Abstract
Purpose
We report a case of rhino-orbital-cerebral mucormycosis (ROCM) with focal anterior cerebritis treated favorably with retrobulbar amphotericin B and systemic antifungals.
Observations
A 55-year-old diabetic male presented to the emergency department with left sided proptosis, left temple headache, maxillary sinus pain, and diplopia of 3 days duration. Biopsy results from the left middle turbinate, ethmoid, and maxillary sinus revealed broad and irregular non-septate hyphae consistent with mucormycosis. Despite treatment with intravenous antifungals and endoscopic debridement of the sinuses, his condition did not improve. Disease progression included the development of left ophthalmoplegia and left-sided cerebritis. The patient received retrobulbar injection of deoxycholate amphotericin B with eventual disease resolution, without exenteration.
Conclusions
We present a case of ROCM with associated cerebritis that responded to retrobulbar amphotericin B, without exenteration.
Keywords: Amphotericin B, Deoxycholate, Mucormycosis, Orbital, Retrobulbar, Rhino-orbital-cerebral
1. Introduction
Mucormycosis is an aggressive infection with a high risk of mortality.1 The causative organism is from the Mucoracea family with Mucor, Rhizopus, and Absidia species being commonly implicated.2 Immunocompromised patients, especially those with poorly controlled diabetes carry the highest risk of developing mucormycosis.3, 4, 5 Fungi spores are inhaled causing a sinusitis which eventually spreads to adjacent structures such as the orbit (rhino-orbital mucormycosis).6 Progressive orbital disease can lead to involvement of the brain (rhino-orbital-cerebral mucormycosis; ROCM) and nearby structures.6 The mainstay of treatment involves reversal of the patient's immunocompromised state, aggressive treatment with systemic antifungals and surgical debridement.7 With unclear guidelines regarding the optimal timing for exenteration, given this procedure's disfiguring outcome, alternative methods of treatment should be considered. A unique and potentially globe sparing approach is retrobulbar antifungal injection. We report the successful use of this technique in a case of ROCM with associated cerebritis.
2. Case report
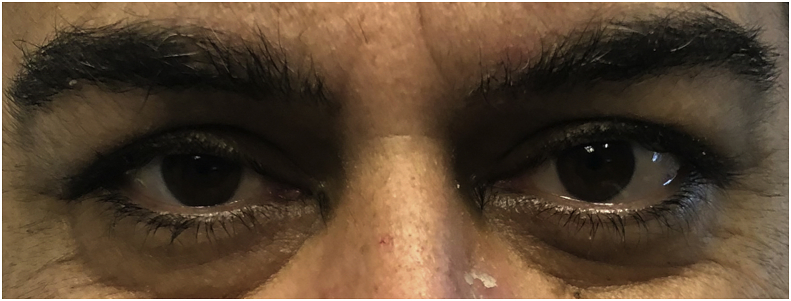
A 55-year-old Hispanic male with poorly controlled type II diabetes mellitus (HgbA1c 15.3%) presented to the emergency department with left sided proptosis, left temple headache, maxillary sinus pain and diplopia of three days duration (Fig. 1).
Fig. 1.
Initial presentation. Note the proptosis in the left eye compared to the non-proptotic right eye.
Best corrected visual acuity was 20/20 in the right eye (OD) and 20/20 in the left eye (OS). Extraocular movements were full OD and reduced OS (−2 in elevation and depression in both adduction and abduction). The pupillary exam was normal. Visual inspection revealed a proptotic left eye. Hertel measurements of the right and left eye were 17 mm and 23 mm, respectively. Confrontational visual fields, color examination, and slit-lamp biomicroscopy were normal in both eyes. Dilated fundus exam revealed moderate non-proliferative diabetic retinopathy without diabetic macular edema. Oral examination demonstrated a left palatal ulcer. Serologic testing for HIV was negative.
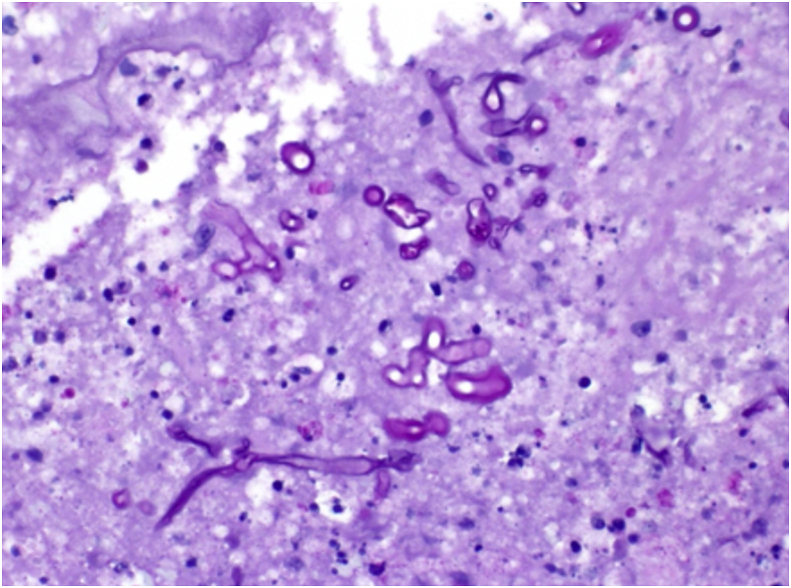
Maxillofacial computed tomography (CT) demonstrated both maxillary and sphenoid sinusitis, with evidence of bony destruction. The patient was admitted and underwent urgent bilateral endoscopic sinus surgery, including maxillary antrostomy, total ethmoidectomy, left sphenoidectomy, and palatal biopsy on hospital day 1. Biopsy specimens demonstrated pauci-septate hyphae in the left middle turbinate, ethmoid, and maxillary sinus confirming the diagnosis of mucormycosis (Fig. 2). With input from the infectious disease service, the patient was initiated on intravenous liposomal amphotericin B 750 mg every 24 hours, intravenous micafungin 150 mg every 24 hours, and oral posaconazole 300 mg every 24 hours.
Fig. 2.
Hematoxylin and Eosin (400x) stained slide of maxillary sinus tissue demonstrating pauci-septate hyphae confirming the diagnosis of mucormycosis.
On hospital day 3, a repeat CT revealed the development of orbital involvement with a left medial wall abscess, left orbital floor subperiosteal abscess, as well as an abscess in the left inferior rectus muscle belly. Uncorrected VA at this time was 20/100 in the left eye. The patient was taken back to the operating room for a second sinus debridement on hospital day 4.
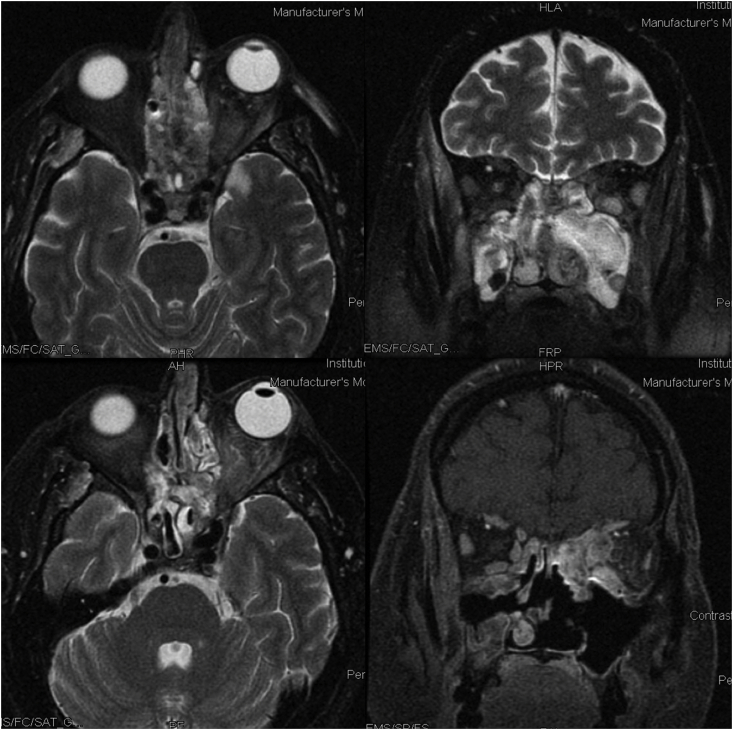
Following the second debridement, the patient developed a complete left external ophthalmoplegia and eyelid ptosis (Fig. 3). The pupil was noted to be fixed and dilated at 5 mm. There was no afferent pupillary defect by reverse. Uncorrected visual acuity in the left eye was 20/200. Emergent MRI of the brain and orbits excluded a cavernous sinus thrombosis. However, the MRI did reveal new left sided temporal lobe cerebritis (Fig. 4).
Fig. 3.
External ophthalmoplegia after repeat endoscopic debridement of the left maxillary sinus. Note the chemosis located inferiorly following retrobulbar injection of amphotericin B.
Fig. 4.
(Top left and top right images) MRI T2 axial and coronal views demonstrating orbital disease and cerebritis; (Bottom left). Repeat MRI T2 axial demonstrating post injection improvement of sinus disease and cerebritis; (Bottom right) T1 post-contrast with fat saturation showing residual inflammatory changes in the medial orbit.
Given evidence of progression on systemic treatment in the presence of a sighted eye and cerebritis, the patient was treated locally with retrobulbar deoxycholate amphotericin B (1 ml of 3.5 mg/ml AMB deoxycholate with an antecedent retrobulbar injection of anesthetic comprised of 2 ml of 2% lidocaine). The patient was given two retrobulbar injections on hospital day 6 and 9. BCVA improved following the first injection to 20/50 and further improved to 20/40 after the second injection. Following the injections, the patient developed an inflammatory response manifested by yellow-tinged inferior conjunctival chemosis, which persisted for 1 week (Fig. 3).
The patient remained clinically stable with no further evidence of progression. The inpatient medicine team continued aggressive antifungal treatment as well as blood sugar control, lowering his HgBA1c to 6.0%. Repeat MRI demonstrated resolution of the left temporal cerebritis. By 3 months, the patient's ptosis completely resolved. There was marked improvement of the ophthalmoplegia, though the −4 deficit in abduction persisted. 15 months following initial presentation, the patient continued to be treated with oral antifungals per the infectious disease specialist.
3. Discussion
Mucormycosis is a potentially life-threatening condition which requires prompt recognition and treatment. Challenges in treating ROCM is due in part to its underlying pathogenesis in which endothelial cell damage leads to vascular thrombosis decreasing the efficacy of systemic antifungals.8 In the setting of progressive orbital disease, exenteration may be recommended; however, there are no clear guidelines regarding optimal timing for exenteration.9 Although potentially life-saving, exenteration carries significant complications including certain blindness, cosmetic disfigurement and psychosocial trauma should the patient survive.10
Management of mucormycosis consists of immediate initiation of systemic anti-fungals. Liposomal amphotericin B is often the antifungal agent of choice due to superior survival rates and the ability to achieve higher blood levels without the immediate nephrotoxic side effects commonly seen with the deoxycholate formulation.11 It is a polyene antifungal, and acts by binding to the ergosterol component of cell membranes forming pores that lead to the loss of cations and eventual cell death.12 Amphotericin B lipid complex is another lipid derivative polyene which has been considered in the treatment of mucormycosis; however, compared to liposomal amphotericin B, it is not able to penetrate the central nervous system to the same extent as the liposomal derivative.11 Our patient was treated initially with intravenous liposomal amphotericin B; however, he developed nephrotoxicity. Throughout his treatment, the amphotericin B was intermittently held to improve renal function and supplemented with the anti-fungals, micafungin and posaconazole. Reports of combination amphotericin B and posaconazole have been reported to achieve clinical success with early initiation of this agent.6 In animal models, combination amphotericin B and micafungin has been demonstrated to work synergistically with improved overall survival rates.11 In our patient, the unavoidable intermittent use of amphotericin B, despite the addition of micafungin and posaconazole, may have contributed, in part, to the progression of his disease suggesting the significance of consistent amphotericin B in the eradication of the causative organism.
In addition to systemic antifungal treatment and reversal of the patient's immunocompromised state, surgical debridement serves a critical role by removing devitalized tissue to allow an adequate concentration of the antifungal to reach the area of active infection; without this crucial step, prognosis is poor.2,8 Conservative orbital debridement with local antifungal irrigation is a viable option as well.13,14 In our patient, the maintenance of vision as well as the radiographic appearance of orbital inflammation rather than necrosis informed our limited surgical approach to the orbit. Despite these efforts, the disease progressed and manifested with an external ophthalmoplegia and cerebritis of his left temporal lobe.
Faced with progressive disease on maximal systemic medication and after sinus debridement, retrobulbar anti-fungal treatment was selected as a non-surgical option to potentially halt orbital progression. Case reports of retro-bulbar antifungal injection in the treatment of orbital fungal infections have been reported15, 16, 17, 18 and one recent report by Hirabayashi et al. detailed the successful use of retrobulbar amphotericin B deoxycholate in ROCM.9 After the administration of retrobulbar amphotericin B in our patient, orbital progression halted and the cerebritis resolved. To our knowledge resolution of cerebritis associated with retrobulbar amphotericin B injection has not been previously reported in the literature. This association is relevant given the proximity of the cerebritis to the orbital infusion although a definitive cause and effect cannot be ascertained as the patient was receiving concurrent systemic therapy. Further studies will need to be undertaken to establish a definitive correlation. However, retrobulbar antifungal injection is a viable option to consider in halting orbital progression and providing an opportunity to avoid exenteration and spare the eye.19,20
The administration of retrobulbar amphotericin B injection may cause a post-injection pro-inflammatory state mediated by increased cytokine expression and increased edema with development of an orbital compartment syndrome. This has been described with the use of the deoxycholate formulation of amphotericin B.9 Our patient experienced a mild form of this reaction with inferior conjunctival chemosis lasting 1 week. Close monitoring of the patient's orbital examination including intraocular pressure (IOP) testing was critical. Should a significant orbital compartment syndrome develop, IOP should be managed accordingly, and if need be, lateral canthotomy and superior and inferior cantholysis or even the judicious use of an IL-6 inhibitor such as Tocilizumab21 can be considered. The development of an orbital compartment syndrome may be mitigated by surgically induced bony decompression/debridement.
4. Conclusions
ROCM is best managed by a multidisciplinary team. Immediate initiation of intravenous anti-fungals, reversing the patient's immunocompromised state, and endoscopic surgical debridement are the basis of treatment. In the setting of progressive orbital disease, retrobulbar amphotericin B treatment should be considered as an option prior to exenteration. Though the injection carries its own risks, it may be a successful therapeutic alternative to conventional therapy and allows for orbit and globe preservation.
Author contribution
The corresponding author had full access to all the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis.
5. Patient consent
The patient(s)/patient's legal guardian consented to publication of the case in writing/orally.
Funding
No funding was received for this work.
Declaration of competing interest
No conflict of interest exists.
Acknowledgements
No funding or grant support. All authors have no financial disclosures. All authors attest that they meet the current ICMJE criteria for Authorship.
References
- 1.Spellberg B., Kontoyiannis D., Fredricks D. Risk factors for mortality in patients with mucormycosis. Med Mycol. 2012;50(6):611–618. doi: 10.3109/13693786.2012.669502. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Wali U., Balkhair A., Al-Mujaini A. Cerebro-rhino orbital mucormycosis: an update. J Infect Public Health. 2012;5:116–126. doi: 10.1016/j.jiph.2012.01.003. [DOI] [PubMed] [Google Scholar]
- 3.Yohai R.A., Bullock J.D., Aziz A.A., Markert R.J. Survival factors in rhino-orbital-cerebral mucormycosis. Surb Ophthalmol. 1994;39:3–22. doi: 10.1016/s0039-6257(05)80041-4. [DOI] [PubMed] [Google Scholar]
- 4.Ferguson B.J. Mucormycosis of the nose and paranasal sinuses. Otolaryngol Clin. 2000;33:349–365. doi: 10.1016/s0030-6665(00)80010-9. [DOI] [PubMed] [Google Scholar]
- 5.Ferry A.P., Abedi S. Diagnosis and management of rhino-orbitocerebral mucormycosis (phycomycosis). A report of 16 personally observed cases. Ophthalmology. 1993;90:1096–1104. doi: 10.1016/s0161-6420(83)80052-9. [DOI] [PubMed] [Google Scholar]
- 6.Zhang J., Kim J.D., Beaver H.A. Rhino-orbital mucormycosis treated successfully with posaconazole without exenteration. Neuro Ophthalmol. 2013;37:198–203. doi: 10.3109/01658107.2013.809463. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Bellazreg F., Hattab Z., Mansouri S. Outcome of mucormycosis after treatment: report of five cases. New Microbe and New Infect. 2015;6:49–52. doi: 10.1016/j.nmni.2014.12.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Mohamed M.S., Abdel-Motaleb H.Y., Mobarak F.A. Management of rhino-orbital mucormycosis. Saudi Med J. 2015;36:865–868. doi: 10.15537/smj.2015.7.11859. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Hirabayashi K.E., Kalin-Hajdu E., Brodie F.L. Retrobulbar injection of amphotericin B for orbital mucormycosis. Ophthalmic Plast Reconstr Surg. 2017;33:e94–e97. doi: 10.1097/IOP.0000000000000806. [DOI] [PubMed] [Google Scholar]
- 10.Ackuaku-Dogbe E.M., Biritwum R.B., Briamah Z.I. Psycho-social challenges of patients following orbital exenteration. East Afr Med J. 2012;89:385–389. [PubMed] [Google Scholar]
- 11.Spellberg B., Ibrahim A., Roilides E. Combination therapy for mucormycosis: why, what, and how? Clin Infect Dis. 2012;54(S1):S73–S78. doi: 10.1093/cid/cir885. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Noor A, Preuss CV. Antifungal Membrane Function Inhibitors (Amphotericin B) [Update 2019 Sep 2]. (In: Stat Pearls [Internet]).
- 13.Seiff S.R., Choo P.H., Carter S.R. Role of local amphotericin B therapy for sino-orbital fungal infections. Ophthalmic Plast Reconstr Surg. 1999;15(1):28‐31. doi: 10.1097/00002341-199901000-00007. [DOI] [PubMed] [Google Scholar]
- 14.Joos Z.P., Patel B.C. Intraorbital irrigation of amphotericin B in the treatment of rhino-orbital mucormycosis. Ophthalmic Plast Reconstr Surg. 2017;33(1) doi: 10.1097/IOP.0000000000000377. e13‐e16. [DOI] [PubMed] [Google Scholar]
- 15.Luna J.D., Ponssa X.S., Rodríguez S.D., Luna N.C., Juárez C.P. Intraconal amphotericin B for the treatment of rhino-orbital mucormycosis. Ophthalmic Surg Laser. 1996;27(8):706‐708. [PubMed] [Google Scholar]
- 16.Colon-Acevedo B., Kumar J., Richard M.J. The role of adjunctive therapies in the management of invasive sino-orbital infection. Ophthalmic Plast Reconstr Surg. 2015:401–405. doi: 10.1097/IOP.0000000000000488. [DOI] [PubMed] [Google Scholar]
- 17.Mainville N., Jordan D.R. Orbital aspergillosis treated with retrobulbar amphotericin B. Orbit. 2012;31:15–17. doi: 10.3109/01676830.2011.603596. [DOI] [PubMed] [Google Scholar]
- 18.Wakabayashi T., Oda H., Kinoshita N. Retrobulbar amphotericin B injections for treatment of invasive sino-orbital aspergillosis. Jpn J Ophthalmol. 2007;51:309–311. doi: 10.1007/s10384-007-0437-2. [DOI] [PubMed] [Google Scholar]
- 19.Kalin-Hajdu E., Hirabayashi K.E., Vagefi M.R., Kersten R.C. Invasive fungal sinusitis: treatment of the orbit. Curr Opin Ophthalmol. 2017;28(5):522–533. doi: 10.1097/ICU.0000000000000394. [DOI] [PubMed] [Google Scholar]
- 20.Mainville N., Jordan D.R. Orbital aspergillosis treated with retrobulbar amphotericin B. Orbit. 2012;31(1):15–17. doi: 10.3109/01676830.2011.603596. [DOI] [PubMed] [Google Scholar]
- 21.Tanaka T., Narazaki M., Kishimoto T. Immunotherapeutic implications of IL-6 blockade for cytokine storm. Immunotherapy. 2016;8(8):959‐970. doi: 10.2217/imt-2016-0020. [DOI] [PubMed] [Google Scholar]