Abstract
Background: Acupuncture intervention in actual practice is rarely reported and may be different from that applied in acupuncture research. Objectives: To review acupuncture practice in an integrative medicine clinic and characterize the association between targeted symptoms, traditional Chinese medicine (TCM) diagnosis, and acupoint selection. Methods: We reviewed outpatient acupuncture records from March 2016 to April 2018. Statistical analyses were applied to characterize referral symptoms and associated TCM diagnosis as well as acupoint selection. Results: The final analysis included 5393 acupuncture records (1264 patients). Twelve TCM diagnosis components were identified in the referral symptoms of pain, neuropathy, xerostomia, and hot flashes. Pain was associated with 78 different TCM diagnoses (combinations of TCM diagnosis components). Total of 217 different acupoints were used in the acupuncture treatments (1739) for neuropathy. The acupoint yintang was used in 73.8% of the visits for neuropathy, yet only in 26.5% (P < .001) of the treatments when patients had a TCM diagnosis of qi deficiency, qi stagnation, and blood stagnation. Similarly, both consistencies and variations were seen in acupoint selection with each targeted symptom and its associated TCM diagnoses. Conclusions: TCM diagnosis was not homogeneous among acupuncture treatments for a single referral symptom. In contrast to most of the research on acupuncture for symptom control, there were considerable variations in acupoint selection among treatments for the same symptom in a clinical setting. Future research is needed to examine the clinical relevance of a fixed intervention structure in acupuncture research and the value of individualized acupuncture treatment.
Keywords: acupuncture, acupuncture point selection, traditional Chinese medicine, integrative medicine, cancer, complementary health approaches
Introduction
Acupuncture, an ancient Chinese medical approach used for more than 2500 years, is gaining interest both in clinical practice and research, particularly in the field of symptom management.1,2 One of the main components of TCM acupuncture treatment planning is selection of the acupoints where the needles will be inserted. Similar to conventional medicine, traditional Chinese medicine (TCM) practice begins with documenting the patient’s medical history and performing a physical examination. TCM principles are followed to identify key problems and reach a diagnosis, which in turn determines the acupuncture treatment plan. A single conventional medical diagnosis or symptom does not usually correspond to only one unique TCM diagnosis. In fact, it could correlate with several different TCM diagnoses that consequently influence acupoint selection.3,4 However, most of the randomized controlled trials on the use of acupuncture for symptom management in cancer patients applied a set of fixed acupoints.5-10 This lack of treatment individualization, which is an important feature of the TCM practice principle, does not accurately represent real-life TCM acupuncture practice and may result in reduced application of acupuncture research evidence in a real-world setting. Only a limited number of studies on acupuncture for symptom management in cancer patients, however, have allowed some adjustment of acupoint selection on the basis of an acupuncturist’s discretion based on individual symptoms in addition to the target symptom.11,12 In a survey of 23 acupuncturists after participating in a randomized controlled trial of acupuncture for depression that utilized a TCM approach, 96% reported applying acupuncture in the trial exactly the same way or similarly as in routine practice.3 Studies showing how TCM diagnosis and acupoint selection are being applied in the actual clinical practice of TCM acupuncture for symptom management are severely lacking. The aim of our study was to review the acupuncture approach for symptom management in an integrative medicine clinic of a large tertiary cancer center and report features of association between targeted symptoms, TCM diagnosis, and acupoint selection in actual clinical practice.
Methods
Study Design and Patients
Acupuncture notes of patients treated from March 2016 to April 2018 were identified through a search of the institutional electronic medical records by acupuncture providers’ names. TCM information was extracted including the primary reason for acupuncture referral, TCM diagnosis, and acupoints used. Treatment sessions were removed from the analysis if the TCM information was incomplete in the acupuncture notes. Patients’ demographic and cancer diagnosis data were obtained from the institutional data warehouse. This retrospective study was approved by The University of Texas MD Anderson Cancer Center’s Institutional Review Board in accordance with an assurance filed with, and approved by, the Department of Health and Human Services.
Intervention
We modeled Macpherson et al’s example to report acupuncture intervention for our study.3 Patients referred to the Integrative Medicine Center from within MD Anderson Cancer Center are initially assessed by a physician-led consulting clinic and may be referred for acupuncture treatment based on the physician’s assessment after reviewing of the patients’ oncology history and symptoms. Acupuncture treatment was provided by 3 licensed, experienced (average >10 years) acupuncturists credentialed through the institution’s Medical Staff Office. All 3 acupuncturists were trained in TCM acupuncture principles and familiar with the same nomenclature. Initial acupuncture visit duration was approximately 1 hour, with follow-up visits of about 30 minutes. The acupuncturists obtained a history from patients, conducted a physical assessment that included pulse palpation and tongue inspection, and then formulated TCM diagnoses and individualized treatment plans including acupoint selection. The TCM diagnoses and chosen acupoints at each acupuncture session were based on the clinical judgment of the treating acupuncturist guided by the principles of TCM. No pretreatment protocols were established. The treatment was with solid, stainless steel, single-use acupuncture needles (SEIRIN acupuncture needles, gauge 36), inserted into specific acupoints on the body and left in place for 20 to 30 minutes. Manual or electrical stimulation of the needles was applied in some cases to augment the acupuncture effects. TCM assessment, diagnoses, and acupoints used were documented in the medical record as part of the acupuncture encounter. One TCM diagnosis may contain one or more components, for instance, a diagnosis of damp accumulation and yin deficiency has 2 components. Each TCM diagnosis component usually represents a group of symptoms rather than a single symptom. For instance, symptoms of fatigue, edema, swelling, abdominal distension, cold extremities, and poor memory and appetite in a patient with hot flashes indicate a diagnosis of damp accumulation, while the presence of sensations of heat, especially in the face and in the afternoon, sweating, cheek flush, dizziness, poor vision (especially at night), insomnia, palpitations, and irritability is consistent with yin deficiency.13
The acupuncture treatment was provided throughout the oncology treatment course including before, during, and after chemotherapy, surgery, and/or radiation treatment except in the presence of significant thrombocytopenia or neutropenia. Safety procedures are followed by all of our acupuncturists. Acupuncture treatments are held if a patient has (1) absolute neutrophil count less than 1000/µL unless specifically approved by an attending physician of our Integrative Medical Center; (2) platelet count less than 25 000/µL; (3) international normalized ratio (INR) of greater than 2.00 or partial thromboplastin time (PTT) of greater than 90 seconds; or (4) unstable medical conditions such as clinically significant cardiac arrhythmias, symptomatic orthostatic hypotension, altered mental state status, and other case-by-case consideration.
Statistical Analysis
The primary endpoints analyzed were referral symptoms, TCM diagnoses, and acupoint selection. We used descriptive statistics to analyze the frequencies, medians, means, and standard deviations of the study variables for the study cohort. Univariate analysis was performed to determine the association between each acupoint and TCM diagnosis. For each referral symptom, a heat map was generated highlighting the frequency of usage of each acupoint for the referral symptom as well as individual TCM diagnosis. For each referral symptom, the frequency of an acupoint usage is measured as follows: acupuncture visits that used the acupoint × 100/total acupuncture visits. For each specific TCM diagnosis associated with the referral symptom, the frequency of an acupoint usage is measured as follows: acupuncture visits with the specific TCM diagnosis that used the acupoint × 100/total acupuncture visits with the specific TCM diagnosis. A heat map color scale was used to represent the frequency of usage of each acupoint. The acupoint frequency for each TCM diagnosis was compared with the acupoint frequency in the referral symptom. Significance was appraised using the χ2 test or Fisher’s exact test, where appropriate. Statistical significance for rejection of the null hypothesis was set at P < .05. All statistical analyses were performed using R software (version 3.5.0, The R Foundation; http://www.r-project.org).
Results
Patient Characteristics
A total of 5393 (90%) acupuncture treatment records from 1264 patients were included in the study after 617 records were excluded from the analysis because of missing data. Patient characteristics are reported in Table 1. The median age was 58 years, and 67% were female. The study cohort had a wide range of cancer diagnoses, with breast cancer being the most frequent (23%).
Table 1.
Patient Demographics.
| Characteristic | N (%) |
|---|---|
| Total patients | 1264 |
| Age, median [IQR], years | 58 [48-66] |
| Race | |
| Caucasian | 887 (70) |
| Black | 118 (9) |
| Asian | 69 (6) |
| Hispanic | 52 (4) |
| Others | 138 (11) |
| Sex | |
| Female | 849 (67) |
| Male | 415 (33) |
| Cancer diagnosis | |
| Breast | 284 (23) |
| Gastrointestinal | 168 (13) |
| Hematological | 114 (9) |
| Head and neck | 105 (8) |
| Sarcoma | 110 (9) |
| Lung | 94 (7) |
| Gynecological | 69 (6) |
| Brain and spinal cord | 65 (5) |
| Genitourinary | 55 (4) |
| Others | 200 (16) |
| Acupuncture treatments, median [IQR] | 2 [1-5] |
Abbreviation: IQR, interquartile range.
Characteristics of Acupuncture Visits
There were 16 referral symptoms (neuropathy, xerostomia, nausea, mucositis, pain, headache, constipation, diarrhea, fatigue, anxiety, insomnia, vertigo, wellness, rash, dysphagia, and hot flashes) identified among the 5393 acupuncture records. The characteristics of the acupuncture visits are summarized in Table 2, including the total visits as well as the top 4 symptoms that were treated. Twelve different TCM diagnosis components were identified: qi deficiency, qi stagnation, blood stagnation, blood deficiency, heart heat, yin deficiency, yin stagnation, yang deficiency, damp accumulation, heat accumulation, stomach damp accumulation and heat stagnation, and phlegm accumulation. Each TCM diagnosis is a unique combination of TCM diagnosis component(s) (eg, qi deficiency, qi stagnation, and blood deficiency is a diagnosis with 3 TCM components). All of the 12 TCM components were observed among the diagnoses for each of the top 4 symptoms that were treated. Pain was the most frequently treated symptom among all the acupuncture visits and was associated with 78 unique TCM diagnoses (combinations of TCM components). As many as 217 different acupoints were used in the treatments for neuropathy.
Table 2.
Characteristics of Acupuncture Visits.
| Presenting symptom | No. of visits | No. of TCM components | No. of TCM diagnoses | No. of acupoints |
|---|---|---|---|---|
| All | 5393 | 12 | 112 | 310 |
| Neuropathy | 1739 | 12 | 66 | 217 |
| Pain | 2005 | 12 | 78 | 287 |
| Xerostomia | 770 | 12 | 49 | 150 |
| Hot flashes | 740 | 12 | 48 | 156 |
Abbreviation: TCM, traditional Chinese medicine.
Acupoint Selection
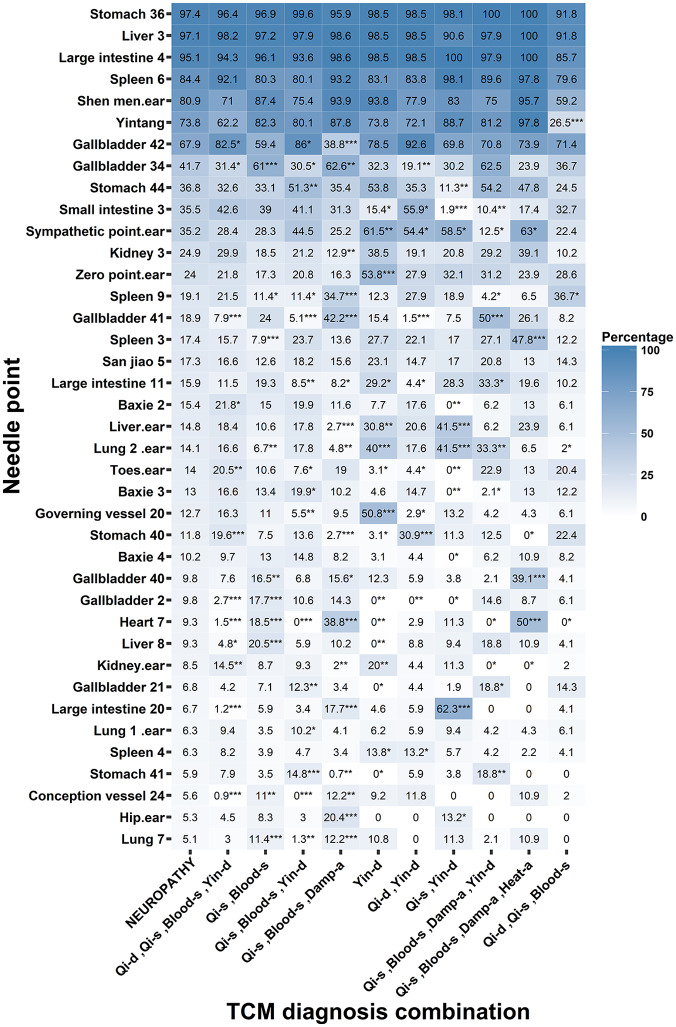
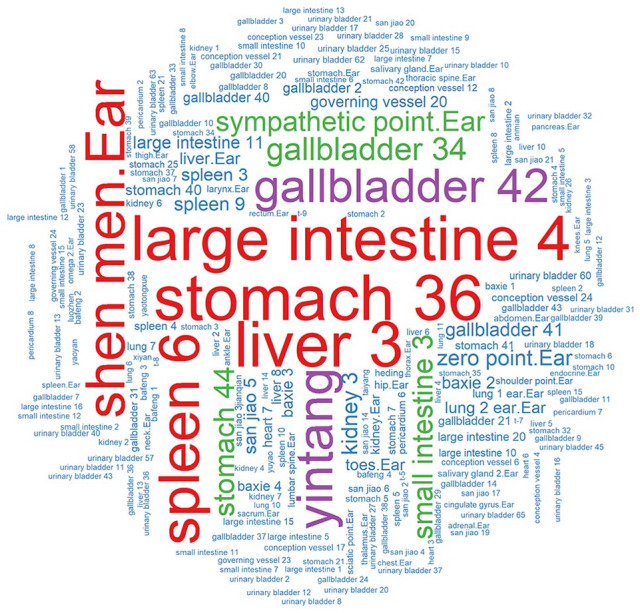
Figure 1 is a word cloud of all the acupoints used for the visits for neuropathy. Word clouds for pain, xerostomia, and hot flashes are shown in the supplemental material (available online). The acupoints ST36, LR3, LI 4, SP6, and Shen men (ear point) occurred most frequently in the acupuncture treatments for neuropathy. Figure 2 is a heat map showing how often each acupoint (defined as visits that used × 100/total visits) was used for all neuropathy visits and for particular TCM diagnoses in the neuropathy visits, with darker blue representing more frequent usage of the acupoint. Acupoints that were used in fewer than 5% of the total visits for neuropathy are not included in Figure 2. The acupoint yintang was used in 73.8% of the visits for neuropathy overall, but it was used only in 26.5% of the neuropathy visits when the patient had a TCM diagnosis of qi deficiency, qi stagnation, and blood stagnation (P < .001; Figure 2). LI 20 was used in only 6.7% of the total neuropathy visits but was used in 62.3% (P < .001) of the visits to treat neuropathy when patients had a TCM diagnosis of qi stagnation and yin deficiency.
Figure 1.
Word cloud of acupoints of acupuncture treatments for neuropathy.
Figure 2.
Heat map for acupoint selection and TCM diagnosis in neuropathy.
Abbreviations: Qi-d, qi deficiency; Qi-s, qi stagnation; Blood-s, blood stagnation; Yin-d, yin deficiency; Damp-a, damp accumulation; Heat-a, heat accumulation.
*P < .05; **P < .01; ***P < .001.
The acupoint selection and frequency, total and by TCM diagnosis, for the other 3 most frequent referral symptoms are reported in supplements: pain (Supplement Figures 1 and 2), hot flashes (Supplement Figures 3 and 4), and xerostomia (Supplement Figures 5 and 6).
Discussion
Traditional Chinese medicine practice is highly individualized. This is probably best explained by its complex diagnostic approach, which is different from conventional Western medicine. For instance, each of the 12 TCM diagnosis components observed in our study can involve several organ systems at the same time; thus, countless TCM diagnoses are possible depending on the varying presence of the TCM components.13 In a randomized controlled trial of acupuncture for 148 patients with back pain,14 65% had more than one TCM diagnosis component. TCM diagnosis may also differ in visits for the same patient if an existing TCM component resolves or a new one becomes present. Correspondingly, acupoint selection varies as the TCM diagnosis changes. The complexity of the TCM diagnostic approach has contributed to inconsistencies in utilizing symptom patterns to obtain TCM diagnosis among practitioners and presented a great test for modern research methods.6,15 This challenge has likely resulted in a scarcity of acupuncture studies for symptom management that base their acupoint selection on TCM diagnosis. It is particular meaningful for our study to report the observed richness of TCM diagnosis and correlation between TCM diagnosis and acupoint selection in a real-time practice. Lately, however, there has been emerging evidence about improved and adequate reliability of TCM diagnostic concordance and correlations between TCM and western diagnoses reported in studies of certain diseases.16 TCM diagnosis may be also important in predicting symptom response to acupuncture treatment.17,18 Our previous review of acupuncture treatment for hot flashes among cancer patients observed that presence of damp accumulation in TCM diagnosis was correlated with greater hot flashes score reduction.17 Future TCM acupuncture research should consider using TCM diagnosis to select a specific subgroup of a disease/syndrome or keep subgroups separate when deciding treatment efficacy. For instance, hot flashes with a TCM diagnosis of kidney yin deficiency, a condition that is usually chronic and age-related, is different from that with a TCM diagnosis of damp and heat accumulation, which is most likely diet-related (ie, alcohol consumption). Acupuncture approaches and treatment response can be different between these 2 pathophysiologic processes of the same symptom. Acupuncture research methods that address such differentiation will provide clinically relevant guidance to “real-life” acupuncture.
Both consistencies and variations in acupoint selection were observed among acupuncture treatments for each symptoms of neuropathy, hot flashes, xerostomia, and pain in our review of acupuncture practice. We found that the acupoints LR3, LI 4, Shen men (ear point), and Yintang were used frequently to treat neuropathy. However, as many as 217 acupoints were used in our acupuncture treatments for neuropathy. Certain acupoints were applied more in some visits than in others, and some of the variation is associated with certain TCM diagnoses, for example, in treatments for neuropathy, LI 20 was used in 62.3% of the visits with a TCM diagnosis of qi stagnation and yin deficiency, but in 1.2% of the treatment sessions if the patient had a TCM diagnosis of qi deficiency, qi stagnation, blood stagnation, and yin deficiency. Previous studies have reported correlations between acupoint selection and single TCM diagnosis components.3,4 Understandably, the combination of acupoint selection changes with different combination of TCM diagnosis components. Our study finding of significant correlation between TCM diagnosis and acupoint selection was consistent with our hypothesis that our acupuncture approach was individualized, rather than with fixed acupoints for a single symptom. Our study signified the gap between actual practice and many acupuncture studies in acupuncture approaches. We suggest that future studies consider TCM diagnosis-based approach in study cohort selection and acupoint selection, and in turn, provide evidence that is meaningful and applicable in clinical practice.
A limitation of our study is that many of the TCM components in our acupuncture documentation were not recorded in an organ system–specific manner. For example, our acupuncture notes did not specify whether qi deficiency was for lung, spleen, blood, or combinations of 2 or more organs. However, the acupoint selected might have followed an organ-specific approach. For instance, a combination of lung and spleen qi deficiency could be documented as qi deficiency, so could spleen and kidney qi deficiency. But the acupoints selected for the same qi deficiency might have been different because one involves lung and the other kidney, in addition to spleen. The lack of specificity in the TCM diagnosis documentation may partly explain why not all of the variations in acupoint selection were relatable to certain TCM diagnoses. In addition, the acupuncturists may have also determined the acupoint selection based on their rating of each TCM diagnosis component as of primary or secondary importance or nonessential (though the rating was not specifically documented), as such that acupoints related to the nonessential TCM diagnosis component may not be selected.
Our study provides information about TCM acupuncture clinical practice in cancer patients that is not adequately reported in the literature. We observed radically more acupoints (Table 2) applied in actual TCM acupuncture practice than reported in most randomized sham-controlled acupuncture research, which typically involve fewer than 10 unique acupoints for a single targeted symptom. MacPherson et al observed TCM acupuncture practice prospectively in 148 patients with back pain and reported 177 different acupoints used in 1269 treatments.14 Acupuncture intervention with fixed acupoints in many research methods is significantly different from a clinical TCM acupuncture approach and may limit the applicability of such research evidence in actual TCM acupuncture clinic practice. A further limitation of our research is that it is generated from the review of a single integrative medicine clinic practice of a large academic cancer center and may not broadly represent all styles of acupuncture practice, private and academic alike. For instance, western medical acupuncture, an adaptation of TCM acupuncture using knowledge of anatomy, physiology, pathology, and the principles of evidence-based medicine, does not adhere to TCM concepts of yin/yang and circulation of qi and uses different concepts than classical acupuncturists when choosing one acupoint over another.19 Our review is retrospective and is limited by data availability, so it may not include all features of TCM acupuncture practice, such as de qi that signifies the intensity of needle sensation during acupuncture and may be related to treatment efficacy.20 Information about target symptoms and use of electro acupuncture is also lacking in our data, and a comment about treatment intensity for each symptom or TCM diagnosis cannot be made. Future studies are needed to define symptom clusters and/or organ system dysfunctions for each TCM diagnosis component to help further understand the pathophysiologic foundation of TCM diagnostics. The value of an individualized TCM treatment approach will also require further evaluation to provide actionable guidelines for acupuncture practice.
Conclusions
Traditional Chinese medicine diagnosis was not homogeneous for a single referral symptom for acupuncture treatment. In contrast to the fixed acupoint interventions for symptom control in most clinical research, variations in acupoint selection among treatments for the same symptom were observed. Some consistency of acupoint selection was associated with certain TCM diagnoses and symptoms. Future research effort is needed to examine the value of highly individualized acupuncture treatment.
Supplemental Material
Supplemental material, Supplemental_data for Association Between Acupoint Selection, Target Symptoms, and Traditional Chinese Medicine Diagnosis in Real-Time Clinical Practice in a Comprehensive Cancer Center by Wenli Liu, Aiham Qdaisat, Gabriel Lopez, Santhosshi Narayanan, Susan Underwood, Michael Spano, Akhila Reddy, Ying Guo, Sai-Ching Yeung, Eduardo Bruera and Lorenzo Cohen in Integrative Cancer Therapies
Footnotes
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: The University of Texas MD Anderson Cancer Center is supported in part by the NIH through Cancer Center Support Grant P30 CA016672. The research was funded in part through the support of the Duncan Family Institute for Cancer Prevention and Risk Assessment and the Richard E. Haynes Distinguished Professorship for Clinical Cancer Prevention at The University of Texas MD Anderson Cancer Center (L. Cohen).
ORCID iDs: Wenli Liu  https://orcid.org/0000-0003-1036-4564
https://orcid.org/0000-0003-1036-4564
Santhosshi Narayanan  https://orcid.org/0000-0003-0591-1500
https://orcid.org/0000-0003-0591-1500
Supplemental Material: Supplemental material for this article is available online.
References
- 1. World Health Organization. WHO traditional medicine strategy: 2014-2023. Published December 2013. Accessed May 6, 2020 http://www.who.int/medicines/publications/traditional/trm_strategy14_23/en/
- 2. Brauer JA, El Sehamy A, Metz JM, Mao JJ. Complementary and alternative medicine and supportive care at leading cancer centers: a systematic analysis of websites. J Altern Complement Med. 2010;16:183-186. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. MacPherson H, Elliot B, Hopton A, Lansdown H, Richmond S. Acupuncture for depression: patterns of diagnosis and treatment within a randomised controlled trial. Evid Based Complement Alternat Med. 2013;2013:286048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Stuardi T, MacPherson H. Acupuncture for irritable bowel syndrome: diagnosis and treatment of patients in a pragmatic trial. J Altern Complement Med. 2012;18:1021-1027. [DOI] [PubMed] [Google Scholar]
- 5. Garcia MK, Graham-Getty L, Haddad R, et al. Systematic review of acupuncture to control hot flashes in cancer patients. Cancer. 2015;121:3948-3958. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Garcia MK, McQuade J, Lee R, Haddad R, Spano M, Cohen L. Acupuncture for symptom management in cancer care: an update. Curr Oncol Rep. 2014;16:418. [DOI] [PubMed] [Google Scholar]
- 7. MacPherson H, Altman DG, Hammerschlag R, et al. ; STRICTA Revision Group. Revised STandards for Reporting Interventions in Clinical Trials of Acupuncture (STRICTA): extending the CONSORT statement. PLoS Med. 2010;7:e1000261. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Liu Z, Yan S, Wu J, et al. Acupuncture for chronic severe functional constipation: a randomized trial. Ann Intern Med. 2016;165:761-769. [DOI] [PubMed] [Google Scholar]
- 9. Bao T, Goloubeva O, Pelser C, et al. A pilot study of acupuncture in treating bortezomib-induced peripheral neuropathy in patients with multiple myeloma. Integr Cancer Ther. 2014;13:396-404. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Rostock M, Jaroslawski K, Guethlin C, Ludtke R, Schröder S, Bartsch HH. Chemotherapy-induced peripheral neuropathy in cancer patients: a four-arm randomized trial on the effectiveness of electroacupuncture. Evid Based Complement Alternat Med. 2013;2013:349653. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Lesi G, Razzini G, Musti MA, et al. Acupuncture as an integrative approach for the treatment of hot flashes in women with breast cancer: a prospective multicenter randomized controlled trial (AcCliMaT). J Clin Oncol. 2016;34:1795-1802. [DOI] [PubMed] [Google Scholar]
- 12. Molassiotis A, Bardy J, Finnegan-John J, et al. Acupuncture for cancer-related fatigue in patients with breast cancer: a pragmatic randomized controlled trial. J Clin Oncol. 2012;30:4470-4476. [DOI] [PubMed] [Google Scholar]
- 13. Wiseman N, Ellis A. Fundamentals of Chinese Medicine. Paradigm Publications; 1996. [Google Scholar]
- 14. MacPherson H, Thorpe L, Thomas K, Campbell M. Acupuncture for low back pain: traditional diagnosis and treatment of 148 patients in a clinical trial. Complement Ther Med. 2004;12:38-44. [DOI] [PubMed] [Google Scholar]
- 15. Birkeflet O, Laake P, Vøllestad NK. Poor multi-rater reliability in TCM pattern diagnoses and variation in the use of symptoms to obtain a diagnosis. Acupunct Med. 2014;32:325-332. [DOI] [PubMed] [Google Scholar]
- 16. White A. Acupuncture and constitutional diagnosis: where now? Acupunct Med. 2011;29:247-248. [DOI] [PubMed] [Google Scholar]
- 17. Liu W, Qdaisat A, Lopez G, et al. Acupuncture for hot flashes in cancer patients: clinical characteristics and traditional Chinese medicine diagnosis as predictors of treatment response. Integr Cancer Ther. 2019;18:1534735419848494. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Avis NE, Coeytaux RR, Levine B, Isom S, Morgan T. Trajectories of response to acupuncture for menopausal vasomotor symptoms: the acupuncture in menopause study. Menopause. 2017;24:171-179. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. White A; Editorial Board of Acupuncture in Medicine. Western medical acupuncture: a definition. Acupunct Med. 2009;27:33-35. [DOI] [PubMed] [Google Scholar]
- 20. Johnson MI, Benham AE. Acupuncture needle sensation: the emerging evidence. Acupunct Med. 2010;28:111-114. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental material, Supplemental_data for Association Between Acupoint Selection, Target Symptoms, and Traditional Chinese Medicine Diagnosis in Real-Time Clinical Practice in a Comprehensive Cancer Center by Wenli Liu, Aiham Qdaisat, Gabriel Lopez, Santhosshi Narayanan, Susan Underwood, Michael Spano, Akhila Reddy, Ying Guo, Sai-Ching Yeung, Eduardo Bruera and Lorenzo Cohen in Integrative Cancer Therapies