Dear editor,
We read with great interest the recent issue1 , 2 regarding the activity of influenza during COVID-19 pandemic, which demonstrated the reduction of influenza in Brazil and Singapore at the same time. The similar findings were also reported in Japan and Taiwan, in which the activity of seasonal influenza was lower in 2020 than before.3 , 4 The decreased activity of seasonal influenza could be due to the implementation of many infection control measures to prevent the spread of SARS-CoV-2 during COVID-19 pandemic.3 , 4 Therefore, we hypothesis that these interventions can also positively impact on other respiratory infectious diseases, such as pulmonary tuberculosis (TB), human immunodeficiency virus (HIV) and Hepatitis C virus (HCV) infections. In this study, we compared the weekly confirmed TB, HIV and HCV cases during COVID-19 outbreak in the 2020 season vs 4 previous seasons.
In this study, we examined this issue using nationwide surveillance data on infectious diseases from 2017 to 2020 provided by the Centers for Disease Control and Prevention (CDC) in Taiwan.5 We compared changes across the first 20 calendar weeks of 2020 with the same period of 2017, 2018, and 2019. Theil-Sen trend test was used to calculate the trend of each event and slope difference in comparison between years.6
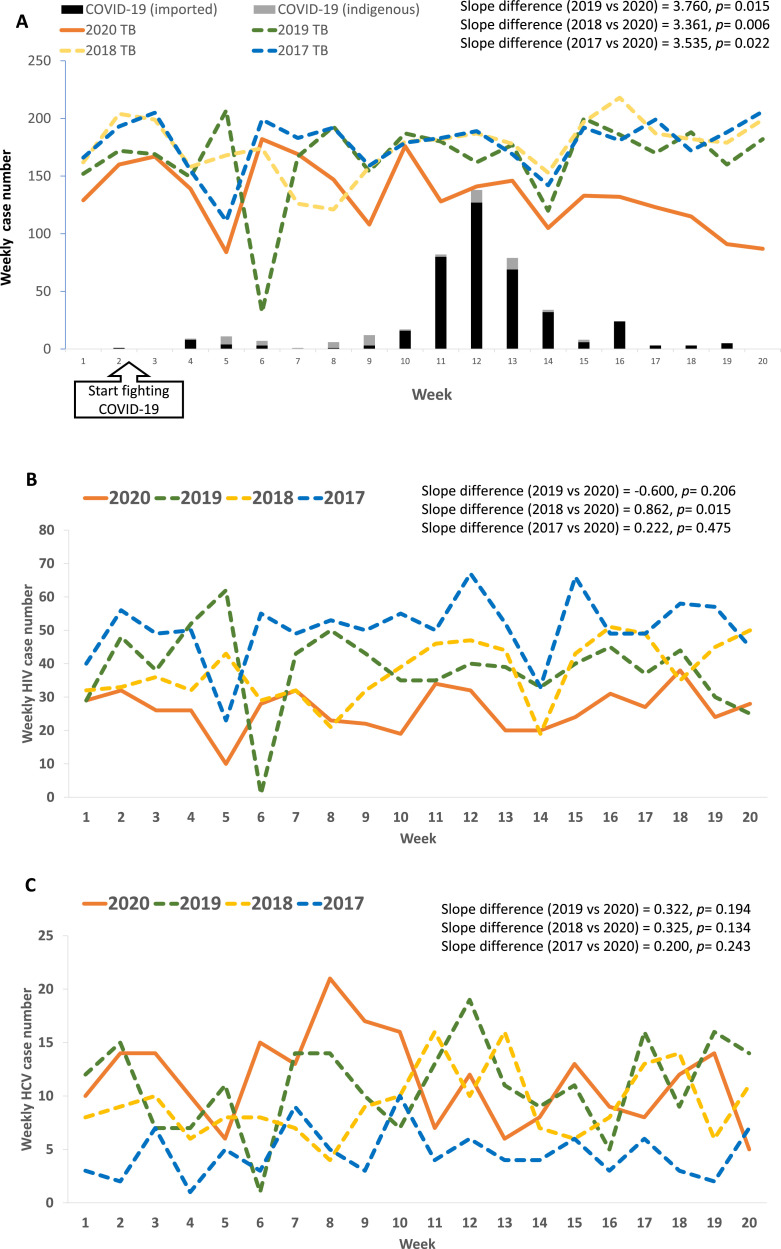
During the first 20 weeks of 2020, a total of 2662 confirmed TB cases were reported, which was lower than those of 2019 (n = 3307), 2018 (n = 3512), and 2017 (n = 3563), with a significant slope difference between 2020 and each of prior years (Fig. 1 A). In contrast, this kind of declining trend of TB during COVID-19 pandemic was not observed for HIV and HCV cases (Fig. 1B and 1C).
Fig. 1.
The trends of infectious events (TB, HIV, and HCV) during the first 20 calendar weeks of 2020 were compared to the events during the corresponding time period in 2017, 2018, and 2019. (A) The COVID-19 outbreak was successfully contained after initiating cotrol measures from the 2nd week, except for some imported cases peaked in the 12th week; the weekly TB cases showing slow decline of TB cases after fitiging COVID-19 outbreak, and significsnt trend difference of TB in 2020 (slope = −2.861) compared to 2019 (slope = 0.899), 2018 (slope = 1.500) and 2017 (slope = 0.674); (B) weekly HIV cases showing no significant trend difference of HIV in 2020 (slope = 0.000) compared to 2019 (slope = −0.600) and 2017 (slope = 0.222), except for 2018 (slope = 0.862); (C) weekly HCV cases showing no significant trend difference of HCV in 2020 (slope = −0.200) compared to 2019 (slope = 0.122), 2018 (slope = 0.125), and 2017 (slope = 0.000).
In this study, we had two major findings. First, the prevention measures for containing SARS-CoV-2 transmission may explain the decline of TB trend. Since early 2020, the Taiwan government and the public have widely promoted measures such as wearing surgical masks, respiratory hygiene, handwashing, maintaining social distance, and suspension of large crowd events7 , 8 and these interventions may also help to contain the spreading of TB. The trend of the decline of TB in this COVID-19 outbreak was more prominent during the 11th-20th calendar weeks than 1st-10th weeks (n = 1201 vs n = 1461). The slope difference between upward trend till the peak (slope = 2.000) and downward trend from the peak (slope = −6.750) reached statistical significance in 2020 (trend difference = 8.750, p = 0.027). The downward speed of decline of TB (from the first case of COVID-19 identified in the second week down to 20th week) was rather slower than that of decreasing influenza activity (from a peak in the second week down to zero case in the 9th week) with a significant trend difference (slope difference = −12.064, p = 0.010). The slower TB decline may probably be due to the longer incubation time of TB activity and some reactivated nature of TB disease, that patients might acquire TB before the COVID-19 outbreak.
Second, we observed that the trends of HIV and HCV infections as control groups did not change as that of TB in this study in spite of the aggressive implementation of infection control measures during this period. The difference might be due to the different transmission routes between TB and comparators of HIV and HCV. TB and COVID-19 are transmitted via the respiratory tract, so the infection control measure for SARS-CoV-2 infection can be helpful for TB control, too. In contrast, HIV is mainly transmitted through sexual behaviors and HCV is a blood-borne disease that can be spread through contamination by blood transfusion, needle or syringe use. Therefore, the current measures for containing the SARS-CoV-2 transmission cannot provide additional help for HIV and HCV control. Furthermore, the maintenance of HCV and HIV trends does not support to consider that physicians would less report infectious diseases like TB while devoted to fighting against the COVID-19 outbreak.
The limitation of the study is that we could not obtain the number of tests for Mycobacterium tuberculosis (MTB). Thus, there was a possibility of confounding factor that whether the COVID-9 outbreak may have lowered the identification of TB through changes in the behavior of symptomatic individuals seeking medical attention or in physicians’ inclination to test for MTB.
In conclusion, we noticed the significant decline of TB activity during fighting against COVID-19 outbreak in Taiwan. Droplet aerosol precaution by prevention measures may offer success in containing SARS-CoV-2 transmission and collateral benefits in TB controls. We also highlight TB diagnosis which should not be forgotten by a physician for patients with respiratory symptoms during the COVID-19 outbreak.
References
- 1.de Souza Luna L.K., Perosa D.A.H., Conte D.D., Carvalho J.M.A., Alves V.R.G., Cruz J.S., Bellei N. Different patterns of Influenza A and B detected during early stages of COVID-19 in a university hospital in São Paulo, Brazil. J Infect. 2020 May 21 doi: 10.1016/j.jinf.2020.05.036. S0163-4453(20)30313-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Chow A., Hein A.A., Kyaw W.M. Unintended Consequence: influenza plunges with public health response to COVID-19 in Singapore. J Infect. 2020 Apr 30 doi: 10.1016/j.jinf.2020.04.035. S0163-4453(20)30262-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Sakamoto H., Ishikane M., Ueda P. Seasonal influenza activity during the SARS-CoV-2 outbreak in Japan. JAMA. 2020;323:1969–1971. doi: 10.1001/jama.2020.6173. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Kuo S.C., Shih S.M., Chien L.H., Hsiung C.A. Collateral benefit of COVID-19 control measures on influenza activity, Taiwan. Emerg. Infect Dis. 2020;26(8) doi: 10.3201/eid2608.201192. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Taiwan CDC. https://nidss.cdc.gov.tw/ch/SingleDisease.aspx?dc=1&dt=3&disease=010. Accessed on May 19, 2020.
- 6.Moses T.P., Klockars A.J. Traditional and proposed tests of slope homogeneity for non-normal and heteroscedastic data. Br J Math Stat Psychol. 2012;65:402–426. doi: 10.1111/j.2044-8317.2011.02034.x. [DOI] [PubMed] [Google Scholar]
- 7.Cheng H.Y., Li S.Y., Yang C.H. Initial rapid and proactive response for the COVID-19 outbreak - Taiwan's experience. J Formos Med Assoc. 2020;119:771–773. doi: 10.1016/j.jfma.2020.03.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Wang C.J., Ng C.Y., Brook R.H. Response to COVID-19 in Taiwan: big data analytics, new technology, and proactive testing. JAMA. 2020 doi: 10.1001/jama.2020.3151. [DOI] [PubMed] [Google Scholar]