Abstract
Objectives. To measure trends before, during, and after implementation of Georgia House Bill 954, a limit on abortion at 22 or more weeks of gestation passed in 2012, in total abortions and abortions by gestational age and state residence.
Methods. We analyzed aggregate year-level induced termination of pregnancy data from the Georgia Department of Public Health from 2007 to 2017. We used linear regression to describe annual trends in the number of abortions and χ2 analyses to describe changes in proportions of abortions by gestational age (< 20 weeks, 20–21 weeks, and > 21 weeks) across policy implementation periods (before, partial, and full implementation) for Georgia residents and nonresidents.
Results. Although the total number of abortions and abortions at 21 weeks or less remained stable from 2007 to 2017, the number of abortions at more than 21 weeks declined (P = .02). The decline in number of abortions at more than 21 weeks was steeper for nonresidents (31/year; Β = −31.3; P = .02) compared with Georgia residents (14/year; Β = −13.9; P = .06).
Conclusions. Findings suggest that implementation of Georgia’s 22-week gestational age limit has effectively limited access to needed abortion services in Georgia and beyond.
Access to abortion is declining in the United States, whereas trends in implementation of policies restricting delivery of abortion services have risen sharply over the past decade.1–7 State-level regulations that limit abortion after specific gestational ages have been among the common types of legislation passed.8 In 2012, the Georgia Assembly passed House Bill 954 (HB954), which prohibits abortions at 22 weeks or more from last menstrual period (LMP), or 20 weeks or more postfertilization. The bill includes exceptions for abortions provided for medically futile pregnancies, to “avert the death … or serious risk of substantial and irreversible physical impairment of the pregnant woman,” or to “preserve the life of an unborn child.”9 The bill was incrementally implemented, with partial implementation on January 1, 2013, following a temporary injunction that effectively changed the gestational age limit to 24 weeks from LMP, and full implementation in October 2015 that reduced the limit to 22 weeks from LMP.
Prior to this policy change, abortion was legal in Georgia up to 26 weeks from LMP, representing the highest gestational limit of abortion services in the Southeast,10 and positioning Georgia as a unique point of access to abortion services for people in the region.10 In 2009, 8 Southeastern states provided data on abortions at later gestational ages, (i.e., Alabama, Arkansas, Georgia, Kentucky, Louisiana, South Carolina, Virginia, and West Virginia); 81% of abortions after 21 weeks of gestation from this region occurred in Georgia.11 Roberts et al.’s initial evaluation of HB954 during the injunction period revealed that half of the people receiving abortions 20 weeks or more from LMP in Georgia came from other states.10 The Turnaway Study, which surveyed and interviewed patients denied an abortion because of a 20-week gestational limit and compared them with “near-limit” patients who received abortions just under 20 weeks of gestation, found that patients seeking abortion after 20 weeks are more likely to be younger and unemployed.12 Moreover, the Turnaway Study demonstrated that most patients seeking abortion after 20 weeks have faced numerous obstacles to earlier abortion care, including travel and procedure costs, conflict with male partners, and raising children without sufficient child care support. Such obstacles are intensified as pregnancy continues given the lack of abortion providers offering services at later gestations, increasing travel distances, and higher cost. Another group of patients who seek abortion after 20 weeks are those diagnosed with severe fetal anomalies, most of whom choose to terminate their pregnancies; denying abortion services for those patients carries important and harmful implications for maternal–infant morbidity and mortality.13 In contexts in which laws do not protect and even restrict access to safe abortion, people are forced to terminate their pregnancies with unsafe, clandestine,14 or self-induction15 methods or carry unplanned pregnancies to term. Unsafe abortion increases the likelihood of complications such as maternal morbidity and mortality—risks that are greatest for medically complicated pregnancies at later gestational ages.14
Given the persistently high rates of unintended pregnancy16 and maternal mortality17 across the Southeast, Georgia’s gestational age limit has important implications for increasing unintended births and adverse maternal–infant outcomes and negatively affecting the long-term health and social well-being of people in Georgia and beyond. The consequences of reduced access to needed abortion services may be especially dire for socially disadvantaged people, as those receiving abortions at 20 weeks or more from LMP are often low income, less educated, of minority status, and single.10 Restrictive policies that increase barriers to abortion care—including time away from work, child care arrangements, transportation and accommodations, and cost of meals18–21—disproportionately affect socially disadvantaged people, potentially exacerbating economic disadvantage and poor health status. For instance, in the Turnaway Study, women forced to carry unwanted pregnancies had 4 times greater odds of living below the federal poverty level.22 Additionally, women denied abortions in the Turnaway Study experienced health consequences, including elevated levels of short-term anxiety, compared with women receiving a wanted abortion.23
Although the broad, negative implications of policies that restrict access to abortion services may be clear, gestational age limit laws have not been well studied to date. We sought to describe trends in abortion by gestational age and state of residence before, during, and after implementation of HB954.
METHODS
Our descriptive study employed χ2 and linear regression to estimate differences in number and proportion of annual abortions provided in Georgia from 2007 to 2017, overall and stratified by gestational age, state of residence, and policy exposure period.
Data
We obtained annual, cross-sectional data on abortions provided in Georgia from 2007 to 2017 from the Georgia Department of Public Health’s (GDPH’s) state-mandated reporting of Induced Termination of Pregnancy (ITOP) certificates.24 According to the GDPH guidelines, each ITOP—the “purposeful interruption of pregnancy with the intention other than to produce a live-born infant or to remove a dead fetus and which does not result in a live birth”25—must be reported to the Georgia Office of Vital Statistics by the institution or clinic within 10 days.26 We aggregated data by year and stratified by gestational age at abortion (by LMP) and state residence status.
Measures
Our outcome measure was the annual number of abortions provided in Georgia. Additional stratification measures included gestational age at abortion, year of abortion (as a proxy for exposure to HB954), and residence status. We categorized gestational age at abortion as less than 20 weeks from LMP, 20 to 21 weeks from LMP, and more than 21 weeks from LMP. We used 3 categories to define exposure to HB954: whether the abortion occurred prior to implementation of HB954 (2007–2012), during partial implementation (2013–2015), or during full implementation (2016 and 2017). State residence status was a dichotomous indicator of whether the patient was a resident of Georgia or another state (i.e., nonresident).
Analyses
We modeled separate linear regressions to estimate annual trends in the number of abortions from 2007 to 2017 provided at different gestational ages—less than 20 weeks from LMP, 20 to 21 weeks from LMP, and more than 21 weeks from LMP—overall and among Georgia residents and nonresidents. Additionally, we used χ2 analyses to compare the proportion of abortions occurring at less than 20 weeks from LMP, 20 to 21 weeks from LMP, and more than 21 weeks from LMP during the 3 policy exposure periods, overall and among residents and nonresidents. We calculated proportions for each group by dividing the number of abortions in each gestational age category during each exposure period by the total number of abortions during each exposure period. For example, to calculate the proportion of abortions at more than 21 weeks from LMP in the pre-policy period among Georgia residents, we divided the number of abortions at more than 21 weeks from LMP among Georgia residents between 2007 and 2012 by the total number of abortions among Georgia residents between 2007 and 2012.
RESULTS
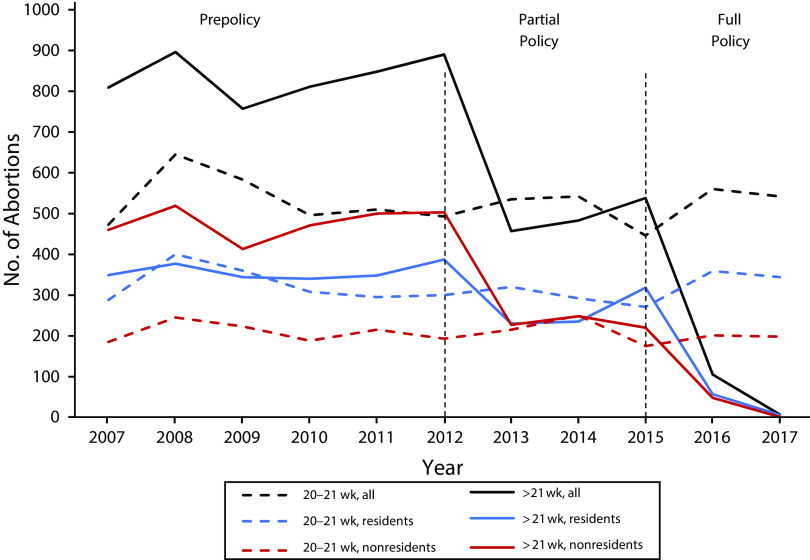
In Georgia, there were 360 972 abortions from 2007 to 2017. The total number of abortions per year (2007 = 33 535; 2017 = 32 234; P = .08), those provided at less than 20 weeks from LMP (2007 = 32 353; 2017 = 31 685; P = .21), and those provided at 20 to 21 weeks from LMP (2007 = 473; 2017 = 542; P = .54) remained relatively stable over the study period (data not shown). However, the number of abortions provided at more than 21 weeks from LMP declined sharply from 2007 to 2017 (2007 = 809; 2017 = 7; P = .02), with the largest declines observed between 2012 and 2013 (from 890 to 457), when the policy was partially implemented, and between 2015 and 2016 (from 538 to 105), when the policy went into full effect (Figure 1). Additionally, nonresidents had more abortions at more than 21 weeks from LMP prior to HB954 and subsequently experienced larger declines in abortions at more than 21 weeks over the study period. From 2007 to 2017, the number of abortions provided at more than 21 weeks from LMP to nonresidents declined by approximately 31 abortions per year (Β = −31.3; P = .02), whereas the number provided to Georgia residents declined by approximately 14 abortions per year (Β = −13.9; P = .06; Figure 1). For both residents and nonresidents, the number of abortions provided at 20 to 21 weeks from LMP remained relatively stable. Trends were similar when we examined changes in the percentages of abortions provided at 20 to 21 weeks from LMP or more than 21 weeks from LMP: whereas the proportion of abortions provided at 20 to 21 weeks remained relatively stable over time among both groups, the proportion of abortions provided at more than 21 weeks declined most discernibly among nonresidents over the study period (Figure A, available as a supplement to the online version of this article at http://www.ajph.org).
FIGURE 1—
Number of Abortions at 20 Weeks or More Provided in Georgia, by Gestational Age and Residence: 2007–2017
In χ2 analyses, the proportion of abortions provided at less than 20 weeks from LMP increased from 97.73% in the pre-policy period to 97.93% in the partial and 98.66% in the full implementation periods among Georgia residents, whereas the proportion of abortions provided at more than 21 weeks from LMP decreased from 1.19% in the pre-policy period to 0.97% in the partial and 0.11% in the full implementation periods (Table 1). Among nonresidents, the proportion of abortions provided at less than 20 weeks from LMP increased from 81.09% in the pre-policy period to 88.49% in the partial and 95.20% in the full implementation periods. The proportion of abortions at more than 21 weeks from LMP declined from 13.17% in the pre-policy period to 5.99% in the partial and 0.53% in the full implementation periods for nonresidents (Table 1).
TABLE 1—
Number and Percentage of Abortions Provided in Georgia, Stratified by Gestational Age, Policy Period, and State Residence Status: 2007–2017
| Residents (n = 318 277) |
Nonresidents (n = 42 695) |
|||||||
| Gestational Age at Termination | Pre-policy (n = 180 720), No. (%) | Partial Policy (n = 80 553), No. (%) | Full Policy (n = 57 004), No. (%) | χ2; P | Pre-policy (n = 21 765), No. (%) | Partial Policy (n = 11 602), No. (%) | Full Policy (n = 9328), No. (%) | χ2; P |
| < 20 wk | 176 624 (97.73) | 78 887 (97.93) | 56 238 (98.66) | 17 650 (81.09) | 10 267 (88.49) | 8 880 (95.20) | ||
| 20–21 wk | 1 951 (1.08) | 883 (1.10) | 703 (1.23) | 548.7; < .001 | 1 249 (5.74) | 640 (5.52) | 399 (4.28) | 1 536.1; < .001 |
| > 21 wk | 2 145 (1.19) | 783 (0.97) | 63 (0.11) | 2 866 (13.17) | 695 (5.99) | 49 (0.53) | ||
DISCUSSION
We found that Georgia’s 22-week gestational age limit appears to have had the intended effect of decreasing abortions at later gestational ages in Georgia after implementation of the policy. The number of abortions at less than 21 weeks from LMP remained stable, and there was a marked decrease in abortions in Georgia at more than 21 weeks from LMP following both the partial and full implementations of HB954. General declining trends in abortion in the United States during this study period and beyond have been recently reported elsewhere.27 Related to Georgia’s specific policy environment, although the impact of gestational age restriction policies has been underresearched, our findings are consistent with and serve to advance Roberts and colleagues’ early evaluation of HB95410 showing a decline in abortions after 20 weeks in Georgia in the first 2 years of the policy’s partial implementation (i.e., 2012–2013). Our study builds upon this prior work by extending the policy observation period to include the injunction period (January 2013 to October 2015), which effectively changed the gestational age limit to 24 weeks from LMP, and the period thereafter, when the 22-week gestational age limit was instated, to estimate a fuller effect of the law. Stable trends in abortions between 20 and 21 weeks potentially suggest that the nonmedical language of the bill—that “20 weeks’ post-fertilization” as utilized in practice equates to 22 weeks from LMP—may not have affected service delivery. However, these data only include patients who received abortions and do not capture those who were not referred, possibly because of a misunderstanding of the policy.
The broader abortion literature has documented numerous barriers to accessing care prior to gestational age limits, including financial constraints; logistical issues such as transportation, lodging, and child care; and not learning about the pregnancy sooner.28,29 Given that patients seeking abortions after 20 weeks are younger and more likely to be unemployed, this policy has the potential to exacerbate health disparities in the region.12 Furthermore, this policy has significant implications for people facing pregnancy-related complications (e.g., severe fetal anomalies) who are denied abortion services.13 By restricting access to wanted and needed abortions in the region, Georgia’s gestational age limit will have a negative impact on the health and economic security of people in the state and region.23 Although these data do not permit investigation of whether residents or nonresidents obtained abortions elsewhere during the study period, it may be unlikely given that until implementation of this policy, Georgia was a critical point of access for people in the Southeast seeking abortions at later gestational ages.10 Indeed, we found that non-Georgia residents experienced the steepest declines in abortion procedures, suggesting that fewer people are traveling to the state to obtain abortions.
Limitations
Our descriptive findings should be considered in the context of several limitations of the ITOP data set. First, because of how the data are structured, we were not able to examine how access to care differed among people of different racial and ethnic groups or socioeconomic backgrounds. Second, Georgia ITOP data do not permit examination of whether people affected by this policy seek and obtain abortion services in other surrounding states; thus, conclusions from our analysis pertain only to how this policy affected abortion care in Georgia. Third, we were not able to adjust for factors beyond the gestational age limit known to influence access to abortion care, such as provider availability or distance from the nearest abortion provider.
Public Health Implications
Nevertheless, our study indicates that Georgia’s 22-week gestational age limit may be adversely affecting access to necessary and desired abortion services for pregnant people across the state and region. Given that economically vulnerable and young people are more likely to need later gestational age services, and that racial and ethnic minority groups are more likely to experience economic vulnerability because of racism, the policy has strong potential to worsen the already-existing reproductive health disparities by income, age, and race/ethnicity in the Southeastern region.30
ACKNOWLEDGMENTS
This study was funded by an anonymous foundation.
Presentations based on the work included in this article were presented at the Clinical and Scientific Meeting of the American College of Obstetricians and Gynecologists; May 3–6, 2019; Nashville, TN; and the Psychosocial Workshop at the Annual Meeting of the Population Association of America; April 9–10, 2019; Austin, TX.
CONFLICTS OF INTEREST
We have no relevant disclosures or conflicts of interest to report.
HUMAN PARTICIPANT PROTECTION
Emory University’s institutional review board reviewed and approved this study; the Georgia Department of Public Health determined that this study was exempt from the requirement for their institutional review board review and approval.
Footnotes
See also Darney and Reid, p. 935.
REFERENCES
- 1.Blank RM, George CC, London RA. State abortion rates: the impact of policies, providers, politics, demographics, and economic environment. J Health Econ. 1996;15(5):513–553. doi: 10.1016/s0167-6296(96)00494-8. [DOI] [PubMed] [Google Scholar]
- 2.Fischer S, Royer H, White C. The impact of reduced access to abortion and family planning services on abortions, births, and contraceptive purchases. J Public Econ. 2018;167:43–68. [Google Scholar]
- 3.Grossman D, Baum S, Fuentes L et al. Change in abortion services after implementation of a restrictive law in Texas. Contraception. 2014;90(5):496–501. doi: 10.1016/j.contraception.2014.07.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Haas-Wilson D. The economic impact of state restrictions on abortion: parental consent and notification laws and Medicaid funding restrictions. J Policy Anal Manage. 1993;12(3):498–511. [PubMed] [Google Scholar]
- 5.Levine PB, Trainor AB, Zimmerman DJ. The effect of Medicaid abortion funding restrictions on abortions, pregnancies and births. J Health Econ. 1996;15(5):555–578. doi: 10.1016/s0167-6296(96)00495-x. [DOI] [PubMed] [Google Scholar]
- 6.Matthews S, Ribar D, Wilhelm M. The effects of economic conditions and access to reproductive health services on state abortion rates and birthrates. Fam Plann Perspect. 1997;29(2):52–60. [PubMed] [Google Scholar]
- 7.New MJ. Analyzing the effect of anti-abortion US state legislation in the post-Casey era. State Polit Policy Q. 2011;11(1):28–47. [Google Scholar]
- 8.Guttmacher Institute. State Bans on Abortions Throughout Pregnancy. New York, NY: Guttmacher Institute; 2019. [Google Scholar]
- 9. HB954, General Session 2011–2012 ed2012.
- 10.Roberts SC, Gould H, Upadhyay UD. Implications of Georgia’s 20-week abortion ban. Am J Public Health. 2015;105(8):e77–e82. doi: 10.2105/AJPH.2015.302728. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Pazol K, Creanga AA, Zane SB, Burley KD, Jamieson DJ. Abortion surveillance—United States, 2009. MMWR Surveill Summ. 2012;61(8):1–44. [PubMed] [Google Scholar]
- 12.Foster DG, Kimport K. Who seeks abortions at or after 20 weeks? [Correction in Perspect Sex Reprod Health. 2019;51(3):185.] Perspect Sex Reprod Health. 2013;45(4):210–218. [DOI] [PubMed]
- 13.Kerns JL, Swanson M, Pena S et al. Characteristics of women who undergo second-trimester abortion in the setting of a fetal anomaly. Contraception. 2012;85(1):63–68. doi: 10.1016/j.contraception.2011.04.012. [DOI] [PubMed] [Google Scholar]
- 14.Haddad LB, Nour NM. Unsafe abortion: unnecessary maternal mortality. Rev Obstet Gynecol. 2009;2(2):122–126. [PMC free article] [PubMed] [Google Scholar]
- 15.Aiken AR, Broussard K, Johnson DM, Padron E. Motivations and experiences of people seeking medication abortion online in the United States. Perspect Sex Reprod Health. 2018;50(4):157–163. doi: 10.1363/psrh.12073. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Kost K. Unintended Pregnancy Rates at the State Level: Estimates for 2010 and Trends Since 2002. New York, NY: Guttmacher Institute; 2015. [Google Scholar]
- 17.MacDorman MF, Declercq E, Cabral H, Morton C. Recent increases in the US maternal mortality rate: disentangling trends from measurement issues. Obstet Gynecol. 2016;128(3):447–455. doi: 10.1097/AOG.0000000000001556. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Baum SE, White K, Hopkins K, Potter JE, Grossman D. Women’s experience obtaining abortion care in Texas after implementation of restrictive abortion laws: a qualitative study. PLoS One. 2016;11(10):e0165048. doi: 10.1371/journal.pone.0165048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Finer LB, Frohwirth LF, Dauphinee LA, Singh S, Moore AM. Timing of steps and reasons for delays in obtaining abortions in the United States. Contraception. 2006;74(4):334–344. doi: 10.1016/j.contraception.2006.04.010. [DOI] [PubMed] [Google Scholar]
- 20.Fuentes L, Lebenkoff S, White K et al. Women’s experiences seeking abortion care shortly after the closure of clinics due to a restrictive law in Texas. Contraception. 2016;93(4):292–297. doi: 10.1016/j.contraception.2015.12.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Jerman J, Frohwirth L, Kavanaugh ML, Blades N. Barriers to abortion care and their consequences for patients traveling for services: qualitative findings from two states. Perspect Sex Reprod Health. 2017;49(2):95–102. doi: 10.1363/psrh.12024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Foster DG, Biggs MA, Ralph L, Gerdts C, Roberts S, Glymour MM. Socioeconomic outcomes of women who receive and women who are denied wanted abortions in the United States. Am J Public Health. 2018;108(3):407–413. doi: 10.2105/AJPH.2017.304247. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Biggs MA, Upadhyay UD, McCulloch CE, Foster DG. Women’s mental health and well-being 5 years after receiving or being denied an abortion: a prospective, longitudinal cohort study. JAMA Psychiatry. 2017;74(2):169–178. doi: 10.1001/jamapsychiatry.2016.3478. [DOI] [PubMed] [Google Scholar]
- 24.Georgia Dept of Public Health. Office of Health Indicators for Planning. Online Analytical Statistical Information System. Induced Termination of Pregnancy (ITOP) Web query. Available at: https://oasis.state.ga.us/oasis/webquery/qryITOP.aspx#. Accessed December 14, 2018.
- 25. Definitions, OCGA §31-10-1.
- 26. Reporting Induced Termination of Pregnancy, OCGA §31-10-19.
- 27.Jones RK, Witwer E, Jerman J. Abortion Incidence and Service Availability in the United States, 2017. New York, NY: Guttmacher Institute; 2019. [Google Scholar]
- 28.Drey EA, Foster DG, Jackson RA, Lee SJ, Cardenas LH, Darney PD. Risk factors associated with presenting for abortion in the second trimester. Obstet Gynecol. 2006;107(1):128–135. doi: 10.1097/01.AOG.0000189095.32382.d0. [DOI] [PubMed] [Google Scholar]
- 29.Janiak E, Kawachi I, Goldberg A, Gottlieb B. Abortion barriers and perceptions of gestational age among women seeking abortion care in the latter half of the second trimester. Contraception. 2014;89(4):322–327. doi: 10.1016/j.contraception.2013.11.009. [DOI] [PubMed] [Google Scholar]
- 30.Upadhyay UD, Weitz TA, Jones RK, Barar RE, Foster DG. Denial of abortion because of provider gestational age limits in the United States. Am J Public Health. 2014;104(9):1687–1694. doi: 10.2105/AJPH.2013.301378. [DOI] [PMC free article] [PubMed] [Google Scholar]