Abstract
Purpose
To report a case of visual recovery and vascular reperfusion after vaso-occlusive retinopathy from anti-phospholipid syndrome associated with systemic lupus erythematosus.
Observations
A 15-year-old boy with a known diagnosis of systemic lupus erythematosus and a clinically significant anti-phospholipid panel presented with sudden vision loss in the left eye. Examination and ocular imaging revealed signs of vaso-occlusive retinopathy. The patient was immediately started on high dose intravenous steroids, followed by mycophenolate mofetil. He remained on aspirin. After showing no improvement in retinal arteriole and capillary perfusion he was started on therapeutic anti-coagulation with enoxaparin. He regained 20/20 vision. Intravenous fluorescein angiography demonstrated reperfusion of retinal arterioles. Optical coherence tomography angiography showed return of flow in the capillary networks.
Conclusions
We present a case of vaso-occlusive retinopathy in a patient with known systemic lupus erythematosus and a clinically significant anti-phospholipid panel, thus meeting criteria for anti-phospholipid syndrome. He was treated with intravenous methylprednisolone, mycophenolate motefil, aspirin, and enoxaparin. The patient not only had great recovery of visual acuity, but also demonstrated reperfusion of arterioles and reconstitution of flow in the retinal capillary network. These findings suggest that the vaso-occlusive disease is reversible if the diagnosis is made promptly and intensive therapy is initiated.
Importance
Currently there are no reported cases of vaso-occlusive retinopathy from APLS and SLE with visual recovery, reperfusion, and return of capillary flow.
Keywords: Systemic lupus erythematosus, Vaso-occlusive retinopathy, APLS, Case report
1. Introduction
Systemic lupus erythematosus (SLE) is a protean autoimmune connective tissue disorder that can involve nearly every organ system and affected patients can present with an array of clinical manifestations.1 SLE can affect any part of the eye including the orbit, eyelids, conjunctiva, cornea, sclera, retina, choroid, and optic nerve.1, 2, 3 Anti-phospholipid syndrome (APLS) is a related autoimmune disorder characterized clinically by recurrent vascular thromboembolic events and fetal loss.4 APLS can occur independently of other autoimmune disorders, but is most commonly associated with SLE, occurring in up to 30% of patients with previously diagnosed lupus.5 The diagnosis of APLS is made based upon the presence of clinical vascular thrombosis and serological presence of elevated anticardiolipin antibodies or anti-beta2-glycoprotein titers.4 Vaso-occlusive retinopathy from APLS is a rare form of retinopathy in patients with SLE, but its visual prognosis is reportedly grim.6,7
Herein, we describe a patient who developed sudden vision loss from vaso-occlusive retinopathy secondary to APLS associated with SLE. He ultimately went on to have good visual recovery and retinal reperfusion after prompt diagnosis and therapy.
1.1. Case report
A 15-year-old boy presented with a 2-week history of sudden, blurred vision in the left eye. His past medical history was significant for a diagnosis of SLE made 1 year previously by pediatric rheumatology. At the time of SLE diagnosis, he developed a malar rash and was found to have elevated titers of anti-double stranded DNA antibodies (312, nl < 30 IU/mL), anti-Smith antibodies (6.1, nl < 1.0 AI), anti-ribonucleoproteins antibodies (4.2, nl < 1.0 AI), Telanti-Sjogren's syndrome antigen A antibodies (8.0, nl < 1.0 AI), anti-nuclear antibody (speckled pattern, 1:1280), Crithidia lucillae testing positive, and low complement C4 levels (6, nl 12–46 mg/dL). He has maintained good control of his symptoms on hydroxychloroquine (400 mg once daily) and prednisone (5 mg once daily). On incremental work up by rheumatology, he was found to have an elevated anti-cardiolipin IgM antibody (32, nl 0–11 MPL) and anti-beta 2 glycoprotein IgM antibody (70, nl < 20 SMU) titers indicative of possible anti-phospholipid syndrome (APLS). His anti-cardiolipin IgM antibody (33 MPL) and anti-beta 2 glycoprotein IgM antibody (52 MPL) titers remained elevated 4 months later on confirmatory testing, thus meeting criteria for a clinically significant antiphospholipid profile. He did not have any clinical signs of vascular thrombosis and he did not have any other clinical manifestations of SLE beyond a malar rash. He was started on prophylactic aspirin 81 mg once daily.
At the time of first ocular examination, visual acuity (VA) was 20/20 in the right eye and 20/80 in the left eye. There was no relative afferent pupillary defect. Intraocular pressure, confrontational visual fields, and extraocular movements were normal. Anterior segment examination was normal. There were no signs of anterior vitreous inflammation. The right fundus was normal. Fundus examination of the left eye demonstrated multiple clustered cotton wool spots in the macula and posterior pole (Fig. 1). In the retina periphery, there was segmental sheathing of both arterioles and venules. On optical coherence tomography (OCT), there was inner retinal hyperreflectivity and thickening, cystoid macular edema, and subretinal fluid (Fig. 2). Intravenous fluorescein angiography (IVFA) was normal in the right eye, but the left eye showed marked macular capillary non-perfusion, arteriole occlusions, delayed venous filling, late macular leakage, and segmental peripheral vascular leakage (Fig. 3a, Fig. 3ba–b). Optical coherence tomography angiography (OCTA) revealed significant flow void in the macula of the left eye (Fig. 4a, Fig. 4ba–b).
Fig. 1.
Fundus photograph of the left eye at the time of patient presentation showing numerous cotton wools spots in the macula and posterior pole.
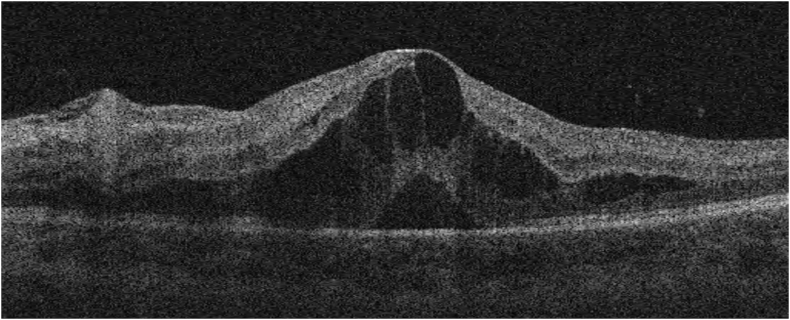
Fig. 2.
OCT of the left eye macula showing retinal thickening, inner retinal hyperreflectivity, cystoid edema, and subretinal fluid.
Fig. 3a.
Late fluorescein angiogram of the right eye demonstrating normal vascular perfusion.
Fig. 3b.
Late fluorescein angiogram of the left eye demonstrating multiple branch retinal artery occlusions, diffuse vascular leakage in the macula, and macular capillary non-perfusion.
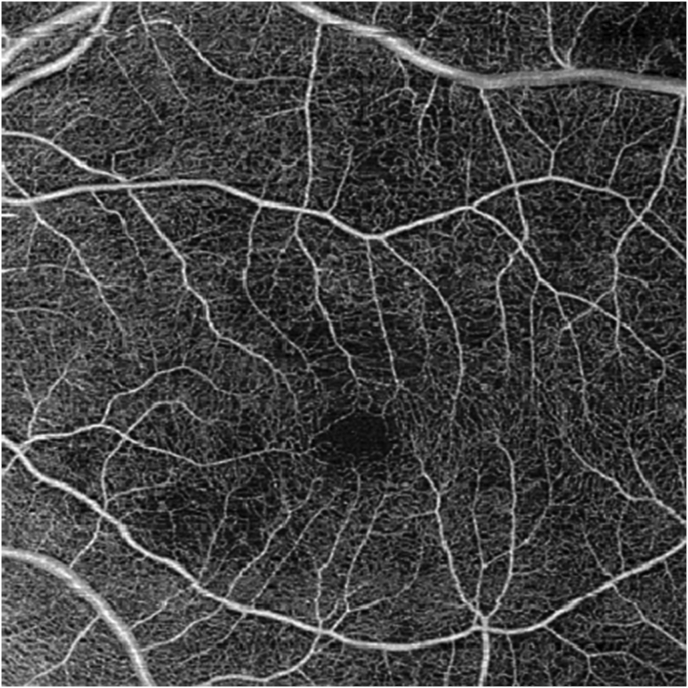
Fig. 4a.
OCT angiography of the unaffected right eye showing a normal flow pattern.
Fig. 4b.
OCT angiography of the left eye showing significant loss of capillary flow signal.
In the setting of new vasothrombotic disease and elevated anti-phospholipid antibody titers a diagnosis of vaso-occlusive retinopathy from APLS was made. The patient was promptly treated with intravenous (IV) methylprednisolone 1 g once daily x 3 days followed by systemic prednisone at 1mg/kg daily, (60 mg once daily) and tapered by 5 mg every week as able. The patient was simultaneously started on mycophenolate mofetil (1000 mg two times per day). At the time of vision loss his APLS panel remained elevated with an anticardiolipin IgM of 20 MPL and an anti-beta2-glycoprotein IgM of 25 SMU. His lupus laboratory tests were abnormal with a low C4 level (9 mg/dL) and an elevated anti-dsDNA antibody titer (312 IU/mL) indicating disease activity.
Despite high dose IV steroids there was minimal improvement detected on interval follow-up OCTA and IVFA. Without improvement in retinal perfusion there was significant concern that permanent visual loss was imminent. One week after initial exam and further discussion with our pediatric rheumatology and hematology/oncology colleagues regarding the risks and benefits of full anti-coagulation in an active 15-year-old boy, the decision was made to therapeutically anti-coagulate the patient with enoxaparin (1 mg/kg every 12 hours, titrated by anti-factor Xa level).
The patient was followed closely and there was remarkable interval improvement in clinical exam, OCTA retinal capillary flow, and IVFA vascular leakage. At 3 months follow-up, the patient's VA improved to 20/20 in the affected left eye. OCTA demonstrated reconstitution of flow in the retinal capillary plexus (Fig. 3a, Fig. 3ba). In addition, there was resolution of CME and SRF on OCT and reperfusion of previously occluded arterioles on IVFA (Fig. 5b, Fig. 5cb–c). Anti-cardiolipin antibody and anti-beta 2 glycoprotein antibody titers normalized. At 4-month follow-up, there was resolution of all cotton wool spots on fundus exam (Fig. 6). However, there were new areas of vascular leakage on IVFA as his oral prednisone was tapered to 15 mg once daily while on mycophenolate 1500 mg twice daily. Rituximab infusions (1000 mg) were initiated at this follow-up visit with a second infusion 2 weeks later in attempt to taper the patient off systemic steroids. The patient was successfully tapered off systemic steroids by month 6 of follow-up. At 10-month follow-up, the patient showed complete resolution of vascular leakage on IVFA (Fig. 7). On final follow-up, 20 months after initial presentation, the patient's VA remained at 20/20 in both eyes on a regimen of aspirin 81 mg once daily, mycophenolate mofetil 1500 mg twice daily, and off of systemic steroids and anti-coagulation therapy. Anti-cardiolipin antibody, anti-beta 2 glycoprotein, anti-Xa activity remained negative.
Fig. 5a.
OCT angiography of the left eye at 3-month follow up showing reconstitution of flow signal in the macula.
Fig. 5b.
OCT of the left eye at 3-month follow up showing resolution of CME and SRF, along with improvement in retina thickening.
Fig. 5c.
Late fluorescein angiography of the left eye showing reperfusion of previously occluded arterioles and improved vascular leakage.
Fig. 6.
Fundus photo of the left eye at 4-month follow up showing resolution of cotton wool spots.
Fig. 7.
Late fluorescein angiography of the left eye at 10-month follow up demonstrating complete resolution of vascular leakage.
2. Discussion
The prevalence of retinopathy in SLE ranges from 3 to 29% in the literature.8, 9, 10 Lupus-associated retinal microangiopathy is the most mild manifestation of posterior segment disease presenting with cotton wools spots, intraretinal hemorrhage, and areas of focal vascular sheathing.11 Microangiopathy accounts for 80% of all lupus-associated retinopathy in one review.11 However, the most severe form of lupus retinopathy is vaso-occlusive disease associated with anti-phospholipid syndrome (APLS) which presents with widespread capillary non-perfusion, central retinal artery or vein occlusions, multiple branch retinal artery or vein occlusions, and the resulting neovascular sequelae of severe ocular ischemia.6 Vaso-occlusive retinopathy is a rare, but a well-documented manifestation of SLE and APLS with widely reported poor visual prognosis despite systemic steroid and immunomodulatory therapy.6,7,12, 13, 14, 15, 16, 17 Jabs et al. reported a poor prognosis in their case series despite treatment with a variety of oral (60–80 mg once daily) and IV (500 mg once daily) steroids, warfarin (40 mg every other day), cyclophosphamide (75–100 mg per day), and/or pan-retinal photocoagulation with a final visual acuity of 20/60 or worse in 55% of affected eyes. More impressive is that this vision loss was CF or worse in 45% of affected eyes.6 In this series of 11 patients, only two affected eyes from the same patient recovered to 20/20 vision, but both eyes required pan-retinal photocoagulation for extensive non-perfusion complicated by neovascularization and vitreous hemorrhage.6 Au et al. reviewed 47 cases of SLE and APLS related vaso-occlusive retinopathy published in the literature and found that 80% of cases had a final visual acuity of 20/60 or worse. The authors contributed a significant extent of this visual loss to 41% of the cases developing neovascularization and/or vitreous hemorrhage from retinal non-perfusion and ischemia. Au et al. go on to conclude that overall the vaso-occlusive process from APLS is irreversible and treatment should be aimed at preventing complications arising from neovascularization and future episodes.7
Treatment of vaso-occlusive retinopathy from APLS and SLE is controversial and there is no one therapy or combination of therapies that is well supported by the current literature. Immunosuppressive therapy with IV or oral steroids, hydroxychloroquine, azathioprine, methotrexate, mycophenolate mofetil, cyclophosphamide, and rituximab have all been advocated for as effective mono- or combination therapy.1 Anti-platelet and anti-coagulation therapies are supported in the literature for systemic thromboembolic disease.18 However, there is no clear benefit from any of these therapies in the treatment of retinal vaso-occlusive disease and in the vast majority of cases treated there is no improvement in vision or there is progressive visual decline.6,7,12, 13, 14, 15 Furthermore, in most cases where immunosuppressive therapy is used it is confounded by other concurrent therapies, making it difficult to interpret which is truly effective.
Our patient presented with sudden vision loss and was found to have signs of vaso-occlusive retinopathy in the setting of known lupus and a clinically significant antiphospholipid profile allowing for rapid diagnosis. He was then immediately and sequentially started on IV steroids, IMT, and therapeutic anti-coagulation. He remained on aspirin. The mechanisms relating SLE-associated vasculitis and APLS thrombosis are complex and not fully understood.19 It has been hypothesized that active vasculitis may disrupt the vascular endothelium and expose phospholipids that can then serve as antigenic stimulus for anti-phospholipid production or a binding target for circulating anti-phospholipid anti-bodies, thus triggering inflammatory pathways and thrombosis.19 Given our patients IVFA findings, we attribute our patient's presentation to a combination of SLE vasculitis and vaso-occlusive retinopathy secondary to APLS, necessitating therapy with both immune suppression and anti-coagulation. Initially there was clinical improvement in the number and size of the cotton wool spots, followed by incremental improvement in VA. Serial IVFA showed reperfusion of previously occluded arterioles and improvement in vascular leakage. Serial OCTA showed return of retinal capillary flow. Although, rare cases of visual recovery have been reported in the literature, to our knowledge this is the first patient to receive concurrent therapy with pulsed IV steroids, therapeutic anti-coagulation, immunosuppressive therapy with mycophenolate, and anti-platelet therapy followed by rituximab to show complete visual recovery, vascular reperfusion as evidenced by IVFA, and return of capillary flow as shown on OCTA.
3. Conclusion
In summary, we present a case of vaso-occlusive retinopathy in a patient with systemic lupus erythematosus and a clinically significant anti-phospholipid panel, thus meeting criteria for anti-phospholipid syndrome. He was treated with intravenous methylprednisolone, mycophenolate motefil, rituximab, aspirin, and enoxaparin. The patient not only had great recovery of visual acuity, but also demonstrated reperfusion and reconstitution of flow in the retinal capillary network suggesting that this vaso-occlusive disease is not irreversible if the diagnosis is made promptly and intensive therapy is initiated.
3.1. Patient consent
Consent to publish the case report was not obtained. The report does not contain any personal information that could lead to identification of the patient.
Funding sources
No funding or grant support.
Disclosures
The following authors have no financial disclosures: JD, AZ, PL, CL.
4. Authorship
All authors attest that they meet the current ICMJE criteria for Authorship.
Acknowledgements
None.
References
- 1.Silpa-archa S., Lee J.J., Foster C.S. Ocular manifestations in systemic lupus erythematosus. Br J Ophthalmol. 2016;100(1):135–141. doi: 10.1136/bjophthalmol-2015-306629. [DOI] [PubMed] [Google Scholar]
- 2.Peponis V., Kyttaris V.C., Tyradellis C., Vergados I., Sitaras N.M. Ocular manifestations of systemic lupus erythematosus: a clinical review. Lupus. 2006;15(1):3–12. doi: 10.1191/0961203306lu2250rr. [DOI] [PubMed] [Google Scholar]
- 3.Acharya N., Pineda R., Uy H.S., Foster C.S. Discoid lupus erythematosus masquerading as chronic blepharoconjunctivitis. Ophthalmology. 2005;112(5):e19–23. doi: 10.1016/j.ophtha.2005.01.035. [DOI] [PubMed] [Google Scholar]
- 4.Miyakis S., Lockshin M.D., Atsumi T. International consensus statement on an update of the classification criteria for definite antiphospholipid syndrome (APS) J Thromb Haemost JTH. 2006;4(2):295–306. doi: 10.1111/j.1538-7836.2006.01753.x. [DOI] [PubMed] [Google Scholar]
- 5.Taraborelli M., Leuenberger L., Lazzaroni M.G. The contribution of antiphospholipid antibodies to organ damage in systemic lupus erythematosus. Lupus. 2016;25(12):1365–1368. doi: 10.1177/0961203316637431. [DOI] [PubMed] [Google Scholar]
- 6.Jabs D.A., Fine S.L., Hochberg M.C., Newman S.A., Heiner G.G., Stevens M.B. Severe retinal vaso-occlusive disease in systemic lupus erythematosus. Arch Ophthalmol. 1986;104(4):558–563. doi: 10.1001/archopht.1986.01050160114025. [DOI] [PubMed] [Google Scholar]
- 7.Au A., O'Day J. Review of severe vaso-occlusive retinopathy in systemic lupus erythematosus and the antiphospholipid syndrome: associations, visual outcomes, complications and treatment. Clin Exp Ophthalmol. 2004;32(1):87–100. doi: 10.1046/j.1442-9071.2004.00766.x. [DOI] [PubMed] [Google Scholar]
- 8.Lanham J.G., Barrie T., Kohner E.M., Hughes G.R. SLE retinopathy: evaluation by fluorescein angiography. Ann Rheum Dis. 1982;41(5):473–478. doi: 10.1136/ard.41.5.473. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Gold D.H., Morris D.A., Henkind P. Ocular findings in systemic lupus erythematosus. Br J Ophthalmol. 1972;56(11):800–804. doi: 10.1136/bjo.56.11.800. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Davies J., Rao P. Ocular manifestations of systemic lupus erythematosus. Curr Opin Ophthalmol. 2008;19(6):512–518. doi: 10.1097/icu.0b013e3283126d34. [DOI] [PubMed] [Google Scholar]
- 11.Stafford‐Brady F.J., Urowitz M.B., Gladman D.D., Easterbrook M. Lupus retinopathy. Arthritis Rheum. 1988;31(9):1105–1110. doi: 10.1002/art.1780310904. [DOI] [PubMed] [Google Scholar]
- 12.Bomar J.G., Branson S.V., McClintic J., Kurup S.K. Reperfusion of retinal vasculature with improved visual acuity in ischemic occlusive vasculitis. JAMA Ophthalmol. 2016;134(4):466–467. doi: 10.1001/jamaophthalmol.2015.6164. [DOI] [PubMed] [Google Scholar]
- 13.Dhirani N.A., Ahluwalia V., Somani S. Case of combination therapy to treat lupus retinal vasculitis refractory to steroids. Can J Ophthalmol. 2017;52(1):e13–e15. doi: 10.1016/j.jcjo.2016.07.027. [DOI] [PubMed] [Google Scholar]
- 14.Monov S., Hristova R., Dacheva R. Acute necrotizing retinal vasculitis as onset of systemic lupus erythematosus. Medicine (Baltim) 2017;96(2) doi: 10.1097/MD.0000000000005754. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Storey P., Ter-Zakarian A., Rao N., Rodger D. Severe bilateral retinal vascular occlusion as first presentation of systemic lupus erythematosus and antiphospholipid syndrome. Retin Cases Brief Rep. 2017;11:S44. doi: 10.1097/ICB.0000000000000398. [DOI] [PubMed] [Google Scholar]
- 16.Durukan A.H., Akar Y., Bayraktar M.Z., Dinc A., Faruk Sahin O. Combined retinal artery and vein occlusion in a patient with systemic lupus erythematosus and antiphospholipid syndrome. Can J Ophthalmol. 2005;40(1):87–89. doi: 10.1016/s0008-4182(05)80126-7. [DOI] [PubMed] [Google Scholar]
- 17.Hwang H.S., Kang S. Combined central retinal vein and artery occlusion in systemic lupus erythematosus patient. Retin Cases Brief Rep. 2012;6(2):187–188. doi: 10.1097/ICB.0b013e31822476d7. [DOI] [PubMed] [Google Scholar]
- 18.Ruiz-Irastorza G., Cuadrado M.J., Ruiz-Arruza I. Evidence-based recommendations for the prevention and long-term management of thrombosis in antiphospholipid antibody-positive patients: report of a task force at the 13th International Congress on antiphospholipid antibodies. Lupus. 2011;20(2):206–218. doi: 10.1177/0961203310395803. [DOI] [PubMed] [Google Scholar]
- 19.Lally L., Sammaritano L.R. Vasculitis in antiphospholipid syndrome. Rheum Dis Clin N Am. 2015;41(1):109–123. doi: 10.1016/j.rdc.2014.09.009. ix. [DOI] [PubMed] [Google Scholar]