Abstract
Background
The predicting bleeding complications in patients undergoing stent implantation and subsequent dual antiplatelet therapy (PRECISE-DAPT) score predicts the risk of bleeding in patients treated with dual antiplatelet therapy after percutaneous coronary intervention. Although the PRECISE-DAPT score is expected to be useful beyond its original field, long-term prognostic value of this score in patients with acute myocardial infarction (AMI) remains unclear. In the current study, we aimed to investigate the performance of the PRECISE-DAPT score in predicting the long-term prognosis in patients with AMI.
Methods and results
Consecutive 552 patients with AMI, who had been discharged from our institution, were enrolled. We divided the patients into three groups, based on their PRECISE-DAPT scores: the low (PRECISE-DAPT < 17), intermediate (17–24) and high (≥25) score groups. Kaplan-Meier analysis (mean follow-up 1424 days) revealed that all-cause mortality increased most steeply in the high score group followed by the intermediate and low score groups (P < 0.001). After adjusting for possible confounding factors, mortality of the intermediate or high score groups were higher than those of low score group (HR 2.945, 95% CI 1.182–7.237, P = 0.020, and HR 5.567, 95% CI 2.644–11.721, P < 0.001, respectively).
Conclusions
In patients with AMI, a high PRECISE-DAPT score was associated with higher long-term all-cause mortality. PRECISE-DAPT score is useful for predicting all-cause mortality, as well as risk stratification of bleeding.
Keywords: Myocardial infarction, PRECISE-DAPT score, Prognosis, Risk stratification
1. Introduction
In recent years, the incidence and mortality of acute myocardial infarction (AMI) have been declining. [1], [2] However, in spite of recent advances in percutaneous coronary intervention (PCI) techniques and devices, patients with AMI still have a higher mortality than that of the general population. [2] Therefore, early risk stratification is important to predict outcomes in patients with AMI.
The predicting bleeding complications in patients undergoing stent implantation and subsequent dual antiplatelet therapy (PRECISE-DAPT) score was developed to predict the bleeding risk in patients treated with dual antiplatelet therapy (DAPT) after PCI. This score is calculated by five items (age, white blood cell count, hemoglobin level, creatinine clearance, and history of spontaneous bleeding) and patients with a score of ≥25 are at a high risk of bleeding. [3] The current guidelines have recommended the use of the PRECISE-DAPT score for bleeding risk stratification, and a score of ≥ 25 indicates that the DAPT period should be shorter 3 to 6 months than that in patients with a score of < 25. [4], [5], [6] Although the PRECISE-DAPT score is expected to be useful beyond its original field, long-term prognostic value of this score in patients with AMI remains unclear. Thus, the aim of the present study was to assess the performance of the PRECISE-DAPT score in predicting the long-term prognosis in patients with AMI.
2. Methods
2.1. Subjects and study protocol
The current study was a prospective observational one, which enrolled a total of 552 consecutive patients with AMI, who had been hospitalized and discharged from Fukushima Medical University between January 2010 and September 2018. The diagnosis of AMI was made based on the World Health Organization (WHO) multinational monitoring of trends and determinants of cardiovascular disease (MONICA) criteria. [7] Patients needed to be registered within 72 h after the onset of symptoms if their level of creatine phosphokinase (CK) or its MB isoform (CK-MB) increased to more than twice the normal range, as previously reported. [8]
The PRECISE-DAPT score was calculated for each patient using web calculator (http://www.precisedaptscore.com) before hospital discharge. We divided the patients into three groups based on their PRECISE-DAPT score, as previously reported [3]: the low (PRECISE-DAPT < 17, n = 210), intermediate (17–24, n = 87) and high (≥25, n = 255) score groups. We compared the clinical features, laboratory data and echocardiographic data, as well as the treated culprit lesion and therapies among the groups.
The patients were followed up until August 2019 for all-cause death. The status and/or dates of death of all patients were obtained from the patients’ medical records, the attending physicians at the patient’s referring hospital, or by contacting the patients by telephone. We were able to follow up all patients. Survival time was calculated from the date of hospitalization until the date of death or last follow-up. Written informed consent was obtained from all study subjects at discharge. The study protocol was approved by the Ethics Committee of Fukushima Medical University, and was carried out in accordance with the principles outlined in the Declaration of Helsinki. Reporting of the study conforms to STROBE, along with references to STROBE and the broader EQUATOR guidelines. [9]
2.2. Co-morbidities and previous history
Co-morbidities were defined as previously reported. [10] A smoker was defined as a patient with a current smoking habit or a habit that had been discontinued ≤ 6 months before hospitalization. Hypertension was defined as the recent use of antihypertensive drugs, a systolic blood pressure of ≥ 140 mmHg, and/or a diastolic blood pressure of ≥ 90 mmHg. Diabetes mellitus was defined as the recent use of antidiabetic drugs, a fasting blood glucose value of ≥ 126 mg/dl, and/or a hemoglobin A1c value of ≥ 6.5%. Dyslipidemia was defined as the recent use of cholesterol-lowering drugs, a triglyceride value of ≥ 150 mg/dL, a low-density lipoprotein cholesterol value of ≥ 140 mg/dL, and/or a high-density lipoprotein cholesterol value of < 40 mg/dL. Chronic kidney disease was defined as an estimated glomerular filtration rate of < 60 ml/min/1.73 cm2. Anemia was defined as hemoglobin levels of < 12.0 g/dl in females and < 13.0 g/dl in males. [11] Atrial fibrillation was identified by an electrocardiogram performed during hospitalization and/or from medical records.
2.3. Laboratory data and Echocardiography
After primary PCI, blood samples were obtained every 3 h, and the peak CK and CK-MB levels of each sample were measured. Blood samples for calculating PRECISE-DAPT score were obtained at hospital discharge. Echocardiography was performed blindly by experienced echocardiographers to assess left ventricular ejection fraction (LVEF) using the modified Simpson’s biplane method. All measurements were performed using ultrasound systems (ACUSON Sequoia, Siemens Medical Solutions USA, Inc., Mountain View, CA, USA).
2.4. Lesions and therapies
Multivessel disease was defined as the presence of lesions with ≥ 75% stenosis in a non-infarct-related coronary artery. [12] ST-elevated myocardial infarction (STEMI) was defined as ST-segment elevation ≥ 0.1 mV (≥0.2 mV for leads V1-V3) in two or more contiguous leads. [12] Since the present study was an observational cohort study, treatment was selected at each physician’s discretion. Door to balloon time was defined as the duration between patient hospital arrival and reperfusion of the culprit coronary artery. Unless there were serious complications, duration of DAPT periods were three months for bare-metal stent and one year for drug-eluting stent, regardless of anticoagulation. After that, an aspirin or a P2Y12 inhibitor has been continued.
2.5. Statistical analysis
Quantitative variables are presented as mean ± SD (for normal distribution of data) or median with interquartile range (for non-normal distribution of data). The categorical variables are expressed as numbers and percentages, and the chi-square test was used for comparisons. We used analysis of variance followed by Bonferroni’s post-hoc test. The Kaplan-Meier method was used for presenting the mortality, with the log-rank test. The prognostic value was tested by univariate and multivariate Cox proportional hazard analyses. The univariate Cox proportional hazard analysis was conducted for possible clinically relevant variables. Because of multicollinearity between PRECISE-DAPT score and its components (age, white blood cell count, hemoglobin level, and creatinine clearance), these components were not included in Cox proportional hazard analysis. The proportional hazards assumption for model was checked by examining log minus-log transformed data. The Kaplan-Meier estimates of the survival curves for three groups were plotted against the time to follow-up period. These curves help in identifying non-proportionality patterns in hazard function such as convergence (difference in risk among the groups decreases with time), divergence, or crossing of the curves. In addition, the Schoenfeld test for violation of proportional hazards, which assesses the correlation between scaled residuals and time, was also conducted. To assess the PRECISE-DAPT score for predicting mortality, we also estimated the areas under the curves (AUC) of the receiver operating curve (ROC) to compare the PRECISE-DAPT score with its components (age, white blood cell count, hemoglobin, and creatinine clearance) using the DeLong test. A value of P < 0.05 was considered statistically significant for all comparisons. These analyses were performed using a statistical software package (SPSS ver. 25.0, IBM, Armonk, NY, USA).
3. Results
3.1. Clinical characteristics
Comparison of clinical characteristics in the low, intermediate, and high PRECISE-DAPT score groups are shown in Table 1. Over 40% of the 552 AMI patients had PRECISE-DAPT ≥ 25, and were therefore classified as being at high risk of bleeding. The high score group was significantly older and had a higher prevalence of female gender, chronic kidney disease, anemia, atrial fibrillation and previous coronary artery bypass graft, and had a lower body mass index and lower prevalence of smokers and dyslipidemia, and lower levels of white blood cells, hemoglobin and creatinine clearance. Regarding lesions and therapies, the high score group had a higher number of diseased vessels, higher prevalence of no-infarct left main trunk lesion, and longer door-to-balloon time. Peak CK was significantly higher in the intermediate score group. In addition, the high score group was less likely to require the use of renin-angiotensin system inhibitors and statins. In contrast, LVEF, prevalence of STEMI, and CK-MB level did not differ among the three groups.
Table 1.
Comparisons of clinical characteristics of patients according to PRECISE-DAPT score (n = 552).
| Low-score (PRECISE-DAPT < 17, n = 210) | Intermediate score (PRECISE-DAPT 17–24, n = 87) | High score (PRECISE-DAPT ≥25, n = 255) | P-value | |
|---|---|---|---|---|
| PRECISE-DAPT score | 9.1 ± 5.3 | 20.9 ± 2.1** | 37.6 ± 11.1**†† | <0.001 |
| Age (years) | 55.9 ± 9.0 | 69.7 ± 5.5** | 76.4 ± 9.3**†† | <0.001 |
| Male gender (n, %) | 191 (91.0) | 67 (77.0) | 174 (68.2) | <0.001 |
| Body mass index (kg/m2) | 25.4 ± 3.7 | 23.8 ± 3.1** | 23.2 ± 3.6** | <0.001 |
| Current smoker (n, %) | 169 (80.5) | 55 (63.2) | 139 (54.5) | <0.001 |
| Co-morbidity or previous history | ||||
| Hypertension (n, %) | 169 (80.5) | 72 (82.8) | 216 (84.7) | 0.485 |
| Diabetes (n, %) | 109 (51.9) | 38 (43.7) | 127 (49.8) | 0.434 |
| Dyslipidemia (n, %) | 205 (97.6) | 83 (95.4) | 228 (89.4) | 0.001 |
| Chronic kidney disease (n, %) | 33 (15.7) | 35 (40.2) | 143 (56.1) | <0.001 |
| Anemia (n, %) | 41 (19.5) | 36 (41.4) | 167 (65.5) | <0.001 |
| Atrial fibrillation (n, %) | 17 (8.1) | 10 (11.5) | 53 (20.8) | <0.001 |
| Previous MI (n, %) | 11 (5.2) | 4 (4.6) | 20 (7.8) | 0.398 |
| Previous PCI (n, %) | 12 (5.7) | 6 (6.9) | 287 (11.0) | 0.108 |
| Previous CABG (n, %) | 0 (0.0) | 0 (0.0) | 6 (2.4) | 0.029 |
| Laboratory data | ||||
| White blood cell (/μL) | 6767 ± 2087 | 6332 ± 1722 | 6305 ± 2318 | 0.055 |
| Hemoglobin (g/dL) | 13.7 ± 1.4 | 12.8 ± 1.4** | 11.4 ± 1.8**†† | <0.001 |
| Creatinine clearance (mL/min) | 93.7 ± 22.8 | 67.4 ± 16.2** | 49.4 ± 20.4**†† | <0.001 |
| Echocardiography | ||||
| LVEF (%) | 49.3 ± 17.7 | 49.5 ± 16.6 | 47.1 ± 19.8 | 0.361 |
| Lesion characteristics | ||||
| Number of diseased vessels | <0.001 | |||
| 1 vessel (n, %) | 125 (59.5) | 40 (46.0) | 93 (37.2) | |
| 2 vessels (n, %) | 49 (23.3) | 33 (37.9) | 87 (34.8) | |
| 3 vessels (n, %) | 33 (15.7) | 14 (16.1) | 68 (27.2) | |
| 0 vessel (n, %) | 3 (1.4) | 0 (0.0) | 2 (0.8) | |
| Unknown (n, %) | 0 (0.0) | 0 (0.0) | 5 (2.0) | |
| No-infarct LMT lesion (n, %) | 4 (1.9) | 4 (4.6) | 17 (6.8) | 0.043 |
| No-infarct CTO lesion (n, %) | 12 (5.7) | 8 (9.2) | 29 (11.4) | 0.102 |
| Culprit lesion | <0.001 | |||
| LAD (n, %) | 109 (51.9) | 43 (49.4) | 96 (37.6) | |
| LCx (n, %) | 30 (14.3) | 18 (20.7) | 32 (12.5) | |
| RCA (n, %) | 64 (30.5) | 24 (27.6) | 108 (42.4) | |
| LMT (n, %) | 4 (1.9) | 2 (2.3) | 12 (4.7) | |
| CSA (n, %) | 3 (1.4) | 0 (0.0) | 2 (0.8) | |
| STEMI (n, %) | 155 (73.8) | 71 (81.6) | 196 (76.9) | 0.346 |
| Peak CK (IU/L) | 1781 (671–3910) | 2143 (1110–4030) | 1566 (673–3335) | 0.099 |
| Peak CK-MB (IU/L) | 196 (49–375) | 236 (109–478) | 194 (63–381) | 0.103 |
| Therapies | ||||
| BMS (n, %) | 53 (25.2) | 16 (18.4) | 63 (24.7) | 0.417 |
| DES (n, %) | 137 (65.2) | 59 (67.8) | 160 (62.7) | 0.667 |
| POBA (n, %) | 10 (4.8) | 7 (8.0) | 13 (5.1) | 0.498 |
| CABG (n, %) | 3 (1.4) | 0 (0.0) | 5 (2.0) | 0.417 |
| No interventional therapy (n, %) | 6 (2.9) | 4 (4.6) | 12 (4.7) | 0.568 |
| Door to balloon time (min) | 85 (69–125) | 74 (59–129) | 104 (75–144) | 0.075 |
| Medications | ||||
| Antiplatelets (n, %) | 204 (97.1) | 86 (98.9) | 247 (96.9) | 0.608 |
| β-blockers (n, %) | 170 (81.0) | 75 (86.2) | 198 (77.6) | 0.212 |
| RAS inhibitors (n, %) | 190 (90.5) | 78 (89.7) | 213 (83.5) | 0.063 |
| Statins (n, %) | 191 (91.0) | 78 (89.7) | 196 (76.9) | <0.001 |
| Anticoagulants (n, %) | 34 (16.2) | 13 (14.9) | 57 (22.4) | 0.143 |
PRECISE-DAPT, the predicting bleeding complications in patients undergoing stent implantation and subsequent dual antiplatelet therapy; MI, myocardial infarction; PCI, percutaneous coronary intervention; CABG, coronary artery bypass graft; LVEF, left ventricular ejection fraction; LMT, left main trunk; CTO, chronic total occlusion; LAD, left anterior descending coronary artery; LCx, left circumflex coronary artery; RCA, right coronary artery; CSA, coronary spastic angina; STEMI, ST-elevated myocardial infarction; CK, creatine kinase; BMS, bare metal stent; DES, drug eluting stent; POBA, plain old balloon angioplasty; RAS, renin-angiotensin system.
*P < 0.05 and **P < 0.01 vs. low score group, †P < 0.05 and ††P < 0.01 vs. intermediate score group.
3.2. Follow-up
During the follow up period (mean 1424 days), there were 88 all-cause deaths, including 24 cardiac deaths and 4 bleeding-related deaths. In the Kaplan-Meier analysis, as shown in Fig. 1, all-cause mortality increased most steeply in the high score group followed by the intermediate and low score groups (P < 0.001).
Fig. 1.
Kaplan-Meier curves for all-cause death in the high, intermediate, and low PRECISE-DAPT score groups. PRECISE-DAPT, the predicting bleeding complications in patients undergoing stent implantation and subsequent dual antiplatelet therapy.
3.3. Cox proportional hazard regression analysis
As shown in Table 2, after adjusting for other potential confounding factors (i.e. severity of co-morbidity, coronary artery lesion, revascularization procedure or medication at discharge) by the multivariate analysis, it was revealed that atrial fibrillation, no-infarct-related chronic total occlusion (CTO) lesion, increase of LVEF, usage of antiplatelets and statins were associated with all-cause mortality, and their hazard ratios were 2.491 (95% CI: 1.381–4.490), 2.477 (1.387–4.423), 0.988 (0.977–1.000), 0.231 (0.074–0.726) and 0.483 (0.263–0.890), respectively. PRECISE-DAPT score was also revealed as an independent prognostic factor and the Cox proportional hazard analysis demonstrated that belonging to the intermediate or high score group had the risk of all-cause mortality in AMI patients compared with low score group (HR 2.945, 95% CI 1.182–7.237, P = 0.020, and HR 5.567, 95% CI 2.644–11.721, P < 0.001, respectively).
Table 2.
Cox proportional hazard model of all-cause mortality (event 88, n = 552).
| Risk factor | Univariable |
Multivariable |
||||
|---|---|---|---|---|---|---|
| HR | 95% CI | P-value | HR | 95% CI | P-value | |
| PRECISE-DAPT score (low) | Ref. | Ref. | ||||
| Intermediate (vs. low) | 3.161 | 1.309–7.630 | <0.001 | 2.945 | 1.182–7.237 | 0.020 |
| High (vs. low) | 7.246 | 3.614–14.527 | <0.001 | 5.567 | 2.644–11.721 | <0.001 |
| Male gender | 0.832 | 0.514–1.349 | 0.456 | |||
| Body mass index | 0.899 | 0.844–0.959 | 0.001 | 0.989 | 0.922–1.061 | 0.759 |
| Current smoker | 0.568 | 0.373–0.864 | 0.008 | 0.940 | 0.590–1.497 | 0.793 |
| Hypertension | 1.040 | 0.499–2.167 | 0.917 | |||
| Diabetes | 1.042 | 0.686–1.584 | 0.846 | |||
| Dyslipidemia | 0.262 | 0.138–0.497 | <0.001 | 1.186 | 0.498–2.825 | 0.701 |
| Atrial fibrillation | 2.701 | 1.686–4.327 | <0.001 | 2.491 | 1.381–4.490 | 0.002 |
| Previous MI | 1.539 | 0.772–3.067 | 0.221 | |||
| Previous PCI | 1.203 | 0.603–2.399 | 0.599 | |||
| Previous CABG | 1.317 | 0.183–9.477 | 0.785 | |||
| LVEF | 0.985 | 0.975–0.994 | 0.002 | 0.988 | 0.977–1.000 | 0.049 |
| Number of diseased vessels | 1.411 | 0.921–2.163 | 0.114 | |||
| No-infarct LMT lesion | 1.993 | 0.918–4.327 | 0.081 | 1.592 | 0.712–3.557 | 0.257 |
| No-infarct CTO lesion | 2.743 | 1.615–4.659 | <0.001 | 2.477 | 1.387–4.423 | 0.002 |
| Culprit lesion (LAD) | 0.778 | 0.506–1.195 | 0.252 | |||
| Log peak CK | 0.924 | 0.577–1.481 | 0.744 | |||
| DES | 0.932 | 0.605–1.436 | 0.750 | |||
| BMS | 0.737 | 0.463–1.174 | 0.199 | |||
| Door to balloon time | 1.002 | 0.999–1.004 | 0.154 | |||
| Antiplatelets | 0.215 | 0.093–0.494 | <0.001 | 0.231 | 0.074–0.726 | 0.012 |
| β-blockers | 0.622 | 0.388–0.995 | 0.047 | 0.796 | 0.473–1.340 | 0.390 |
| RAS inhibitors | 0.491 | 0.289–0.835 | 0.009 | 0.551 | 0.303–1.001 | 0.051 |
| Statins | 0.249 | 0.159–0.390 | <0.001 | 0.483 | 0.263–0.890 | 0.020 |
| Anticoagulants | 1.562 | 0.977–2.498 | 0.062 | 0.877 | 0.497–1.550 | 0.652 |
PRECISE-DAPT, the predicting bleeding complications in patients undergoing stent implantation and subsequent dual antiplatelet therapy; MI, myocardial infarction; PCI, percutaneous coronary intervention; CABG, coronary artery bypass graft; LVEF, left ventricular ejection fraction; LMT, left main trunk; CTO, chronic total occlusion; LAD, left anterior descending coronary artery; CK, creatine kinase; DES, drug eluting stent; BMS, bare metal stent; RAS, renin-angiotensin system.
3.4. ROC analysis
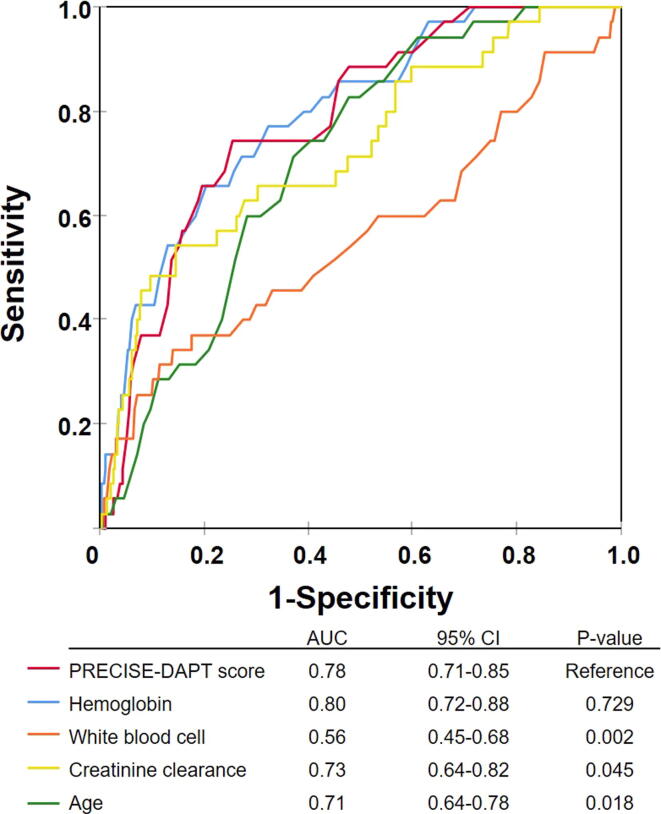
As shown in Fig. 2, the AUC values of the PRECISE-DAPT score and its components (hemoglobin, white blood cell count, creatinine clearance, and age) for all-cause mortality were 0.78 (95% CI 0.71–0.85), 0.80 (0.72–0.88), 0.56 (0.45–0.68), 0.73 (0.64–0.82) and 0.71 (0.64–0.78), respectively. ROC analysis demonstrated that the predictive value of the PRECISE-DAPT score for long-term mortality was superior to three components of the score (white blood cell count, creatinine clearance and age), whereas there was no significant difference compared to hemoglobin.
Fig. 2.
Receiver operating curves (ROC) to predict mortality in patients with AMI. PRECISE-DAPT, the predicting bleeding complications in patients undergoing stent implantation and subsequent dual antiplatelet therapy.
4. Discussion
To the best of our knowledge, the current study is the first to report that the long-term mortality was significantly higher in AMI patients with a high PRECISE-DAPT score than in those with a low score, regardless of severity of co-morbidity, coronary artery lesion, revascularization procedure or medication at discharge.
In patients with AMI, various short and long-term prognostic factors have been reported. Co-morbidities such as diabetes, chronic kidney disease, anemia and atrial fibrillation are well known to be associated with long-term prognosis in patients with AMI. [13], [14], [15], [16] LVEF is also associated with one-year or longer-term mortality in patients with AMI. [17] Presence of CTO lesion in a non-infarct-related coronary artery has been reported to worsen 30-day mortality. [18] Regarding treatment, β-blockers, renin-angiotensin system inhibitors, and statins are common treatments as secondary prevention for patients with AMI, [19], [20], [21] and administration of these medications are reported to be associated with good long-term outcomes. [22] The global registry of acute coronary events (GRACE) score has been widely used for estimating admission to 6-month mortality for patients with acute coronary syndrome. This score is calculated from eight items (age, history of heart failure, history of myocardial infarction, heart rate, blood pressure, ST-segment depression, serum creatinine, elevated cardiac enzymes, and no-PCI), and 2 factors out of them (age and renal function) are shared with the PRECISE-DAPT score. [23] In the present study, atrial fibrillation, no-infarct-related CTO lesion, decrease of LVEF, and disuse of antiplatelets and/or statins were associated with all-cause mortality after multivariate analysis. As mentioned above, these prognostic factors have already been reported individually. [16], [17], [18], [21], [24] The PRECISE-DAPT score includes several values (hemoglobin, white blood cell count, and creatinine clearance), which can be obtained from routine blood test. In the present study, we compared the PRECISE-DAPT score with these factors and age. The ROC analysis demonstrated that the prognostic value of this score was superior to that of white blood cell count, creatinine clearance, and age, and comparable to that of hemoglobin (Fig. 2).
The PRECISE-DAPT score is a recently developed concept, and its usefulness beyond its original usage (predict bleeding risk) is being demonstrated in other fields. Yildirim et al. reported that the PRECISE-DAPT score was associated with high-degree atrioventricular block and atrial fibrillation in patients with STEMI who underwent PCI. [25] Another previous study has identified that the PRECISE-DAPT score is a significant independent predictor of contrast-induced nephropathy in STEMI patients treated with primary PCI. [26] On the other hand, a few studies have reported on the association between PRECISE-DAPT score and the mortality of patients with AMI. Tanik et al. reported that the PRECISE-DAPT score is a significant independent predictor of in-hospital mortality in patients with STEMI. [27] The follow-up period of our present study was longer than that in their report, and we demonstrated the prognostic value of the PRECISE-DAPT score in predicting post-discharge long-term outcomes.
5. Clinical implications
Since East Asian people, including Japanese, have a higher risk of bleeding than Europeans or Americans, [28] we should always pay attention to patient management after PCI from this perspective. The setting of the DAPT period is one of the important issues, and the PRECISE-DAPT score is very useful for that determination. At the same time, if this score can predict the long-term prognosis of patients with AMI, we are able to provide personalized medical care, for example, enhanced risk factor management for atherosclerotic disease. The PRECISE-DAPT score can be easily calculated, can be used to determine the optimal DAPT period, and also will be useful as a long-term prognostic factor beyond its original field, for patients with AMI.
6. Study limitations
There are several limitations in the present study. First, as a prospective observational cohort study of a single center with a relatively small number of patients, the study may be somewhat underpowered. Second, we used only variables on hospitalization in this study, without taking into consideration changes in medical parameters and post-discharge treatment. Therefore, the present results should be viewed as preliminary, and further studies with a larger population are needed.
7. Conclusions
In patients with AMI, a high PRECISE-DAPT score was associated with higher long-term all-cause mortality. Therefore, the PRECISE-DAPT score could be useful not only for the risk stratification of bleeding with antiplatelet therapy, but also for predicting all-cause mortality in patients with AMI. We suspect that the PRECISE-DAPT score will be useful in various fields beyond its originally intended usage.
CRediT authorship contribution statement
Takuya Ando: Methodology, Formal analysis, Investigation, Writing - original draft. Kazuhiko Nakazato: Methodology, Formal analysis, Investigation, Writing - original draft, Supervision. Yusuke Kimishima: Investigation. Takatoyo Kiko: Investigation. Takeshi Shimizu: Investigation. Tomofumi Misaka: Formal analysis. Shinya Yamada: Formal analysis. Takashi Kaneshiro: Formal analysis. Akiomi Yoshihisa: Methodology, Formal analysis, Writing - review & editing. Takayoshi Yamaki: Investigation. Hiroyuki Kunii: Investigation. Yasuchika Takeishi: Methodology, Writing - review & editing, Project administration.
Acknowledgments
Acknowledgements
None.
Disclosures
There were no conflicts of interest.
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.ijcha.2020.100552.
Appendix A. Supplementary material
The following are the Supplementary data to this article:
References
- 1.Yamamoto T., Yoshida N., Takayama M. Temporal trends in acute myocardial infarction incidence and mortality between 2006 and 2016 in Tokyo - report from the Tokyo CCU network. Circ. J. 2019;83:1405–1409. doi: 10.1253/circj.CJ-19-0187. [DOI] [PubMed] [Google Scholar]
- 2.Piironen M., Ukkola O., Huikuri H., Havulinna A.S., Koukkunen H., Mustonen J. Trends in long-term prognosis after acute coronary syndrome. Eur. J. Prev. Cardiol. 2017;24:274–280. doi: 10.1177/2047487316679522. [DOI] [PubMed] [Google Scholar]
- 3.Costa F., van Klaveren D., James S., Heg D., Raber L., Feres F. Derivation and validation of the predicting bleeding complications in patients undergoing stent implantation and subsequent dual antiplatelet therapy (PRECISE-DAPT) score: a pooled analysis of individual-patient datasets from clinical trials. Lancet. 2017;389:1025–1034. doi: 10.1016/S0140-6736(17)30397-5. [DOI] [PubMed] [Google Scholar]
- 4.Valgimigli M., Bueno H., Byrne R.A., Collet J.P., Costa F., Jeppsson A. 2017 ESC focused update on dual antiplatelet therapy in coronary artery disease developed in collaboration with EACTS: The Task Force for dual antiplatelet therapy in coronary artery disease of the European Society of Cardiology (ESC) and of the European Association for Cardio-Thoracic Surgery (EACTS) Eur. Heart J. 2018;39:213–260. doi: 10.1093/eurheartj/ehx419. [DOI] [PubMed] [Google Scholar]
- 5.Levine G.N., Bates E.R., Bittl J.A., Brindis R.G., Fihn S.D., Fleisher L.A. 2016 ACC/AHA Guideline Focused Update on Duration of Dual Antiplatelet Therapy in Patients With Coronary Artery Disease: A Report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines: An Update of the 2011 ACCF/AHA/SCAI Guideline for Percutaneous Coronary Intervention, 2011 ACCF/AHA Guideline for Coronary Artery Bypass Graft Surgery, 2012 ACC/AHA/ACP/AATS/PCNA/SCAI/STS Guideline for the Diagnosis and Management of Patients With Stable Ischemic Heart Disease, 2013 ACCF/AHA Guideline for the Management of ST-Elevation Myocardial Infarction, 2014 AHA/ACC Guideline for the Management of Patients With Non-ST-Elevation Acute Coronary Syndromes, and 2014 ACC/AHA Guideline on Perioperative Cardiovascular Evaluation and Management of Patients Undergoing Noncardiac Surgery. Circulation. 2016;134:e123–155. doi: 10.1161/CIR.0000000000000404. [DOI] [PubMed] [Google Scholar]
- 6.Kimura K., Kimura T., Ishihara M., Nakagawa Y., Nakao K., Miyauchi K. JCS 2018 guideline on diagnosis and treatment of acute coronary syndrome. Circ. J. 2019;83:1085–1196. doi: 10.1253/circj.CJ-19-0133. [DOI] [PubMed] [Google Scholar]
- 7.The World Health Organization MONICA Project (monitoring trends and determinants in cardiovascular disease): a major international collaboration. WHO MONICA Project Principal Investigators. J. Clin. Epidemiol. 1988;41:105–114. doi: 10.1016/0895-4356(88)90084-4. [DOI] [PubMed] [Google Scholar]
- 8.Yamaki T., Nakazato K., Kijima M., Maruyama Y., Takeishi Y. Impact of the Great East Japan Earthquake on acute myocardial infarction in Fukushima prefecture. Disaster Med. Public Health Prep. 2014;8:212–219. doi: 10.1017/dmp.2014.37. [DOI] [PubMed] [Google Scholar]
- 9.von Elm E., Altman D.G., Egger M., Pocock S.J., Gotzsche P.C., Vandenbroucke J.P. Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement: guidelines for reporting observational studies. BMJ. 2007;335:806–808. doi: 10.1136/bmj.39335.541782.AD. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Yoshihisa A., Kanno Y., Watanabe S., Yokokawa T., Abe S., Miyata M. Impact of nutritional indices on mortality in patients with heart failure. Open Heart. 2018;5 doi: 10.1136/openhrt-2017-000730. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Ponikowski P, Voors AA, Anker SD, Bueno H, Cleland JG, Coats AJ, et al. 2016 ESC Guidelines for the diagnosis and treatment of acute and chronic heart failure: The Task Force for the diagnosis and treatment of acute and chronic heart failure of the European Society of Cardiology (ESC). Developed with the special contribution of the Heart Failure Association (HFA) of the ESC. Eur. J. Heart Fail. 2016; 18: 891-975. [DOI] [PubMed]
- 12.Steg P.G., James S.K., Atar D., Badano L.P., Blomstrom-Lundqvist C., Borger M.A. ESC Guidelines for the management of acute myocardial infarction in patients presenting with ST-segment elevation. Eur. Heart J. 2012;33:2569–2619. doi: 10.1093/eurheartj/ehs215. [DOI] [PubMed] [Google Scholar]
- 13.Gruppetta M., Calleja N., Fava S. Long-term survival after acute myocardial infarction and relation to type 2 diabetes and other risk factors. Clin. Cardiol. 2010;33:424–429. doi: 10.1002/clc.20776. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Roldan Torres I., Salvador Mercader I., Cabades Rumbeu C., Diez Gil J.L., Ferrando Cervello J., Monteagudo Viana M. Long-term prognosis of chronic kidney disease in non-ST elevation acute coronary syndrome treated with invasive strategy. Nefrologia. 2017;37:276–284. doi: 10.1016/j.nefro.2016.11.011. [DOI] [PubMed] [Google Scholar]
- 15.Colombo M.G., Kirchberger I., Amann U., Heier M., Thilo C., Kuch B. Association between admission anemia and long-term mortality in patients with acute myocardial infarction: results from the MONICA/KORA myocardial infarction registry. BMC Cardiovasc. Disord. 2018;18:50. doi: 10.1186/s12872-018-0785-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Jabre P., Roger V.L., Murad M.H., Chamberlain A.M., Prokop L., Adnet F. Mortality associated with atrial fibrillation in patients with myocardial infarction: a systematic review and meta-analysis. Circulation. 2011;123:1587–1593. doi: 10.1161/CIRCULATIONAHA.110.986661. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Perelshtein Brezinov O., Klempfner R., Zekry S.B., Goldenberg I., Kuperstein R. Prognostic value of ejection fraction in patients admitted with acute coronary syndrome: a real world study. Medicine. 2017;96 doi: 10.1097/MD.0000000000006226. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Mizuguchi Y., Takahashi A., Hashimoto S., Yamada T., Taniguchi N., Nakajima S. Impact of the presence of chronic total occlusion in a non-infarct-related coronary artery in acute myocardial infarction patients. Int. Heart J. 2015;56:592–596. doi: 10.1536/ihj.15-080. [DOI] [PubMed] [Google Scholar]
- 19.Dargie H.J. Effect of carvedilol on outcome after myocardial infarction in patients with left-ventricular dysfunction: the CAPRICORN randomised trial. Lancet. 2001;357:1385–1390. doi: 10.1016/s0140-6736(00)04560-8. [DOI] [PubMed] [Google Scholar]
- 20.Indications for ACE inhibitors in the early treatment of acute myocardial infarction: systematic overview of individual data from 100,000 patients in randomized trials. ACE Inhibitor Myocardial Infarction Collaborative Group. Circulation. 1998; 97: 2202-2212. [DOI] [PubMed]
- 21.Raposeiras-Roubin S., Abu-Assi E., Cespon-Fernandez M., Ibanez B., Garcia-Ruiz J.M., D'Ascenzo F. Impact of renin-angiotensin system blockade on the prognosis of acute coronary syndrome based on left ventricular ejection fraction. Rev. Esp. Cardiol. 2020;73:114–122. doi: 10.1016/j.rec.2019.02.012. [DOI] [PubMed] [Google Scholar]
- 22.Siddiqui A.J., Holzmann M.J. Association between reduced left ventricular ejection fraction following non-ST-segment elevation myocardial infarction and long-term mortality in patients of advanced age. Int. J. Cardiol. 2019;296:15–20. doi: 10.1016/j.ijcard.2019.07.019. [DOI] [PubMed] [Google Scholar]
- 23.Fox K.A.A., Dabbous O.H., Goldberg R.J., Pieper K.S., Eagle K.A., Van de Werf F. Prediction of risk of death and myocardial infarction in the six months after presentation with acute coronary syndrome: prospective multinational observational study (GRACE) BMJ. 2006;333:1091–1094. doi: 10.1136/bmj.38985.646481.55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Chiang F.T., Shyu K.G., Wu C.J., Mar G.Y., Hou C.J., Li A.H. Predictors of 1-year outcomes in the Taiwan Acute Coronary Syndrome Full Spectrum Registry. J. Formos. Med. Assoc. 2014;113:794–802. doi: 10.1016/j.jfma.2013.08.001. [DOI] [PubMed] [Google Scholar]
- 25.Yildirim E., Turkkan C., Ozcan K.S., Ceylan U.S., Zengin A. The predictive value of PRECISE-DAPT score for arrhythmic complications in patients with ST-elevation myocardial infarction. Coron. Artery Dis. 2019;30:499–504. doi: 10.1097/MCA.0000000000000788. [DOI] [PubMed] [Google Scholar]
- 26.Cinar T., Tanik V.O., Arugaslan E., Karabag Y., Cagdas M., Rencuzogullari I. The association of PRECISE-DAPT score with development of contrast-induced nephropathy in patients with ST-elevation myocardial infarction undergoing primary percutaneous coronary intervention. Cardiovasc. Interv. Ther. 2019;34:207–215. doi: 10.1007/s12928-018-0545-6. [DOI] [PubMed] [Google Scholar]
- 27.Tanik V.O., Cinar T., Arugaslan E., Karabag Y., Hayiroglu M.I., Cagdas M. The Predictive Value of PRECISE-DAPT Score for In-Hospital Mortality in Patients With ST-Elevation Myocardial Infarction Undergoing Primary Percutaneous Coronary Intervention. Angiology. 2019;70:440–447. doi: 10.1177/0003319718807057. [DOI] [PubMed] [Google Scholar]
- 28.Levine G.N., Jeong Y.-H., Goto S., Anderson J.L., Huo Y., Mega J.L. World heart federation expert consensus statement on antiplatelet therapy in east asian patients with ACS or undergoing PCI. Glob. Heart. 2014;9:457–467. doi: 10.1016/j.gheart.2014.08.001. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.