Abstract
Study objective
In the initial period of the coronavirus disease 2019 (COVID-19) pandemic, there has been a substantial decrease in the number of patients seeking care in the emergency department. A first step in estimating the impact of these changes is to characterize the patients, visits, and diagnoses for whom care is being delayed or deferred.
Methods
We conducted an observational study, examining demographics, visit characteristics, and diagnoses for all ED patient visits to an urban level 1 trauma center before and after a state emergency declaration and comparing them with a similar period in 2019. We estimated percent change on the basis of the ratios of before and after periods with respect to 2019 and the decline per week using Poisson regression. Finally, we evaluated whether each factor modified the change in overall ED visits.
Results
After the state declaration, there was a 49.3% decline in ED visits overall, 35.2% (95% confidence interval −38.4 to −31.9) as compared with 2019. Disproportionate declines were seen in visits by pediatric and older patients, women, and Medicare recipients, as well as for presentations of syncope, cerebrovascular accidents, urolithiasis, and abdominal and back pain. Significant proportional increases were seen in ED visits for upper respiratory infections, shortness of breath, and chest pain.
Conclusion
There have been significant changes in patterns of care seeking during the COVID-19 pandemic. Declines in ED visits, especially for certain demographic groups and disease processes, should prompt efforts to understand these phenomena, encourage appropriate care seeking, and monitor for the morbidity and mortality that may result from delayed or deferred care.
Introduction
As the novel coronavirus disease 2019 (COVID-19) pandemic has spread, state governments and health systems have enacted a range of mitigation strategies and operational changes to anticipate and address an increasing number of patients with severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) infection. At the same time, during the early days of the pandemic, health systems have also seen a decrease in the number of patients presenting for acute care unrelated to COVID-19.1 Less care sought and received for these acute conditions may put patients at significant risk for preventable morbidity and mortality in the future. The characteristics of those patients who are and are not presenting to emergency departments during the early days of the SARS-CoV-2 pandemic have not yet been substantially examined in the medical literature. We report changes in the characteristics of patients and presentations to the ED of an urban level 1 trauma center before and after the statewide announcement of a “peacetime emergency” and public health measures to respond to the pandemic on March 13, 2020.2
Editor’s Capsule Summary.
What is already known on this topic
Media reports have described a drop in emergency department (ED) volumes in the weeks preceding the rise in ED cases of coronavirus disease 2019 (COVID-19).
What question this study addressed
This study looked at the demographic differences of ED patients after an emergency declaration and compared them with comparable volumes in 2019.
What this study adds to our knowledge
The study provides a preliminary look at patients who have likely not sought ED care during the COVID-19 pandemic.
How this is relevant to clinical practice
This is an initial study on how the COVID-19 pandemic has affected acute care. This will help guide future public health initiatives to address neglected health care needs.
Materials and Methods
Study Design, Setting, and Selection of Participants
We conducted an observational study of visits to the ED of a level 1 trauma center (Regions Hospital, St. Paul, MN) from a period of 28 days before through 28 days after the state’s emergency declaration on March 13, 2020. The ED has an annual census of nearly 90,000 and is located in a metropolitan area that over the study period had not yet seen a surge in COVID-19 infections, given that the state’s first confirmed case was recorded on March 6, 2020. The declaration on March 13, 2020 included announcements about social-distancing measures, the closure of all nonessential business, to begin on March 16, and the closure of all schools, to begin on March 18. The state’s first stay-at-home order was declared on March 25. We chose the earliest of these dates to provide the most conservative estimate of the potential effects of such measures on public willingness to seek care.
Methods of Measurement
We examined a cross section of visits from February 15 to April 10, 2020 and, for historical comparison, a similar period of weekdays and weekends from February 16 to April 12, 2019. Data were obtained through a systematic query of the electronic health record as part of institutional operations and quality improvement and were therefore deemed by the Institutional Review Board to be exempt from review. We obtained demographics, visit characteristics, and diagnoses for all visits during the foregoing periods. Diagnoses were identified by coded individual diagnoses or according to a diagnostic grouper when there was more than 1 diagnostic code for the disease entities examined. We preselected the diagnoses examined to include the 10 most common conditions in patients presenting to the ED and a list provided by department and hospital administration of conditions of higher and lower urgency or severity, all of which are reported.
Data Analysis
We estimated the ratios of before and after periods with respect to the same periods in 2019 by using Poisson regression and including the period, year, and period-year interaction as fixed effects. The period-year interaction corresponds to the log of the ratio of ratios, and thus we used this estimate to derive the percent change. In addition, we estimated the decline per week by including week as a continuous variable, and the interaction with period, year, and period-year week corresponding to an interrupted time series analysis. We evaluated the goodness of fit test for this model and scaled the model to correct for overdispersion. We estimated the percent change with respect to 2019 for the total number of ED visits by patient characteristics, diagnoses, and the decline per week. We used type III P values to evaluate whether characteristics and diagnoses modified the ED volume decline by including a second-order interaction for each factor with period and year. In addition, we analyzed total ED and total hospital exclusive charges both overall and by urgency using a log normal distribution and a difference in differences to estimate the percent change. All analyses were performed using SAS software version 9.3 (SAS Institute, Cary, NC). Additional statistical information is provided in Appendix E1, available online at http://www.annemergmed.com.
Results
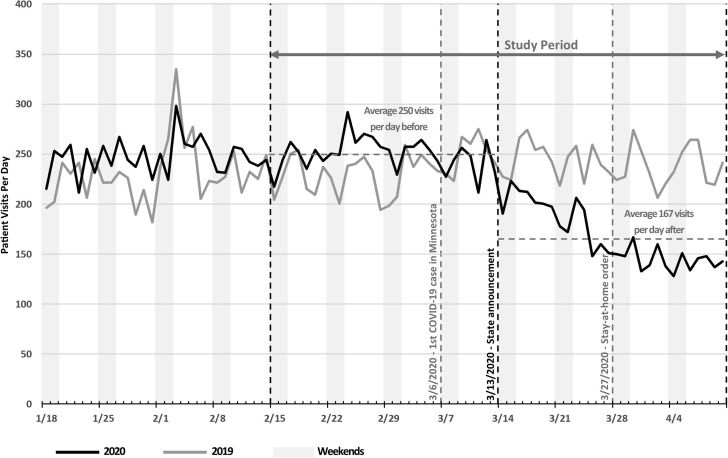
After the state declaration, the ED experienced a gradual but significant decline from an average of 250 daily visits for the 28 days before to an average of 167 daily visits for the 28 days after the declaration (Figure 1 ). This represented a 7.7% (95% confidence interval [CI] 1.1% to 13.7%) weekly decline in ED visits, a 49.3% decline overall, and a 35.2% (95% CI −38.4 to −31.9%) decline with respect to 2019. We found significant changes in the decline after the state declaration by patient demographics and visit characteristics, particularly in patient age, sex, race, insurance, arrival mode, and disposition (Table 1 ). There were significantly disproportionate declines in ED visits by patients younger than 18 years of age (−60.1%) and older than 65 years of age (−41.3%), women (−40.2%), White and Asian patients (−37.8% and 40.2%, respectively), and patients with Medicare (−40.8%) and other insurance (−74.1%; eg, liability, no-fault, workers’ compensation), as well as ambulatory patients (−38.1%) and those who left before evaluation or discharge (−75.6%).
Figure.
Trend of daily emergency department visits before and after state announcement. COVID-19, Coronavirus disease 2019.
Table.
Characteristics of emergency department patients and presentations before and after state declaration.
| Characteristics |
Feb 16 – Mar 15, 2019 |
Mar 16 – Apr 12, 2019 |
Feb 15 – Mar 13, 2020 |
Mar 14 – Apr 10, 2020 |
% Change 2020 With Respect to 2019 (95%CI) |
P Value∗ |
|---|---|---|---|---|---|---|
| Total No. of ED visits |
6,547 |
6,744 |
6,993 |
4,666 |
−35.2 (−38.4 to −32.9) |
— |
| N (%) or Median (IQR) | N (%) or Median (IQR) | N (%) or Median (IQR) | N (%) or Median (IQR) | |||
| Demographics | ||||||
| Age, median (IQR), y | 44 (28–59, 0–106) | 44 (28–58, 0–100) | 42 (29–60, 0–102) | 42 (29–59, 0–104) | — | — |
| 0–18 | 420 (6.4) | 427 (6.3) | 436 (6.2) | 177 (3.8) | −60.1 (−68.0 to −50.2) | <.001 |
| 18 to <65 | 4,990 (76.2) | 5,186 (76.9) | 5,246 (75.0) | 3,723 (79.8) | −31.7 (−35.5 to −27.7) | |
| ≤65 | 1,137 (17.4) | 1,131 (16.8) | 1,311 (18.7) | 766 (16.4) | −41.3 (−33.7 to −48.0) | |
| Sex | ||||||
| Female | 3,342 (51.0) | 3,386 (50.2) | 3,585 (51.3) | 2,171 (46.6) | −40.2 (-44.4 to -35.8) | <.001 |
| Male | 3,205 (49.0) | 3,358 (49.8) | 3,408 (48.7) | 2,492 (53.4) | −30.2 (−35.0 to −25.1) | |
| Race | ||||||
| Asian | 374 (5.7) | 416 (6.2) | 475 (6.8) | 316 (6.8) | −40.2 (−51.0 to −27.0) | .04 |
| African American | 1,902 (29.1) | 1,962 (29.1) | 2,005 (28.7) | 1,304 (28.0) | −37.0 (−42.6 to −30.7) | |
| White | 3,305 (50.5) | 3,489 (51.2) | 3,503 (50.1) | 2,302 (49.3) | −37.8 (−42.0 to −33.2) | |
| Hispanic or Latino | 456 (7.0) | 403 (6.0) | 477 (6.8) | 323 (6.9) | −23.4 (−36.9 to −6.9) | |
| Native American | 114 (1.7) | 95 (1.4) | 99 (1.4) | 62 (1.3) | −24.9 (−50.5 to 14.2) | |
| Native Hawaiian or OPI | 21 (0.3) | 19 (0.3) | 16 (0.2) | 13 (0.3) | −10.2 (−65.6 to 134.4) | |
| Other or multiracial | 375 (5.7) | 360 (5.3) | 418 (6.0) | 346 (7.4) | −13.8 (−29.6 to 5.6) | |
| Insurance | ||||||
| Commercial | 3,315 (50.6) | 3,261 (48.4) | 3,452 (49.4) | 2,322 (49.8) | −31.6 (−36.3 to −26.6) | <.001 |
| Medicare | 1,119 (17.1) | 1,095 (16.2) | 1,128 (16.1) | 654 (14.0) | −40.8 (−47.8 to −32.7) | |
| Medicaid | 1,193 (18.2) | 1,242 (18.4) | 1,175 (16.8) | 782 (16.8) | −36.1 (−43.3 to −27.9) | |
| Self−pay | 710 (10.8) | 757 (11.2) | 936 (13.4) | 759 (16.3) | −23.9 (−33.9 to −12.5) | |
| Other | 210 (3.2) | 391 (5.7) | 301 (4.7) | 145 (3.1) | −74.1 (−80.0 to −66.5) | |
| Visit characteristics | ||||||
| Arrival | ||||||
| Ambulatory | 4,575 (69.9) | 4,783 (70.9) | 4,872 (69.7) | 3,151 (67.5) | −38.1 (−41.8 to −34.3) | .02 |
| EMS, helicopter, fire | 1,823 (27.8) | 1,812 (26.9) | 2,000 (28.6) | 1,417 (30.4) | −28.7 (−35.1 to −21.7) | |
| Police | 149 (2.3) | 149 (2.2) | 121 (1.7) | 98 (2.1) | −19.0 (−42.9 to 14.9) | |
| ESI urgency or severity | ||||||
| 1 (high) | 122 (1.9) | 128 (1.9) | 139 (2.0) | 103 (2.2) | −29.4 (−50.5 to 0.8) | .53 |
| 2 | 2,096 (32) | 2,085 (30.9) | 2,198 (31.4) | 1,366 (29.3) | −37.5 (−42.9 to −31.6) | |
| 3 | 2,996 (45.8) | 3,271 (48.5) | 3,186 (45.6) | 2,252 (48.3) | −35.3 (−39.8 to −30.3) | |
| 4 | 1,109 (16.9) | 1,063 (15.8) | 1,216 (17.4) | 760 (16.3) | −34.8 (−42.4 to −26.2) | |
| 5 (low) | 197 (3) | 169 (2.5) | 224 (3.2) | 156 (3.3) | −18.8 (−39.2 to 8.5) | |
| Unknown | 27 (0.4) | 28 (0.4) | 30 (0.4) | 29 (0.6) | ||
| Disposition | ||||||
| Hospitalization | 1,658 (25.3) | 1,787 (26.5) | 1,811 (25.9) | 1,230 (26.4) | −37.0 (−42.9 to −30.5) | <.001 |
| Discharged | 4,661 (71.2) | 4,712 (69.9) | 4,933 (70.5) | 3,360 (72.0) | −32.6 (−36.5 to −28.5) | |
| AMA, eloped, LWBS | 217 (3.3) | 237 (3.5) | 240 (3.4) | 64 (1.4) | −75.6 (−82.5 to −66.0) | |
| Died | 11 (0.2) | 8 (0.1) | 9 (0.1) | 12 (0.3) | ||
| Diagnoses | ||||||
| Dizziness (6)†‡ | 166 (2.6) | 190 (2.9) | 178 (2.6) | 103 (2.3) | −49.4 (−30.4 to −63.3) | .12 |
| Syncope (9) c | 78 (1.2) | 101 (1.5) | 115 (1.7) | 44 (1.0) | −70.5 (−53.4 to −81.3) | .001 |
| Headache (2)‡ | 242 (3.7) | 303 (4.5) | 215 (3.1) | 152 (3.3) | −43.5 (−56.8 to −26.2) | .30 |
| Cerebrovascular accident§ | 80 (1.2) | 96 (1.4) | 104 (1.5) | 52 (1.1) | −58.3 (−73.3 to −34.9) | .049 |
| Chest pain (1)‡ | 495 (7.6) | 492 (7.3) | 528 (7.6) | 456 (9.8) | −13.1 (−27.2 to 3.7) | <.001 |
| STEMI, NSTEMI, angina§ | 171 (2.6) | 142 (2.1) | 121 (1.7) | 92 (2.0) | −8.4 (−35.5 to 30.0) | .05 |
| VTE disease† | 43 (0.7) | 40 (0.6) | 38 (0.5) | 24 (0.5) | −32.1 (−65.2 to 32.5) | .89 |
| Congestive heart failure‡ | 145 (2.2) | 134 (2.0) | 144 (2.1) | 115 (2.5) | −13.6 (−38.5 to 21.4) | .09 |
| Shortness of breath | 149 (2.3) | 157 (2.3) | 198 (2.8) | 261 (5.6) | 25.1 (−6.4 to 67.3) | <.001 |
| URI, pharyngitis, sinusitis (7)§ | 260 (4.0) | 253 (3.8) | 282 (4.0) | 247 (5.3) | −10.0 (−29.4 to 14.8) | .01 |
| Asthma or COPD§ | 261 (4.0) | 253 (3.8) | 264 (3.8) | 179 (3.8) | −30.0 (−45.9 to −9.6) | .55 |
| Influenza or pneumonia§ | 215 (3.3) | 153 (2.3) | 358 (5.1) | 152 (3.3) | −40.3 (−55.0 to −21.0) | .53 |
| COVID-19 or coronavirus infection‡ | 0 (0) | 0 (0) | 0 (0) | 20 (0.4) | — | — |
| Abdominal pain (4)‡ | 809 (12.4) | 863 (12.8) | 958 (13.7) | 579 (12.4) | −43.3 (−50.8 to −34.8) | .045 |
| Appendicitis§ | 21 (0.3) | 18 (0.3) | 21 (0.3) | 15 (0.3) | −16.7 (−66.6 to 107.85) | .59 |
| GB, biliary, pancreas§ | 75 (1.1) | 86 (1.3) | 66 (0.9) | 49 (1.1) | −35.3 (−60.0 to 4.9) | .1.0 |
| Renal stone, colic§ | 44 (0.7) | 62 (0.9) | 52 (0.7) | 22 (0.5) | −70.0 (−84.0 to −43.6) | .01 |
| Urinary tract infection§ | 214 (3.3) | 243 (3.6) | 240 (3.4) | 156 (3.3) | −42.8 (−56.4 to −24.8) | .37 |
| Sepsis (3)‡ | 154 (2.4) | 146 (2.2) | 183 (2.6) | 148 (3.2) | −14.7 (−37.6 to 16.7) | .08 |
| Diabetes complications§ | 267 (4.3) | 291 (4.5) | 280 (4.2) | 176 (3.9) | −42.3 (−55.1 to −25.85) | .35 |
| Diabetic ketoacidosis‡ | 26 (0.4) | 20 (0.3) | 32 (0.5) | 29 (0.6) | 17.8 (−45.4 to 154.4) | .13 |
| Injuries§ | 1,080 (16.5) | 933 (13.8) | 1,005 (14.4) | 607 (13.0) | −30.1 (−38.8 to −20.1) | .21 |
| Head injury (5)§ | 427 (7.0) | 378 (5.9) | 419 (6.4) | 254 (5.8) | −31.5 (−44.4 to −15.7) | .59 |
| Fractures‡ | 321 (4.9) | 260 (3.9) | 304 (4.3) | 161 (3.5) | −34.6 (−49.2 to −15.9) | .93 |
| Dental complaints‡ | 93 (1.4) | 111 (1.6) | 91 (1.3) | 61 (1.3) | −43.8 (−63.3 to −14.1) | .51 |
| Back pain (8)§ | 357 (5.5) | 349 (5.2) | 342 (4.9) | 165 (3.5) | −50.7 (−61.1 to −37.4) | .02 |
| Anxiety/stress§ | 249 (3.8) | 292 (4.3) | 251 (3.6) | 195 (4.2) | −33.8 (−48.5 to −14.8) | .86 |
| Depression§ | 300 (4.8) | 342 (5.3) | 307 (4.6) | 227 (5.1) | −35.1 (−48.5 to −18.3) | .99 |
| Suicidal ideation (10)‡ | 196 (3.0) | 225 (3.3) | 201 (2.9) | 179 (3.8) | −22.4 (−41.3 to 2.4) | .20 |
| Intoxication/substance use§ | 945 (16.9) | 994 (17.3) | 1,040 (17.5) | 765 (19.6) | −30.1 (−38.5 to −20.4) | .20 |
| Alcohol withdrawal‡ | 53 (0.8) | 69 (1.0) | 60 (0.9) | 60 (1.3) | −23.2 (−53.7 to 27.4) | .51 |
| Poisoning‡ | 95 (1.5) | 101 (1.5) | 117 (1.7) | 101 (2.2) | −18.8 (−44.8 to 19.5) | .25 |
IQR, interquartile range; OPI, other Pacific Islander; EMS, Emergency Medical Services; ESI, Emergency Severity Index; AMA, against medical advice; LWBS, left without being seen; STEMI, ST-segment elevation myocardial infarction; NSTEMI, non–ST-segment elevation myocardial infarction; VTE, venous thromboembolic; URI, upper respiratory infection; COPD, chronic obstructive pulmonary disease; GB, gallbladder.
P value represents the type III P value for the interaction between the overall change in ED visits and the change in each category of patient and visit characteristics and diagnoses. Bolded values are statistically significant.
Numbers indicate historical top 10 diagnoses for visits to our ED.
Determined from a search of diagnosis names within the first 3 coder diagnoses.
Determined from a search of diagnostic-related groups within the first 3 coder diagnoses.
When we examined diagnoses, we noted significant decreases in the proportions of patients presenting with syncope (−70.5%), cerebrovascular accidents (−58.3%), abdominal pain (−43.3%), urolithiasis (−70.0%), and back pain (−50.7%). We also saw significant increases in the proportions of patients presenting with upper respiratory infections (−10.0%), shortness of breath (25.1%), and chest pain (−13.1%). For all other conditions, the declines in presentations were proportionate to the overall change in ED visits.
When we looked at charges, there was a 32.8% (95% CI −36.1% to −29.4%) reduction in total ED charges, and a 23.2% (95% CI −27.6% to −18.7%) reduction in hospital charges, with respect to 2019 when adjusted for inflation and without changes in billing or reimbursement rates between periods. Decreases in ED charges by level of urgency were generally proportionate to the overall adjusted decline in ED visits, although the decline in ED charges for urgency level 5 visits was smaller (−26.2%; 95% CI −43.5% to −3.5%). The decline in hospital charges for urgency level 1 visits was disproportionately large (−42.1%; 95% CI −59.6% to −17.2%), whereas the decline in hospital charges for urgency levels 2 and 4 visits was smaller than the overall adjusted decline in ED visits (−19.2%; 95% CI −26.7% to −10.9%; and −17.6; 95% CI −30.9% to −1.7%).
Limitations
This study is limited by its single-center and cross-sectional nature, the short study time frame, and lack of adjustment for multiple potentially confounding factors related to patients and their presentations to the ED, including disease severity, comorbidities, and COVID-19 risk factors. However, we have found notable differential changes in the demographic factors, visit characteristics, and diagnoses of presentations to the ED.
Discussion
Echoing anecdotal reports, we noted a temporal association between our state’s emergency declaration and a gradual but significant overall decline in daily ED visits. We also noted significant albeit smaller declines in both ED and hospital charges, a difference that may be attributable to changes in urgency or severity distribution. Both phenomena have been experienced by EDs and health systems across the country, thus prompting staff furloughs and other responses even as preparations are made for a growing number of patients with SARS-CoV-2 infection.
In addition, we found significant changes in ED patient demographics and visit characteristics. We found significant proportional decreases in visits by the overlapping populations of patients older than 65 years of age and Medicare recipients. There were also significant disproportionate declines in visits by pediatric and ambulatory patients, women, and certain racial categories. We also noted a disproportionate decline in the number of patients who left before evaluation or discharge. That change may in part reflect the substantial operational changes made in response to the pandemic. Those changes have further streamlined patient triage, rooming, and evaluation, thereby potentially decreasing triage bottlenecks that can occur when the department is more crowded.
We also found significant changes in the diagnoses of patients presenting to the ED. We saw significant proportional increases in ED visits for upper respiratory infections, chest pain, and shortness of breath. These are symptoms that could bring patients to the ED with concerns for COVID-19 infection, but they may also represent exacerbations and presentations of other conditions. The most concerning finding of this report, however, is the overall decline in patients seen for acute and potentially life-threatening conditions unrelated to COVID-19.1 One would expect to find, as we did, a disproportionate decrease in presentations of less acute conditions such as back pain and other nonspecific pain. However, we also found unexpectedly disproportionate declines in visits for conditions of substantially higher urgency or severity, such as syncope, cerebrovascular accidents, and urolithiasis, similar to those noted elsewhere for presentations of myocardial infarction.3 , 4 Similar trends in patient presentations have been seen around the world,5 during prior disease outbreaks,6 and in the outpatient setting.7
These changes in patient presentation patterns may reflect concerns about contracting COVID-19 in health care settings, overburdening the health care system with unrelated conditions, and adhering to public health recommendations.1 It is also possible that they are related to changing patterns of activity leading to a change in disease incidence or to the increased availability of other venues for seeking care, such as telemedicine. Changes in activity noted during the pandemic could contribute to diminished air pollution, traffic, and infectious disease transmission. Such phenomena could potentially contribute to improved population health over the long term and to a decreased incidence of exacerbations of respiratory conditions, COVID-19 infections,8 or traumatic injuries in the short term. However, most of the other conditions seen and managed in the ED would not be expected to decrease in incidence suddenly. Alternative care venues such as telemedicine have also been developed and are expanding, offering valuable ways to provide continued outpatient care. Telemedicine providers can care for many nonacute concerns and ambulatory care–sensitive conditions, but patients with concerning symptoms or significant diagnostic uncertainty may still need to be referred to the ED for evaluation.7 Most local telemedicine alternatives were not substantially established or bolstered until at least 2 weeks after the state announcement. As such, telemedicine would not be expected to have a major impact on the number of patients presenting with acute medical conditions over the study period.
These are still early days, and the timeline for the COVID-19 pandemic and resulting changes in patterns of ED use promises to be much longer than that covered in our preliminary study. Further efforts should and are being made to reassure and affirm the appropriateness of seeking emergency care,9 particularly for the groups and disease processes highlighted here and elsewhere.1 , 3 , 4 Further research will also be needed to examine these and other factors contributing to delayed or deferred care and to monitor for the morbidity and mortality that are likely to result4 , 7 and that may already be occurring.10
Acknowledgments
The authors would like to thank Hrafn P. Gudjonsson (“Patrick”) for his valuable assistance in querying and creating the data set used in this study.
Footnotes
Please see page 596 for the Editor’s Capsule Summary of this article.
Supervising editor: Daniel A. Handel, MD, MBA. Specific detailed information about possible conflict of interest for individual editors is available at https://www.annemergmed.com/editors.
Author contributions: BCW, MWM, and MDZ contributed to the study conception and design, material preparation, and data collection. GV-B and LOE performed the analyses. The first draft of the manuscript was written by BCW and MWM. All authors commented on previous versions and have read and approved the final manuscript for submission. BCW takes responsibility for the paper as a whole.
All authors attest to meeting the four ICMJE.org authorship criteria: (1) Substantial contributions to the conception or design of the work; or the acquisition, analysis, or interpretation of data for the work; AND (2) Drafting the work or revising it critically for important intellectual content; AND (3) Final approval of the version to be published; AND (4) Agreement to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Funding and support: By Annals policy, all authors are required to disclose any and all commercial, financial, and other relationships in any way related to the subject of this article as per ICMJE conflict of interest guidelines (see www.icmje.org). The authors have stated that no such relationships exist.
A podcast for this article is available at www.annemergmed.com.
Supplementary Data
Additional statistical information.
References
- 1.Wong L.E., Hawkins J.E., Langness S. Where are all the patients? Addressing Covid-19 fear to encourage sick patients to seek emergency care. NEJM Catal. 2020 https://catalyst.nejm.org/doi/full/10.1056/CAT.20.0193?query=C19 Available at: [Google Scholar]
- 2.Bakst B. Minnesota Public Radio News; March 13, 2020. Walz advises no gatherings over 250 people as MN COVID-19 cases hit 14.https://www.mprnews.org/story/2020/03/13/14-covid19-cases-now-in-mn-walz-to-unveil-new-control-measures Available at: [Google Scholar]
- 3.Garcia S., Albaghdadi M.S., Meraj P.M. Reduction in ST-segment elevation cardiac catheterization laboratory activations in the United States during COVID-19 pandemic. J Am Coll Cardiol. 2020;75:2871–2872. doi: 10.1016/j.jacc.2020.04.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Tam D.F., Cheung K., Lam S. Impact of coronavirus disease 2019 (COVID-19) outbreak on ST-segment–elevation myocardial infarction care in Hong Kong, China. Circ Cardiovasc Qual Outcomes. 2020;13 doi: 10.1161/CIRCOUTCOMES.120.006631. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Ong CW, Goletti D. Impact of the global COVID-19 outbreak on the management of other communicable diseases. Int J Tuberc Lung Dis. 20201;24:547-548 [DOI] [PubMed]
- 6.Huang Y.T., Lee Y.C., Hsiao C.J. Hospitalization for ambulatory-care-sensitive conditions in Taiwan following the SARS outbreak: a population-based interrupted time series study. J Formos Med Assoc. 2009;108:386–394. doi: 10.1016/S0929-6646(09)60082-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Rosenbaum L. The untold toll — the pandemic’s effects on patients without Covid-19. N Engl J Med. 2020;382:2368–2371. doi: 10.1056/NEJMms2009984. [DOI] [PubMed] [Google Scholar]
- 8.Wu X., Nethery R.C., Sabath B.M. Exposure to air pollution and COVID-19 mortality in the United States. Preprint. medRxiv. 2020 doi: 10.1126/sciadv.abd4049. 2020.04.05.20054502. doi:10.1101/2020.04.05.20054502. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.American College of Emergency Physicians Amidst COVID-19 concerns, emergency physicians urge public not to delay necessary medical care. Press release. April 15, 2020. https://www.emergencyphysicians.org/press-releases/2020/4-15-20-amidst-covid-19-concerns-emergency-physicians-urge-public-not-to-delay-necessary-medical-care Available at:
- 10.Leon D.A., Schkolnikov V.M., Smeeth L. COVID-19: a need for real-time monitoring of weekly excess deaths. Lancet. 2020;395:e81. doi: 10.1016/S0140-6736(20)30933-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Additional statistical information.