Dear Editors,
We found that there were no changes in cesarean section rate during the COVID-19 pandemic in New York City. New York City has seen a surge in the number of pregnant women diagnosed with coronavirus disease (COVID-19) [1]. New York City Health and Hospitals (NYCH+H) is the largest municipal healthcare system in the country. NYCH+H delivers a total of approximately 16,000 pregnancies across 11 acute-care facilities per year. These women are among the highest risk groups for infection [2]. A recent systematic review from Bologna Italy by Della Gatta et al. found that of the 51 women diagnosed with COVID-19, 46 (90.2%) women underwent cesarean delivery [3]. This was similar to initial reports of pregnancy outcomes from Wuhan China for 118 women diagnosed with COVID-19 over 3.5 months [4]. In this analysis, the authors reported that 93% of women underwent cesarean section. A recent case series from New York City found that of the 18 women who delivered between March 13 – March 27, 2020, 8 (44.4%) had a cesarean delivery [1].
Although data on COVID-19 continues to inform our understanding of this disease, information as it pertains to pregnant woman still remains limited. We therefore conducted a retrospective analysis to evaluate the relationship between cesarean section rates among those women who were tested for severe acute respiratory syndrome coronavirus 2 (SARS-CoV2). Our study period was from March 8th, 2020 until April 20th, 2020. During the outlined time period, the clinical protocol of the department was to perform a chart review across all NYCH+H in pregnant women all over the outlined time period. The subjects were divided into three groups: [1] COVID positive women [2]; COVID negative women; and [3] Untested women.
From March 8, 2020 to April 20, 2020, a total of 1952 pregnant women delivered in our hospitals. Of these, 478 (24.5%) pregnant women were tested for SARS-CoV2 infection and 131 (6.7%) were confirmed positive for COVID-19. In our population throughout NYCH+H, only 31.3% of SARS-CoV2 positive women underwent cesarean section, a rate which was not different from the expected average rate of 31% from previous years. The rate of cesarean section for women that were not tested was 31.4% and was 33.9% for those who were SARS-CoV2 negative.
Of all the pregnant women analyzed, the median age of the women was 19 years (range, 13–55); 131 of 1952 (6.7%) had been infected with SARS-CoV2 in the third trimester. Of those pregnant women who tested positive for SARS-CoV2, 90 of 131 (68.7%) had term delivery, 41 of 131 (31.3%) had pre-term delivery, and there were no neonatal deaths.
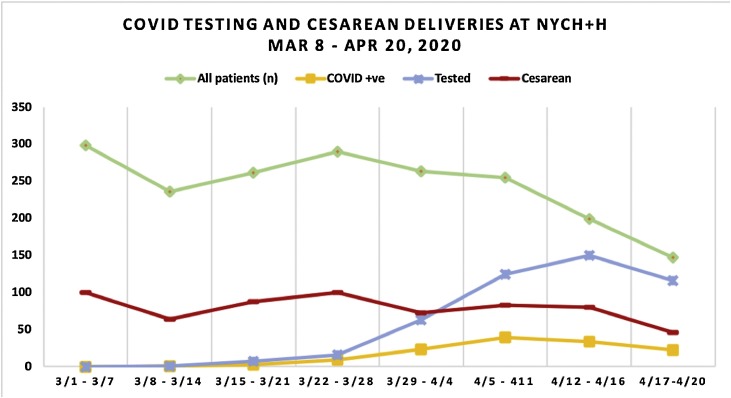
At the start of the pandemic, NYCH+H offered testing to symptomatic patients, and then transitioned to universal testing by the second week of April. Despite adoption of universal testing, our findings suggest that there was a continued adherence to best practices for the care of our pregnant patients and the cesarean section rates did not increase, which is shown in Fig. 1 . Previous reports suggest an increased rate of cesarean section amongst pregnant women who were found to be positive for SARS-CoV2 [1,3,4]. Our data suggest that infection with SARS-CoV2 does not affect route of delivery. It is fundamental that future studies provide more detailed information on maternal and fetal conditions, as well as the rationale behind obstetrical interventions.
Fig. 1.
Route of Delivery of Pregnant Patients in Response to Increase in COVID-19 Testing, March 1-April 20, 2020.
Declaration of Competing Interest
The authors have no conflict of interest to declare.
Acknowledgement
On Behalf of the NYC H+H Perinatal COVID Research Committee. We would like to thank Dr. Judith Chervenak for her assistance in study design and editing and Hugo Theo for his assistance in data analysis and validation.
References
- 1.Breslin Noelle, Baptiste Caitlin, Gyamfi-Bannerman Cynthia, Miller Russell, Martinez Rebecca, Bernstein Kyra. Coronavirus disease 2019 infection among asymptomatic and symptomatic pregnant women: two weeks of confirmed presentations to an affiliated pair of New York City hospitals. Am J Obstet Gynecol MFM. 2020;2(2) doi: 10.1016/j.ajogmf.2020.100118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.2020. Maternal mortality and disparate racial outcomes. [online] Available at: < http://www.health.ny.gov/community/adults/women/task_force_maternal_mortality/docs/maternal_mortality_report.pdf> [Accessed 20 April 2020] [Google Scholar]
- 3.Della Gatta Anna Nunzia, Rizzo Roberta, Pilu Gianluigi, Simonazzi Giuliana. COVID19 during pregnancy: a systematic review of reported cases. Am J Obstet Gynecol. 2020 doi: 10.1016/j.ajog.2020.04.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Chen Lian, Li Qin, Zheng Danni, Jiang Hai, Wei Yuan, Zou Li. Clinical characteristics of pregnant women with Covid-19 in Wuhan, China. N Engl J Med. 2020;382(25) doi: 10.1056/nejmc2009226. [DOI] [PMC free article] [PubMed] [Google Scholar]