Abstract
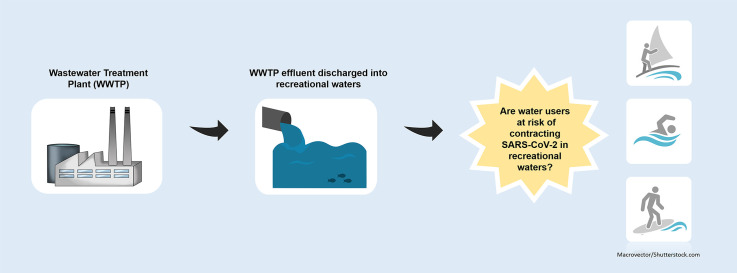
Coronavirus disease 2019 (COVID-19), the respiratory illness caused by the novel virus, severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), which has lead to high morbidity and mortality rates worldwide, has been causing major public health concerns since first detected in late 2019. Following identification of novel pathogens, questions in relation to dissemination of the pathogen and transmission routes begin to emerge. This rapidly spreading SARS-CoV-2 virus has been detected in both faecal and wastewater samples across the globe, highlighting the potential for faecal-oral transmission of the virus. As a result, concerns regarding the transmission of the virus in the environment and the risk associated with contracting the virus in recreational waters, particularly where inadequately treated wastewater is discharged, have been emerging in recent weeks. This paper highlights the need for further research to be carried out to investigate the presence, infectivity and viability of this newly identified SARS-CoV-2 virus in wastewater effluent and receiving recreational waters.
Keywords: Coronavirus, COVID-19, SARS-CoV-2, Wastewater, Aquatic environment
Graphical abstract
1. Introduction
The newly identified coronavirus, SARS-CoV-2, known to cause respiratory illness, Covid-19, in humans, has now been declared a pandemic by the World Health Organisation. The virus, which was first detected in the Chinese city of Wuhan in the Hubei Provence in December 2019, has since spread rapidly across the globe, resulting in almost 7 million confirmed cases and over 400,000 deaths by the beginning of June 2020 (WHO, 2020a). SARS-CoV-2 is an enveloped virus belonging to the coronavirus family, which consists of six other coronaviruses known to cause human illness (Cascella et al., 2020; CDC, 2020a). This novel coronavirus is closely related to other coronaviruses known to have caused outbreaks previously such as the Severe Acute Respiratory Syndrome (SARS-CoV-1) and Middle East Respiratory Syndrome (MERS-CoV) related coronaviruses, both of which have the ability to cause severe illness in humans. SARS-CoV-2 is reported as being most genetically identical to SARS-CoV-1 in particular, with studies reporting a genetic relatedness of ~80% (Chan et al., 2020; Zhou et al., 2020).
The main route of transmission of SARS-CoV-2 between humans occurs via respiratory droplets and contact (Jin et al., 2020; WHO, 2020b). However, concerns regarding environmental transmission and the associated public health risk are beginning to emerge. In relation to SARS-CoV-2, the risk of transmission to humans through recreational water bodies is unclear, as there have been no reports to date on the detection of or the ability of this particular virus to remain viable in such water bodies. It is believed that the SARS-CoV-2 virus may behave in similar ways to other coronaviruses, therefore, data reported on previously identified coronaviruses in relation to transmission routes and viability in the environment may be comparable to this novel virus (WEF, 2020). Carducci et al. (2020) highlight the need for enhanced understanding of the fate of coronaviruses, including SARS-CoV-2, in the aquatic environment (Carducci et al., 2020).
2. Faecal-oral transmission - a potential route of transmission for SARS-CoV-2?
Studies reporting the detection of SARS-CoV-2 viral RNA in faecal samples from infected humans have been emerging in recent months (Cai et al., 2020; Holshue et al., 2020; J. Zhang et al., 2020a; Wölfel et al., 2020). Although viral RNA has been detected, this does not necessarily indicate the presence of the virus in its infectious state (Holshue et al., 2020). However, the isolation of the live virus from stool samples has also been documented recently (Wang et al., 2020; Xiao et al., 2020; Y. Zhang et al., 2020c). A number of studies have reported persistent viral shedding in faeces of previously SARS-CoV-2 positive patients following negative respiratory samples. The number of days, post negative respiratory swabs, in which viral shedding was noted in faeces ranged extensively from 7 days (Chen et al., 2020), to 10 days (T. Zhang et al., 2020b), to 20 days (Xing et al., 2020) to a surprising 33 days (Y. Wu et al., 2020).
In recent weeks, Medema et al. (2020) reported the first detection of SARS-CoV-2 viral RNA in untreated wastewater collected from wastewater treatment plants (WWTP) in the Netherlands. Since then, there have been further reports indicating detection of the viral RNA in WWTP influent in Australia, the U.S.A, and France (Ahmed et al., 2020; F. Wu et al., 2020; Wurtzer et al., 2020).
At present, the viability of this novel virus in both faecal and wastewater samples is not known, however, data has been reported previously on the viability of the closely related SARS-CoV-1 virus in such samples. The SARS-CoV-1 virus, believed to be of zoonotic origin, which like SARS-CoV-2 causes respiratory illness, caused an outbreak in 2003 killing almost 700 people across the globe (Lam et al., 2004). Reports have indicated that the SARS-CoV-1 virus has been found to survive in faecal samples for up to 17 days at 4 °C, however at a higher temperature of ~20 °C, length of survival significantly reduced to 3–4 days (WHO, 2003; Wang et al., 2005). Similarly, in wastewater samples, the SARS-CoV-1 virus was found to survive for up to 14 days at 4 °C, however, only 2–3 days at an elevated temperature of ~20 °C (Wang et al., 2005; Gundy et al., 2009).
Following detection of new pathogenic microorganisms, such as SARS-CoV-2, concerns begin to arise in relation to transmission routes and generally, the risks associated with the spread of such pathogens through the environment (Brainard et al., 2017). To date, there have been no reports of humans contracting the SARS-CoV-2 virus via faecal-oral transmission (CDC, 2020b). However, where the SARS-CoV-2 virus is present in its infectious state following excretion from the body, the potential of faecal transmission cannot be ruled out. The importance of considering this route of transmission has been highlighted, especially where humans may become exposed to faeces or wastewater containing the virus i.e. in water bodies contaminated with raw discharge (Heller et al., 2020; Qu et al., 2020; Wigginton and Boehm, 2020; Xiao et al., 2020; Xing et al., 2020; Yeo et al., 2020; Yuen et al., 2020; Y. Zhang et al., 2020c).
3. The effect of wastewater treatment on SARS-CoV-2
Wastewater containing human excreta serves as a potential route for dissemination of pathogenic microorganisms in the environment. Therefore, the discharge of inadequately treated wastewater containing such microorganisms poses a risk to human health (EPA, 2019). In general, wastewater is treated at a WWTP prior to its discharge into the aquatic environment. In relation to SARS-CoV-2, very little research has been carried out on the effects of the wastewater treatment processes on the virus to date. A major challenge to understanding the role of wastewater in transmission of SARS-Co-V-2 is lack of standardised methodologies for detection and quantification in wastewater samples (Kitajima et al., 2020). Although Wurtzer et al. (2020) reported the detection of SARS-CoV-2 RNA in both untreated and treated wastewater samples collected from WWTP's in France, they did document a decrease in the viral load following wastewater treatment. It is important to note that as this was viral RNA detected in the wastewater samples, it does not indicate the presence of the infectious virus.
Although little data is available in relation to the effects of wastewater treatment on SARS-CoV-2, there is no evidence to suggest that this virus behaves in a different manner to other coronaviruses. A previous study which investigated coronavirus survival following primary and secondary wastewater treatment, but before disinfection, reported reduced viability of the virus in secondary effluent (Gundy et al., 2009). The inactivation of the closely related SARS-CoV-1 by common antiseptics and disinfectants, such as ethanol, chlorine and bleach, has been reported previously indicating susceptibility to such agents (Rabenau et al., 2005; Geller et al., 2012). According to the Water Environment Federation (2020) and World Health Organisation (2020c), previous studies have indicated that filtration and disinfection systems in place at municipal WWTP's should be sufficient for the inactivation of viruses. Although reports have indicated the disinfection process to be a crucial step in wastewater treatment for the reduction in viability of viruses, there is still a possibility of the virus remaining in the WWTP effluent (Wigginton et al., 2015). However, even if the virus does enter the aquatic environment, enveloped viruses, which include coronaviruses, are believed to have a short survival rate in such waters (Wigginton et al., 2015).
4. Conclusion
According to the Centres for Disease Control and Prevention (CDC), 2020a, Centres for Disease Control and Prevention (CDC), 2020b, the expected risk associated with contracting the SARS-CoV-2 virus via water sources including wastewater and recreational water bodies' remains low. However, further research is warranted to investigate both viability and infectivity of this novel virus in wastewater and in receiving water bodies. Such research is important to gain a better understanding of the risk associated with contracting the virus in recreational waters and to assist public health authorities in the development and implementation of policies and guidelines for the protection of human health.
CRediT authorship contribution statement
Niamh Cahill: Conceptualization, Writing - original draft. Dearbháile Morris: Conceptualization, Writing - original draft.
Declaration of competing interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Editor: Damia Barcelo
References
- Ahmed W. First confirmed detection of SARS-CoV-2 in untreated wastewater in Australia: a proof of concept for the wastewater surveillance of COVID-19 in the community. Sci. Total Environ. 2020 doi: 10.1016/j.scitotenv.2020.138764. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brainard J., Pond K., Hunter P.R. Censored regression modeling to predict virus inactivation in wastewaters. Environ. Sci. Technol. 2017;51(3):1795–1801. doi: 10.1021/acs.est.6b05190. [DOI] [PubMed] [Google Scholar]
- Cai J. A case series of children with 2019 novel coronavirus infection: clinical and epidemiological features. Clin. Infect. Dis. 2020 doi: 10.1093/cid/ciaa198. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carducci A. Making waves: coronavirus detection, presence and persistence in the water environment: state of the art and knowledge needs for public health. Sci. Total Environ. 2020 doi: 10.1016/j.watres.2020.115907. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cascella M. StatPearls Publishing; Treasure Island, FL, USA: 2020. Features, Evaluation and Treatment Coronavirus (COVID-19)www.ncbi.nlm.nih.gov/books/NBK554776 Available at. [PubMed] [Google Scholar]
- Centres for Disease Control and Prevention (CDC) Coronavirus, human coronavirus types. 2020. www.cdc.gov/coronavirus/types.html Available at.
- Centres for Disease Control and Prevention (CDC) Healthy water. 2020. www.cdc.gov/healthywater/index.html Available at.
- Chan J.F. Genomic characterization of the 2019 novel human-pathogenic coronavirus isolated from a patient with atypical pneumonia after visiting Wuhan. Emerging Microbes & Infections. 2020;9(1):221–236. doi: 10.1080/22221751.2020.1719902. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen Y. The presence of SARS-CoV-2 RNA in feces of COVID-19 patients. J. Med. Virol. 2020 doi: 10.1002/jmv.25825. [DOI] [PubMed] [Google Scholar]
- Environmental Protection Agency (EPA) Urban waste water treatment in 2018. 2019. www.epa.ie/pubs/reports/water/wastewater/uwwreport2018.html Available at.
- Geller C., Varbanov M., Duval R.E. Human coronaviruses: insights into environmental resistance and its influence on the development of new antiseptic strategies. Viruses. 2012;4(11):3044–3068. doi: 10.3390/v4113044. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gundy P.M., Gerba C.P., Pepper I.L. Survival of coronaviruses in water and wastewater. Food and Environmental Virology. 2009;1(1) (doi:10.1007%2Fs12560-008-9001-6) [Google Scholar]
- Heller L., Mota C.R., Greco D.B. COVID-19 faecal-oral transmission: are we asking the right questions? Sci. Total Environ. 2020;729 doi: 10.1016/j.scitotenv.2020.138919. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Holshue M. First case of 2019 novel coronavirus in the United States. N. Engl. J. Med. 2020;832(10):929–936. doi: 10.1056/NEJMoa2001191. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jin Y. A rapid advice guideline for the diagnosis and treatment of 2019 novel coronavirus (2019-nCoV) infected pneumonia (standard version) Military Medical Research. 2020;7(1):1–23. doi: 10.1186/s40779-020-0233-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kitajima M., Ahmed W., Bibby K. SARS-CoV-2 in wastewater: state of the knowledge and research needs. Sci. Total Environ. 2020 doi: 10.1016/j.scitotenv.2020.139076. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lam, C. W. K., Chan, M. H. M. and Wong, C. K. (2004) ‘Severe acute respiratory syndrome: clinical and laboratory manifestations’, The Clinical biochemist. Reviews, 25(2), pp. 121–123. Available at: https://pubmed.ncbi.nlm.nih.gov/18458712/. [PMC free article] [PubMed]
- Medema G. 2020. Presence of SARS-Coronavirus-2 in Sewage. medRxiv. [DOI] [PubMed] [Google Scholar]
- Qu G. An imperative need for research on the role of environmental factors in transmission of novel coronavirus (COVID-19) Environmental Science & Technology. 2020;54(7):3730–3732. doi: 10.1021/acs.est.0c01102. [DOI] [PubMed] [Google Scholar]
- Rabenau H.F. Efficacy of various disinfectants against SARS coronavirus. J. Hosp. Infect. 2005;61(2):107–111. doi: 10.1016/j.jhin.2004.12.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang X. Study on the resistance of severe acute respiratory syndrome-associated coronavirus. J. Virol. Methods. 2005;126(1–2):171–177. doi: 10.1016/j.jviromet.2005.02.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang W. Detection of SARS-CoV-2 in different types of clinical specimens. JAMA. 2020 doi: 10.1001/jama.2020.3786. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Water Environment Federation (WEF) The water professional's guide to COVID-19. 2020. www.wef.org/news-hub/wef-news/the-water-professionals-guide-to-the-2019-novel-coronavirus Available at.
- Wigginton K.R., Boehm A.B. Environmental engineers and scientists have important roles to play in stemming outbreaks and pandemics caused by enveloped viruses. Environmental Science & Technology. 2020;54(7):3736–3739. doi: 10.1021/acs.est.0c01476. [DOI] [PubMed] [Google Scholar]
- Wigginton K., Ye Y., Ellenberg R. Emerging investigators series: the source and fate of pandemic viruses in the urban water cycle. Environmental Science.: Water Research and Technology. 2015;1(6):735–746. doi: 10.1039/c5ew00125k. [DOI] [Google Scholar]
- Wölfel R. Virological assessment of hospitalized patients with COVID-2019. Nature. 2020 doi: 10.1038/s41586-020-2196-x. [DOI] [PubMed] [Google Scholar]
- World Health Organisation First data on stability and resistance of SARS coronavirus compiled by members of WHO laboratory network. 2003. www.who.int/csr/sars/survival_2003_05_04/en/ Available at.
- World Health Organisation (WHO) Coronavirus disease 2019 (COVID-19) situation report - 115. 2020. www.who.int/emergencies/diseases/novel-coronavirus-2019/situation-reports Available at.
- World Health Organisation (WHO) (2020b) Report of the WHO-China joint mission on coronavirus disease 2019 (COVID-19). Available at: www.who.int/publications-detail/report-of-the-who-china-joint-mission-on-coronavirus-disease-2019-(covid-19).
- World Health Organisation (WHO) Water , sanitation , hygiene , and waste management for the COVID-19 virus. 2020. www.who.int/publications-detail/water-sanitation-hygiene-and-waste-management-for-covid-19 Available at.
- Wu F. 2020. SARS-CoV-2 Titers in Wastewater Are Higher than Expected from Clinically Confirmed Cases. medRxiv. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wu Y. Prolonged presence of SARS-CoV-2 viral RNA in faecal samples. The Lancet Gastroenterology & Hepatology. 2020;5(5):434–435. doi: 10.1016/S2468-1253(20)30083-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wurtzer S. 2020. Time Course Quantitative Detection of SARS-CoV-2 in Parisian Wastewaters Correlates with COVID-19 Confirmed Cases. medRxiv. [DOI] [Google Scholar]
- Xiao F. Evidence for gastrointestinal infection of SARS-CoV-2. Gastroenterology. 2020 doi: 10.1053/j.gastro.2020.02.055. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Xing Y. 2020. Prolonged Presence of SARS-CoV-2 in Feces of Pediatric Patients during Convalescent Phase. medRxiv. [DOI] [Google Scholar]
- Yeo C., Kaushal S., Yeo D. Enteric involvement of coronaviruses: is faecal – oral transmission of SARS-CoV-2 possible ? The Lancet Gastroenterology & Hepatology. 2020;5(4):335–337. doi: 10.1016/S2468-1253(20)30048-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yuen K.S. SARS -CoV- 2 and COVID - 19: the most important research questions. Cell & Bioscience. 2020;10(40) doi: 10.1186/s13578-020-00404-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhang J., Wang S., Xue Y. Fecal specimen diagnosis 2019 novel coronavirus – infected pneumonia. J. Med. Virol. 2020;92(6):680–682. doi: 10.1002/jmv.25742. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhang T. Detectable SARS-CoV-2 viral RNA in feces of three children during recovery period of COVID-19 pneumonia. J. Med. Virol. 2020 doi: 10.1002/jmv.25795. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhang Y. Isolation of 2019-nCoV from a stool specimen of a laboratory- confirmed case of the coronavirus disease 2019 (COVID-19) China CDC Weekly. 2020;2(8):123–124. http://weekly.chinacdc.cn/en/article/id/ffa97a96-db2a-4715-9dfb-ef662660e89d Available at. [PMC free article] [PubMed] [Google Scholar]
- Zhou P. A pneumonia outbreak associated with a new coronavirus of probable bat origin. Nature. 2020;579:270–273. doi: 10.1038/s41586-020-2012-7. [DOI] [PMC free article] [PubMed] [Google Scholar]