Abstract
Objectives. To examine the association between residence in different housing typologies and all-cause and cause-specific mortality, and to compare with the 25 × 25 risk factors defined by the World Health Organization.
Methods. We used data from EPIPorto cohort (Porto, Portugal; n = 2485). We georeferenced and matched participants to a housing type—conventional, affordable, social, or substandard housing (locally called ilhas). We used Poisson regression models to estimate mortality rates and associations.
Results. Age- and sex-adjusted mortality rates (per 100 000 person-years) were 713 (95% confidence interval [CI] = 584, 863) for individuals residing in conventional housing, and 1019 (95% CI = 637, 1551), 1200 (95% CI = 916, 1551), and 1239 (95% CI = 839, 1772) for individuals residing in affordable housing, social housing, and ilhas, respectively. After further adjustment, the associations between mortality and residence in social housing (rate ratio [RR] = 1.59; 95% CI = 1.22, 2.06) and in ilhas (RR = 1.64; 95% CI = 1.12, 2.33) remained. The association between disadvantaged housing and mortality was stronger than that observed for well-established risk factors such as hypertension, sedentariness, heavy drinking, manual occupation, or obesity.
Conclusions. Disadvantaged housing is a major risk factor for mortality that should be accounted for by health policies and surveillance systems.
Housing is a human right, a key social determinant of health, and a pivotal mechanism of the relationship between poverty and health.1 Poor housing can affect health through material and psychosocial pathways and lead to an array of health conditions, including respiratory infections, asthma, injuries, and mental illness.2–6 The material pathway refers to the physical conditions of the home (e.g., need for repair) and residents’ exposure to physical (e.g., extreme temperatures), biological (e.g., presence of mold), and chemical (e.g., lead) hazards, which all have well-documented health consequences.5 On the other hand, the psychosocial pathway refers to the “symbolic meaning of the home”; the home plays an important role as a place of refuge in our society and is an important source of identity and social relationships, and a source of stigma or prestige, so that living in poor housing may lead to low expectations, dissatisfaction, and stress, which affect both physical and mental health.1,5,7
Improvements in housing conditions were targeted by the urban salubrity reforms in the 19th century. Despite the current interest in the social determinants of health, there has been little research on the topic, particularly in Europe.3,7–9 Nevertheless, recent reports revealed that a large share of the population has difficulties in accessing affordable housing, and more than 15% of Europeans still live in poor-quality and overcrowded homes.10 While housing conditions in Portugal have significantly improved in the past decade, problems such as overcrowding and poor thermal comfort persist.11,12 In addition, since 2015, Porto and Lisbon, Portugal, like many other European cities, have been facing an unprecedented housing crisis characterized by increasing property values, rising rents, increasing levels of homelessness, and a lack of public investment.13 Thus, availability and affordability of decent housing has emerged again as an important societal concern.
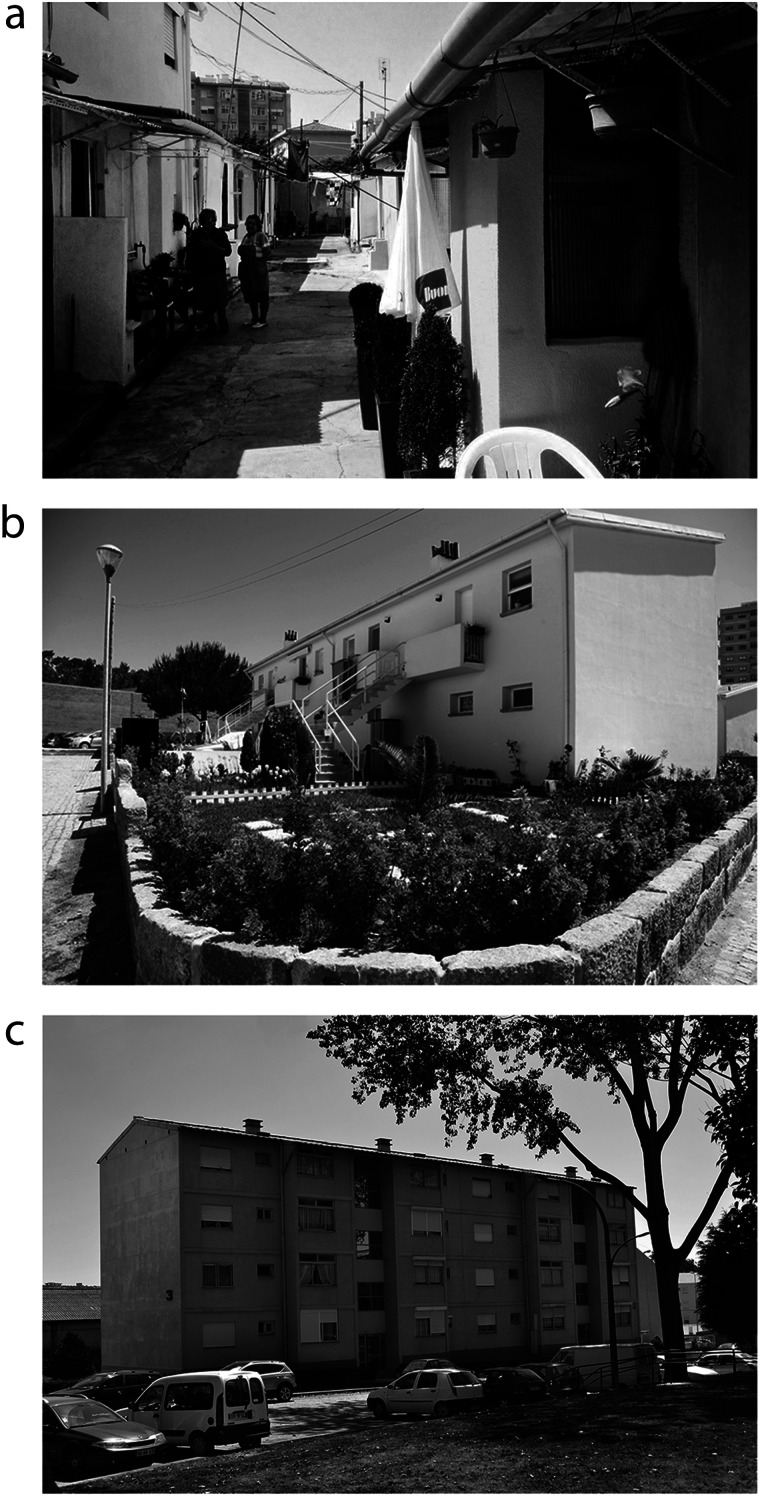
In most cities, diverse housing types coexist, reflecting the evolution of the housing policies as well as secular demographic and social changes. Despite their relatively small size, Portuguese cities, particularly Porto and Lisbon, hold a great diversity of housing types: conventional nonsubsidized housing, substandard housing (locally called ilhas), and subsidized forms of housing such as affordable and social housing, which are all depicted in the photographs from Figure 1.
FIGURE 1—
Photographs Depicting Each of the Studied Housing Types: (a) Ilha, (b) Affordable Housing, and (c) Social Housing: Porto, Portugal, 2019
Note. Ilha is the local word for substandard housing.
Source. Porto City Council; figures are copyright-free.
Ilhas (which translates to “islands”) were illegal constructions that emerged in the late 19th century in Porto and the Porto metropolitan area when industrialization and massive rural exodus started.14 Ilhas consisted of rows of 10 to 20 small houses, usually with a single floor (with 16 square meters of private area, on average), that grew in the backyards of the middle-class houses and that are known for their substandard living conditions.14–16 The access to the street is made through a narrow central (or side) corridor.16 This housing typology is very similar to the “back-to-back houses” built in England in the 18th century.17 Although some ilhas have been demolished or upgraded in the recent past years, they are still part of the urban fabric.15
Because the neighborhoods where these houses were built were the focus of epidemics in the 19th and 20th centuries, such as tuberculosis, plague, and cholera, the governments began to invest in subsidized forms of housing. However, despite previous sporadic initiatives, it was only after 1935, within Salazar’s political regime, that the provision of public housing was launched: first the affordable houses program (casas económicas) and later the social housing program. Affordable houses were single-family houses that were commonly distributed to lower-middle-class civil servants who were members of corporative trade unions.16 Workers’ unions were not free, but controlled by the state, which namely supervised union elections, in which usually ran only 1 list, sponsored by the regime. These regime unions selected the beneficiaries of the affordable houses.
From the 1950s to the 1970s, with increased industrialization and urbanization, public provision became insufficient to meet housing needs. In response, the national government along with the municipalities invested in social housing (i.e., apartment buildings based on functionalist principles [large buildings devoid of decorative elements] in the periphery of Lisbon and Porto).16
Because these housing types have different physical characteristics and spatial locations within the city, we hypothesized that the health status of individuals residing in these housing types are different from each other, even after we controlled for personal demographic and socioeconomic characteristics. While there is evidence on the health effects of social housing and specific housing conditions,18–20 few studies have assessed how living in different housing types, each reflecting the housing policies of that time and embodying a particular social and political context, affects population health, and even fewer have assessed its impact on mortality.20 To fill this gap and to test our hypothesis, we relied on georeferenced data of a population-based adult cohort from Porto to examine the association between residence in different housing typologies and all-cause and cause-specific mortality. In addition, under the hypothesis that housing is a major health determinant, we also aimed to compare the strength of association between disadvantaged housing and mortality with that of the 25 × 25 risk factors defined by the World Health Organization. The 25 × 25 risk factors include major risk factors that should be improved to reduce premature mortality from noncommunicable diseases by 25% by 2025.21
METHODS
The Porto municipality is located in the northwest of continental Portugal and comprised approximately 238 000 inhabitants according to the most recent census (2011), distributed across 41.7 square kilometers of land. Porto is limited by the Atlantic coast and extends along the Douro River estuary. It is an industrial and port town within the Porto metropolitan area, the second largest metropolitan area of Portugal, with roughly 1.3 million inhabitants.22
Participants
We used data from EPIPorto, a prospective adult closed cohort study from Porto. Being a closed cohort, this sample gains no new participants and is expected to be followed until death. The EPIPorto study started in 1999 and recruited adult community dwellers in the city of Porto by random digit dialing with households as the sampling frame. Once a household was selected, all residents were identified by age and sex, and 1 resident (aged ≥ 18 years) was randomly selected as the respondent, without allowing for replacement in case of refusal. The response rate was 70%, resulting in a total of 2485 participants.23 The EPIPorto cohort is still ongoing and, since recruitment, there have been 3 additional waves (in 2005–2008, 2013–2015, and 2017–2018) and specific surveys on subsamples. At each evaluation, a structured questionnaire to assess participants’ sociodemographic, behavioral, and clinical characteristics is administered by trained professionals during face-to-face interviews.
Housing Typologies and Address Geocoding
The EPIPorto questionnaire has no question on the type of housing because asking participants to label the housing type in which they reside could be a sensitive question, as living in ilhas and social housing is associated with social stigma. Yet, we geocoded all participants based on their home address,24 which allows matching them to a housing type based on their coordinates. We obtained maps locating each housing type from Porto City Council Web site25 and from a recent housing survey.15 Then we overlaid the point location of each participant’s residence with the housing maps to match each participant to a housing type. We performed overlay operations in ArcGIS 10.5.1 (Environmental Systems Research Institute, Redlands, CA). We classified participants whose house did not intersect with any of these housing types as residents in conventional, nonsubsidized housing.
Mortality
We assessed participants’ vital status and cause and date of death through record linkage with administrative data. We classified underlying cause of death according to the International Classification of Diseases, 10th Revision (ICD-10; Geneva, Switzerland: World Health Organization; 1992), and we examined mortality from the following causes: all-cause mortality, cancer (ICD-10 C00–C97), and cardiovascular disease (I00–I99). Other causes of death include all remaining deaths. We focused on cardiovascular and cancer mortality as these were the main causes of death in our sample. We computed follow-up time as the difference between the date of death and the date of baseline evaluation.
Covariates
We adjusted estimates to baseline sociodemographic variables, namely age, sex, occupation, education, duration of residence in Porto for 20 years or more (yes or no), marital status (married or cohabiting, or living alone), and to 6 out of 7 of the 25 × 25 risk factors21—current smoking, heavy drinking, physical inactivity, obesity, hypertension, and diabetes (we omitted salt intake because of data unavailability).
We grouped educational attainment into the following classes: (1) primary and lower secondary school (7 to 9 years after kindergarten, from here onward referred to as “low”); (2) higher secondary school (around 4 to 5 years more, high-school diploma level, “medium”); and (3) tertiary education (any degree after high school, “high”). We grouped occupation class into 3 classes—manual workers, nonmanual workers, and others (e.g., retired, housewives, students)—used previously to estimate socioeconomic inequalities in mortality.26,27
We categorized self-reported smoking into current, former, and never smoker. We measured alcohol consumption in alcohol units per week; we categorized participants as abstainers (0 units/week), moderate drinkers (1–21 units/week for men; 1–14 for women), and heavy drinkers (> 21 units/week for men; > 14 for women).
We expressed physical activity as a dichotomous variable indicating whether the person led an active (any moderate or vigorous physical activity weekly) or sedentary lifestyle (none). We calculated body mass index as weight in kilograms divided by the square of height in meters (kg/m2) and categorized it as underweight or normal (< 25 kg/m2), overweight (25 to < 30 kg/m2), or obese (≥ 30 kg/m2). We defined hypertension as the presence of at least 1 of the following conditions: systolic blood pressure greater than or equal to 140 millimeters of mercury, diastolic blood pressure greater than or equal to 90 millimeters of mercury, current intake of antihypertensive medication, or self-reported hypertension. We defined diabetes as the presence of at least 1 of the following conditions: fasting glucose greater than or equal to 7 millimoles per liter or self-reported diabetes. These variable categorization schemes have been employed elsewhere.26,28,29
Statistical Analysis
For the descriptive analysis, we calculated the median and interquartile range for continuous variables and counts and proportions for categorical ones. For group comparisons, we used χ2 test (or Fisher exact test) and analysis of variance for categorical and continuous variables, respectively. We adopted a significance level of P less than .05 for these analyses.
We used Poisson regression models to estimate the age- and sex-adjusted mortality rates and the associations between housing typologies and mortality because, for large samples, low incidence, and relatively short follow-up, Poisson regression yields similar results to the Cox proportional hazard model.30 We also formally evaluated the adequacy of Poisson models by using the deviance goodness-of-fit test, which revealed good fit (P = 1.00), and by investigating the presence of multicollinearity and overdispersion.
To account for time at risk, we used the log of the person-years as an offset. To remove the influence of unequal sex and age distribution, we included sex and age (centered at the mean of all individuals) in all the models. We subsequently adjusted the models for individual-level socioeconomic characteristics (i.e., education, occupation, marital status, residence in Porto for 20 years or more), hypothesized as confounders of the studied associations. We then adjusted models for the previously mentioned 25 × 25 risk factors to test if, after accounting for these well-known risk factors, differences in mortality across housing typologies remained. We fitted these 3 sequential models for all-cause mortality, cardiovascular mortality, and cancer mortality.
Furthermore, we compared the strength of the association between housing type and all-cause mortality with the strength of the association observed for each of the 25 × 25 risk factors (plus occupation and education) using (1) minimally adjusted models (which included housing type as the explanatory variable, and sex and age as covariates, with mortality as the outcome) and (2) mutually adjusted models (which included housing type as the explanatory variable, and sex, age, occupation, education, and the 25 × 25 risk factors as covariates, with mortality as the outcome). A similar approach was used before.18,19
We present results as age- and sex-adjusted mortality rates and rate ratios (RRs) and corresponding 95% confidence intervals (95% CIs). We used residence in conventional, nonsubsidized housing as reference category. We performed statistical analysis with R software (R Foundation, Vienna, Austria).
RESULTS
This study included 2485 participants (61.9% women; mean age = 52.9 years), of whom 4.3%, 15.9%, and 4.8% resided in affordable housing, social housing, and ilhas, respectively. Over a mean of 16.3 years of follow-up, there were 413 deaths.
Table 1 shows the participants’ characteristics according to the housing typology. Individuals residing in affordable housing, social housing, and ilhas were more likely to have low levels of education and to be employed in manual occupations, particularly those residing in social housing and in ilhas. Regarding the 25 × 25 risk factors, individuals residing in social housing and in ilhas were also more likely to be heavy drinkers, obese, and sedentary. Hypertension was also more common among individuals residing in social housing and ilhas. Only 14.6% of the residents in conventional housing died during the follow-up period, versus 21.7%, 21.3%, and 28.3% among those residing in affordable housing, social housing, and ilhas, respectively.
TABLE 1—
Participants’ Characteristics According to Housing Typology: EPIPorto Cohort Study, Porto, Portugal, 1999–2019
| Variable | Conventional Housing, No. (%) or Mean ±SD | Affordable Housing, No. (%) or Mean ±SD | Social Housing, No. (%) or Mean ±SD | Ilhas, No. (%) or Mean ±SD | P |
| No. | 1863 (75.1) | 106 (4.3) | 394 (15.9) | 120 (4.8) | |
| Female gender | 1137 (61.0) | 75 (70.8) | 253 (64.2) | 73 (60.8) | .17 |
| Age, y | 52.2 ±15.6 | 56.0 ±15.5 | 54.3 ±14.9 | 57.3 ±14.2 | < .001 |
| Married or similar marital status | 1253 (67.3) | 76 (71.7) | 266 (67.5) | 85 (70.8) | .69 |
| Educational attainment | |||||
| Low | 967 (51.9) | 79 (74.5) | 355 (90.1) | 113 (94.2) | < .001 |
| Medium | 277 (14.9) | 10 (9.4) | 28 (7.1) | 5 (4.2) | |
| High | 619 (33.2) | 17 (16.0) | 11 (2.8) | 2 (2.7) | |
| Occupation | |||||
| Manual | 201 (10.8) | 15 (14.3) | 130 (33.0) | 35 (29.2) | < .001 |
| Nonmanual | 829 (44.5) | 33 (31.4) | 46 (11.7) | 16 (13.3) | |
| Other (retired, housewives, unemployed) | 832 (44.7) | 57 (54.3) | 218 (55.3) | 69 (57.5) | |
| Residence in Porto ≥ 20 y | 1512 (81.2) | 86 (81.1) | 315 (79.9) | 91 (75.8) | .53 |
| Alcohol intake | |||||
| Abstainer | 635 (34.9) | 42 (41.2) | 115 (30.5) | 37 (32.7) | < .001 |
| Low | 846 (46.6) | 42 (41.2) | 164 (43.5) | 42 (37.2) | |
| High | 336 (18.5) | 18 (17.6) | 98 (26.0) | 18 (30.1) | |
| Smoking | |||||
| Never smokers | 995 (54.4) | 69 (67.6) | 232 (61.5) | 67 (59.3) | .020 |
| Former smokers | 399 (21.8) | 14 (13.7) | 59 (15.7) | 21 (18.6) | |
| Current smokers | 434 (23.7) | 19 (18.6) | 86 (22.8) | 25 (22.1) | |
| Body mass indexa | |||||
| Underweight or normal | 745 (40.8) | 33 (31.4) | 97 (25.0) | 33 (27.7) | < .001 |
| Overweight | 729 (39.9) | 46 (43.8) | 162 (41.8) | 51 (42.9) | |
| Obese | 351 (19.2) | 26 (24.8) | 129 (33.2) | 35 (29.4) | |
| Physical inactivity | 1354 (74.0) | 83 (81.4) | 324 (85.7) | 95 (84.1) | <. 001 |
| Hypertension | 889 (47.8) | 53 (50.0) | 230 (58.7) | 69 (57.5) | <. 001 |
| Diabetes | 225 (12.1) | 10 (9.2) | 59 (15.0) | 19 (15.8) | .21 |
| Deaths | 272 (14.6) | 23 (21.7) | 84 (21.3) | 34 (28.3) | < .001 |
| Cardiovascular disease | 68 (25.0)b | 5 (21.7) | 21 (25.0) | 13 (38.2) | < .001 |
| Cancer | 64 (23.5) | 6 (26.0) | 19 (22.6) | 9 (26.4) | .06 |
| Other causes of death | 140 (51.5) | 12 (52.2) | 44 (52.4) | 12 (35.3) | .06 |
| Premature deaths (before aged 70 y) | 58 (21.3) | 3 (13.0) | 14 (16.7) | 9 (26.5) | .12 |
| Years follow-up | 16.6 ±4.1 | 15.9 ±4.7 | 15.5 ±4.3 | 15.5 ±4.3 | < .001 |
Note. Ilha is the local word for substandard housing. The sample size was n = 2485.
Weight in kilograms divided by the square of height in meters (kg/m2): underweight or normal (< 25 kg/m2), overweight (25 to < 30 kg/m2), or obese (≥ 30 kg/m2).
Percentage in relation to the number of deaths in each housing typology.
We observed differences in the causes of deaths according to housing typology—cardiovascular disease mortality was significantly more frequent among residents from ilhas, accounting for 38.2% of the deaths (vs 25.0% in conventional housing, 21.7% in affordable housing, and 25.0% in social housing). Premature deaths (before the age of 70 years) also seemed more frequent in individuals residing in ilhas, where 26.5% of the deceased participants died prematurely.
The age- and sex-adjusted mortality rate (per 100 000 person-years) was 713 (95% CI = 584, 863) for individuals residing in conventional housing types, and 1019 (95% CI = 637, 1551), 1200 (95% CI = 916, 1551), and 1239 (95% CI = 839, 1772) in individuals residing in affordable housing, social housing, and ilhas, respectively. Minimally adjusted models, shown in Table 2, revealed a significant association between residence in social housing (RR = 1.68; 95% CI = 1.30, 2.15) and in ilhas (RR = 1.74; 95% CI = 1.19, 2.45) and all-cause mortality. On the other hand, all-cause mortality was unrelated with residence in affordable housing. After adjustment for social and economic factors, associations between all-cause mortality and residence in social housing (RR = 1.59; 95% CI = 1.22, 2.06) and in ilhas (RR = 1.64; 95% CI = 1.12, 2.33) remained. Adjustment for 25 × 25 risk factors further reduced the magnitude of the associations, but the association between all-cause mortality and residence in social housing persisted (RR = 1.52; 95% CI = 1.14, 1.99).
TABLE 2—
Associations Between All-Cause and Cause-Specific Mortality and Housing Typology: EPIPorto Cohort Study, Porto, Portugal, 1999–2019
| Model 1, RR (95% CI) | Model 2, RR (95% CI) | Model 3, RR (95% CI) | |
| All-cause mortality | |||
| Conventional housing (Ref) | 1 | 1 | 1 |
| Affordable housing | 1.43 (0.91, 2.14) | 1.37 (0.86, 2.08) | 1.38 (0.83, 2.16) |
| Social housing | 1.68 (1.30, 2.15) | 1.59 (1.22, 2.06) | 1.52 (1.14, 1.99) |
| Ilhas | 1.74 (1.19, 2.45) | 1.64 (1.12, 2.33) | 1.45 (0.96, 2.12) |
| Cardiovascular mortality | |||
| Conventional housing (Ref) | 1 | 1 | 1 |
| Affordable housing | 1.14 (0.40, 2.55) | 0.94 (0.29, 2.28) | 0.83 (0.20, 2.29) |
| Social housing | 1.64 (0.98, 2.64) | 1.64 (0.96, 2.70) | 1.29 (0.69, 2.28) |
| Ilhas | 2.46 (1.30, 4.30) | 2.48 (1.29, 4.43) | 2.36 (1.18, 4.35) |
| Cancer mortality | |||
| Conventional housing (Ref) | 1 | 1 | 1 |
| Affordable housing | 1.64 (0.63, 3.50) | 1.63 (0.63, 3.49) | 1.87 (0.72, 4.03) |
| Social housing | 1.55 (0.90, 2.53) | 1.51 (0.86, 2.54) | 1.53 (0.86, 2.62) |
| Ilhas | 1.95 (0.90, 3.73) | 1.86 (0.85, 3.62) | 1.63 (0.71, 3.30) |
Note. CI = confidence interval; RR = rate ratio. Ilha is the local word for substandard housing. The sample size was n = 2485. Model 1 = adjusted for sex and age. Model 2 = additionally adjusted for residence in Porto for 20 years or more, education, occupation, and marital status. Model 3 = additionally adjusted for 25 × 25 risk factors (current smoking, harmful use of alcohol, insufficient physical activity, obesity, hypertension, and diabetes).
Table 2 also shows the results for the associations between housing type and cause-specific mortality. Although our estimates were based on observations with a wide variance, we observed that residents in substandard and subsidized housing types tended to have a higher risk of cardiovascular and cancer mortality. Particularly strong associations were found for residents in ilhas, who showed a 2.4 times higher risk of dying of cardiovascular disease as compared with those living in conventional housing, even after successive adjustments (RR = 2.36; 95% CI = 1.18, 4.35).
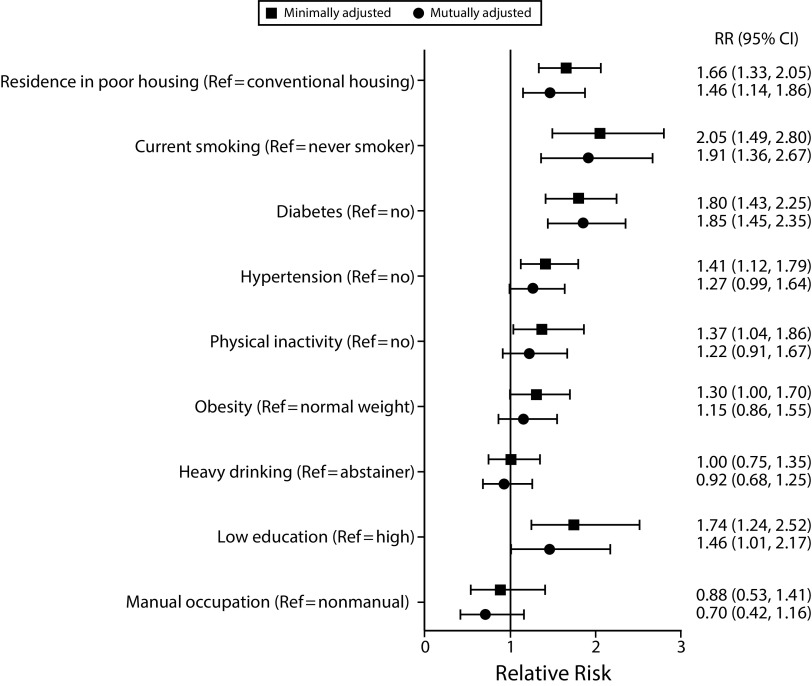
Figure 2 shows the mortality risk associated with the 25 × 25 risk factors, socioeconomic factors such as education and occupation, and housing type (here grouping residence in ilhas or social housing, compared with conventional, nonsubsidized housing). As evidenced in the plot, we observed greater increases in mortality for current smoking, diabetes, low education, and residence in poor housing—the strength of the association between residence in poor housing and mortality was very similar to that of low education and greater than the strength of the association of physical inactivity, hypertension, obesity, occupation, and heavy drinking. We observed similar trends in the mutually adjusted models, in which residence in disadvantaged housing ranked in third place in terms of mortality, right after current smoking and diabetes.
FIGURE 2—
Associations Between All-Cause Mortality, Housing Typology, and 25 × 25 Risk Factors: EPIPorto Cohort Study, Porto, Portugal, 1999–2019
Note. CI = confidence interval; RR = rate ratio. The sample size was n = 2485. Minimally adjusted models included housing type as the explanatory variable, and sex and age as covariates, with mortality as outcome; mutually adjusted models included housing type as the explanatory variable, and sex, age, occupation, education, and the 25 × 25 risk factors as covariates, with mortality as outcome.
DISCUSSION
In this study, we found that residence in substandard housing (locally called ilhas) and in social housing was associated with worse health, as measured by mortality. This association remained even after we accounted for individuals’ occupation class and education level, meaning that individuals with the exact same age, sex, education, and occupation have different mortality risks according to the type of house they occupy. In addition, we found that the association between mortality and residence in disadvantaged housing types was comparable and even stronger than the associations observed for conventional risk factors, such as low education, hypertension, physical inactivity, heavy drinking, manual occupation, and obesity.
Because this housing type can only be found in Portugal, no other contemporaneous study has been published, to our knowledge, on the health effects of residing in ilhas. Yet, historical reports have documented that the levels of mortality in ilhas, especially infant mortality, were extremely high, and that the 19th- and 20th-century epidemics were concentrated in these parts of the city.25 Furthermore, a previous ecological study about the distribution of old-age survival in Porto highlighted that the neighborhoods of significantly lower survival coincided with the locations of social housing and of ilhas.22 Analysis according to cause of death revealed that residence in ilhas was particularly detrimental to cardiovascular health, as people living in this housing type showed a 2.4 times higher risk of dying of cardiovascular disease compared with people living in conventional housing. The pathways beyond this association should be further investigated—namely stress, violence, and multiple psychosocial factors—because the traditional cardiovascular risk factors that we accounted for in the multivariable models do not fully explain this excess risk.
International investigations have compared the health status of individuals residing in social housing versus those in conventional housing and, similarly to us, found that the first presented worse health profiles. Although the premise behind the development of social housing was to guarantee adequate housing to unprivileged individuals, studies have shown a significant association between residing in social housing and poor health, including higher risk of obesity, hypertension, respiratory disease, and mortality.18–20 Seng et al. found that residence in public rental housing was associated with increased risk of all-cause mortality (hazard ratio = 1.57),20 which is in accordance with the RRs we obtained. Fertig and Reingold, looking at maternal health, found that residence in social housing worsens mothers’ health status and increases the probability that a mother becomes overweight.18 Likewise, and although our study was conducted in overall population, not exclusively among mothers, we observed a 75% higher prevalence of obesity among participants residing in social housing. Finally, in the United States, residence in public housing was strongly associated with asthma in a large sample of adult residents of Boston, Massachusetts.19
Limitations
Our study presents a number of limitations that need to be discussed. We do not have information about the quality of the physical environments inside the houses, such as indoor air pollution, temperature, and presence of molds, which would provide valuable information to better understand the observed associations. However, ilhas and social housing are known for their adverse environmental conditions,31 so that poor physical environment is a very plausible mediator of the observed associations.
Psychosocial stress might be another relevant mediator, as residence in typologized housing might create stigma, thereby increasing psychosocial stress, which, in turn, affects both physical and mental health. It is also important to mention that, although we examined cause-specific mortality, because of the relatively small number of deaths, we could only explore 2 major causes (cancer and cardiovascular disease), and because of reduced statistical power, our estimates have a high variance. Moreover, our findings can be partially explained by residual confounding attributable to unaccounted socioeconomic variables (e.g., tenure status, income) and unmeasured indoor and outdoor environmental factors (e.g., pollution, access to services). Nevertheless, most observed associations were strong and persisted after successive adjustments for other important risk factors.
Furthermore, despite the longitudinal study design and control for current socioeconomic conditions, we cannot fully separate what is the effect of living in disadvantaged housing from the transgenerational effects and the effect of early life health and living conditions. For instance, parental socioeconomic conditions and birth cohort have well-known health effects and can also determine housing choices and social mobility, thereby representing potentially important confounders.32,33 Finally, although Southern European countries share, to some degree, the same housing policies, our results need to be considered taking into account the specificities of other spatiotemporal contexts.
Public Health Implications
These limitations need to be weighed against the implications of these findings that could help guide housing policies even in other settings with similar demographic profiles and housing schemes. A substantial number of individuals still reside in substandard housing, such as these ilhas, and these individuals present poor health status, meaning that, despite the fact that ilhas are gradually disappearing, more vulnerable individuals, especially the oldest, still live under very unprivileged conditions and deserve special attention. Also, despite the fact that social housing programs have been developed to solve these types of societal issues, individuals residing in social housing still have significantly worse mortality levels than the population living in conventional, nonsubsidized housing, which indicates that there may exist a need to further improve the physical and social environments inside and around these housing complexes. Knowing that residing in disadvantaged housing types is as strongly associated with mortality as other major risk factors suggests that housing should be ranked a priority health determinant in local and national policies and surveillance systems, which may require a coordinated multisectoral approach of different areas of policy targeting social determinants of health.
Summing up, our study provides novel evidence that housing is a major public health issue and that it should be viewed as a priority by policymakers. We expect that this study will reignite awareness about the fundamental link between housing and health.
ACKNOWLEDGMENTS
This study was supported by the European Regional Development Fund (FEDER) through the Competitiveness and Internationalization Operational Programme and national funding from the Foundation for Science and Technology (FCT; Portuguese Ministry of Science, Technology, and Higher Education) under the Unidade de Investigação em Epidemiologia—Instituto de Saúde Pública da Universidade do Porto (EPIUnit; POCI-01-0145-FEDER-006862; Ref. UID/DTP/04750/2019). This study was also funded by the FEDER, through the Competitiveness and Internationalization Operational Programme, and by national funding from the FCT under the scope of the project PTDC/GES-AMB/30193/2017 (POCI-01-0145-FEDER-030193, 02/SAICT/2017 - 30193). This study was supported by the European Commission (Horizon 2020 grant 633666) and is also a result of the project DOCnet (NORTE-01–0145-FEDER-000003), supported by Norte Portugal Regional Operational Programme (NORTE 2020), under the PORTUGAL 2020 Partnership Agreement, through the European Regional Development Fund.
The authors gratefully acknowledge the participants enrolled in EPIPorto for their kindness, all members of the research team for their enthusiasm and perseverance, and the participating hospitals and their staff for their help and support. The authors also kindly acknowledge André Tadeu for help in classifying causes of deaths, and Raquel Lucas and José Pedro Silva for the revision of earlier versions of this article.
CONFLICTS OF INTEREST
The authors declare no conflicts of interest.
HUMAN PARTICIPANT PROTECTION
The local ethics committee approved the study. The study was carried out according to the Helsinki Declaration, and all participants completed the informed written consent form.
REFERENCES
- 1.Shaw M. Housing and public health. Ann Rev Public Health. 2004;25(1):397–418. doi: 10.1146/annurev.publhealth.25.101802.123036. [DOI] [PubMed] [Google Scholar]
- 2.Krieger J, Higgins DL. Housing and health: time again for public health action. Am J Public Health. 2002;92(5):758–768. doi: 10.2105/ajph.92.5.758. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Marsh A, Gordon D, Heslop P, Pantazis C. Housing deprivation and health: a longitudinal analysis. Housing Studies. 2000;15(3):411–428. [Google Scholar]
- 4.Marí-Dell’Olmo M, Novoa AM, Camprubí L et al. Housing policies and health inequalities. Int J Health Serv. 2016;47(2):207–232. doi: 10.1177/0020731416684292. [DOI] [PubMed] [Google Scholar]
- 5.Dunn JR. The population health approach to housing: a framework for research. Ottawa, ON: Canada Mortgage and Housing Corporation; 2002. [Google Scholar]
- 6.Hernández D, Swope CB. Housing as a platform for health and equity: evidence and future directions. Am J Public Health. 2019;109(10):1363–1366. doi: 10.2105/AJPH.2019.305210. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Howden-Chapman P. Housing standards: a glossary of housing and health. J Epidemiol Community Health. 2004;58(3):162–168. doi: 10.1136/jech.2003.011569. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Dunn JR. Housing and health inequalities: review and prospects for research. Housing Studies. 2000;15(3):341–366. [Google Scholar]
- 9.Clair A, Reeves A, Loopstra R, McKee M, Dorling D, Stuckler D. The impact of the housing crisis on self-reported health in Europe: multilevel longitudinal modelling of 27 EU countries. Eur J Public Health. 2016;26(5):788–793. doi: 10.1093/eurpub/ckw071. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Pittini A, Ghekière L, Dijol J, Kiss I. The state of housing in the EU 2015. Brussels, Belgium: Housing Europe, the European Federation for Public, Cooperative and Social Housing; 2015. [Google Scholar]
- 11.Ribeiro AI, Launay L, Guillaume E, Launoy G, Barros H. The Portuguese version of the European Deprivation Index: development and association with all-cause mortality. PLoS One. 2018;13(12):e0208320. doi: 10.1371/journal.pone.0208320. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Marques TS, Matos FL, Guerra P, Ribeiro D. Housing problems in Portugal: a challenge to define a territorialised policy in times of crisis. Paper presented at: Proceedings of the International Conference the Welfare State in Portugal in the Age of Austerity; May 9–10, 2014; Lisbon, Portugal.
- 13.Pittini A, Dijol J, Turnbull D, Whelan M. The state of housing in the EU 2019. Brussels, Belgium: Housing Europe, the European Federation of Public, Cooperative and Social Housing; 2019. [Google Scholar]
- 14.Matos F. Social housing in the urban space of Porto [in Portuguese] Anal Soc. 1994;127(3):677–695. [Google Scholar]
- 15.Breda-Vásquez I, Conceição P. Survey and characterization [in Portuguese] Porto, Portugal: Domus Social, Câmara Municipal do Porto; 2015. Islands of Porto. [Google Scholar]
- 16.Varady DP, Matos F. Comparing public housing revitalization in a liberal and a Mediterranean society (US vs. Portugal) Cities. 2017;64:37–46. [Google Scholar]
- 17.Harrison J. The origin, development and decline of back-to-back houses in Leeds, 1787–1937. Ind Archaeol Rev. 2017;39(2):101–116. [Google Scholar]
- 18.Fertig AR, Reingold DA. Public housing, health and health behaviors: is there a connection? J Policy Anal Manage. 2007;26(4):831–859. doi: 10.1002/pam.20288. [DOI] [PubMed] [Google Scholar]
- 19.Mehta AJ, Dooley DP, Kane J, Reid M, Shah SN. Subsidized housing and adult asthma in Boston, 2010–2015. Am J Public Health. 2018;108(8):1059–1065. doi: 10.2105/AJPH.2018.304468. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Seng JJB, Kwan YH, Goh H, Thumboo J, Low LL. Public rental housing and its association with mortality—a retrospective, cohort study. BMC Public Health. 2018;18(1):665. doi: 10.1186/s12889-018-5583-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Global action plan for the prevention and control of noncommunicable diseases 2013–2020. Geneva, Switzerland: World Health Organization; 2013. [Google Scholar]
- 22.Ribeiro AI, Krainski ET, Autran R, Teixeira H, Carvalho MS, de Pina MF. The influence of socioeconomic, biogeophysical and built environment on old-age survival in a Southern European city. Health Place. 2016;41:100–109. doi: 10.1016/j.healthplace.2016.08.008. [DOI] [PubMed] [Google Scholar]
- 23.Santos AC, Barros H. Prevalence and determinants of obesity in an urban sample of Portuguese adults. Public Health. 2003;117(6):430–437. doi: 10.1016/S0033-3506(03)00139-2. [DOI] [PubMed] [Google Scholar]
- 24.Ribeiro AI, Olhero A, Teixeira H, Magalhães A, Pina MF. Tools for address georeferencing—limitations and opportunities every public health professional should be aware of. PLoS One. 2014;9(12):e114130. doi: 10.1371/journal.pone.0114130. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Domus Social. Bairros. 2019. Available at: http://www.domussocial.pt/habitacoes/c/bairros. Accessed October 15, 2019.
- 26.Stringhini S, Carmeli C, Jokela M et al. Socioeconomic status and the 25 × 25 risk factors as determinants of premature mortality: a multicohort study and meta-analysis of 1.7 million men and women. Lancet. 2017;389(10075):1229–1237. doi: 10.1016/S0140-6736(16)32380-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.d’Errico A, Ricceri F, Stringhini S et al. Socioeconomic indicators in epidemiologic research: a practical example from the LIFEPATH study. PLoS One. 2017;12(5):e0178071. doi: 10.1371/journal.pone.0178071. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Stringhini S, Carmeli C, Jokela M et al. Socioeconomic status, non-communicable disease risk factors, and walking speed in older adults: multi-cohort population based study. BMJ. 2018;360:k1046. doi: 10.1136/bmj.k1046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Ribeiro AI, Fraga S, Kelly-Irving M et al. Neighbourhood socioeconomic deprivation and allostatic load: a multi-cohort study. Sci Rep. 2019;9(1):8790. doi: 10.1038/s41598-019-45432-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Callas PW, Pastides H, Hosmer DW. Empirical comparisons of proportional hazards, Poisson, and logistic regression modeling of occupational cohort data. Am J Ind Med. 1998;33(1):33–47. doi: 10.1002/(sici)1097-0274(199801)33:1<33::aid-ajim5>3.0.co;2-x. [DOI] [PubMed] [Google Scholar]
- 31.Soares S, Brochado S, Ramos N et al. Health and living conditions in social housing: comparison between rehabilitated and non-rehabilitated neighbourhoods. J Public Health. 2016;24(6):535–544. [Google Scholar]
- 32.Fu Q. The persistence of power despite the changing meaning of homeownership: an age-period-cohort analysis of urban housing tenure in China, 1989–2011. Urban Stud. 2015;53(6):1225–1243. [Google Scholar]
- 33.Zhu Y. Spatiality of China’s market-oriented urbanism: the unequal right of rural migrants to city space. Territ Politic Gov. 2014;2(2):194–217. [Google Scholar]