Highlights
-
•
Unenhanced chest CT is indicated for patients with suspected COVID-19 presenting with dyspnea, polypnea or arterial blood oxygen desaturation.
-
•
Most typical CT features of COVID-19 pneumonia include bilateral and multifocal ground-glass opacities predominating in the peripheral, posterior and basal parts of the lungs.
-
•
Between 15 and 30% of hospitalized patients with COVID-19 progress to acute respiratory distress syndrome, which is the main cause of mortality.
Keywords: COVID-19, Tomography, X-ray computed, Severe acute respiratory syndrome coronavirus 2, Pulmonary embolism
Abbreviations: AI, Artificial Intelligence; ARDS, Acute Respiratory Distress Syndrome; COVID-19, coronavirus disease 2019; CT, Computed Tomography; RT-PCR, Reverse Transcriptase Polymerase Chain Reaction; SARS-CoV-2, Severe Acute Respiratory Syndrome Coronavirus 2
Abstract
The current COVID-19 pandemic has highlighted the essential role of chest computed tomography (CT) examination in patient triage in the emergency departments, allowing them to be referred to “COVID” or “non-COVID” wards. Initial chest CT examination must be performed without intravenous administration of iodinated contrast material, but contrast material administration is required when pulmonary embolism is suspected, which seems to be frequent in severe forms of the disease. Typical CT features consist of bilateral ground-glass opacities with peripheral, posterior and basal predominance. Lung disease extent on CT correlates with clinical severity. Artificial intelligence could assist radiologists for diagnosis and prognosis evaluation.
1. Introduction
By June 16, 2020, the COVID-19 pandemic had affected more than 7.8 million people worldwide, resulting in 477,474 deaths [1]. The most typical clinical presentation of COVID-19 is an acute febrile respiratory infection with dry cough, dyspnea, fatigue and myalgia. Approximately 15–20% of patients have severe disease and the mortality is around 2-3% [2], [3], [4].
In the absence of vaccine or specific therapy available to date, it is essential to be able to diagnose this disease as early as possible in order to isolate infected subjects and thus limit the spread of the disease. The method of reference is laboratory testing of nasopharyngeal aspirates for identification of SARS-CoV-2 by reverse transcriptase-polymerase chain reaction (RT-PCR). However, it takes several hours to obtain the results, and the sensitivity of the test is only 60 to 70%, depending on the quality of the sample and the rate of viral replication in the upper respiratory tract [5], [6].
Chest computed tomography (CT) has rapidly emerged as a rapid and effective diagnostic tool, given the often quite characteristic presentation of COVID-19 pneumonia [7], [8]. Now that the “first wave” has passed and the pandemic appears to be under control, we propose to review and update the current knowledge on COVID-19 pneumonia imaging.
2. Role of chest CT in the management of suspected patients
The massive arrival of patients suspected of having COVID-19 pneumonia in emergency departments has prompted the setting up of “COVID” and “non COVID” pathways, making it necessary to triage patients as early as possible. According to the ESR/ESTI advice paper and recommendations of the French Society of Thoracic Imaging, unenhanced chest CT is currently indicated for patients presenting with dyspnea, polypnea or desaturation in order to refer them to “COVID” or “non COVID” wards, pending RT-PCR results [9]. Chest CT sensitivity for the diagnosis of COVID-19 is greater than 90%, with false-negative findings mostly in patients who are symptomatic for less than 3 days [5], [10]. CT specificity is more variable. Series from China and Italy reported specificity values between 25% and 56% [5], [11]. A meta-analysis, including mainly Asian studies, reported pooled sensitivity and specificity of 94% and 37% respectively for the diagnosis of COVID-19 pneumonia [12]. Furthermore, this meta-analysis reported a high degree of variability in positive predictive value of chest CT according to prevalence. Depending on whether the prevalence is 1%, 10% or 39%, the positive predictive value would become 1.5%, 14.2% or 48.8%, respectively. Thus, the use of CT as a screening tool in low prevalence areas would lead to a large number of false positives. In addition, it should be noted that inter-reader agreement of chest CT for COVID-19 diagnosis is generally reported to be good or even excellent [13], [14].
In practice, chest CT results can lead to three scenarios:
-
•
when chest CT is very suggestive of COVID-19, the patient will be hospitalized in a COVID-19 isolation ward, and RT-PCR testing will generally confirm the diagnosis;
-
•
when chest CT shows an obvious alternate diagnosis (e.g. bacterial lobar pneumonia or left ventricular failure), the patient will be hospitalized in a “non COVID-19” ward;
-
•
when chest CT findings are indeterminate, RT-PCR testing along with clinical symptoms will be essential for referral to the most appropriate ward.
Chest CT scans should not be performed for screening purpose in asymptomatic patients. Neither chest X-ray nor ultrasonography is recommended for the diagnosis of COVID-19, as their performance appears to be significantly inferior to that of CT.
3. Typical CT presentation
The most typical CT features of COVID-19 pneumonia are bilateral and multifocal ground-glass opacities. Lesions classically predominate in the peripheral, posterior and basal part of the lungs (Fig. 1 ) [10]. Other signs have been reported such as the presence of fine reticulations, peribronchovascular thickening, vascular dilatations within pneumonia areas, or architectural distortion [15]. Usually, there are no micronodules, excavations, septal lines, mediastinal lymph node enlargement or pleural effusions. Some infected but asymptomatic patients may have slight ground-glass opacities but these are generally not extensive [16].
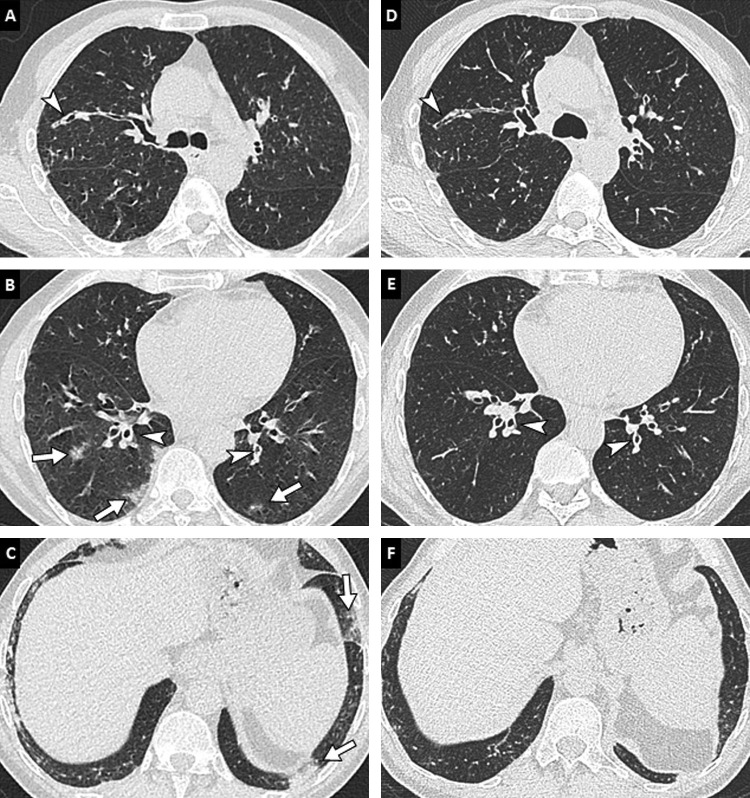
Fig. 1.
64-year-old man with COVID-19 pneumonia. Unenhanced CT images of the chest (lung window: W1600/L-500 HU) in the axial (A, B) and coronal (C, D) planes reveal bilateral multifocal ground-glass opacities (arrows) predominantly located in the peripheral and posterior part of the lungs.
Chest CT appearance of COVID-19 pneumonia may be quite similar to that of other viral pneumonitis. However, the peripheral location of the lesions, involvement of the five lobes, the presence of thin reticulations and peribronchovascular thickening would be more frequently found in COVID-19 pneumonitis [17], [18]. In influenza pneumonia, nodular or micronodular tree-in-bud pattern may be more common, as may pleural effusions [19].
4. Atypical CT presentation
In approximately 10% of patients, lung involvement of by COVID-19 pneumonia may present as arciform or pseudonodular consolidation suggesting a pattern of organizing pneumonia [20], sometimes with a “reverse halo sign” similar to the one observed in other infectious diseases [21]. Unilateral presentation is possible in about 20–30% of patients, usually at an early stage before bilateralization of the lesions [5], [22]. Peribronchovascular or apical predominance is also described (Fig. 2 ) [23]. When COVID-19 pneumonia occurs in a previously abnormal lung (e.g., with underlying emphysema or fibrosis), CT presentation becomes less specific, making a careful comparison with previous CT examinations, when available, mandatory (Fig. 3 ) [24].
Fig. 2.
Unenhanced CT examination in a 26-year-old woman with COVID-19 pneumonia. Unenhanced CT image of the chest (lung window: W1600/L-500 HU) in the axial plane reveals apical and perihilar predominant pulmonary lesions (arrows) with a “reverse halo sign” (arrowhead).
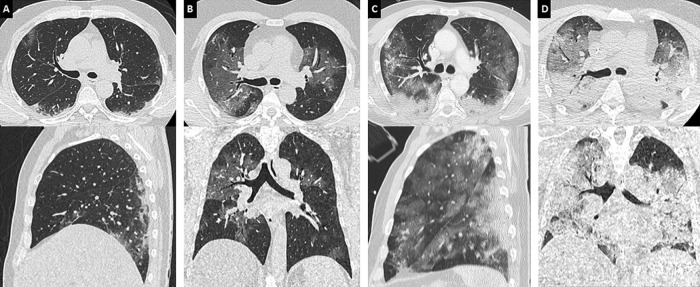
Fig. 3.
75-year-old man with history of chronic bronchiolitis recently diagnosed with COVID-19 pneumonia. (A, B, C) Chest CT images in the axial plane show multifocal, patchy, ground-glass opacities (arrows) as well as diffuse thickening of bronchial walls (arrowheads). (D, E, F) The diagnosis of COVID-19 pneumonia was facilitated by the comparison with chest CT images obtained 2 months earlier that already showed bronchitis and bronchiolitis (arrowheads) but no lung opacities.
5. Evolution of CT findings
Ground-glass opacities tend to progress over time, both in extent and attenuation value, and evolve either towards crazy paving areas (i.e., superimposition of ground-glass and intra-lobular reticulations), or towards linear and retractile consolidation areas (Fig. 4 ) [10], [25], [26], [27]. Lung damage is maximal at around day 10 and then generally decreases progressively in size and attenuation value [28]. However, early available data on the late appearance of lung parenchyma are still scarce. While complete resolution seems to be common in patients with mild pneumonia, it seems that many patients, especially those with initial severe disease, still present reticular pattern of fibrotic streaks after more than one month of evolution (Fig. 4). According to a recent study, lung abnormalities could persist beyond one month in 98% of patients [29]. There is therefore some concern about a significant number of pulmonary fibrotic sequelae, although the proportion is not yet known [15], [26].
Fig. 4.
78-year-old woman with COVID-19 pneumonia. (A, B) Initial unenhanced chest CT image in the axial plane (lung window: W1600/L-500 HU) shows bilateral and peripheral areas of ground-glass and consolidation. (C, D) Follow-up contrast-enhanced CT images performed 13 days later to rule out pulmonary embolism reveal progression in extent and in density of pulmonary lesions with a crazy paving pattern (white arrowheads) and consolidation areas (arrows). (E, F) Contrast-enhanced CT images obtained 28 days after the onset of symptoms show partial regression of consolidation areas but persistence of fibrotic streaks (black arrowheads) with architectural distortion.
6. Severity signs
The total extent of lung involvement on the first CT examination correlates with clinical severity [13], [25], [30]. The French Society of Thoracic Imaging (SIT) recommends grading lung involvement as absent or minimal (< 10%), moderate (10–25%), extensive (25–50%), severe (50–75%) or critical (> 75%) (Fig. 5 ). The density of pulmonary lesions is also a marker of severity, since lung consolidation areas appear more extensive than ground-glass opacities in critically ill patients [30]. Pleural effusion and early architectural distortion with traction bronchiectasis on initial chest CT would also indicate a poor prognosis [15]. A Chinese series suggests that consolidation in upper lobes on initial CT is also associated with poor outcomes [31].
Fig. 5.
Various degrees of lung involvement in COVID-19 pneumonia in four different patients. Unenhanced CT images of the chest (lung window: W 1600/L–500 HU) in the axial (up) and coronal (down) planes show typical examples of moderate (< 25%), extensive (25–50%), severe (50–75%) and critical (> 75%) lung involvement (A, B, C, D, respectively). The latter images are (D) characteristic of acute respiratory distress syndrome with a gravitationally dependent gradient.
7. Complications
Between 15 and 30% of hospitalized patients progress to acute respiratory distress syndrome (ARDS), which is the main cause of mortality in COVID-19. ARDS is characterized in CT by extensive bilateral lung consolidation with a predominance in dependent areas (Fig. 5) [4], [32]. In addition, several complications can occur in the clinical course of these patients. Pulmonary bacterial superinfection will be suspected in case of additional alveolar consolidation areas with pleural effusion and/or enlarged lymph nodes [15]. In a recent study, COVID-19 associated pulmonary aspergillosis was reported in 5 of 19 consecutive patients with ARDS (Fig. 6 ) [33]. However, distinction between COVID-19 and pulmonary aspergillosis lesions with CT remains difficult [34].
Fig. 6.
59-year-old man with COVID-19 and a 3-fold positive endotracheal swab for aspergillus fumigatus. Unenhanced CT images of the chest in the axial (A) and coronal (B) planes (lung window: W 1600/L–500 HU) show subpleural ground-glass opacities presumed to correspond to COVID-19 lesions (arrowheads) as well as an extensive apical consolidation area presumed to correspond to invasive aspergillosis (arrow).
Pulmonary embolism has been reported in COVID-19 patients (Fig. 7 ) [35], [36], [37], [38]. In critically ill patients, there is an exacerbated systemic inflammatory response leading to a hypercoagulability state, reflected by the marked increase of D-dimer serum level in these patients [39]. The occurrence of pulmonary embolism is mainly reported in intensive care unit patients, based on retrospective studies. The exact prevalence of pulmonary embolism in COVID19 remains unknown, and would require a prospective evaluation, with systematic assessment of clinical symptoms, CT features and D-dimers. Routine CT pulmonary angiography to check for pulmonary embolism is so far not indicated as a first-line diagnostic tool. However, a clinical-radiological discordance (dyspnea and hypoxemia without lung abnormality) or respiratory worsening in a known COVID-19 patient should prompt the use of contrast medium injection. It would be worth assessing the value of routine CT pulmonary angiography in patients with highly elevated D-dimer levels. Finally, radiologists should be aware that pulmonary infarction secondary to pulmonary embolism may be quite similar in appearance to COVID-19 pneumonia (Fig. 8 ).
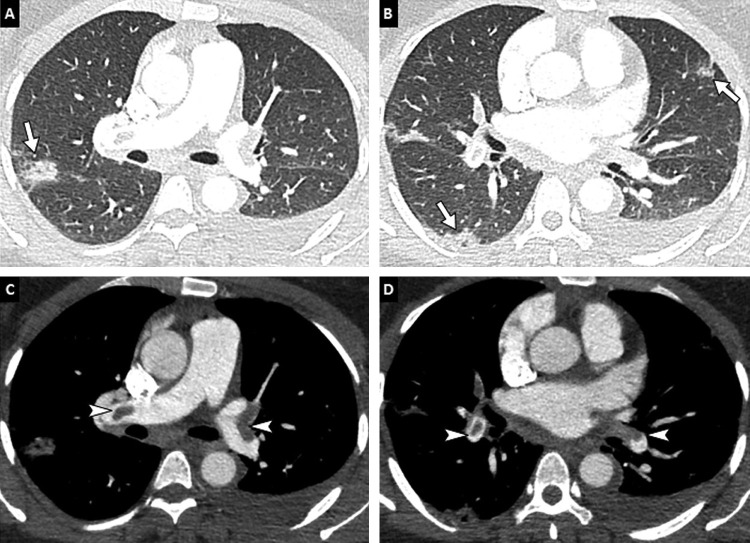
Fig. 7.
36-year-old woman positive for COVID-19 and pulmonary embolism. CT pulmonary angiography images in the axial (A, B) and coronal (C, D) planes show typical peripheral ground-glass areas related to COVID-19 pneumonia (arrows) and bilateral proximal pulmonary embolism (arrowheads).
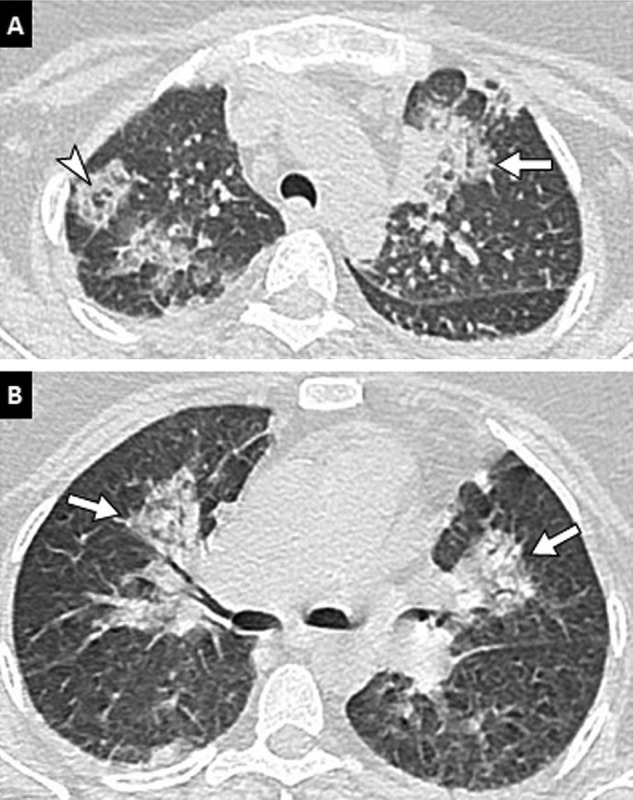
Fig. 8.
74-year-old woman with COVID-19 pneumonia. (A, B) Baseline CT images obtained after intravenous administration of contrast material show peripheral ground-glass opacities (black arrowheads), bilateral proximal pulmonary embolism (white arrowheads) and a quadrangular well-demarcated subpleural consolidation containing central lucencies corresponding to a pulmonary infarction (arrow). (C, D) Follow-up CT images obtained 7 days later show progression of COVID-19 pulmonary lesions with reticulations, fibrotic streaks and architectural distortion (black arrowheads) and persisting thrombus (white arrowhead).
8. Specificities in children and pregnant women
In the pediatric population, pulmonary involvement on CT is often less extensive than in adults. There are often no CT abnormalities [40]. In case of lung involvement, ground glass is the predominant sign [40], [41]. The “halo sign” is found more frequently than in adults [39], [41]. Coinfections, especially viral, are also more frequent [42].
In pregnant women, there is no evidence of maternal-fetal transmission of SARS-CoV-2 and no specific per or post-partum complications [43]. Consolidation might be more common than in the general population [44]. It appears to be no increased mortality related to COVID-19 in pregnant women [45].
9. Artificial intelligence (AI) in imaging of COVID-19
Machine learning techniques have the potential to dramatically transform medical imaging [46], [47], [48]. Several deep learning and radiomics based tools are currently being developed for automated diagnosis, quantification of lesion extension and prognostic estimation of COVID19 pneumonia. They show great promise for making the positive diagnosis of COVID-19 pneumonia, for automatically quantifying pulmonary lesion extension and for identifying biomarkers that could be of prognostic interest. In a study from the city of Wuhan in China, carried out on a database of 4356 CT examinations (30% with COVID-19, 40% with community pneumonia and 30% with non-infectious pneumonia), a deep learning model diagnosed COVID-19 pneumonia with a sensitivity of 90% and a specificity of 96%, allowing reliable differential diagnosis with community acquired pneumonia [49]. Huang et al. trained a deep learning algorithm on an annotated database of 842 COVID-19 patients, and tested it on an independent series of 126 patients. The percentages of lung involvement were significantly different for mild, moderate and severe clinical conditions, and automatic quantification also allowed longitudinal follow-up of patients [50].
AI certainly has an important role to play in assessing the prognosis of COVID-19 and identifying biomarkers predictive of patient outcomes. For this purpose, several national and international databases are currently being built to enable AI models to be trained on massive data.
10. Conclusion
CT imaging plays a key role in the management of COVID-19 pneumonia, particularly for early evaluation by allowing rapid triage of dyspneic patients, and also in the event of clinical worsening to detect complications, particularly thromboembolic ones. Pulmonary CT extension correlates with clinical severity and should be assessed in a semi-quantitative manner by the radiologist. In a near future, AI techniques should make it possible to automate the positive diagnosis as well as the quantitative assessment of lesions, and perhaps allow the extraction of biomarkers to predict the outcome of COVID-19 patients.
Informed consent and patient details
The authors declare that this report does not contain any personal information that could lead to the identification of the patient(s).
Disclosure of interest
The authors declare that they have no competing interest.
Funding
This work did not receive any grant from funding agencies in the public, commercial, or not-for-profit sectors.
Author contributions
All authors attest that they meet the current International Committee of Medical Journal Editors (ICMJE) criteria for Authorship.
CRediT authorship contribution statement
Carole Jalaber: writing- original draft preparation- literature research, reviewing and editing.
Thibaut Lapotre: reviewing and editing.
Thibaud Morcet-Delattre: reviewing and editing.
Felix Ribet: reviewing and editing.
Stéphane Jouneau: reviewing and editing.
Mathieu Lederlin: writing- reviewing and editing.
References
- 1.https://www.santepubliquefrance.fr/maladies-et-traumatismes/maladies-et-infections-respiratoires/infection-a-coronavirus/articles/infection-au-nouveau-coronavirus-sars-cov-2-covid-19-france-et-monde#block-242818
- 2.Wu Z., McGoogan J.M. Characteristics of and important lessons from the coronavirus disease 2019 (COVID-19) outbreak in China: summary of a report of 72,314 cases from the Chinese Center for Disease Control and Prevention. JAMA. 2020 doi: 10.1001/jama.2020.2648. [DOI] [PubMed] [Google Scholar]
- 3.Guan W., Ni Z., Hu Y., Liang W., Ou C., He J. Clinical characteristics of coronavirus disease 2019 in China. N Engl J Med. 2020 doi: 10.1056/NEJMoa2002032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Huang C., Wang Y., Li X. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet. 2020;395:497. doi: 10.1016/S0140-6736(20)30183-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Ai T., Yang Z., Hou H., Zhan C., Chen C., Lv W. Correlation of chest CT and RT-PCR testing in coronavirus disease 2019 (COVID-19) in China: a report of 1014 cases. Radiology. 2020 doi: 10.1148/radiol.2020200432.200642. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Fang Y., Zhang H., Xie J., Lin M., Ying L., Pang P. Sensitivity of chest CT for COVID-19: comparison to RT-PCR. Radiology. 2020 doi: 10.1148/radiol.2020200432. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Pan F., Ye T., Sun P., Gui S., Liang B., Li L. Time course of lung changes at chest CT during recovery from coronavirus disease 2019 (COVID-19) Radiology. 2020;295:715–721. doi: 10.1148/radiol.2020200370. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Hani C., Trieu N.H., Saab I., Dangeard S., Bennani S., Chassagnon G. COVID-19 pneumonia: a review of typical CT findings and differential diagnosis. Diagn Interv Imagin. 2020;101:263–268. doi: 10.1016/j.diii.2020.03.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Revel M.-P., Parkar A.P., Prosch H., Silva M., Sverzellati N. COVID-19 patients and the radiology department–advice from the European Society of Radiology (ESR) and the European Society of Thoracic Imaging (ESTI) Eur Radiol. 2020 doi: 10.1007/s00330-020-06865-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Bernheim A., Mei X., Huang M., Yang Y., Fayad Z.A., Zhang N. Chest CT findings in coronavirus disease-19 (COVID-19): relationship to duration of infection. Radiology. 2020;295:200463. doi: 10.1148/radiol.2020200463. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Caruso D., Zerunian M., Polici M., Pucciarelli F., Polidori T., Rucci C. Chest CT features of COVID-19 in Rome, Italy. Radiology. 2020 doi: 10.1148/radiol.2020201237. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Kim H., Hong H., Yoon S.H. Diagnostic performance of CT and reverse transcriptase-polymerase chain reaction for coronavirus disease 2019: a meta-analysis. Radiology. 2020 doi: 10.1148/radiol.2020201343. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Yang R., Li X., Liu H., Zhen Y., Zhang X., Xiong Q. Chest CT severity score: an imaging tool for assessing severe COVID-19. Radiol Cardiothorac Imaging. 2020;2:e200047. doi: 10.1148/ryct.2020200047. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Himoto Y., Sakata A., Kirita M. Diagnostic performance of chest CT to differentiate COVID-19 pneumonia in non-high-epidemic area in Japan. Jpn J Radiol. 2020;38:400–406. doi: 10.1007/s11604-020-00958-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Zhao W., Zhong Z., Xie X., Yu Q., Liu J. Relation between chest CT findings and clinical conditions of coronavirus disease (COVID-19) pneumonia: a multicenter study. Am J Roentgenol. 2020;214:1072–1077. doi: 10.2214/AJR.20.22976. [DOI] [PubMed] [Google Scholar]
- 16.Inui S., Fujikawa A., Jitsu M., Kunishima N., Watanabe S., Suzuki Y. Chest CT findings in cases from the cruise ship “Diamond Princess” with coronavirus disease 2019 (COVID-19) Radiol Cardiothorac Imaging. 2020;2:e200110. doi: 10.1148/ryct.2020200110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Bai H.X., Hsieh B., Xiong Z., Halsey K., Choi J.W., Tran T.M.L. Performance of radiologists in differentiating COVID-19 from viral pneumonia on chest CT. Radiology. 2020 doi: 10.1148/radiol.2020200823. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Li X., Fang X., Bian Y., Lu J. Comparison of chest CT findings between COVID-19 pneumonia and other types of viral pneumonia: a two-center retrospective study. Eur Radiol. 2020 doi: 10.1007/s00330-020-06925-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Liu M., Zeng W., Wen Y., Zheng Y., Lv F., Xiao K. COVID-19 pneumonia: CT findings of 122 patients and differentiation from influenza pneumonia. Eur Radiol. 2020 doi: 10.1007/s00330-020-06928-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Bekci T. “Reversed halo sig” on 3D CT in COVID-19. Diagn Interv Radiol. 2020 doi: 10.5152/dir.2020.20254. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Martini K., Loubet A., Bankier A., Bouam S., Morand P., Cassagnes L. Nodular reverse halo sign in active pulmonary tuberculosis: a rare CT feature? Diagn Interv Imaging. 2020;101:281–287. doi: 10.1016/j.diii.2020.01.013. [DOI] [PubMed] [Google Scholar]
- 22.Shi H., Han X., Jiang N., Cao Y., Alwalid O., Gu J. Radiological findings from 81 patients with COVID-19 pneumonia in Wuhan, China: a descriptive study. Lancet Infect Dis. 2020;20:425–434. doi: 10.1016/S1473-3099(20)30086-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Chung M., Bernheim A., Mei X., Zhang N., Huang M., Zeng X. CT imaging features of 2019 novel coronavirus (2019-nCoV) Radiology. 2020;295:202–207. doi: 10.1148/radiol.2020200230. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Langlet B., Dournes G., Laurent F. CT features of pulmonary interstitial emphysema. Diagn Interv Imaging. 2019;100:825–826. doi: 10.1016/j.diii.2019.04.004. [DOI] [PubMed] [Google Scholar]
- 25.Xiong Y., Sun D., Liu Y., Fan Y., Zhao L., Li X. Clinical and high-resolution CT features of the COVID-19 infection: comparison of the initial and follow-up changes. Invest Radiol. 2020;55:332–339. doi: 10.1097/RLI.0000000000000674. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Wang Y., Dong C., Hu Y., Li C., Ren Q., Zhang X. Temporal changes of CT findings in 90 patients with COVID-19 pneumonia: a longitudinal study. Radiology. 2020 doi: 10.1148/radiol.2020200843. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Liang T., Liu Z., Wu C.C., Jin C., Zhao H., Wang Y. Evolution of CT findings in patients with mild COVID-19 pneumonia. Eur Radiol. 2020 doi: 10.1007/s00330-020-06823-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Zhou S., Zhu T., Wang Y., Xia L. Imaging features and evolution on CT in 100 COVID-19 pneumonia patients in Wuhan, China. Eur Radiol. 2020 doi: 10.1007/s00330-020-06879-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Ding X., Xu J., Zhou J., Long Q., Chest C.T. findings of COVID-19 pneumonia by duration of symptoms. Eur J Radiol. 2020;127:109009. doi: 10.1016/j.ejrad.2020.109009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Li K., Wu J., Wu F., Guo D., Chen L., Fang Z. The clinical and chest CT features associated with severe and critical COVID-19 pneumonia. Invest Radiol. 2020;55:327–331. doi: 10.1097/RLI.0000000000000672. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Yu Q., Wang Y., Huang S., Liu S., Zhou Z., Zhang S. Multicenter cohort study demonstrates more consolidation in upper lungs on initial CT increases the risk of adverse clinical outcome in COVID-19 patients. Theranostics. 2020;10:5641–5681. doi: 10.7150/thno.46465. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Wang D., Hu B., Hu C., Zhu F., Liu X., Zhang J. Clinical characteristics of 138 hospitalized patients with 2019 novel coronavirus–infected pneumonia in Wuhan, China. JAMA. 2020;323:1061–1069. doi: 10.1001/jama.2020.1585. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Koehler P., Cornely O., Böttiger B., Dusse F., Eichenauer D. COVID-19 associated pulmonary aspergillosis. Mycoses. 2020 doi: 10.1111/myc.13096. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Rutsaert L., Steinfort N., Van Hunsel T., Bomans P., Naesens R. COVID-19-associated invasive pulmonary aspergillosis. Ann Intensive Care. 2020 doi: 10.1186/s13613-020-00686-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Grillet F., Behr J., Calame P., Aubry S., Delabrousse E. Acute pulmonary embolism associated with COVID-19 pneumonia detected by pulmonary CT angiography. Radiology. 2020 doi: 10.1148/radiol.2020201544. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Leonard-Lorant I., Delabranche X., Severac F., Helms J., Pauzet C., Collange O. Acute pulmonary embolism in COVID-19 patients on CT angiography and relationship to D-dimer levels. Radiology. 2020 doi: 10.1148/radiol.2020201561. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Poissy J., Goutay J., Caplan M., Parmentier E., Duburcq T., Lassalle F. Pulmonary embolism in COVID-19 patients: awareness of an increased prevalence. Circulation. 2020 doi: 10.1161/circulationaha.120.047430. [DOI] [PubMed] [Google Scholar]
- 38.Bompard F., Monnier H., Saab I., Tordjman M., Abdoul H., Fournier L. Pulmonary embolism in patients with Covid-19 pneumonia. Eur Respir J. 2020 doi: 10.1183/13993003.01365-2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Tang N., Li D., Wang X., Sun Z. Abnormal coagulation parameters are associated with poor prognosis in patients with novel coronavirus pneumonia. J Thromb Haemost. 2020;18:844–847. doi: 10.1111/jth.14768. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Song W., Li J., Zou N., Guan W., Pan J., Xu W. Clinical features of pediatric patients with coronavirus disease (COVID-19) J Clin Virol. 2020;127:104377. doi: 10.1016/j.jcv.2020.104377. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Zhen-Dong Y., Gao-Jun Z., Run-Ming J., Zhi-Sheng L., Zong-Qi D., Xiong X. Clinical and transmission dynamics characteristics of 406 children with coronavirus disease 2019 in China: a review. J Infect. 2020 doi: 10.1016/j.jinf.2020.04.030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Xia W., Shao J., Guo Y., Peng X., Li Z., Hu D. Clinical and CT features in pediatric patients with COVID-19 infection: different points from adults. Pediatr Pulmonol. 2020;55:1169–1174. doi: 10.1002/ppul.24718. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Qiao J. What are the risks of COVID-19 infection in pregnant women? Lancet. 2020;395:760–762. doi: 10.1016/S0140-6736(20)30365-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Liu H., Liu F., Li J., Zhang T., Wang D., Lan W. Clinical and CT imaging features of the COVID-19 pneumonia: focus on pregnant women and children. J Infect. 2020;80:e7–e13. doi: 10.1016/j.jinf.2020.03.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Schwartz D.A. An analysis of 38 pregnant women with COVID-19, their newborn infants, and maternal-fetal transmission of SARS-CoV-2: maternal coronavirus infections and pregnancy outcomes. Arch Pathol Lab Med. 2020 doi: 10.5858/arpa.2020-0901-SA. [DOI] [PubMed] [Google Scholar]
- 46.Waymel Q., Badr S., Demondion X., Cotten A., Jacques T. Impact of the rise of artificial intelligence in radiology: what do radiologists think? Diagn Interv Imaging. 2019;100:327–3236. doi: 10.1016/j.diii.2019.03.015. [DOI] [PubMed] [Google Scholar]
- 47.Colevray M., Tatard-Leitman Vm, Gouttard S., Douek P., Boussel L. Convolutional neural network evaluation of over-scanning in lung computed tomography. Diagn Interv Imaging. 2019;100:177–183. doi: 10.1016/j.diii.2018.11.001. [DOI] [PubMed] [Google Scholar]
- 48.SFR-IA Group; CERF; French Radiology Community Artificial intelligence and medical imaging 2018: French radiology community white, paper. Diagn Interv Imaging. 2018;99:727–742. doi: 10.1016/j.diii.2018.10.003. [DOI] [PubMed] [Google Scholar]
- 49.Li L., Qin L., Xu Z., Yin Y., Wang X., Kong B. Artificial intelligence distinguishes COVID-19 from community-acquired pneumonia on chest CT. Radiology. 2020 doi: 10.1148/radiol.2020200905. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Huang L., Han R., Ai T., Yu P., Kang H., Tao Q. Serial quantitative chest CT assessment of COVID-19: deep-learning approach. Radiol Cardiothorac Imaging. 2020;2:e200075. doi: 10.1148/ryct.2020200075. [DOI] [PMC free article] [PubMed] [Google Scholar]