Abstract
Objective
The purpose of this paper is to describe the rapid deployment of telehealth, particularly real time video conference, for chiropractic services as a response to COVID-19.
Methods
Two health centers at 2 campuses of a large California corporation have chiropractic care integrated into physical medicine services. Care was suspended beginning on March 17, 2020 to prevent spread of severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) among patients and staff. On March 19, the Governor of California issued a stay at home order. With musculoskeletal problems being common in the employee patient population, telehealth services were quickly developed to continue chiropractic care for patients. Using existing infrastructure, several members of the health center team developed chiropractic telehealth operations within 2 days.
Results
Musculoskeletal telehealth services included examinations, risk assessment, advice, and rehabilitative exercises. These telehealth visits facilitated care that would have otherwise been unavailable to employees. Patients reported that the appointments were helpful, addressed their concerns, and provided a safe method to see their doctor. Regular interprofessional teamwork and relations between the clinic operator and client company were key contributors to operationalizing this service in our integrated healthcare environment.
Conclusion
We were able to quickly implement real time video conferencing and other forms of telehealth for chiropractic services at 2 worksite health centers. This paper includes information and insights to providers about setting up similar telehealth systems so they may also provide this benefit for patients in their communities during pandemics or disasters.
Key Indexing Terms: Chiropractic, Telemedicine, Telecommunications, COVID-19 [Supplementary Concept], Pandemics
Introduction
The coronavirus disease-2019 (COVID-19) pandemic, caused by severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), has driven rapid changes in many areas of healthcare.1 From private practices to multi-disciplinary health centers, providers have witnessed their practices dwindle, or even close.2 Due to the risks of spreading SARS-CoV-2 that are inherent to in-clinic patient care, patients are losing access to health services and healthcare facilities are struggling to maintain patient contact.3 Thus, telehealth is advancing at a speed never thought possible prior to the pandemic.4 Practitioners of musculoskeletal care are turning to telehealth as 1 option to maintain contact with patients.5 , 6
Telehealth is the use of information and telecommunications technologies to support remote health care.7 Previously known as telemedicine, the term telehealth is now preferred when discussing the application of information and telecommunications technologies by multiple disciplines.8 In telehealth, all forms of technology are included that support health care, public health, patient monitoring, and healthcare administration.7 , 9 Telehealth includes real time videoconferencing (RTVC), such as video consultation, video visit, or video encounter. Medicare has traditionally labeled RTVCs as telehealth and uses its own lexicon for other reimbursable services.10 Terminology pertaining to telehealth is broad and in a constant state of flux. A brief glossary of common telehealth terms is provided in Table 1 .
Table 1.
Telehealth terms and definitions essential to implementing telehealth.
| Term | Definition |
|---|---|
| Telemedicine | “The use of telecommunications and information technologies for the provision of medicine at a distance.”9 |
| Telehealth | “Telehealth is a collection of means or methods for enhancing health care, public health, and health education delivery and support using telecommunications technologies.”8 |
| Telerehabilitation | The delivery of rehabilitation services using telehealth technologies, encompassing a range of clinical services from patient evaluation through patient care management.11 |
| Synchronous communication | “A mode of communication where the transfer takes place simultaneously. Examples include real time videoconferencing or standard telephone calls.”9 |
| Real time videoconferencing | An encounter where both parties are available and interacting simultaneously by videoconferencing.9 |
| Asynchronous communication | Communication over a period of time, rather than simultaneously (eg, secure patient messaging, forwarding of imaging results).9 |
| Telecommunications | Transmission and reception of voice, video, or other data over a distance. Telecommunications can be from one person to another or broadcast from one person to many people.9 |
We are unaware of any papers published about the use of telehealth for chiropractic care. Papers on telehealth in worksite health centers (WSHCs) are rare.12 We only found 1 study, which described the use of telehealth for a variety of concerns seen by primary care providers in a WSHC.12
Some evidence is available from other health professions in non-worksite health center environments and we are applying it to chiropractic practice in our WSHCs, however there are no reports about chiropractic use. During this time of the COVID-19 pandemic, there is an urgent need for telehealth to reduce potential exposure of health care workers and patients to SARS-CoV-2. Therefore, the purpose of this paper is to describe the rapid deployment of remote musculoskeletal care through telehealth, particularly using real time video conferencing, for chiropractic services integrated in 2 health centers located on 2 campuses of a large company in California.
Methods
Ethics
This is a descriptive report of how we transitioned from in-clinic to telehealth care during the COVID-19 pandemic. Thus, this is a retrospective description of clinical operations. It is not a prospective experiment, nor does it report information on human subjects. Therefore, this report did not require institutional review board review.
Setting
The 2 WSHCs reported here are in California, located 450 miles apart, and are operated by Stanford Health Care (SHC). SHC is a large university-based healthcare system that provides a full spectrum of primary care and specialty healthcare services. SHC includes an Employer Based Integrated Primary Care Health Centers unit, which operates several WSHCs for client companies in California. WSHCs are clinics where employees, and sometimes the dependents of employees, have access to a variety of health care services at or near the workplace of the employees.13 , 14 Some of these WSHCs include chiropractic.15 , 16 These partnerships allow for the development of environments to try various integrated care and value-based care models. Thus, clinic services, outreach programs, health center hours of operation, and other logistics are influenced by collaboration between SHC and its client businesses. Thus, rapid transitions and innovations in care are often possible.
Response to the COVID-19 Pandemic
The first case of SARS-CoV-2 in California, which was the third case in the US, was reported on January 26, 2020.17 Five days later, the seventh nationwide case was reported in the county of 1 of our WSHCs and the first US COVID-19 fatality occurred on February 6, 2020 in this same county.18 The incidence of COVID-19 was increasing rapidly in the counties of both WSHCs. By March 12, 2020, the client company issued guidance for employees to work from home. The WSHCs continued to remain open for routine care; however, with the briskly changing COVID-19 status, WSHC leadership and staff considered how the pandemic might change employee access to the clinic.
Musculoskeletal disorders are common in the employee population served by the WSHCs and there was an ongoing need for care of these concerns. Many employees often worked from home before the pandemic. However, as employees switched to working at home on a full-time basis, they began to report new musculoskeletal concerns, associating them with increased work and personal stress, restraints on physical activity options, and working in awkward positions in home environments not always set up for computer work. However, there were public health and ethical implications to consider with maintaining in-clinic care during a pandemic of a deadly disease with rapidly rising incidence. We faced the reality of losing contact with established patients and not being accessible to new patients. The nexus of our original mission of serving the employees in an integrated onsite primary care health center in the midst of a public health crisis that did not allow employees to come onsite created an opportunity to re-think how we delivered care.
On March 17, we held the first of several meetings to integrate RTVC for chiropractic care. RTVC had never been attempted for chiropractic at either of the WSHCs. However, to continue serving the employees during the crisis, rapid deployment of RTVC was necessary. There were 3 distinct challenges to operationalizing remote RTVCs: (1) the chiropractors had to conduct their part of the visits from their homes; (2) the patients had to access visits from home; and (3) there was no direct contact with the interprofessional provider team, health center management, or technical support. It all had to be done by remote means.
On March 18, to prevent spread of the virus between patients and health center staff, clinic operations changed. In-clinic care for chiropractic, acupuncture, optometry, nutrition, diabetes education, and behavioral health were suspended, and the providers were directed to stay at home. Services for primary care were reduced and physical therapy was limited to post-surgical cases that required in-clinic care. The next day, when the statewide number of cases exceeded 1000,19 the Governor of California declared a state of emergency and a statewide shelter-in-place/stay-at-home order.20
Preparation
Because the WSHCs are operated by SHC, much infrastructure was already in place that allowed for rapid change. Telehealth services (eg, secure patient messaging, electronic health record, patient scheduling, and records app) were already in use by all WSHC providers. However, the dietician and diabetes prevention training team were the only providers frequently using RTVC. Thus, with these operations already supported by an information technology (IT) field service technician dedicated to assist the WSHCs, we were able to prepare quickly.
Computers with HIPPA compliant security requirements and remote synchronous video capacity were obtained from the IT department the same day that the decision was made to offer chiropractic RTVCs. It was a requirement for each computer to have access to the existing electronic health record (EHR) and for the RTVC to be integrated in a secure EHR platform. To test that the video, audio, and EHR systems worked reliably, we rehearsed RTVCs using mock patients that were integrated into the EHR. The IT field technician played the role of the mock patient and we conducted the visit live with the technician. We then created EHR documentation templates specifically for RTVC that included documentation that the encounter was a video visit (vs in-clinic), clinical notes, and proper telehealth coding.
We equipped our remote offices for the RTVC with the secure computer, proper lighting, backgrounds free of clutter and professional in appearance, educational materials, and improvised home rehabilitation equipment. With more than 1 person working remotely in each of our homes, we staggered videoconferences, teleconferences, and RTVCs to avoid crosstalk and privacy violations. The use of headsets with microphones and earphones helped reduce voice volume and speaker noise to avoid interrupting others in the home environment.
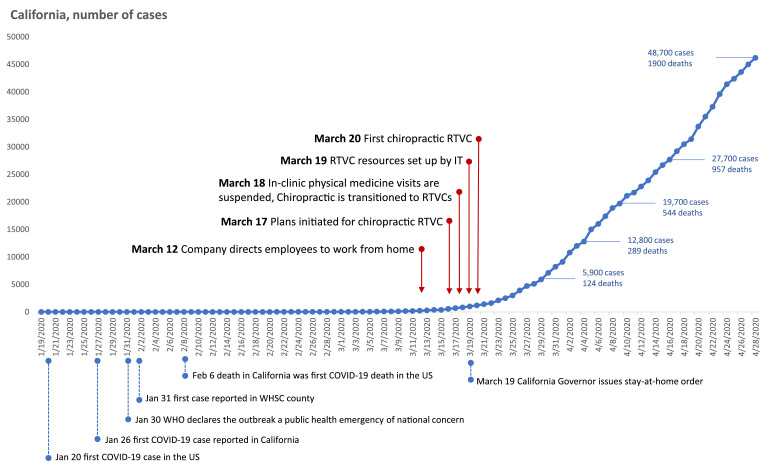
We set up and tested the infrastructure and were ready for remote patient visits within 2 days at 1 health center and 7 days at the other. The first RTVCs with patients began 20 March. As can be seen in Figure 1 , the deployment of RTVC for chiropractic care was completed just in time, right before the Governor's stay at home order and a sharp rise in COVID-19 cases in the state.
Fig 1.
Timeline of key events in the deployment of real time videoconferencing (RTVC) with patients. WSHC, worksite health center; WHO, World Health Organization.
Communication with the Client Company, Patients, and Staff
Our interprofessional colleagues at the WSHCs were accustomed to relying upon chiropractic services for onsite care. However, given the hands-on nature of chiropractic treatment, how chiropractic could be successfully implemented through RTVC was not clear to these providers or the supporting staff and clinic managers. Therefore, we developed informative materials that explained that the chiropractic clinical encounter usually includes many processes in addition to hands-on assessment and treatment. For RTVC we would use all procedures except for manual ones. Thus, like clinical encounters in primary medical care, many procedures for chiropractic would be done through telehealth. We communicated information about the ability to offer chiropractic care through RTVC during morning all-staff brief telemeetings, personal e-mail, telephone calls, and e-mail sent to all providers. Providers gave us feedback that this was helpful for them to understand how chiropractic care through telehealth could be achieved.
The client company informed the workforce what services were available for care. Information pertaining to these services, how to access care, hours of operation, and advice regarding symptoms of COVID-19 were periodically sent to employees by the company and SHC.
The chiropractors and clinic managers helped to develop the information that the telephone schedulers needed to triage patients for appointments. This included information that chiropractic visits were being held by RTVC, what patients could expect, and how to prepare for a video encounter. The information included that RTVCs were being used for public health reasons, that RTVCs could be helpful in assisting with musculoskeletal problems, and that many parts of the typical in-clinic visit could be accomplished via RTVC. The script for the schedulers included instructions on accessing the SHC smartphone patient portal app to access the video service, how to test the app and hardware, how to log in to the RTVC appointment, and to have a California identification card ready to show to the chiropractor. Patients could also self-schedule using the EHR app and these instructions were included in the app.
Results
The following is a description of the workflow we use for the typical chiropractic RTVC.
Administrative Tasks
The patient enters the RTVC by using the EHR app on the smart phone or computer and may do so up to 5 minutes prior to the appointment. On our EHR screen, a video icon illuminates, indicating that the patient has entered the RTVC. We can then enter the appointment by clicking the icon. Then, a screen with live video of the patient and provider opens in the EHR. When we connect with the patient, we first obtain the telephone number of the patient in case of technical difficulties, dropped video connection or audio problems.
We then check the patient in to the visit, verify 2 patient identifiers, check a photo identification, and verify that the patient is physically in the state where we are licensed to practice, thereby satisfying jurisdictional regulations. After we review with the patient the limitations and benefits of video visits, verbal consent is obtained from the patient that he or she agrees to have the health care visit via RTVC. The visit then continues according to the patient's needs.
Clinical History
We perform a standard history of the present complaint. Other applications that we have found useful include the following. We conduct health behavior risk assessment for home ergonomics and physical activity. We assess compliance with home exercise plans (if this is a return patient). We query regarding social distancing practices. We examine the patient's at-home computer ergonomics remotely using the patient's smart phone or laptop computer camera. Since we are virtually in the patient's home environment and can see the physical setting of the patient's work, we feel that we can obtain more accurate ergonomics information than we do during an in-clinic encounter.
Examination
The physical examination has been modified to accommodate the virtual encounter. Posture is assessed by asking the patient to step back from the camera so that we may view body habitus remotely. Specific areas of concern per body region are visually assessed for discoloration or swelling by having the patient bring the camera close to the painful area. Palpation for pain assessment is conducted by having the patient point to the areas that hurt and then press on them to inform us how much tenderness they experience. Active ranges of motion and movements of directional preference are visually assessed. Many provocative or orthopedic tests are performed by having the patient actively do them with demonstration or verbal guidance. Heel walk and toe walk are assessed visually and upper extremity myotomes are accomplished by instructing the patient how to perform them on themselves by using the opposite hand. Evaluation for sensory functions, such as light touch, are performed by having the patient lightly touch the area of concern and compare it to the opposite side and report back what they feel.
Report of Findings and Treatment
Following the history and examination for new complaints, we proceed with a report of findings. We explain to the patient what we have found, the working diagnosis, a suggested treatment plan and what they will be doing to actively participate in their care. We describe the potential benefits and risks of treatment. We then obtain consent for the next appropriate clinical steps, as is standard practice. We then proceed with providing additional education or referrals if necessary.
For treatment within the context of telehealth, prescribing therapeutic exercises requires creativity and innovation. Typically, we explain the exercises, demonstrate them to the patient, and then have the patient demonstrate the exercises back to us to confirm that they have learned them. With the 2-dimensional nature of video, we have found that the exercises need to be demonstrated by both the chiropractor and the patient in at least 2 angles (eg, front and side). For exercises requiring resistance, if elastic exercise bands are unavailable to the patient, we suggest using towels, canned or bagged food (eg, soup cans or flour).
Before the end of the encounter, the treatment plan is reviewed and the frequency of future appointments is agreed upon. Following the completion of each encounter, we send the patient a review of self-care instructions and home exercises by using the secure patient messaging system contained within the EHR. These messages are immediately sent to the patient and may be obtained by them on their computer or smart phone. We then notify the scheduling staff by secure email or secure instant messaging to call the patient and schedule them according to the agreed upon treatment plan. Alternatively, the patient may self-schedule using the app.
Documentation
We record the patient encounter in the EHR after the visit is complete to help us avoid the distraction of typing into the EHR while talking with the patient. Thus, we write notes on a “scribble sheet” from the Washington University Department of Internal Medicine.21 Once the RTVC is complete, we refer to our “scribble sheet” as we enter our notes into the EHR template. In our EHR documentation, we use 2 forms of consent. One is that the patient consents to have the visit using RTVC. The second is informed consent regarding treatment. Also, in our documentation, we record how procedures are performed if the methods are different than what we typically use in the clinic. For example, if palpation is performed, we record that we ask the patient to touch the area of concern and describe the pain they experience.
Discussion
To the authors’ knowledge, this is the first published description of the use of chiropractic telehealth and the use of telehealth for musculoskeletal care in a WSHC. Given the lack of peer-reviewed journal articles about these topics and the current pandemic of COVID-19, we feel that this report is timely and hope that others transitioning to telehealth will find this paper helpful.
We perceive that the video visits seem to be effective in providing time for case management and patient education. Patients who participate in the RTVCs comment that they like these encounters, feel that they are helpful, and we are able to address their concerns. Our experience with patient satisfaction is consistent with the literature on rehabilitation via telehealth22, 23, 24 and with what has been shown in studies in several countries.24 This literature includes the US and India,25 , 26 both of which represent large segments of the workforce we serve. With respect to precautions related to the COVID-19 pandemic, the patients are grateful that there is an option for care that does not involve the health risks that might be associated with attending an in-clinic visit or urgent care facility.
The setting and context of the WSHC environment is a key part of how we have operationalized the use of chiropractic RTVCs. The interprofessional collaborative team that staffs the health center greatly facilitates the ability to transition rapidly from in-clinic care to RTVCs. The providers have a regular practice of working as a team. The schedulers, medical assistants, nurses, clinic managers, and other staff are adept at providing support to the providers and to one another. Thus, this interprofessional collaboration is the foundation for the ability to move to full telehealth and maintain a sense of cohesion amongst the staff and providers. Further, the entire WSHC team already employs various modalities of telehealth in daily operations, although RTVC was least used until the pandemic.
For musculoskeletal services, primary care relies heavily on the physical medicine team, which at our locations includes physical therapists, chiropractors, and acupuncturists, who provide the bulk of musculoskeletal services. While the decision was made to suspend in-clinic physical medicine care, acute walk-in patients were still able to be seen by the primary care provider on-site each day. At this time, chiropractic care remains available through all telehealth modalities for referrals from other providers and direct access. Physical therapy has also transitioned to RTVC for returning patient visits.
The client company and SHC work closely together to promote the health of the entire workforce in addition to individual patients. Because of this, certain barriers to telehealth were lowered and this was critical to success. First, the company encouraged us to contact the entire workforce population, including those that were current patients and those who did not yet use the health center. This capacity to contact the entire community we serve was essential to inform people that WSHC services remained open. Because the company is self-insured, barriers to telehealth reimbursement were lowered. The company encouraged us to implement telehealth to provide care, which reduced problems that are often associated with reimbursement coding for telehealth. Finally, SHC contracts with the client company to provide services. Care was not provided on a fee-for-service basis and providers were paid on a salary or contract basis. The client and SHC agreed to keep all providers on staff during the difficult times of COVID-19 pandemic, reducing anxiety amongst staff. We feel this engendered the capacity to be creative in our approach to deploying RTVC for chiropractic care.
Applications and Recommendations
Since beginning the use of telehealth at our location, we continue to gather information to help inform this process. Here we share protocols and recommendations, such as those recommended by the American Telemedicine Association's principles for delivering telerehabilitation services.11 To effectively and legally implement video visits, one must consider several requirements. We recommend A Blueprint for Telerehabilitation Guidelines by Brennen and colleagues of the Association, which is a comprehensive guide to providing effective and safe services.27 This guide may be helpful for practitioners in private practice settings where there may be no experts in IT or telehealth on staff. We have outlined several potential problems associated with video visit delivery and associated solutions to assist others in implementing video-based care (Table 2 ).4 , 21 , 28, 29, 30, 31
Table 2.
Barriers and potential solutions to video-based care
| Barrier | Solution |
|---|---|
| Privacy laws and relation to video visits | The US Department of Health and Human Services recently relaxed HIPAA compliance guidelines for the COVID-19 pandemic.28 Consult state and national organizations for further guidance in your jurisdiction. |
| Video communication programs | Free or low cost apps exist for use on computers and smart phones.29 |
| Secure video telehealth | To prevent an outside party from inadvertently joining the patient encounter, use all available security features of the video platform including a unique link for each appointment and password protection. A valid and reliable telehealth security self-assessment questionnaire is available and very useful.30 |
| Potential malpractice litigation | Contact your professional liability carrier to see if telehealth is covered under your policy. |
| Reimbursement | For providers of all types, how and for how much telehealth will be reimbursed during the COVID-19 pandemic is an unknown and varies from region to region depending on insurance providers. For more details regarding chiropractic care, consider information available from NCMIC Group.31 |
| Service and coding terminology is confusing | Magoon provides a helpful table that compares various telehealth modalities in Medicare terms, elements of service necessary to define each, and a convenient algorithm to determine which service to code.10 |
| There is a learning curve for the provider and staff when implementing telehealth | Have patience, conduct staff training, and develop protocols. Assume that anything involving new technology will have problems. Plan for at least 1 back up, if not 2 backup plans, in case something fails. |
| It is difficult to focus on the patient's concerns and exam and enter data into the EHR simultaneously. | A “scribble sheet” from the Washington University Department of Internal Medicine21 is helpful in patient communication and encounter documentation. This is freely available and can easily be modified for chiropractic practice. |
| It is hard to make a specific diagnosis by video | This may be the case. However, making a specific diagnosis in person is not always attained because there may need to be a therapeutic trial or more tests may be necessary. This can be discussed frankly with the patient; in our experience patients are appreciative of the discussion and willing to accept the limitations of the video visit. Obtain the information that allows you to move ahead with patient management. As 2 authors remarked, “Focusing on actionable information is more important than diagnostic accuracy.”4 |
| My office does not have a script for schedulers to use in communicating with patients about COVID-19 | Schmidt has shared 1 for both new and returning patients that is highly relevant to standard office procedures.21 |
| It might be difficult to triage patients with potential systemic problems using telehealth | Immediate practice-relevant protocols and practice aids are available open-access from Washington University Department of Internal Medicine.21 This is also a good time to reach out to local medical doctors, many of whom are also setting up telehealth practices, if referral consultations are needed. |
Evidence does exist to address the validity of the telehealth examination for musculoskeletal concerns.32 Although there is not a plethora of high level evidence, there is some support from the scientific literature. For patients with musculoskeletal concerns and chronic pain, 2 of the primary problems addressed by chiropractors, both have evidence supporting the use of telehealth for patient care.24 , 33 , 34 Telehealth methods for ergonomic evaluation are supported by the American Occupational Therapy Association and other reports.35, 36, 37 Postural examination has been shown to possess good levels of concordant validity with in-person assessment.32 Active range of motion virtual assessment is supported by good levels of concordant validity with in-person assessment. Telehealth assessment of directional movement preference for assessment and treatment of low back pain has been shown to be equally as effective as in-person observation.38 According to a recent study, research regarding the validity of the virtual general physical examination is limited.39 However, Cottrell and colleagues have demonstrated that a high level of agreement exists between telehealth and in-person assessments for clinical decisions and diagnosis of patients with chronic musculoskeletal conditions and that telehealth may be considered an effective method of assessment.40
We have found some practical limitations to examination procedures during RTVC. For example, some provocative or orthopedic tests are unable to be performed. Also, muscle stretch reflexes, procedures requiring resisted muscle testing, and passive range of motion testing are limited within the telehealth visit. However, the neuromuscular examination procedures that may be delivered via RTVC are still sufficient for the majority of RTVC encounters in musculoskeletal practice.
Considerations for the Future
While we had not used remote video-based chiropractic care before the COVID-19 pandemic, we feel that it will likely occupy a valuable place in our clinical care in the future. The company that we serve has a diverse workforce that is located throughout the US and the world. Given the high global prevalence and burden of musculoskeletal problems, particularly spine disorders,41 there exists significant opportunity to provide care to a much larger segment of the workforce.
In our experience, chiropractic by telehealth is feasible. Real-time telerehabilitation appears to be effective and comparable to conventional methods of healthcare delivery for the improvement of physical function and pain in a variety of musculoskeletal conditions.24 It has already been reported in the areas of spine pain, chronic pain, and a variety of musculoskeletal disorders,38 , 42, 43, 44, 45, 46, 47 which are common in chiropractic practice. Telehealth has enabled us to maintain continuity of care with our patients and we plan on further enabling RTVC as a valuable tool.
Using telehealth as a first step in seeking health care is a concept gaining popularity with the COVID-19 pandemic. Changes in care pathways made during this time may not revert to normal after this pandemic. It is possible that these new access pathways will become the convention and the strategy upon which other points of care are built. For interprofessional clinics, this could open an opportunity for chiropractors and other musculoskeletal experts to provide triage for musculoskeletal problems via telehealth. This can direct patients to the right care at the right time and lighten the load of primary care providers.
We will be looking at video visits in the future to save time for patient visits that do not require manual therapy or other in-person assessment or care. By better deploying telehealth, we may be able to improve access to care for these patients. This may indirectly improve access to care for patients requiring in-clinic care.
One reason client companies have WSHCs is to reduce lost work time and productivity.15 , 48 While the convenience and location of the WSHC on campus helps to reduce lost work time, video visits may reduce that further. Informal surveys performed at our WSHC have found that if a patient travels off site for a health care appointment, it takes about 2 hours from the time they leave the facility until they return. Yet, the appointment rarely lasts more than 15 minutes. This is supported by studies done elsewhere.49 We may be able to leverage our telehealth capacities to further reduce lost work time. Working from home may continue at a prevalence higher than it was before the pandemic and RTVC may continue to serve the workforce in this capacity.
We find RTVCs for chiropractic care to be feasible, enjoyable, and patients seem to like them. Deploying RTVC requires infrastructure, patience, and organization, which can be implemented at some level in many practice environments. From the COVID-19 crisis we are learning much about our capacity to reach patients that would otherwise not receive care and it is stimulating us to be creative in several ways. We look forward to our future in using RTVCs. Telehealth does not replace good health care, but it can facilitate it. As recently stated by 2 telehealth innovators, “Disasters and pandemics pose unique challenges to health care delivery. Though telehealth will not solve them all, it's well suited for scenarios in which infrastructure remains intact and clinicians are available to see patients.”50 We agree.
Future Research
Future research in this area can inform our knowledge about the use of telehealth in chiropractic practice. The application and effectiveness of telehealth has been reported in several specialties, such as neurology, radiology, stroke care, traumatic brain injury management, cardiac rehabilitation, and others.42 , 44 , 51 Since it has not been reported in chiropractic, this represents fertile grounds for research with immediate practice relevance. The rate of use and preferences of the chiropractic population for telehealth are unknown. Having such knowledge could enable chiropractors to provide video care to the patients most likely to benefit from it and be more effective in practice. Cross-sectional studies of conditions seen and treatments rendered via RTVC chiropractic would help inform the profession of the potential capacity of this communication modality. While we found anecdotally that our patients who use RTVCs liked them, there are no data on satisfaction rates with this approach to chiropractic care. This would be valuable in designing programs that best meet patient expectations. Finally, research that investigates what components of the clinical encounter should and should not be used in video-based visits would be highly relevant to practice.
Limitations
This paper is a descriptive report. Our findings may not necessarily be generalized to other locations or replicated by chiropractors or other physical medicine providers in other settings. Some of the processes and resources were already present in our system and these resources may be different from what are found in other practices. This report represents just a snapshot in time. The situation with the COVID-19 pandemic continues to change. Therefore, the response that we describe here will likely evolve both with the expansion of telehealth and the passage of laws pertaining to telehealth. What we report here may not be legally allowable in other regions or jurisdictions. We recommend that anyone wishing to implement telehealth consult with their regional experts for advice.
Conclusion
Confronted with the rising public health problem of the COVID-19 pandemic, government stay-at-home orders, and a decision to suspend physical medicine care, we faced the reality of losing contact with established patients and not being accessible to new ones. With a patient population with many musculoskeletal disorders, we had to re-think how we delivered care. We decided to offer chiropractic care via telehealth, which we rapidly deployed within 1 week. We have reported on how we developed and delivered chiropractic telehealth for musculoskeletal care integrated in 2 worksite health centers. Along the way we discovered some barriers and found solutions to implementing and sustaining telehealth for chiropractic services and have shared those resources.
Acknowledgements
We thank Diana Felix, MBA for her review of this paper and assistance with facilitating its completion.
Funding Sources and Conflicts of Interest
The authors received no funding for this study. The views and opinions expressed in this paper are those of the authors and do not necessarily reflect the official policy or position of any agency, educational institution, or association (eg, National University of Health Sciences, Stanford University, or Stanford Health Care). Author BNG is the JMPT Associate Editor; however, he received no directive or remuneration for this paper. No other conflicts of interest were reported.
Contributorship Inforamtion
Concept development (provided idea for the research): B.N.G., T.P., L.K.
Design (planned the methods to generate the results): B.N.G.
Supervision (oversight, organization and implementation, writing of the manuscript): B.N.G.
Literature search (performed the literature search): B.N.G., T.P.
Writing (responsible for writing a substantive part of the manuscript): B.N.G., T.P., J.R.P.
Critical review (revised manuscript for intellectual content, this does not relate to spelling and grammar checking): B.N.G., T.P., L.K., J.R.P.
Practical Applications.
-
•
This paper describes the rapid implementation of real time video conferencing for chiropractic services at 2 worksite health centers.
-
•
A typical workflow for the chiropractic RTVC is provided.
-
•
We provide information about setting up similar telehealth systems so they may also provide this benefit for patients in their communities during pandemics or disasters.
Alt-text: Unlabelled box
References
- 1.Kamerow D. Will covid-19 change US healthcare for the better? BMJ. 2020;369:m1784. doi: 10.1136/bmj.m1784. [DOI] [PubMed] [Google Scholar]
- 2.Primary Care Collaborative. Quick COVID-19 Primary Care Survey: Series 5.https://www.pcpcc.org/sites/default/files/news_files/C19%20Series%205%20National%20Executive%20Summary.pdf. Published April 23, 2020. Accessed April 17, 2020.
- 3.Primary Care Collaborative. Quick COVID-19 Primary Care Survey: Series 7.https://www.pcpcc.org/sites/default/files/news_files/C19%20Series%205%20National%20Executive%20Summary.pdf. Published April 30, 2020. Accessed April 27, 2020.
- 4.Hollander JE, Sites FD. The transition from reimagining to recreating health care is now. NEJM Catalyst. 2020;8 doi: 10.1056/CAT.20.0093. [DOI] [Google Scholar]
- 5.Sarsak HI. Telerehabilitation services: A successful paradigm for occupational therapy clinical services? Int Phys Med Rehabil J. 2020;5(2):93–98. [Google Scholar]
- 6.Turolla A, Rossettini G, Viceconti A, Palese A, Geri T. Musculoskeletal Physical Therapy During the COVID-19 Pandemic: Is Telerehabilitation the Answer? Phys Ther. 2020 doi: 10.1093/ptj/pzaa093. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.HealthIT.gov. Telemedicine and Telehealth. US Department of Health and Human Services.https://www.healthit.gov/topic/health-it-initiatives/telemedicine-and-telehealth. Published September 28, 2017. Accessed April 9, 2020.
- 8.California Telehealth Resource Center. What is telehealth? California Telehealth Resource Center. Available from: caltrc.org/telehealth/what-is-telehealth. Published April 4, 2020. Accessed April 4, 2020.
- 9.Johnston B, Alvarez I, Allen D, Fowler S. California Telemedicine & eHealth Center; Sacramento: 2006. A Glossary of Telemedicine and eHealth. [Google Scholar]
- 10.Magoon V. Operationalizing virtual visits during a public health emergency. Fam Pract Manag. 2020;27(3):5–12. [PubMed] [Google Scholar]
- 11.Richmond T, Peterson C, Cason J. American Telemedicine Association's Principles for Delivering Telerehabilitation Services. Int J Telerehabil. 2017;9(2):63–68. doi: 10.5195/ijt.2017.6232. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Varkey P, Schumacher K, Swanton C, Timm B, Hagen PT. Telemedicine in the work site: a study of feasibility, and patient and provider satisfaction. J Telemed Telecare. 2008;14(6):322–325. doi: 10.1258/jtt.2008.080512. [DOI] [PubMed] [Google Scholar]
- 13.Brugh V, McCarthy M. Employer-sponsored medical clinics: Much more than convenience care. Benefits Q. 2014;1st Quarter:19–24. [Google Scholar]
- 14.Fuld & Company . Fuld & Company; Cambridge: 2009. The Growth of On-Site Health Clinics. [Google Scholar]
- 15.Kindermann SL, Hou Q, Miller RM. Impact of chiropractic services at an on-site health center. J Occup Environ Med. 2014;56(9):990–992. doi: 10.1097/JOM.0000000000000215. [DOI] [PubMed] [Google Scholar]
- 16.Lord DJ, Wright JR, Fung R. Integrated Physical Medicine at Employer-Sponsored Health Clinics Improves Quality of Care at Reduced Cost. J Occup Environ Med. 2019;61(5):382–390. doi: 10.1097/JOM.0000000000001536. [DOI] [PubMed] [Google Scholar]
- 17.Wheeler I. Orange County coronavirus patient released, in good condition, health officials say. The Orange County Register.https://www.ocregister.com/2020/2002/2004/risk-of-catching-coronavirus-in-so-cal-is-low-health-officials-say/. Published February 4, 2020. Accessed April 23, 2020.
- 18.Hanna J, Moon S, Stella Chan. 2 Californians died of coronavirus weeks before previously known 1st US death. CNN. April 22, 2020: https://www.cnn.com/2020/2004/2022/us/california-deaths-earliest-in-us/index.html.
- 19.Newsom G, Executive Department State of California . N-33-20. Office of the Governor; Sacramento: March 19, 2020. Executive Order.https://covid19.ca.gov/img/Executive-Order-N-33-20.pdf Available from: [Google Scholar]
- 20.California Department of Public Health. State Officials Announce Latest COVID-19 Facts. The Department; 2020. https://www.cdph.ca.gov/Programs/OPA/Pages/NR20-028.aspx. Published March 20, 2020. Accessed April 12, 2020.
- 21.Schmidt JM. Seeking evidence-based COVID-19 preparedness: A FEMA framework for clinic management. NEJM Catalyst. 2020 https://catalyst.nejm.org/doi/full/10.1056/CAT.1020.0079?cid=DM89279_NEJM_COVID-89219_Newsletter&bid=175085410 in press:Available from: [Google Scholar]
- 22.Kairy D, Tousignant M, Leclerc N, Cote AM, Levasseur M, Researchers TT. The patient's perspective of in-home telerehabilitation physiotherapy services following total knee arthroplasty. Int J Environ Res Public Health. 2013;10(9):3998–4011. doi: 10.3390/ijerph10093998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Kairy D, Lehoux P, Vincent C, Visintin M. A systematic review of clinical outcomes, clinical process, healthcare utilization and costs associated with telerehabilitation. Disabil Rehabil. 2009;31(6):427–447. doi: 10.1080/09638280802062553. [DOI] [PubMed] [Google Scholar]
- 24.Cottrell MA, Galea OA, O'Leary SP, Hill AJ, Russell TG. Real-time telerehabilitation for the treatment of musculoskeletal conditions is effective and comparable to standard practice: a systematic review and meta-analysis. Clin Rehabil. 2017;31(5):625–638. doi: 10.1177/0269215516645148. [DOI] [PubMed] [Google Scholar]
- 25.Davis LE, Coleman J, Harnar J, King MK. Teleneurology: successful delivery of chronic neurologic care to 354 patients living remotely in a rural state. Telemed J E Health. 2014;20(5):473–477. doi: 10.1089/tmj.2013.0217. [DOI] [PubMed] [Google Scholar]
- 26.Ganapathy K. Telemedicine and neurosciences. Neurol India. 2018;66(3):642–651. doi: 10.4103/0028-3886.232346. [DOI] [PubMed] [Google Scholar]
- 27.Brennan DM, Tindall L, Theodoros D. A blueprint for telerehabilitation guidelines–October 2010. Telemed J E Health. 2011;17(8):662–665. doi: 10.1089/tmj.2011.0036. [DOI] [PubMed] [Google Scholar]
- 28.US Department of Health and Human Sciences . The Department; Washington, DC: 2020. Notification of Enforcement Discretion for Telehealth Remote Communications During the COVID-19 Nationwide Public Health Emergency.https://www.hhs.gov/hipaa/for-professionals/special-topics/emergency-preparedness/notification-enforcement-discretion-telehealth/index.html Available from: HHS.gov. [Google Scholar]
- 29.Calton B, Abedini N, Fratkin M. Telemedicine in the time of coronavirus. J Pain Symptom Manage. 2020 doi: 10.1016/j.jpainsymman.2020.03.019. in press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Zhou L, Thieret R, Watzlaf V, Dealmeida D, Parmanto B. A telehealth privacy and security self-assessment questionnaire for telehealth providers: Development and validation. Int J Telerehabil. 2019;11(1):3–14. doi: 10.5195/ijt.2019.6276. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Gwilliam E. Billing for Telemedicine in Chiropractic. NCMIC Group Inc.https://www.ncmic.com/learning-center/articles/risk-management/operational-staff-risks/billing-for-telemedicine-in-chiropractic/. Published October 30, 2019. Accessed April 9, 2020
- 32.Truter P, Russell T, Fary R. The validity of physical therapy assessment of low back pain via telerehabilitation in a clinical setting. Telemed J E Health. 2014;20(2):161–167. doi: 10.1089/tmj.2013.0088. [DOI] [PubMed] [Google Scholar]
- 33.Adamse C, Dekker-Van Weering MG, van Etten-Jamaludin FS, Stuiver MM. The effectiveness of exercise-based telemedicine on pain, physical activity and quality of life in the treatment of chronic pain: A systematic review. J Telemed Telecare. 2018;24(8):511–526. doi: 10.1177/1357633X17716576. [DOI] [PubMed] [Google Scholar]
- 34.Herbert MS, Afari N, Liu L. Telehealth versus in-person acceptance and commitment therapy for chronic pain: A randomized noninferiority trial. J Pain. 2017;18(2):200–211. doi: 10.1016/j.jpain.2016.10.014. [DOI] [PubMed] [Google Scholar]
- 35.American Occupational Therapy Association Telehealth in Occupational Therapy. Am J Occup Ther. 2018;72(Supplement_2) 7212410059p7212410051-7212410059p7212410018. [Google Scholar]
- 36.Baker N, Jacobs K. Telerehabilitation. In: Kumar S, Cohn ER, editors. Health Informatics. Springer; London; New York: 2013. pp. 163–174. [Google Scholar]
- 37.Backman CL, Village J, Lacaille D. The ergonomic assessment tool for arthritis: development and pilot testing. Arthritis Rheum. 2008;59(10):1495–1503. doi: 10.1002/art.24116. [DOI] [PubMed] [Google Scholar]
- 38.Mbada CE, Olaoye MI, Dada OO. Comparative efficacy of clinic-based and telerehabilitation application of Mckenzie therapy in chronic low-back pain. Int J Telerehabil. 2019;11(1):41–58. doi: 10.5195/ijt.2019.6260. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Ansary AM, Martinez JN, Scott JD. The virtual physical exam in the 21st century. J Telemed Telecare. 2019 doi: 10.1177/1357633X19878330. 1357633X19878330. [DOI] [PubMed] [Google Scholar]
- 40.Cottrell MA, O'Leary SP, Swete-Kelly P. Agreement between telehealth and in-person assessment of patients with chronic musculoskeletal conditions presenting to an advanced-practice physiotherapy screening clinic. Musculoskelet Sci Pract. 2018;38:99–105. doi: 10.1016/j.msksp.2018.09.014. [DOI] [PubMed] [Google Scholar]
- 41.March L, Smith EU, Hoy DG. Burden of disability due to musculoskeletal (MSK) disorders. Best Pract Res Clin Rheumatol. 2014;28(3):353–366. doi: 10.1016/j.berh.2014.08.002. [DOI] [PubMed] [Google Scholar]
- 42.Galea MD. Telemedicine in rehabilitation. Phys Med Rehabil Clin N Am. 2019;30(2):473–483. doi: 10.1016/j.pmr.2018.12.002. [DOI] [PubMed] [Google Scholar]
- 43.Howard IM, Kaufman MS. Telehealth applications for outpatients with neuromuscular or musculoskeletal disorders. Muscle Nerve. 2018;58(4):475–485. doi: 10.1002/mus.26115. [DOI] [PubMed] [Google Scholar]
- 44.Tenforde AS, Hefner JE, Kodish-Wachs JE, Iaccarino MA, Paganoni S. Telehealth in physical medicine and rehabilitation: A narrative review. PM R. 2017;9(5S):S51–S58. doi: 10.1016/j.pmrj.2017.02.013. [DOI] [PubMed] [Google Scholar]
- 45.Cottrell MA, Hill AJ, O'Leary SP, Raymer ME, Russell TG. Clinicians' perspectives of a novel home-based multidisciplinary telehealth service for patients with chronic spinal pain. Int J Telerehabil. 2018;10(2):81–88. doi: 10.5195/ijt.2018.6249. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Gialanella B, Ettori T, Faustini S. Home-based telemedicine in patients with chronic neck pain. Am J Phys Med Rehabil. 2017;96(5):327–332. doi: 10.1097/PHM.0000000000000610. [DOI] [PubMed] [Google Scholar]
- 47.Amorim AB, Pappas E, Simic M. Integrating mobile-health, health coaching, and physical activity to reduce the burden of chronic low back pain trial (IMPACT): A pilot randomised controlled trial. BMC Musculoskelet Disord. 2019;20(1):71. doi: 10.1186/s12891-019-2454-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Mercer LLC; New York: 2018. Worksite Medical Clinics 2018 Survey Report. [Google Scholar]
- 49.Ray KN, Chari AV, Engberg J, Bertolet M, Mehrotra A. Disparities in time spent seeking medical care in the United States. JAMA Intern Med. 2015;175(12):1983–1986. doi: 10.1001/jamainternmed.2015.4468. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Hollander JE, Carr BG. Virtually perfect? Telemedicine for COVID-19. N Engl J Med. 2020;382(18):1679–1689. doi: 10.1056/NEJMp2003539. [DOI] [PubMed] [Google Scholar]
- 51.Rawstorn JC, Gant N, Direito A, Beckmann C, Maddison R. Telehealth exercise-based cardiac rehabilitation: a systematic review and meta-analysis. Heart. 2016;102(15):1183–1192. doi: 10.1136/heartjnl-2015-308966. [DOI] [PubMed] [Google Scholar]