Abstract
Introduction
A late aortic aneurysm at the site of previous open surgery for coarctation of the aorta (CoA) is a life threatening complication. Several strategies have been reported, however, these strategies have issues. This is the report of a case involving successful ascending to descending aortic bypass concomitant with endovascular embolisation for a pseudoaneurysm.
Report
The patient was a 23 year old man with a history of patch aortoplasty for coarctation of the aorta (CoA) via a left thoracotomy and patch closure of a ventricular septal defect. Enhanced computed tomography (CT) angiography performed in 2014 revealed a pseudoaneurysm at the site of the previous patch aortoplasty. CT also revealed a hypoplastic and severely kinked aortic arch that made it difficult to perform conventional thoracic endovascular aortic repair for this aneurysm. Therefore in order to prevent rupture, a combination of ascending to descending aortic bypass and endovascular embolisation using Amplatzer vascular plugs and coils was employed. Transection of the aortic arch and transposition of the left subclavian artery were performed to prevent antegrade flow into the aneurysm.
Discussion
The aneurysm was successfully excluded without complications. CT performed three years after the operation showed that the pseudoaneurysm had shrunk completely. Extra-anatomic bypass concomitant with endovascular embolisation for a late coarctation patched site aneurysm might be an alternative strategy that should be carefully considered in specific cases.
Keywords: Ascending to descending aortic bypass, Coarctation of the aorta, Endovascular embolisation, Open surgery, Pseudoaneurysm
Highlights
-
•
A case of late coarctation patched site pseudoaneurysm is presented.
-
•
Ascending to descending aortic bypass was performed successfully.
-
•
The aneurysm was treated successfully by endovascular embolisation.
-
•
Follow up computed tomography showed that the pseudoaneurysm had shrunk completely.
-
•
This approach might be an alternative strategy that should be carefully considered.
Introduction
A late aortic aneurysm at the site of previous open surgery for coarctation of the aorta (CoA) is a life threatening complication. Conservative management is associated with a considerable mortality rate,1 therefore, surgical intervention should be considered in such cases. Several strategies, including open surgical2 and endovascular repair,3,4 have been reported. However, these strategies have some issues. Redo open surgery is considered technically challenging because of its high morbidity and mortality.1 Thoracic endovascular aortic repair (TEVAR) has anatomical limitations. This report describes a case involving a combination of ascending to descending aortic bypass and endovascular embolisation for a late CoA patched site pseudoaneurysm. This approach was used to prevent previously reported issues and to safely treat the aneurysm. To the present authors’ knowledge, this is the first such case in the literature.
Case report
A 23 year old man with a history of polytetrafluoroethylene patch aortoplasty for CoA via a left thoracotomy one month after birth and patch closure for ventricular septal defect (VSD) at one year of age, was followed at the study institution. In April 2014, enhanced computed tomography angiography (CTA) revealed a pseudoaneurysm at the site of the previous CoA patch repair (Fig. 1). The aortic arch was hypoplastic, only 15 mm in diameter at the narrowest part, and severely kinked (Fig. 1). He was also followed for a bicuspid aortic valve using echocardiography. The peak velocity at the aortic valve was 1.59 m/s, and the peak pressure gradient at the aortic valve was only 10 mmHg, which had not deteriorated adversely over the recent past. No residual VSD shunting was noted on pre-operative echocardiography. There was no need to treat the valve, and therefore it was decided to treat only the late CoA patched site aneurysm. To exclude the pseudoaneurysm, a combination of ascending to descending aortic bypass and endovascular embolisation was planned. Simultaneous transection of the aortic arch and transposition of the left subclavian artery were planned in order to prevent antegrade flow into the aneurysm.
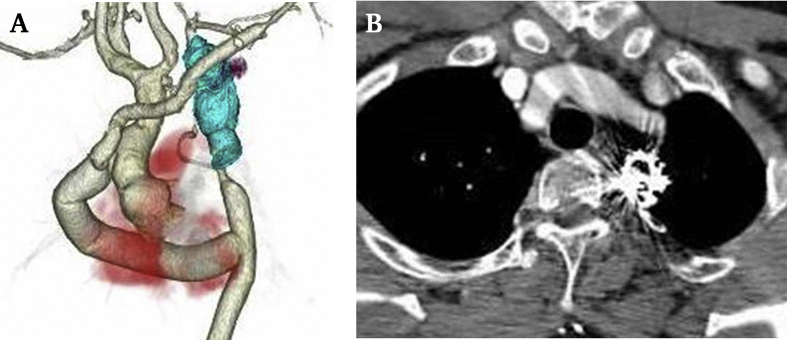
Figure 1.
Pre-operative three dimensional computed tomography shows a pseudoaneurysm of the proximal descending thoracic aorta and shows that the aortic arch is hypoplastic and severely kinked.
Open surgical procedure
A median sternotomy was performed, and the right femoral artery (FA) exposed and cannulated for cardiopulmonary bypass (CPB). The left axillary artery was also exposed through a infraclavicular incision, and an 8 mm Dacron graft (Gelweave; Teromo, Tokyo, Japan) was anastomosed end to side to transpose the left subclavian artery. Following the establishment of CPB, the apex of the left ventricle was lifted to facilitate exposure of the posterior pericardium. A T-shaped incision was made in the posterior pericardium, and the descending aorta was exposed. After clamping of the descending aorta, a longitudinal aortotomy was performed. A 20 mm Dacron graft (Hemashield Platinum; Maquet, Wayne, NJ, USA) was anastomosed end to side to the descending aorta. This graft was led to the lateral side of the right atrium, which was passed under the inferior vena cava. A single branched 20 mm Dacron graft (Hemashield Platinum; Maquet) was anastomosed end to end to the ascending aorta, similar to the distal anastomosis. These two grafts were then joined end to end, and the ascending to descending aortic bypass was completed. Subsequently, the aortic arch was clamped, and transection was attempted in order to prevent antegrade blood flow into the pseudoaneurysm. This resulted in massive bleeding that was difficult to control because of extreme aortic wall fragility. Therefore, transection of the aortic arch was performed under deep hypothermic circulatory arrest at 20°C. Finally, the 8 mm Dacron graft anastomosed to the left axillary artery was led to the anterior mediastinum and anastomosed end to end to the branch of the 20 mm graft, completing the transposition of the left subclavian artery.
Endovascular procedure
Endovascular embolisation was performed simultaneously with open surgical repair. The right FA was used for embolisation of the pseudoaneurysm. After accurately confirming the locations of the left subclavian artery, descending aorta, and pseudoaneurysm with intra-operative angiography, three Amplatzer vascular plugs (AVPs; AVP2; St. Jude Medical Inc., St. Paul, MN, USA) were deployed between the left subclavian artery and the proximal descending aorta. Additionally, Penumbra coils (Medicos-Hirata, Tokyo, Japan) and 0.035 inch diameter Nester coils (Cook Medical, Bloomington, IN, USA) were deployed to fill the gap between the AVPs to exclude the pseudoaneurysm (Fig. 2).
Figure 2.
Intra-operative angiography shows that Amplatzer vascular plugs (AVPs) have been deployed between the left subclavian artery and the proximal descending thoracic aorta. Coils are also deployed to fill the gap between the AVPs. There is no evidence of anastomotic stenosis of the ascending to descending aortic bypass or the graft to left axillary artery bypass.
Post-operative course
Post-operative enhanced CTA revealed that the sac of the pseudoaneurysm was completely thrombosed (Fig. 3A). The patient had a pleural effusion, which prolonged hospitalisation, but he was discharged 26 days after the operation without other major complications. Enhanced CTA performed three years post-operatively revealed that the aneurysm sac had shrunk completely (Fig. 3B).
Figure 3.
(A) Post-operative three dimensional computed tomography (CT) shows that the sac of the pseudoaneurysm has thrombosed. The two bypasses are patent without evidence of anastomotic stenosis. (B) CT performed three years after the operation shows that the aneurysm sac had shrunk completely.
Discussion
Late aortic aneurysm formation after previous open CoA repair is a life threatening complication. The incidence of aneurysm formation is approximately 7–47% according to several authors.1,2,5,6 The mortality rate with conservative observation of these aneurysms is high because of aneurysm rupture. Knyshov et al.1 reported that, without re-operation, 18 of 48 patients died as a result of haemorrhage. Therefore, surgical intervention should be considered in such a situation.
For a young adult, direct repair of a CoA patched site pseudoaneurysm via a left thoracotomy should be the first choice. However, a repeat direct approach is considered technically challenging because of the high mortality rate.1 The incidence of complications associated with a redo left thoracotomy is high, and it has been reported that the post-operative respiratory complication rate can reach approximately 20–30%.7,8 In the present case, adhesions in the chest cavity and a saccular lesion of the aneurysm arising toward the left side made it difficult and dangerous to expose the proximal site of the aneurysm through a left thoracotomy. In addition, if the aortic wall is fragile because of a hypoplastic aortic arch, it has to be extensively dissected to the ascending aorta. Additionally, in this case, which involved not only a left thoracotomy but also a median sternotomy, extensive dissection to the ascending aorta via a left thoracotomy was considered extremely difficult. On the other hand, a median sternotomy alone cannot be considered to expose the distal site of the aneurysm. Thus, the risk associated with direct repair of the patched site pseudoaneurysm in this patient was considered high.
Recently, TEVAR has been considered a feasible and attractive procedure for these aneurysms3,4 because of its reduced invasiveness and good short and long term results.3,4 Unfortunately, in the present case, TEVAR was contraindicated because of the characteristic morphology of the aortic arch (hypoplastic and severely kinked), which would make it difficult to secure an adequate sealing zone. In addition, the distance between left subclavian artery orifice and the pseudoaneurysm was short and the diameter of the aorta below the left subclavian artery orifice was small and unsuitable as an adequate landing zone for TEVAR.
Thus, ascending to descending aortic bypass concomitant with pseudoaneurysm embolisation was adopted as an alternative to the conventional strategy. Extra-anatomic bypass is usually indicated in high surgical risk patients. Reliability in the long term is the major concern, and it remains controversial to perform this procedure in a young patient. However, considering the excellent outcomes reported by Said et al.,9 extra-anatomic bypass might be safe and acceptable even in a young patient. In the present case, the embolised aneurysm sac shrank completely three years after the surgery, and this result was considered to reduce the risk of aneurysm rupture at least in the mid term.
Transection of the aortic arch appears to be a logical and reliable approach to prevent antegrade blood flow into the aneurysm, but it can be fatal and requires risky techniques (circulatory arrest with deep hypothermia). Considering the characteristic anatomy of the aortic arch, an occlusion cuff could have been placed or embolisation performed to prevent massive bleeding during the operation. Weakness of the proximal aortic arch stump and the prosthetic graft anastomosis remain an important clinical problem, which could affect the prognosis in the long term. A previous article reported proximal pseudoaneurysm formation after ascending to descending aortic bypass,10 therefore, annual follow up CT is needed.
Conclusion
The findings of this case suggest that ascending to descending aortic bypass concomitant with endovascular embolisation for a late CoA patched site aneurysm might be an alternative strategy that should be carefully considered in specific cases, including those in whom conventional TEVAR is contraindicated. The short and mid term results of this procedure are satisfactory with regard to the prevention of aneurysm rupture.
Conflicts of interest
None.
References
- 1.Knyshov G.V., Sitar L.L., Glagola M.D., Atamanyuk M.Y. Aortic aneurysms at the site of the repair of coarctation of the aorta: a review of 48 patients. Ann Thorac Surg. 1996;61:935–939. doi: 10.1016/0003-4975(95)01189-7. [DOI] [PubMed] [Google Scholar]
- 2.Cramer J.W., Ginde S., Bartz P.J., Tweddell J.S., Litwin S.B., Earing M.G. Aortic aneurysms remain a significant source of morbidity and mortality after use of Dacron(®) patch aortoplasty to repair coarctation of the aorta: results from a single center. Pediatr Cardiol. 2013;34:296–301. doi: 10.1007/s00246-012-0442-1. [DOI] [PubMed] [Google Scholar]
- 3.Kotelis D., Bischoff M.S., Rengier F., Ruhparwar A., Gorenflo M., Bockler D. Endovascular repair of pseudoaneurysms after open surgery for aortic coarctation. Interact Cardiovasc Thorac Surg. 2016;22:26–31. doi: 10.1093/icvts/ivv297. [DOI] [PubMed] [Google Scholar]
- 4.Khavandi A., Bentham J., Marlais M., Martin R.P., Morgan G.J., Parry A.J. Transcatheter and endovascular stent graft management of coarctation-related pseudoaneurysms. Heart. 2013;99:1275–1281. doi: 10.1136/heartjnl-2012-303488. [DOI] [PubMed] [Google Scholar]
- 5.Walhout R.J., Lekkerkerker J.C., Oron G.H., Hitchcock F.J., Meijboom E.J., Bennink G.B. Comparison of polytetrafluoroethylene patch aortoplasty and end-to-end anastomosis for coarctation of the aorta. J Thorac Cardiovasc Surg. 2003;126:521–528. doi: 10.1016/s0022-5223(03)00030-8. [DOI] [PubMed] [Google Scholar]
- 6.Choudhary P., Canniffe C., Jackson D.J., Tanous D., Walsh K., Celermajer D.S. Late outcomes in adults with coarctation of the aorta. Heart. 2015;101:1190–1195. doi: 10.1136/heartjnl-2014-307035. [DOI] [PubMed] [Google Scholar]
- 7.Etz C.D., Zoli S., Kari F.A., Mueller C.S., Bodian C.A., Di Luozzo G. Redo lateral thoracotomy for reoperative descending and thoracoabdominal aortic repair: a consecutive series of 60 patients. Ann Thorac Surg. 2009;88:758–766. doi: 10.1016/j.athoracsur.2009.04.140. discussion 767. [DOI] [PubMed] [Google Scholar]
- 8.Kawaharada N., Morishita K., Fukuda J., Hachiro Y., Takahashi K., Abe T. Thoracoabdominal aortic aneurysm repair through redo left-sided thoracotomy. Ann Thorac Surg. 2004;77:1304–1308. doi: 10.1016/j.athoracsur.2003.09.043. [DOI] [PubMed] [Google Scholar]
- 9.Said S.M., Burkhart H.M., Dearani J.A., Connolly H.M., Schaff H.V. Ascending-to-descending aortic bypass: a simple solution to a complex problem. Ann Thorac Surg. 2014;97:2041–2047. doi: 10.1016/j.athoracsur.2014.02.030. discussion 2047–8. [DOI] [PubMed] [Google Scholar]
- 10.Rekik S., Jacq L., Bourlon F., Bernasconi F., Quaegebeur J.M., Dreyfus G. Large compressive proximal pseudoaneurysm after ascending-to-descending aortic bypass in a 62 year-old patient with severe aortic coarctation: first reported case. Int J Cardiol. 2014;172:e453–e457. doi: 10.1016/j.ijcard.2014.01.019. [DOI] [PubMed] [Google Scholar]