. General health examination] (2.1 h/month), [19. Stress-check] (2.1 h/month), [8. Follow-up of examination] (1.9 h/month), and [3. Round of the work area] (1.8 h/month). From a detailed observation of [19. Stress-check], OPs wished to allocate more time for both [19-2. Interview with high-stress employees] (1.2 h/month), and [19-1. Management of Stress-check system] (1.4 h/month).
The discrepancy between the current and the desired allocation was greatest for [14. Development of comfortable workplaces] (332% as the desired/current ratio). The discrepancy for [11. Health promotion activity] and [10. Health and hygiene education] were great as well (271 and 267%, respectively). In contrast, time allocation for fields related to periodical general health examinations appeared to be sufficient (i.e., Fields 7 and 8 in the Difference column in Table 4).
Difficulties encountered by OPs
In 2016, difficulties were experienced most often in [19. Stress-check] (112 OPs; Table 5). The former was followed by [12. Mental health care] (66 OPs), [13. Prevention of health hazard due to overwork] (61 OPs) and [16. Diagnosis of return to work] (38 OPs). From a detailed observation of [19. Stress-check], OPs encountered difficulties more in [19-2. Interview with high-stress employees] than [19-1. Management of Stress-check system].
Table 5. Fields of difficulties experienced by occupational physicians in 2008 and 2016.
| Field of services | 2008 | 2016 | χ2 test | |
|---|---|---|---|---|
| Cases (%)a | Cases (%)b | p-value | ||
| 1 | Plan and advice for OSH policy | 3 (3) | 11 (6) | NA |
| 2 | Attendance at the meeting of HS committee | 3 (3) | 11 (6) | NA |
| 3 | Rounds of the work area | 3 (3) | 18 (10) | NA |
| 4 | Risk assessment | 14 (16) | 24 (13) | NS |
| 5 | Maintenance and management of work | 11 (13) | 16 (9) | NS |
| 6 | Maintenance and management of work environment | 11 (13) | 15 (8) | NS |
| 7 | General health examination | 0 (0) | 6 (3) | NA |
| 8 | Follow-up of examination | 4 (5) | 9 (5) | NA |
| 9 | Specific health examination | 12 (14) | 19 (10) | NS |
| 10 | Health and hygiene education | 4 (5) | 15 (8) | NA |
| 11 | Health promotion activity | 2 (2) | 9 (5) | NA |
| 12 | Mental health care | 36 (42) | 66 (36) | NS |
| 13 | Prevention of health hazards due to overwork | 30 (35) | 61 (34) | NS |
| 14 | Development of comfortable workplaces | 6 (7) | 15 (8) | NS |
| 15 | Guidance of workers on sick leave | 11 (13) | 30 (17) | NS |
| 16 | Diagnosis for return to work and follow-up | 15 (17) | 38 (21) | NS |
| 17 | Pre-employment health examination | 1 (1) | 7 (4) | NA |
| 18 | Health examination at the start of employment | 3 (3) | 7 (4) | NA |
| 19 | Stress-check | - (---) | 112 (62) | - |
| 19-1 | Management of Stress-check system | - (---) | 37 (20) | - |
| 19-2 | Interview with high-stress employees | - (---) | 75 (41) | - |
| 20 | Risk assessment of chemicals | - (---) | 34 (19) | - |
| 21 | Others | 4 (5) | 4 (4) | NA |
| Total | 173 | 527 | ||
OSH: Occupational safety and health; HS: Health and safety; NS: Not significant; NA: Not assessable due to insufficient number of data. aPercentage for 86 occupational physicians. bPercentage for 181 occupational physicians.
There was essentially no difference between difficulties encountered by OPs in 2008 and those in 2016. Because most OPs major in general practice, the respondents were generally self-confident regarding physical health management (typically providing general health examinations) except for a few specific health examination issues both in 2006 and 2016.
To solve the problems related to lack of experience with mental health issues including Stress-check, proposals were made by 39 OPs. Dominant opinions were increase of training course for information exchange of experiences on these issues with experts such as psychiatrists or highly professional OPs (9 OPs) and sharing roles of mental health issues with psychiatrists (8 OPs). Of the 181 OPs in 2016, 45 (25%) answered that training for JMA qualification was sufficient.
Reasons for terminating OP activities
As stated above, 139 physicians responded that they were no longer active as OPs. When asked (by multiple choice) for their reasons for ending such service, the most common answer was shortage of time (93 cases, 51%), followed by lack of suitable enterprises (44 cases, 24%). Insufficiency of knowledge and experiences were mentioned in 14 cases (8%).
Discussion
The present study disclosed that major points concerning the involvement of OPs in Kyoto Prefecture, Japan; 1. a majority of OPs serve less than 6 h/month, 2. the leading service provided by OPs are practice of general health examinations and stress-check related issues in 2016, and 3. the stress-check related activities and the mental health issues create the major difficulties in OPs’ daily OHS activities in 2016.
The analyses reported in the present survey were primarily based on responses from 181 currently active OPs in 2016. The fact that 139 physicians (38% of 363 respondents) were inactive at the time of the present survey suggests that many physicians are not active as OPs despite the fact that they possess JMA certification. Terada et al.10) observed that only 94 (23%) physicians were active out of 405 private clinic- or hospital-based physicians who had registered as OPs in a labour standard inspection office in central Tokyo. The number of OPs registered by the Kyoto Medical Association as certified OPs represent 946 members of the Association. It is quite conceivable that the OHS participation rate of the 946 certified OPs may not be high.
Among the 181 respondents, the proportion of men (87%) was approximately equal to the proportion of men among all physicians, i.e., 78.9% for men vs. 21.1% for women21). In the report of Japan Medical Association in 2018, 82.0% of OPs, were reported to be men22). These results suggest that OHS is provided by the two genders with no specific bias in this study. Many OPs (36.8%) serve in only one enterprise in the report of Japan Medical Association as well.
With regard to age distributions, a large fraction of the present survey participants was >60 yrs of ages. The OPs participating in the present survey are older than those in the report of Japan Medical Association, where the modes in age distribution fell within the 50’s22). Similar studies implemented by other prefectures did not collect data on age16,17,18).
The results of classification by type of business of enterprises where OPs served showed that proportion of the clinical or health and welfare-related enterprises increased significantly. In 2019, the Japan Medical Association22) reported that many of OPs of hospitals belonged to the same hospital where they were serving as an OP, and have their main job as a clinician in the hospital. Since 2015, owner/employer physicians of hospitals had been prohibited to be an OP of their own hospital (Ordinance on Industrial Safety and Health)23). After the amendment of the Ordinance, OPs in hospitals are supposed to be shifting from owner/employer physicians to employee physicians gradually. Moreover, the subjects of our survey did not involve owner/employer physicians in hospitals in 2008 and 2016. These situations might have affected the increase of the proportion of clinical or health and welfare-related enterprises in the present study.
OPs reported spending many hours for [12. Mental health care], [13. Prevention of health hazards due to overwork], [19. Stress-check] as well as [7.+8. General examinations and follow-up]. Except for [19. Stress-check], time allocation for these major services did not differ from 2008 to 2016. It is interesting to note that while OPs in other studies in Japan, like the OPs in the present survey, reported spending many hours for health examination and follow-up24), or health counseling22), OPs in other studies reported spending less time on management of mental health issues and over-work cases than OPs in the present analysis. Management of mental health and health hazards due to overwork, however, has been among the important issues of OH3, 25, 26). The report of Japan Medical Association22) stated that 67.5% of OPs take up interview with high-stress employee. Reduction of [9. specific health examination], [10. health and hygiene education], [11. health promotion activity], and [14. development of a comfortable workplace] from 2008 to 2016 might be affected by that most of OPs need to spend substantial hours for SC since enforcement of the stress-check program in 2015. Despite the reduction of these fields, the total working hours appeared to be increased from 2008 to 2016 (7.4 h/month to 9.9 h/month, statistically not significant). This could be important considering that the introduction of SC occurred during this period. All OPs in the present study were private practitioners or based in hospitals, and served in a part-time basis as an OP. Therefore the increase of total working hours as a part-time OP would arise difficulty in time management of their whole working hours.
With regard to the current versus desired time allocation, the results obtained in the present survey of part-time OPs generally agree with previous findings on part-time OPs in 200819). In 2008, OPs expressed the desire to have more time for 1. Plan and advice for Occupational safety and health (OSH) policy, 2. Attendance at the meeting of HS committee, 3. Rounds of the work area, 4. Risk assessment, 5. Maintenance and management of work, 6. Maintenance and management of work environment, and 12. Mental health care. There are great increases in 10. Health and hygiene education, 11. Health promotion activity, and 14. Development of comfortable workplace from 2008 to 2016. However, increases of these fields might have been affected by the decreases of the current hours for these fields in 2016 compared to 2008. Therefore these differences suggested that OPs in 2016 wished to regain the hours for preventive services reduced by enforcement of SC since 2015. OPs in 2008 wished to increase time allocation for mental health care including 12. Mental health care and 13. Prevention of health hazards due to overwork (Desired/Current=132%, p<0.01; Wilcoxon test), OPs in 2016 also wished to increase time allocation for those fields and 19. Stress-check (Desired/Current=123% p<0.01; Wilcoxon test). These results suggested that OP regarded hours for mental health care were still insufficient after enforcement of SC since 2015.
In 2016, majority of OP felt difficulty in SC-related issues, especially in interview with high-stress employees (Table 5). In many countries, mental health-related issues are one of the main targets of OH activities14, 27). In Japan, a questionnaire survey for OPs belonging to an enterprise or OH service organization (that may mean full-time OP) showed that 86% of OPs felt employers’ high expectation for mental health related activities as well28). However most of part-time OPs in Japan have primary job in their own clinic or hospital, and working as an OP is sometimes regarded as their side job. Because most of respondents in the present study were specialized in general practice or internal medicine, they might have thought SC-related issues were out of their realm of expertise. In the report of Japan Medical Association, 16% of OPs described the reason of not dealing with the SC-related issues that they are not specialized in mental health22). Similar reason might have affected the feeling of difficulty of OPs in the present study.
The SC program has been newly introduced in OH in Japan. It is a unique approach for employees’ mental health. The WHO and ILO proposed risk assessment and management of psychosocial risk at work as a major strategy for improving employees’ mental health29, 30). The Psychosocial Risk Management Excellence Framework (PRIMA-EF) also proposed a European risk assessment and management at work31). These approaches focus on the psychosocial factors in workplaces. However, the SC in Japan focuses on psychosocial stress of individual employees. Although physician’s interview with high-stress employee is mandatory for employers, improvement of work environment is not obligated to the employers. It is attributable to the context that health examinations are provided by employers to the individual employees in Japan, which is unique in the world as well.
Many OPs wished to increase the training course for information exchange of experiences on mental health issue with psychiatrists or highly professional OPs. Nagata et al.32) has made a proposal of 15 minimum practical requirements of non-specialist OPs like OPs in the present study. Three items of 15 requirements were related to mental health. Therefore it would be reasonable to increase the training course for mental health. The minimum legal requirement of OPs is the completion of 50 h training to obtain the JMA certification, and a 20 h training to renew the certification in Japan. Although there is variation in postgraduate training for OPs among countries, OPs are obliged to have several years of training and pass the exit examination in many countries33). In France and the Netherlands, physicians have to finish 4 years of postgraduate training to work as an OP34, 35). When compared to other countries, it is relatively easy to obtain the certification in Japan. To reduce the difficulties of OPs, increase of training hours should be considered.
The answers of reasons for ending OP activities showed that the dominant reasons were shortage of time and lack of suitable enterprises. In this context, lack of suitability may imply inconvenience of commuting to the base clinical facilities or poor economic efficiency.
The present analysis has several limitations. First, only 12.1% of the enterprises served by the present 181 OPs had less than 50 employees (Table 2), whereas the enterprises with less than 50 employees accounted for 97.0% in Kyoto Prefecture36) and 96.8 in Kyoto City37). Thus, although a majority of the enterprises studied were of small- and medium-scale, the enterprise size of the present survey (Table 2) was skewed toward to larger ones. There is no legal stipulation that the enterprises with less than 50 employees have OPs in Japan38). Therefore although most of enterprises in Kyoto were small-size, situation of SC-related activities in those enterprises without OPs could not be investigated sufficiently in the present study.
With regard to the types of enterprises, health-related and manufacturing enterprises were two leading types of enterprises that employed the OPs surveyed in the present study. Both in Kyoto Prefecture39) and in Kyoto City40), the health-related and manufacturing enterprises took the 5th and the 3rd positions in the number of enterprises, indicating that the present study is biased in the distribution of types of industries studied.
A third limitation of the present study is that, while both musculoskeletal disorder and mental ill health were some of main symptoms reported by employees in Europe41), musculoskeletal disorder issues were not specifically addressed in the present analyses. In addition, Horppu et al.42) stressed the positive role of OPs in enabling the early return of employees to workplaces after episodes of musculoskeletal pain or depressive symptoms. Although the return of employees to workplaces was discussed in general, specific needs such as post-stroke care43) were not addressed.
Conflict of Interests
The authors declare that they have no conflict of interests.
Acknowledgments
The authors are grateful to the administration and staff of the Kyoto Industrial Health Association and the Kyoto Medical Association for their interest in and support of this work.
Appendix.
The questionnaires
References
- 1.Ministry of Health, Labour and Welfare, Japan (2006) Ordinance on Industrial Safety and Health (Article 14 amended in 2015). Ministry of Health, Labour and Welfare, the Government of Japan, Tokyo, Japan (in Japanese). [Google Scholar]
- 2.Japan Industrial Safety and Health Association (2018) General Guidebook on Industrial Health, 2018 version. 22–23, and 43. Japan Industrial Safety and Health Association, Tokyo (in Japanese). [Google Scholar]
- 3.Yamauchi T, Yoshikawa T, Takamoto M, Sasaki T, Matsumoto S, Kayashima K, Takeshima T, Takahashi M. (2017) Overwork-related disorders in Japan: recent trends and development of a national policy to promote preventive measures. Ind Health 55, 293–302. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Japan Society for Occupational Health (2018) Number of certified associate occupational physician. https://ssl.jaoh-caop.jp/roster.html (in Japanese). Accessed October 27, 2018.
- 5.Japan Medical Association (2018) Acquisition and renewal course for certification of occupational physicians. http://jmaqc.jp/sang/guide/index.php (in Japanese). Accessed October 27, 2018.
- 6)Japan Medical Association (2018) Cases counted in the list (2018 version) of Japan Medical Association-certified occupational physicians.
- 7.Ministry of Health, Labour and Welfare, Japan (2016) Special survey on Industrial Safety and Health. https://www.mhlw.go.jp/toukei/list/h28-46–50.html (in Japanese). Accessed November 8, 2018.
- 8.Nakamura H, Isse T, Sakai A. (2017) Changes of working responsibilities and intentions of industrial physicians (Graduates of University of Occupational and Environmental Health, Japan) in a comparison between 2001, 2008 and 2015 questionnaire analyses. J UOEH 39, 47–54. [DOI] [PubMed] [Google Scholar]
- 9.Hino Y, Furuki K, Minami M, Fujishiro K. (2005) Activities of part-time occupational physicians visiting from external occupational health organizations. Occup Health J 28, 75–80. [Google Scholar]
- 10.Terada H, Sone T, Takemura S. (2005) [Study on actual situation of community industrial physicians for small and medium-sized enterprises and their involvement in community occupational health services]. Sangyo Eiseigaku Zasshi 47, 259–68. [DOI] [PubMed] [Google Scholar]
- 11.Kudo Y, Okada M, Tsunoda M, Satoh T, Aizawa Y. (2009) Predictors of Japanese workers’ motivation to use the results of worksite health checkups in their daily health management. Tohoku J Exp Med 219, 231–41. [DOI] [PubMed] [Google Scholar]
- 12.Moriguchi J, Ikeda M, Sakuragi S, Takeda K, Muto T, Higashi T, Weel ANH, van Dijk FJ. (2010) Activities of occupational physicians for occupational health services in small-scale enterprises in Japan and in the Netherlands. Int Arch Occup Environ Health 83, 389–98. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Lalloo D, Demou E, Kiran S, Cloeren M, Mendes R, Macdonald EB. (2016) International perspective on common core competencies for occupational physicians: a modified Delphi study. Occup Environ Med 73, 452–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Persechino B, Fontana L, Buresti G, Rondinone BM, Laurano P, Imbriani M, Iavicoli S. (2016) Professional activity, information demands, training and updating needs of occupational medicine physicians in Italy: National survey. Int J Occup Med Environ Health 29, 837–58. [DOI] [PubMed] [Google Scholar]
- 15.Gallagher F, Pilkington A, Wynn P, Johnson R, Moore J, Agius R. (2007) Specialist competencies in occupational medicine: appraisal of the peer-reviewed literature. Occup Med (Lond) 57, 342–8. [DOI] [PubMed] [Google Scholar]
- 16.Niigata Occupational Health Promotion Center (2012) A survey on occupational health activities desired by part-time occupational physicians and employers. Japan Labour Health and Welfare Organization, Kawasaki, Japan (in Japanese). [Google Scholar]
- 17.Chiba Occupational Health Promotion Center (2011) A survey on activities by active occupational physicians and their circumstances. Japan Labour Health and Welfare Organization, Kawasaki, Japan (in Japanese). [Google Scholar]
- 18.Kumamoto Occupational Health Promotion Center (2005) A survey on activities of occupational physicians in Kumamoto prefecture. Japan Labour Health and Welfare Organization, Kawasaki, Japan (in Japanese). [Google Scholar]
- 19.Moriguchi J, Sakuragi S, Takeda K, Mori Y, Muto T, Higashi T, Ohashi F, Ikeda M. (2013) Activities of private clinic- or hospital-based occupational physicians in Japan. Ind Health 51, 326–35. [DOI] [PubMed] [Google Scholar]
- 20.Ministry of Health, Labour and Welfare, Japan (2015) Mental health measures in workplaces. https://www.mhlw.go.jp/bunya/roudoukijun/anzeneisei12/ (in Japanese). Accessed March 31, 2019.
- 21.Ministry of Health, Labour and Welfare, Japan (2016) Physicians, Dentists and Pharmaceutists Survey. https://www.mhlw.go.jp/toukei/saikin/hw/ishi/16/index.html (in Japanese). Accessed March 31, 2019.
- 22.Japan Medical Association Japan (2018) Report of occupational health committee. http://dl.med.or.jp/dl-med/teireikaiken/20180404_3.pdf (in Japanese). Accessed March 31, 2019.
- 23.Ministry of Health, Labour and Welfare, Japan (2006) Ordinance on Industrial Safety and Health (Article 13–2 amended in 2015). Ministry of Health, Labour and Welfare, the Government of Japan, Tokyo, Japan (in Japanese). [Google Scholar]
- 24.Kagoshima Occupational Health Total Support Center (2014) A study on occupational health activities in small enterprises and their support by occupational health promotion center and regional occupational health center. Japan Labour Health and Welfare Organization, Kawasaki, Japan (in Japanese). [Google Scholar]
- 25.Tsuchiya M, Kawakami N, Ono Y, Nakane Y, Nakamura Y, Fukao A, Tachimori H, Iwata N, Uda H, Nakane H, Watanabe M, Oorui M, Naganuma Y, Furukawa TA, Kobayashi M, Ahiko T, Takeshima T, Kikkawa T. (2012) Impact of mental disorders on work performance in a community sample of workers in Japan: the World Mental Health Japan Survey 2002–2005. Psychiatry Res 198, 140–5. [DOI] [PubMed] [Google Scholar]
- 26.Nagata T, Mori K, Ohtani M, Nagata M, Kajiki S, Fujino Y, Matsuda S, Loeppke R. (2018) Total health-related costs due to absenteeism, presenteeism, and medical and pharmaceutical expenses in Japanese employers. J Occup Environ Med 60, e273–80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Ikonen A, Räsänen K, Manninen P, Rautio M, Husman P, Ojajärvi A, Husman K. (2012) Work-related primary care in occupational health physician’s practice. J Occup Rehabil 22, 88–96. [DOI] [PubMed] [Google Scholar]
- 28.Nakamura H, Isse T, Matsumoto T, Tokura Y. (2009) [Changes of working responsibilities and intentions of industrial physicians who are graduates of University of Occupational and Environmental Health, Japan, in 2001 and 2008 questionnaire analyses]. J UOEH 31, 281–91. [DOI] [PubMed] [Google Scholar]
- 29.Leka S, Griffiths A, Cox T, World Health Organization, Geneva (2004) Work organization and stress. Protecting workers’ health series No. 3. https://www.who.int/occupational_health/publications/en/oehstress.pdf. Accessed April 16, 2019.
- 30.International Labour Office Geneva (2012) Stress prevention at work checkpoints. http://www.ilo.org/wcmsp5/groups/public/—dgreports/—dcomm/—publ/documents/publication/wcms_168053.pdf. Accessed April 16, 2019.
- 31.Leka S, Jain A, Cox T, Kortum E. (2011) The development of the European framework for psychosocial risk management: PRIMA-EF. J Occup Health 53, 137–43. [DOI] [PubMed] [Google Scholar]
- 32.Nagata M, Mori K, Ishikawa A, Nagata T. (2016) Surveys on minimum practical abilities required by nonspecialist occupational physicians in Japan. J Occup Health 58, 276–88. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Cashman C, Slovak A. (2005) The Occupational Medicine agenda: routes and standards of specialization in Occupational Medicine in Europe. Occup Med (Lond) 55, 308–11. [DOI] [PubMed] [Google Scholar]
- 34.Elders L, Burdorf A. (2010) Occupational medicine in The Netherlands. Occup Med (Lond) 60, 314. [DOI] [PubMed] [Google Scholar]
- 35.Matsuda S. (2013) [The occupational physician in France]. J UOEH 35 Suppl, 67–72. [DOI] [PubMed] [Google Scholar]
- 36.Office of Kyoto Prefecture Kyoto (2015) Statistics in Kyoto Prefecture. https://data.pref.kyoto.lg.jp/dataset/260002_tokeisyo0507 (in Japanese). Accessed May 10, 2019.
- 37.Office of Kyoto City (2016) Statistics in Kyoto City. https://data.city.kyoto.lg.jp/node/95905 (in Japanese). Accessed May 10, 2019.
- 38.Ministry of Health, Labour and Welfare, Japan (1975) Industrial Safety and Health Act (Article 13). Ministry of Health, Labour and Welfare, the Government of Japan, Tokyo, Japan (in Japanese). [Google Scholar]
- 39.Office of Kyoto Prefecture Kyoto (2015) Statistics in Kyoto Prefecture. https://data.pref.kyoto.lg.jp/dataset/260002_tokeisyo0506 (in Japanese). Accessed May 10, 2019.
- 40.Office of Kyoto City (2016) Statistics in Kyoto City. http://www2.city.kyoto.lg.jp/sogo/toukei/Publish/Analysis/News/101EconomicCensus2016A.pdf (in Japanese). Accessed May 10, 2019.
- 41.European Foundation for the Improvement of living and Working Condition, Luxembourg (2017) Sixth European Working Conditions Survey. https://www.eurofound.europa.eu/sites/default/files/ef_publication/field_ef_document/ef1634en.pdf. Accessed May 10, 2019.
- 42.Horppu R, Martimo KP, Viikari-Juntura E, Lallukka T, MacEachen E. (2016) Occupational physicians’ reasoning about recommending early return to work with work modifications. PLoS One 11, e0158588. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Doucet T, Muller F, Verdun-Esquer C, Debelleix X, Brochard P. (2012) Returning to work after a stroke: a retrospective study at the Physical and Rehabilitation Medicine Center La Tour de Gassies. Ann Phys Rehabil Med 55, 112–27. [DOI] [PubMed] [Google Scholar]




