Abstract
Cardiorespiratory fitness, as assessed through peak oxygen uptake (VO2peak), is a powerful health indicator. We aimed to evaluate the influence of several candidate causal genetic variants on VO2peak level in untrained Han Chinese people. A total of 1009 participants (566 women; age [mean ± SD] 40 ± 14 years, VO2peak 29.9 ± 7.1 mL/kg/min) performed a maximal incremental cycling test for VO2peak determination. Genomic DNA was extracted from peripheral whole blood, and genotyping analysis was performed on 125 gene variants. Using age, sex, and body mass as covariates, and setting a stringent threshold p-value of 0.0004, only one single nucleotide polymorphism (SNP), located in the gene encoding angiotensin-converting enzyme (rs4295), was associated with VO2peak (β = 0.87; p < 2.9 × 10−4). Stepwise multiple regression analysis identified a panel of three SNPs (rs4295 = 1.1%, angiotensin II receptor type 1 rs275652 = 0.6%, and myostatin rs7570532 = 0.5%) that together accounted for 2.2% (p = 0.0007) of the interindividual variance in VO2peak. Participants carrying six ‘favorable’ alleles had a higher VO2peak (32.3 ± 8.1 mL/kg/min) than those carrying only one favorable allele (24.6 ± 5.2 mL/kg/min, p < 0.0001). In summary, VO2peak at the pre-trained state is partly influenced by several polymorphic variations in candidate genes, but they represent a minor portion of the variance.
Keywords: VO2max, maximal oxygen uptake, single nucleotide polymorphism, genomics, endurance performance
1. Introduction
Cardiorespiratory fitness (CRF) is positively associated with endurance exercise performance [1] and is a strong prognostic factor of morbidity and mortality from all causes and, particularly, from cardiovascular disease (CVD) [2,3]. While both physical activity (PA) and exercise training can modify CRF and are inversely associated with morbidity and mortality rates [4], CRF per se is a much stronger predictor of prognosis in CVD and metabolic disorders [5,6]. The measure of an individual’s peak capacity to perform dynamic aerobic exercise is dependent on the synergistic action of pulmonary, cardiovascular and muscle tissue via a suite of physiological actions that effectively transport and deliver oxygen from the atmosphere to mitochondria in working muscles [7,8]. Accordingly, CRF can be assessed by directly measuring the peak oxygen uptake (VO2peak) reached during a graded dynamic exercise test until exhaustion, involving large muscle masses (e.g., running or bicycling), or by indirectly estimating this variable from the peak workload achieved. Nevertheless, direct evaluation of VO2peak is considered the gold standard measure of CRF and, indeed, the American Heart Association recently advocated for the routine assessment of this measure as a clinical vital sign [9].
VO2peak is characterized by a high interindividual variability even in people of the same sex, age and with the same level of PA and exercise training. This variability is believed to be related, at least partly, to heredity. A seminal study by Claude Bouchard and colleagues found comparable VO2peak values in brothers of the same sibship, and the similarities in VO2peak were even greater in dizygotic and monozygotic twins [10]. The authors suggested that the genetic effect on VO2peak reached ~40%. In a similar study of 170 individuals and their offspring (n = 259), it was found that about 50% of the interindividual variance in VO2peak corresponded to heritable factors after adjusting for age, sex, body mass, and body composition [11]. These findings have been replicated in subsequent studies with siblings and twins [12] and, to date, it is commonly accepted that VO2peak is influenced by both genetic (~50–60%) and environmental factors. It has also been reported that twins with similar VO2peak values present with comparable levels of a variety of PA indices [13], suggesting that part of the heritability of VO2peak in twins might be due to the similarity of their PA levels. In fact, in a recent analysis of 123,545 single nucleotide polymorphisms (SNPs), only nine were associated with VO2peak [14]. The authors of this study found that those individuals whose genotype was associated with a high VO2peak value had a lower CVD risk (e.g., less visceral fat or lower total blood cholesterol), but they did not calculate the additive effect that the nine SNPs had on the interindividual variability of VO2peak. There is therefore controversy on the influence of genetics on VO2peak, which mostly likely stems from the discrepancies between studies conducted on siblings/twins vs those conducted on individuals with no familial connection. In this regard, determining the actual genetic contribution to the interindividual variability in VO2peak would be of major importance to inform how environmental factors—including lifestyle—might contribute to heightened VO2peak values. It is possible that if the influence of genetics on VO2peak is low, exercise training might be a determining factor to enhance ‘innate’ VO2peak even in those less genetically predisposed, with obvious subsequent benefits for cardiovascular health. Indeed, previous research has reported VO2peak increases of up to 44% after strenuous training interventions, which would support a strong influence of environmental factors on CRF [15].
Aerobic/endurance exercise-based training appears to be the most effective way to augment VO2peak. Exercise training increases rather than decreases the individual differences seen at baseline VO2peak because the response to training itself shows large variation [16]. A genome-wide association study based on 324,611 SNPs found that only 21 SNPs could explain 48.6% of the change in VO2peak induced by a 20-week exercise training program [17]. Among them, rs6552828, located in the acyl-CoA synthase long-chain member 1 (ACSL1) gene, accounted by itself for 6% of the training-induced enhancement in VO2peak. In a recent meta-analysis of 35 articles on the genetic influence on VO2peak trainability, a total of 97 genes were associated with this phenotype, although only 13 genetic variants were reproduced by more than two investigations [18].
Knowledge on the genetic influence on baseline VO2peak (i.e., in isolation from training) is mainly based on studies conducted on siblings/twins or in individuals of Caucasian descent, and it remains to be determined whether the genetic variants that might be associated with baseline VO2peak are similar or different in individuals of other ethnicities. Thus, the aim of the present study was to assess the influence of several candidate genetic variants in the interindividual variation of baseline CRF measured as VO2peak, in Han Chinese individuals.
2. Materials and Methods
2.1. Participants
A total of 1047 participants (56% women) volunteered to participate in the study. The sample was recruited from five cities in China: Beijing, Xi’an, Guangzhou, Shenyang, and Tianjin. Inclusion criteria were the following: male/female aged 18–69 years; being of Chinese (Han) descent and unrelated to the other participants; having no CVD, diabetes or abnormal glucose tolerance, or any other acute or chronic disease; and being untrained (i.e., ≤ 2 sessions/week of ≤ 30min of regular physical exercise in the previous 12 months). One week before the start of the investigation, participants were fully informed of the experimental procedures and signed an informed written consent to participate in the investigation. The study protocol was approved by the Institutional Review Board of the China Institute of Sport Science.
2.2. Experimental Design
This is an observational cross-sectional study aimed at determining the genetic influence of target genes on the interindividual variability in VO2peak values in untrained Han Chinese individuals. We selected untrained individuals to avoid any influence of exercise training or planned PA in the analysis.
2.3. Experimental Protocol
The day of the first experimental trial, participants underwent a medical examination (including medical history and other routine physical examinations) carried out by a licensed physician, to ensure the suitability of all participants to take part in the research protocols. On the same day, whole body dual-energy X-ray absorptiometry (GE Lunar DPX system, Madison, WI, USA) assessments were performed and used to calculate body fat and fat-free mass following previous recommendations [19]. VO2peak (in mL/kg/min) was determined during a continuous incremental exercise test to volitional fatigue performed on a bicycle ergometer (Ergoselect 100, Ergoline GmbH, Bitz, Germany). Before tests, participants were familiarized with the ergometer and with the rating of perceived exertion (RPE), as measured by the Borg 6–20 scale [20]. Participants performed a standardized warm-up (5 min cycling at 20 W and 60 rpm), and the workload (starting at 20 W) was then increased by 25 W (men) or 20 W (women) every 2 minutes until volitional exhaustion. In participants >60 years of age, the workload was increased by 20 W (men) or 15 W (women) every 2 minutes. During the test, gas exchange data were measured ‘breath-by-breath’ with a metabolic cart (MetaMax 3B, Cortex Biophysik GmbH, Leipzig, Germany). Certified calibration gases (16.0% O2, 5.0% CO2, Cortex Biophysik) and a 3-L syringe were used to calibrate the gas analyzer and the flow meter, respectively, before each test. VO2peak was defined as the highest VO2 value (60-s average) obtained during the test. VO2peak was considered valid when participants achieved at least two of the following criteria: (i) RPE >17, (ii) VO2 difference between the last two consecutive loads <0.15 L/min, (iii) respiratory exchange ratio >1.1, and (iv) peak heart rate >85% of the age-adjusted estimate [21]. Heart rate was recorded with a chest strap transmitter (Polar RS400, Polar Electro, Kempele, Finland). The environmental temperature was similar in all measurement centers (~22 °C, 40% relative humidity).
On a different day during the week of testing, genomic DNA was extracted from peripheral whole blood samples using the Wizard Genomic DNA Purification Kit (Promega; Madison, WI, USA). Genotyping was performed at Shanghai Benegene Biotechnology, LTD (Shanghai, China). For analysis, a list of 125 SNPs (Table A1 and Table A2, Table A3 and Table A4) for the Han population of Beijing, China (CHB) was obtained from the International HapMap Project database. Haplotype-tag SNPs were selected using the following criteria: minor allele frequency ≥0.01 and measure of linkage disequilibrium (r2 > 0.8). Initially, genes associated with cardiovascular responses to exercise were chosen, and genes associated with endurance performance, muscle performance, or body composition were then added as all of these factors might contribute to the value of VO2peak (Table 1).
Table 1.
Target genes selected for the investigation.
| Gene | Numbers of SNPs | Chromosome Location | References |
|---|---|---|---|
| ACE | 3 | chr17:58,908,166-58,928,711 | [22] |
| ACE2 | 2 | chrX:15,489,077-15,529,058 | [23,24] |
| ACSL1 | 15 | chr4: 185,911,544-185,986,209 | [17,25] |
| ACTN3 | 1 | chr11:66,313,866-66,330,800 | [26,27] |
| AGT | 13 | chr1:228,902,892-228,918,564 | [28,29] |
| AGTR1 | 9 | chr3:149,898,348- 149,943,480 | [30,31] |
| AGTR2 | 3 | chrX:115,214,031-115,221,847 | [32] |
| BDKRB2 | 28 | chr14:95,738,950-95,782,536 | [33] |
| FGF21 | 2 | chr19:53,949,156-53,955,394 | [34] |
| FGFR2 | 1 | chr10:123,237,848-123,357,972 | [34] |
| FNDC5 | 3 | chr1:33,327,869-33,338,083 | [35] |
| FST | 3 | chr5: 52,812,352-52,817,659 | [36,37] |
| FTO | 3 | chr16:53,737,875-54,155,853 | [38] |
| GDF8 | 4 | chr2:190,920,423-190,927,455 | [39,40] |
| IL-6 | 7 | chr7:22,733,345-22,738,141 | [41] |
| IL-15 | 2 | chr4:142,557,752-142,665,140 | [42,43] |
| ITLN1 | 5 | chr1:160,846,329-160,854,960 | [44] |
| PGC-1α | 6 | chr4: 23,756,664-23,905,712 | [45] |
| PGC -1β | 1 | chr5:149,109,861-149,234,585 | [45] |
| PPRC1 | 1 | chr10: 103, 880, 777-103, 902, 078 | [45] |
| PRDM16 | 2 | chr1: 2,985,732-3,355,185 | [46] |
| PYY | 5 | chr17:39,385,633-39,437,363 | [47] |
| REN | 5 | chr1: 202,390,571-202,402,088 | [48] |
| RETN | 1 | chr19:7,639,972-7,641,340 | [49] |
Abbreviations: SNP, single nucleotide polymorphism. Abbreviations for gene names: ACE, angiotensin-converting enzyme; ACE2, angiotensin-converting enzyme 2; ACSL1, acyl-CoA synthase long-chain member 1; ACTN3, alpha-actinin-3; AGT, angiotensinogen; AGTR1, angiotensin II receptor type 1; AGTR2, angiotensin II receptor type 2; BDKRB2, bradykinin receptor B2; FGF21, Fibroblast growth factor 21; FGFR2, fibroblast growth factor receptor 2; FNDC5, fibronectin type III domain-containing protein 5; FST, follistatin; FTO, fat mass and obesity-associated protein (also known as ‘alpha-ketoglutarate-dependent dioxygenase’; GDF8, growth differentiation factor 8 (also known as ‘myostatin’); IL-6, interleukin 6; IL-15, interleukin 15; ITLN1, intelectin 1; PGC-1α, peroxisome proliferator-activated receptor-gamma coactivator (PGC)-1alpha; PGC-1β, peroxisome proliferator-activated receptor-gamma coactivator (PGC)-1beta; peroxisome PPRC1, proliferator-activated receptor gamma, coactivator-related 1; PRDM16, PR domain containing 16; PYY, peptide YY; REN, renin; RETN, resistin.
For high-throughput genotyping of SNPs, we used a matrix-assisted laser desorption/ionization time-of-flight mass spectrometry (MALDI-TOF MS) platform (Agena, San Diego, CA, USA). Primers for the polymerase chain reaction (PCR) and single-base extension were designed using the Assay Designer software package (Assay Design Suite V2.0, Agena, San Diego, CA, USA). Genotyping was performed as described elsewhere [50].
2.4. Statistical Analysis
All statistical analyses were performed using SAS 9.4 statistical package (SAS institute, Inc., Cary, NC, USA) and PLINK (v1.07). Hardy–Weinberg Equilibrium (HWE) was tested using χ2 tests. Linear regression analyses were conducted to assess the association—expressed as standardized regression coefficients (β)—between each SNP and VO2peak, with age, body mass and sex as covariates. The Bonferroni correction for multiple comparisons was applied to test for statistically significant associations between SNPs and VO2peak, thereby setting the minimum level of significance at p < 0.0004 (i.e., 0.05 divided by the number of SNPs, i.e., 125). A multivariable regression analysis was then conducted to assess the overall contribution of the most significant SNPs to the interindividual variability of VO2peak. All SNPs with p < 0.05 were included, and a regression model with backward elimination was used to filter-out redundant SNPs. By using a threshold of 5.0 points in the variance inflation factor, we avoided multicollinearity. SNPs that were retained in the final backward elimination model were then analyzed with a multivariate regression model using forward selection. The produced regression equation was accepted at a significance level of p <0.01. The values of R2 were adjusted for the number of cases and parameters in the analysis. The relative contribution (R2) of each SNP in relation to the explained variance in VO2peak was calculated as follows (Equation (1)):
| Partial contribution (R2 adjusted) = ([β for parameter] / Σ [of all β in equation]), | (1) |
In the SNPs retained in multiple regression, VO2peak values were compared among genotypes by using one-way analysis of variance (ANOVA). When the ANOVA showed a significant F value, pairwise differences were assessed using the Tukey post-hoc test. By using the SNPs retained in multiple regression analyses, we calculated a weighted genotype score to assess the combined influence of the SNPs on VO2peak following the procedure of Williams and Folland [51]. First, each genotype was scored within each SNP by assigning 0 arbitrary units (a.u.) to homozygotes for the allele theoretically associated with low VO2peak, 1 a.u. to heterozygotes, and 2 a.u. to homozygotes for the allele associated with high VO2peak, following an additive model. Each SNP was then weighted by its β-coefficient (allele effect) based on the assumption that all SNPs of interest have independent effects and contribute in an additive manner to VO2peak. Finally, the scores obtained for each SNP were summed to obtain a unique weighted genotype score for each participant (theoretical range: 0–6 a.u.). For clarity, we merged data of participants by using intervals of 1 a.u. Differences in VO2peak between participants in the different groups were assessed by one-way analysis of variance and using the least significant difference post hoc test. Finally, the ability of weighted genotype score to distinguish individuals with low or intermediate CRF (i.e., below or above 28 mL/kg/min, as proposed by Kodama et al. [52]) was assessed using a receiver operating characteristic (ROC) curve and by determining the area under the ROC curve (AUC).
3. Results
Of the initial 1047 individuals recruited, valid VO2peak measurements were obtained for 1009 individuals (566 women), and thus only these participants were included in the analyses. The main characteristics of the participants are shown in Table 2.
Table 2.
Main characteristics of the study participants (N = 1009) and their association with peak oxygen uptake.
| Variable | Mean ± SD | Range | β | p-Value |
|---|---|---|---|---|
| Age (year) | 40 ± 14 | 19–69 | −0.27 | <0.001 |
| Height (cm) | 165.3 ± 8.3 | 146.2–187.0 | 0.31 | <0.001 |
| Body mass (kg) | 64.3 ± 11.6 | 39–104 | −0.01 | 0.523 |
| Body mass index (kg/m2) | 23.4 ± 3.1 | 15.6–34.8 | −0.64 | <0.001 |
| Body fat (%) | 27.1 ± 8.8 | 4.5–44.5 | −0.58 | <0.001 |
| Fat-free mass (kg) | 43.8 ± 9.5 | 24.8–70.1 | 0.31 | <0.001 |
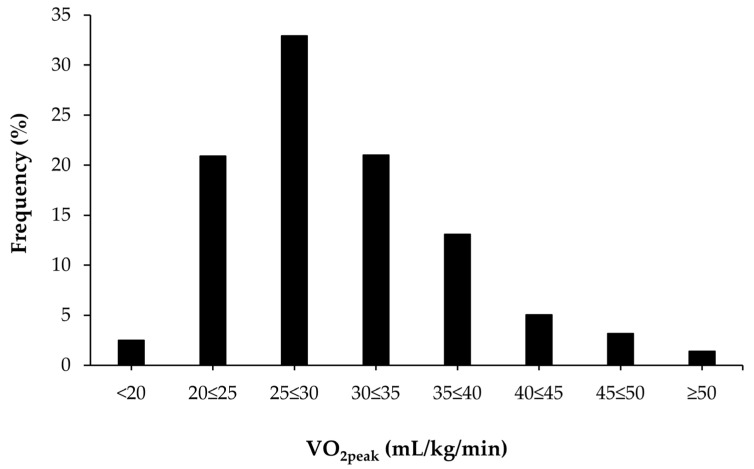
Figure 1 shows the distribution of VO2peak values in the study sample. Approximately 2.5% of all participants had a VO2peak <20 mL/kg/min and 1.4% had a VO2peak level >50 mL/kg/min.
Figure 1.
Distribution of peak oxygen uptake (VO2peak) data in the study participants.
Genotyping was successful (i.e., successful determinations for all SNPs) in 1006 of 1009 participants (99.7%). From the 125 SNPs analyzed, 10 were discarded because they deviated from HWE (Table A2), 10 because they had a MAF <5% (Table A3), and two because only one genotype was detected across the group of participants (Table A4). From the remaining pool of 103 SNPs, only rs4295, located in the angiotensin-converting enzyme (ACE) gene, was significantly associated with VO2peak (p < 2.9 × 10−4, β = 0.87; minor allele (G) frequency, 38.1%, heterozygosity frequency, 47.4%).
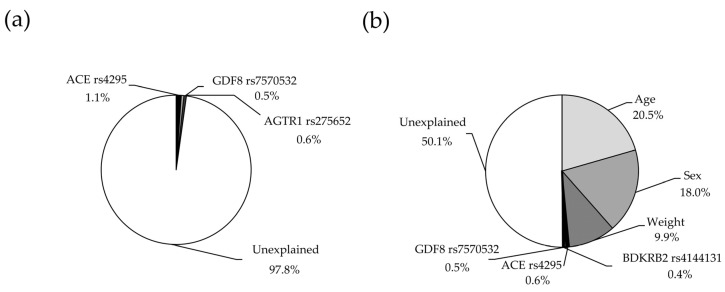
In multiple regression analysis, and after excluding those SNPs with collinearity, only three were retained in the final model (ACE rs4295, AGTR1 rs275652, GDF8 rs7570532), which explained together 2.2% (p = 0.0007) of the variance in VO2peak (Figure 2a, statistical power = 0.987). The partial contribution of each SNP to the variance in VO2peak is shown in Table 3. The explained variance of VO2peak increased to 50.1% (p < 0.0001) when including covariates such as age, sex and weight in the model (Figure 2b, statistical power = 1.00).
Figure 2.
Variance in peak oxygen uptake in the study participants explained by genetic variants alone (a) and by genetic variants plus anthropometric covariates (b). Abbreviations for gene names: ACE, angiotensin-converting enzyme; AGTR1, angiotensin II receptor type 1; BDKRB2, bradykinin receptor B2; GDF8, growth differentiation factor 8 (also known as ‘myostatin’).
Table 3.
List of single nucleotide polymorphisms associated with peak oxygen uptake in the study participants. Model 1, with genetic-only influence; model 2 with covariates.
| SNP | Partial R2 | p-Value | |
|---|---|---|---|
| Model 1 | ACE rs4295 | 0.0110 | 0.0024 |
| AGTR1 rs275652 | 0.0056 | 0.0293 | |
| GDF8 rs7570532 | 0.0053 | 0.0342 | |
| Model 2 | Age | 0.2052 | <0.0001 |
| Sex | 0.1800 | <0.0001 | |
| Weight | 0.0994 | <0.0001 | |
| ACE rs4295 | 0.0063 | 0.0015 | |
| GDF8 rs7570532 | 0.0046 | 0.0058 | |
| BDKRB2 rs4144131 | 0.0037 | 0.0135 |
Abbreviation: SNP, single nucleotide polymorphism; Abbreviations for gene names: ACE, angiotensin-converting enzyme; AGTR1, angiotensin II receptor type 1; BDKRB2, bradykinin receptor B2; GDF8, growth differentiation factor 8 (also known as ‘myostatin’).
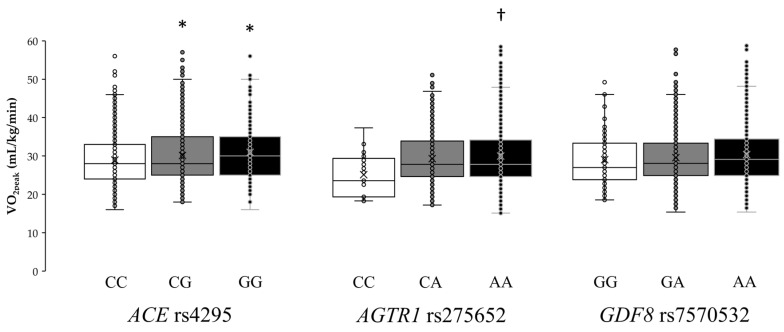
Individual VO2peak values for each genotype of the ACE rs4295, AGTR1 rs275652, and GDF8 rs7570532 polymorphisms are shown in Figure 3. The one-way ANOVA revealed statistically significant differences in ACE rs4295 (F = 4.95, p = 0.007) and AGTR1 rs275652 (F = 3.90, p = 0.021) polymorphisms, while the ANOVA did not show differences for GDF8 rs7570532 (F = 1.64, p = 0.194) polymorphism. Specifically, GG homozygotes in ACE rs4295 had a mean VO2peak of 31.1 ± 7.9 mL/kg/min, which was higher than that found in heterozygotes (GC, 29.8±6.9 mL/kg/min; p = 0.049) or in homozygotes for the common allele (CC, 28.9 ± 6.7 mL/kg/min; p = 0.013). In addition, AA homozygotes in AGTR1 rs275652 had a mean VO2peak of 30.0 ± 7.3 mL/kg/min, which was higher than that found in homozygotes for the minor allele (CC, 25.5 ± 5.3 mL/kg/min; p = 0.024).
Figure 3.
Box-and-whisker plots showing peak oxygen uptake (VO2peak) in the study participants according to genetic variations in the genes for angiotensin-converting enzyme (ACE; rs4295), angiotensin II receptor type 1 (AGTR1; rs275652), and growth differentiation factor 8 (GDF8, also known as ‘myostatin’; rs7570532). The lines in the box represent the first, second (median) and third quartiles, and the whiskers represent 1.5 × interquartile ranges. Each dot represents one individual within the specified genotype. (*) Depicts a statistically significant difference from CC genotype in ACE rs4295 polymorphism at p < 0.05. (†) Depicts a statistically significant difference from CC genotype in AGTR1 rs275652 polymorphism at p < 0.05.
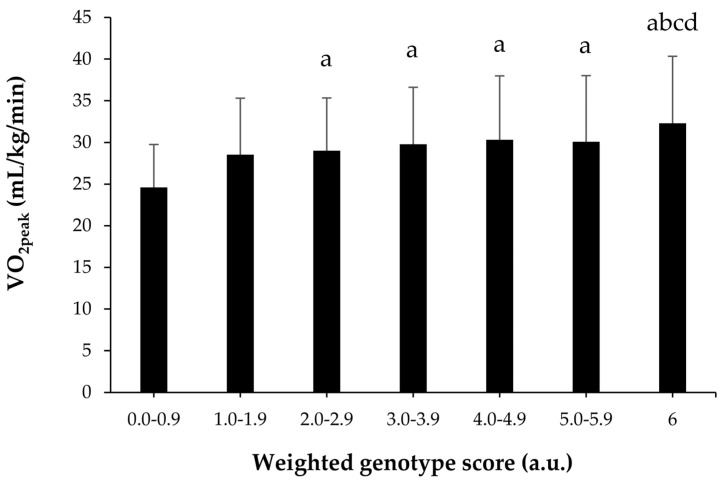
A weighted genotype score was constructed using the three SNPs shown in model 1 of genetic-only influence. Participants were categorized with a genotype score from 0 a.u., indicating the presence of homozygosity for all the alleles associated with a lower VO2peak in ACE (rs4295), AGTR1 (rs275652) and GDF8 (rs7570532), to 6 a.u., indicating the presence of homozygosity for all the alleles associated with a higher VO2peak in the aforementioned SNPs. A linear effect was found for genotype score on VO2peak (Figure 4). Specifically, the individuals with 6 a.u. had a higher VO2peak than those with scores up to 4.0 a.u. (p < 0.05). In addition, participants with scores >2 a.u. had a higher VO2peak than those with scores <1.0 a.u. (p < 0.05). ROC analysis showed significant discriminatory accuracy of the weighted genotype score in the identification of individuals with low/intermediate CRF (AUC = 0.542) with a sensitivity of 0.733 and a specificity of 0.305.
Figure 4.
Peak oxygen uptake (VO2peak) levels in the study participants according to the genotype score (computed by using a weighted score of angiotensin-converting enzyme rs4295, angiotensin II receptor type 1 rs275652 and growth differentiation factor 8 rs7570532 genotypes). Abbreviations/symbols: a.u., arbitrary units; a, difference from 0–0.9 a.u. at p<0.05; b, difference from 1.0–1.9 a.u. at p < 0.05; c, difference from 2.0–2.9 a.u. at p < 0.05; d, difference from 3.0–3.9 a.u. at p < 0.05.
4. Discussion
CRF, particularly when objectively determined as VO2peak, is strongly associated with endurance performance and health outcomes. Indeed, VO2peak reflects the peak integrative ability of the organism to deliver oxygen from the atmosphere to the mitochondria of working muscles. The VO2peak is thus determined, among other factors, by peak cardiac output and pulmonary ventilation, lung diffusion capacity, blood and plasma volume, hemoglobin mass, and muscle capillary density and oxidative capacity [53]. Importantly, the mean values of VO2peak of our participants (29.9 ± 7.1 mL/kg/min or 8.5 metabolic equivalents, i.e., METs) were barely above the minimum healthy threshold for all-cause and CVD mortality in middle-aged men/women (i.e., 8 METs [52]). It is thus of medical importance to determine whether genetic factors (including specific gene variants) are associated with variability of CRF around (i.e., above vs below) the 8-MET cutoff. Previous research in siblings/twins suggests that 50%–60% of the variance of VO2peak is associated with heredity [10,12]. These values seem surprisingly high given the variety of physiological processes and body tissues involved in the uptake and utilization of oxygen in muscle mitochondria. Indeed, there is open debate about the limits of the evidence that support the relative influence of genetics on the variability and trainability of CRF [54,55].
Our findings question the high heritability of VO2peak, at least in Chinese individuals with no familial connection. From the 125 SNPs selected for our study, only one (ACE rs4295) was associated with VO2peak. Also, the best model obtained through multiple regression analyses could only explain ~2.2% of the interindividual variance in VO2peak. As in the study by Bye et al. [14], we created a polygenic score to determine whether those individuals with a higher number of alleles associated with VO2peak did indeed present with higher values of this parameter. The only differences found between our findings and those of the Bye et al. study were the number of SNPs included in the polygenic score (7 vs 3, respectively) and the use of an intermediate genotype score for heterozygotes, which was not included by Bye et al. Interestingly, in both studies, participants with the theoretically lowest (or ‘less favorable’) genotype scores had the lowest VO2peak (22–24 mL/kg/min), which was significantly lower than for those with the theoretically highest (or ‘most favorable’) genotype score (~32 mL/kg/min). These findings suggest that only a small number of SNPs are associated with the odds of having high VO2peak values in untrained individuals. The variance of the interindividual variability in VO2peak explained with these genotypes is low and the addition of favorable alleles might produce a change of 8–10 mL/kg/min. This genetic influence might be considerable in clinical terms because each 1-MET (or 3.5 mL/kg/min) increase in CRF has been shown to confer a 12% improvement in survival in Caucasian (North-American) men [6]. Moreover, as mentioned above, it is of clinical importance to surpass the 8-MET threshold, and in fact, adults with a CRF clearly above this level (>10 METs) have a remarkably reduced CVD risk [56]. In this regard, the probability of surpassing the 8-MET threshold (equivalent to 28 mL/kg/min) was doubled in those participants that carried the six ‘favorable’ alleles (Figure 4).
Only three SNPs were included in the final multiple regression model. ACE rs4295 has not been previously associated with endurance performance, but it is located in the same linkage disequilibrium block as the widely studied ACE insert(I)/deletion(D) polymorphism (rs4340) [57]. The ACE gene encodes angiotensin-converting enzyme and the I allele might be associated with lower circulating levels of enzyme, and the II genotype potentially associated with performance in endurance athletes (odds ratio 1.35; 95% confidence interval, 1.17 to 1.55 [58]). However, several studies have found no association between the ACE I/D genotype and VO2peak values in trained [59] and untrained [60,61] individuals. With regard to the ACE rs4295 variation found in the present study, although its influence on CRF needs to be replicated in other cohorts, our findings bolster the role of angiotensin-converting enzyme and its coding gene as predictors of CRF-related phenotypes. We also found that carriage of the C allele in the AGTR1 rs275652 polymorphism was negatively associated with VO2peak values. This gene encodes the angiotensin II receptor 1 (AT1R), and polymorphisms in AGTR1 have been suggested to be involved in the physiological response to hypoxia [62]. AT1R is broadly expressed in different tissues and mediates most of the classical actions of angiotensin II, including vasoconstriction and vascular smooth muscle cell proliferation [63]. Thus, under hypoxic conditions, angiotensin II engages AT1R to modulate the pulmonary vasoconstrictive response [64]. Although speculative, it is possible that the C allele in AGTR1 rs275652 might exacerbate pulmonary vasoconstriction during exercise owing to a higher activation of AT1R for a given concentration of angiotensin II [65]. The last SNP included in the model explaining VO2peak was rs7570532, a genetic variation in GDF8 encoding myostatin. This and other SNPs in GDF8 have been indirectly associated with a major cardiometabolic condition, obesity [39], but other authors have reported no association of rs7570532 with endurance performance [40]. Myostatin controls the differentiation and proliferation of skeletal muscle throughout embryonic development and regulates muscle growth during adulthood. Mutations in GDF8 that produce non-functional myostatin result in the increased growth of skeletal muscle, demonstrating the existence of a powerful mechanism to control muscle size in normal individuals through this protein [66]. Based on these findings and given the positive association between muscle mass and VO2peak [66,67,68], it is possible that GDF8 rs7570532 confers a small but significant predisposition to higher VO2peak values. Further research on these three SNPs is clearly warranted.
We acknowledge that the current investigation has some limitations. First, our study sample was heterogeneous in terms of age, sex, and anthropometric characteristics (Table 1). Although we used these variables as covariates in linear regression analyses, the high variability of these variables might have partially influenced our results. In fact, when they were included in multiple regression analyses (Figure 2b), the explained variance of VO2peak increased up to 50.1%. Second, our study only included participants of Han Chinese descent and the results might therefore not be applicable to other ethnicities. Of note, the Han Chinese constitute the world’s largest ethnic group (constituting ~18% of the global population), but further studies in other large ethnic groups will be needed to confirm/discard the generalizability of these results. Lastly, we only analyzed 125 SNPs and thus it is plausible that other candidate genes might have an influence on VO2peak.
5. Conclusions
The present study shows that in a cohort of untrained Han Chinese individuals, VO2peak is influenced by a very few polymorphic variations in key genes even in isolation of training adaptations. The genetic influence accounted for ~2.2% of the interindividual variance in VO2peak, at least with the 125 SNPs included in this investigation. Although more research is needed, these data suggest that environment, probably more than genetics, is responsible for most of the interindividual variability in VO2peak among healthy Han Chinese adults.
Acknowledgments
The authors would like to thank all the participants in the study.
Appendix A
Table A1.
List of SNPs investigated for association with VO2peak (mL/kg/min) in Han Chinese untrained individuals.
| Gene | SNP | MA | MAF |
|---|---|---|---|
| ACE | rs4295 | G | 38.1 |
| ACE | rs4341 | G | 34.9 |
| ACE | rs4363 | G | 38.7 |
| ACE2 | rs6632677 | C | 9.2 |
| ACSL1 | rs10022018 | G | 24.4 |
| ACSL1 | rs11732302 | C | 24.7 |
| ACSL1 | rs12503643 | G | 45.9 |
| ACSL1 | rs12644905 | T | 19.6 |
| ACSL1 | rs13126272 | T | 11.0 |
| ACSL1 | rs1803898 | A | 7.3 |
| ACSL1 | rs2292898 | C | 7.8 |
| ACSL1 | rs13120078 | A | 8.2 |
| ACSL1 | rs2280297 | C | 47.6 |
| ACSL1 | rs2292899 | A | 38.1 |
| ACSL1 | rs3749233 | A | 25.9 |
| ACSL1 | rs3792312 | G | 41.7 |
| ACSL1 | rs4069938 | G | 37.7 |
| ACSL1 | rs6552828 | G | 35.2 |
| ACSL1 | rs902177 | C | 28.2 |
| ACTN3 | rs1815739 | T | 41.7 |
| AGT | rs10864770 | T | 34.5 |
| AGT | rs11568046 | C | 12.9 |
| AGT | rs2478523 | C | 46.0 |
| AGT | rs2478544 | C | 21.8 |
| AGT | rs2493132 | T | 37.3 |
| AGT | rs3789671 | G | 45.5 |
| AGT | rs3789678 | T | 18.7 |
| AGT | rs3889728 | A | 49.4 |
| AGT | rs5050 | G | 14.8 |
| AGT | rs6687360 | C | 33.1 |
| AGT | rs699 | T | 19.7 |
| AGT | rs7079 | A | 16.2 |
| AGT | rs7536290 | G | 22.0 |
| AGTR1 | rs2131127 | T | 37.4 |
| AGTR1 | rs275652 | C | 13.6 |
| AGTR1 | rs3772616 | A | 17.8 |
| AGTR1 | rs385338 | G | 18.0 |
| AGTR1 | rs5182 | C | 28.1 |
| AGTR1 | rs6801836 | C | 14.2 |
| BDKRB2 | rs10130005 | C | 18.3 |
| BDKRB2 | rs10132462 | T | 28.1 |
| BDKRB2 | rs11160322 | C | 23.0 |
| BDKRB2 | rs11627176 | G | 12.0 |
| BDKRB2 | rs11627761 | T | 15.3 |
| BDKRB2 | rs11848502 | T | 30.1 |
| BDKRB2 | rs12433275 | T | 16.3 |
| BDKRB2 | rs12888402 | C | 16.7 |
| BDKRB2 | rs1799722 | C | 48.0 |
| BDKRB2 | rs1959053 | T | 25.3 |
| BDKRB2 | rs2069575 | A | 20.4 |
| BDKRB2 | rs2069578 | G | 39.1 |
| BDKRB2 | rs2069586 | A | 16.5 |
| BDKRB2 | rs2069588 | T | 18.0 |
| BDKRB2 | rs2369521 | G | 35.6 |
| BDKRB2 | rs4144131 | A | 43.9 |
| BDKRB2 | rs4900315 | C | 46.5 |
| BDKRB2 | rs4900318 | A | 49.7 |
| BDKRB2 | rs4905470 | A | 20.0 |
| BDKRB2 | rs4905474 | A | 37.1 |
| BDKRB2 | rs6575577 | G | 22.5 |
| BDKRB2 | rs7155797 | T | 44.4 |
| BDKRB2 | rs7161665 | C | 47.9 |
| BDKRB2 | rs8013400 | T | 28.5 |
| BDKRB2 | rs8016905 | A | 32.7 |
| BDKRB2 | rs885818 | T | 13.4 |
| BDKRB2 | rs945039 | T | 42.9 |
| FGFR2 | rs2071616 | T | 8.8 |
| FNDC5 | rs16835198 | T | 47.7 |
| FNDC5 | rs3480 | G | 24.8 |
| FST | rs3797296 | G | 17.3 |
| FST | rs3797297 | T | 12.8 |
| FTO | rs1421085 | C | 10.4 |
| FTO | rs1558902 | A | 10.6 |
| FTO | rs9939609 | A | 10.4 |
| GDF-8 | rs16832288 | A | 19.9 |
| GDF-8 | rs7570532 | G | 26.0 |
| IL-15 | rs1057972 | A | 49.9 |
| IL-6 | rs1524107 | C | 29.3 |
| IL-6 | rs2069840 | G | 7.3 |
| IL-6 | rs2069830 | G | 27.2 |
| IL-6 | rs2069837 | G | 20.1 |
| IL-6 | rs2069852 | G | 37.0 |
| ITLN1 | rs2274906 | A | 36.5 |
| ITLN1 | rs2274910 | T | 29.6 |
| ITLN1 | rs2297560 | T | 13.9 |
| ITLN1 | rs6427552 | C | 24.7 |
| PGC-1α | rs12374310 | C | 43.9 |
| PGC-1α | rs12650562 | C | 49.5 |
| PGC-1α | rs251468 | T | 19.8 |
| PGC-1α | rs4452416 | G | 13.4 |
| PGC-1α | rs4697425 | G | 30.8 |
| PGC-1α | rs6821591 | C | 29.9 |
| PRDM16 | rs12409277 | C | 42.0 |
| PRDM16 | rs2236518 | A | 44.5 |
| PYY | rs10853114 | C | 37.8 |
| PYY | rs12953033 | A | 6.9 |
| PYY | rs162430 | G | 35.3 |
| PYY | rs1859223 | G | 27.2 |
| REN | rs11571078 | T | 12.7 |
| REN | rs1464816 | T | 24.4 |
| REN | rs2368564 | T | 20.3 |
| REN | rs4951313 | G | 29.1 |
| REN | rs5707 | G | 40.3 |
| RETN | rs3745367 | A | 35.5 |
Abbreviations: MA, minor allele; MAF, minor allele frequency; SNP, single nucleotide polymorphism; VO2peak, peak oxygen uptake. Abbreviations for gene names: ACE, angiotensin-converting enzyme; ACE2, angiotensin-converting enzyme 2; ACSL1, acyl-CoA synthase long-chain member 1; ACTN3, alpha-actinin-3; AGT, angiotensinogen; AGTR1, angiotensin II receptor type 1; AGTR2, angiotensin II receptor type 2; BDKRB2, bradykinin receptor B2; FGF21, Fibroblast growth factor 21; FGFR2, fibroblast growth factor receptor 2; FNDC5, fibronectin type III domain-containing protein 5; FST, follistatin; FTO, fat mass and obesity-associated protein (also known as ‘alpha-ketoglutarate-dependent dioxygenase’; GDF8, growth differentiation factor 8 (also known as ‘myostatin’); IL-6, interleukin 6; IL-15, interleukin 15; ITLN1, intelectin 1; PGC-1α, peroxisome proliferator-activated receptor-gamma coactivator (PGC)-1alpha; PRDM16, PR domain containing 16; PYY, peptide YY; REN, renin; RETN, resistin.
Appendix B
Table A2.
List of SNPs discarded for analyses because did not meet the Hardy–Weinberg equilibrium.
| Gene | SNP | MA | MAF |
|---|---|---|---|
| ACE2 | rs2074192 | T | 42.6 |
| ACE2 | rs6632677 | C | 9.2 |
| AGTR1 | rs12721241 | A | 12.0 |
| AGTR1 | rs2675511 | G | 13.9 |
| AGTR2 | rs5193 | T | 15.9 |
| AGTR2 | rs12840631 | G | 18.1 |
| AGTR2 | rs6608590 | T | 41.6 |
| BDKRB2 | rs4900313 | A | 16.2 |
| PGC1β | rs17110586 | G | 14.8 |
| PRC | rs17114388 | G | 19.7 |
Abbreviations: see Table A1.
Table A3.
List of SNPs discarded for analyses because the frequency of the minor allele was inferior to 5%.
| Gene | SNP | MA | MAF |
|---|---|---|---|
| FGF21 | rs838133 | A | 1.1 |
| FGF21 | rs838145 | G | 1.3 |
| FNDC5 | rs726344 | A | 0.2 |
| FST | rs12152850 | T | 1.6 |
| GDF-8 | rs1805086 | C | 0.2 |
| GDF-8 | rs3791784 | G | 2.3 |
| IL-6 | rs1800795 | C | 0.7 |
| IL-15 | rs1589241 | T | 0.8 |
| IL-6 | rs1554606 | T | 1.8 |
| ITLN1 | rs11265509 | T | 4.7 |
Abbreviations: see Table A1.
Table A4.
List of SNPs discarded for analyses because all individuals of the sample had the same genotype.
| Gene | SNP | Genotype |
|---|---|---|
| AGTR1 | rs12721276 | CC |
| PYY | rs432747 | GG |
Abbreviations: see Table A1.
Author Contributions
Conceptualization, Z.H., J.D.C., P.L.V. and A.L.; methodology, Z.H.; formal analysis, Z.H., J.D.C., R.D.-P., and A.L.; assessments G., Z.G., W.G., R.Y.; data curation, Z.H., J.D.C., and A.L.; writing—original draft preparation, Z.H., J.D.C.; writing—review and editing, Z.H., J.D.C., R.D.-P., P.L.V. and A.L.; supervision, A.L.; funding acquisition, Z.H. All authors have read and agreed to the published version of the manuscript.
Funding
This research was funded by key research and development projects of the Ministry of Science and Technology (2018YFF0300402, 2018YFC2000600), China Institute of Sport Science (13-13, 14-08), and projects in the National Science & Technology Pillar Program during the twelfth Five-year Plan Period (2012BAK23B01). P.L.V is supported by University of Alcalá (FPI2016). Research by A.L. is funded by and the Spanish Ministry of Science and Innovation (Fondo de Investigaciones Sanitarias and Fondos FEDER [grant number PI18/00139]) and Fondos FEDER.
Conflicts of Interest
The authors declare no conflict of interest. The funders had no role in the design of the study; in the collection, analyses, or interpretation of data; in the writing of the manuscript, or in the decision to publish the results.
References
- 1.Joyner M.J., Coyle E.F. Endurance exercise performance: The physiology of champions. J. Physiol. 2008;586:35–44. doi: 10.1113/jphysiol.2007.143834. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Fletcher G.F., Landolfo C., Niebauer J., Ozemek C., Arena R., Lavie C.J. Promoting Physical Activity and Exercise: JACC Health Promotion Series. J. Am. Coll. Cardiol. 2018;72:1622–1639. doi: 10.1016/j.jacc.2018.08.2141. [DOI] [PubMed] [Google Scholar]
- 3.Lavie C.J., Ozemek C., Carbone S., Katzmarzyk P.T., Blair S.N. Sedentary Behavior, Exercise, and Cardiovascular Health. Circ. Res. 2019;124:799–815. doi: 10.1161/CIRCRESAHA.118.312669. [DOI] [PubMed] [Google Scholar]
- 4.Lavie C.J., Carbone S., Kachur S., O’keefe E.L., Elagizi A. Effects of Physical Activity, Exercise, and Fitness on Obesity-Related Morbidity and Mortality. Curr. Sports Med. Rep. 2019;18:292–298. doi: 10.1249/JSR.0000000000000623. [DOI] [PubMed] [Google Scholar]
- 5.Harber M.P., Kaminsky L.A., Arena R., Blair S.N., Franklin B.A., Myers J., Ross R. Impact of Cardiorespiratory Fitness on All-Cause and Disease-Specific Mortality: Advances Since 2009. Prog. Cardiovasc. Dis. 2017;60:11–20. doi: 10.1016/j.pcad.2017.03.001. [DOI] [PubMed] [Google Scholar]
- 6.Myers J., Prakash M., Froelicher V., Do D., Partington S., Edwin Atwood J. Exercise capacity and mortality among men referred for exercise testing. N. Engl. J. Med. 2002;346:793–801. doi: 10.1056/NEJMoa011858. [DOI] [PubMed] [Google Scholar]
- 7.Ozemek C., Laddu D.R., Lavie C.J., Claeys H., Kaminsky L.A., Ross R., Wisloff U., Arena R., Blair S.N. An Update on the Role of Cardiorespiratory Fitness, Structured Exercise and Lifestyle Physical Activity in Preventing Cardiovascular Disease and Health Risk. Prog. Cardiovasc. Dis. 2018;61:484–490. doi: 10.1016/j.pcad.2018.11.005. [DOI] [PubMed] [Google Scholar]
- 8.Valenzuela P.L., Maffiuletti N.A., Joyner M.J., Lucia A., Lepers R. Lifelong Endurance Exercise as a Countermeasure Against Age-Related VO2max Decline: Physiological Overview and Insights from Masters Athletes. Sport. Med. 2019:50. doi: 10.1007/s40279-019-01252-0. [DOI] [PubMed] [Google Scholar]
- 9.Ross R., Blair S.N., Arena R., Church T.S., Després J.P., Franklin B.A., Haskell W.L., Kaminsky L.A., Levine B.D., Lavie C.J., et al. Importance of Assessing Cardiorespiratory Fitness in Clinical Practice: A Case for Fitness as a Clinical Vital Sign: A Scientific Statement from the American Heart Association. Circulation. 2016;134:e653–e699. doi: 10.1161/CIR.0000000000000461. [DOI] [PubMed] [Google Scholar]
- 10.Bouchard C., Lesage R., Lortie G., Simoneau J.A., Hamel P., Boulay M.R., Pérusse L., Thériault G., Leblanc C. Aerobic performance in brothers, dizygotic and monozygotic twins. Med. Sci. Sports Exerc. 1986;18:639–646. doi: 10.1249/00005768-198612000-00006. [DOI] [PubMed] [Google Scholar]
- 11.Bouchard C., Warwick Daw E., Rice T., Pérusse L., Gagnon J., Province M.A., Leon A.S., Rao D.C., Skinner J.S., Wilmore J.H. Familial resemblance for VO(2max) in the sedentary state: The HERITAHE family study. Med. Sci. Sports Exerc. 1998;30:252–258. doi: 10.1097/00005768-199802000-00013. [DOI] [PubMed] [Google Scholar]
- 12.Schutte N.M., Nederend I., Hudziak J.J., Bartels M., de Geus E.J.C. Twin-sibling study and meta-analysis on the heritability of maximal oxygen consumption. Physiol. Genomics. 2016;48:210–219. doi: 10.1152/physiolgenomics.00117.2015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Mustelin L., Latvala A., Pietiläinen K.H., Piirilä P., Sovijärvi A.R., Kujala U.M., Rissanen A., Kaprio J. Associations between sports participation, cardiorespiratory fitness, and adiposity in young adult twins. J. Appl. Physiol. 2011;110:681–686. doi: 10.1152/japplphysiol.00753.2010. [DOI] [PubMed] [Google Scholar]
- 14.Bye A., Klevjer M., Ryeng E., da Silva G.J.J., Moreira J.B.N., Stensvold D., Wisløff U. Identification of novel genetic variants associated with cardiorespiratory fitness. Prog. Cardiovasc. Dis. 2020 doi: 10.1016/j.pcad.2020.02.001. [DOI] [PubMed] [Google Scholar]
- 15.Hickson R.C., Bomze H.A., Holloszy J.O. Linear increase in aerobic power induced by a strenuous program of endurance exercise. J. Appl. Physiol. Respir. Environ. Exerc. Physiol. 1977;42:372–376. doi: 10.1152/jappl.1977.42.3.372. [DOI] [PubMed] [Google Scholar]
- 16.Bouchard C., Rankinen T. Individual differences in response to regular physical activity. Med. Sci. Sports Exerc. 2001;33 doi: 10.1097/00005768-200106001-00013. [DOI] [PubMed] [Google Scholar]
- 17.Bouchard C., Sarzynski M.A., Rice T.K., Kraus W.E., Church T.S., Sung Y.J., Rao D.C., Rankinen T. Genomic predictors of the maximal O2 uptake response to standardized exercise training programs. J. Appl. Physiol. 2011;110:1160–1170. doi: 10.1152/japplphysiol.00973.2010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Williams C.J., Williams M.G., Eynon N., Ashton K.J., Little J.P., Wisloff U., Coombes J.S. Genes to predict VO2max trainability: A systematic review. BMC Genomics. 2017;18:831. doi: 10.1186/s12864-017-4192-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Shepherd J.A., Ng B.K., Sommer M.J., Heymsfield S.B. Body composition by DXA. Bone. 2017;104:101–105. doi: 10.1016/j.bone.2017.06.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Borg G. Psychophysical scaling with applications in physical work and the perception of exertion. Scand. J. Work. Environ. Heal. 1990;16:55–58. doi: 10.5271/sjweh.1815. [DOI] [PubMed] [Google Scholar]
- 21.Edvardsen E., Hem E., Anderssen S.A. End criteria for reaching maximal oxygen uptake must be strict and adjusted to sex and age: A cross-sectional study. PLoS ONE. 2014;9:e85276. doi: 10.1371/journal.pone.0085276. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Puthucheary Z., Skipworth J.R.A., Rawal J., Loosemore M., Van Someren K., Montgomery H.E. The ACE gene and human performance: 12 Years on. Sport. Med. 2011;41:433–448. doi: 10.2165/11588720-000000000-00000. [DOI] [PubMed] [Google Scholar]
- 23.Chen Y.Y., Zhang P., Zhou X.M., Liu D., Zhong J.C., Zhang C.J., Jin L.J., Yu H.M. Relationship between genetic variants of ACE2 gene and circulating levels of ACE2 and its metabolites. J. Clin. Pharm. Ther. 2018;43:189–195. doi: 10.1111/jcpt.12625. [DOI] [PubMed] [Google Scholar]
- 24.Wang S., Fu C., Zou Y., Wang H., Shi Y., Xu X., Chen J., Song X., Huan T., Hui R. Polymorphisms of angiotensin-converting enzyme 2 gene associated with magnitude of left ventricular hypertrophy in male patients with hypertrophic cardiomyopathy. Chin. Med. J. (Engl). 2008;121:27–31. doi: 10.1097/00029330-200801010-00006. [DOI] [PubMed] [Google Scholar]
- 25.Yvert T., He Z.-H., Santiago C., Hu Y., Li Y.-C., Gómez-Gallego F., Fiuza-Luces C., Verde Z., Muniesa C.A., Oliván J., et al. Acyl coenzyme A synthetase long-chain 1 (ACSL1) gene polymorphism (rs6552828) and elite endurance athletic status: A replication study. PLoS ONE. 2012;7:e41268. doi: 10.1371/journal.pone.0041268. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Del Coso J., Hiam D., Houweling P., Pérez L.M., Eynon N., Lucía A. More than a ‘speed gene’: ACTN3 R577X genotype, trainability, muscle damage, and the risk for injuries. Eur. J. Appl. Physiol. 2019;119:49–60. doi: 10.1007/s00421-018-4010-0. [DOI] [PubMed] [Google Scholar]
- 27.Del Coso J., Moreno V., Gutiérrez-Hellín J., Baltazar-Martins G., Ruíz-Moreno C., Aguilar-Navarro M., Lara B., Lucía A. ACTN3 R577X genotype and exercise phenotypes in recreational marathon runners. Genes (Basel) 2019;10:413. doi: 10.3390/genes10060413. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Takakura Y., Yoshida T., Yoshioka K., Umekawa T., Kogure A., Toda H., Kagawa K., Fukui S., Yoshikawa T. Angiotensinogen gene polymorphism (Met235Thr) influences visceral obesity and insulin resistance in obese Japanese women. Metabolism. 2006;55:819–824. doi: 10.1016/j.metabol.2006.02.008. [DOI] [PubMed] [Google Scholar]
- 29.Purkait P., Halder K., Thakur S., Ghosh Roy A., Raychaudhuri P., Bhattacharya S., Sarkar B.N., Naidu J.M. Association of angiotensinogen gene SNPs and haplotypes with risk of hypertension in eastern Indian population. Clin. Hypertens. 2017;23:12. doi: 10.1186/s40885-017-0069-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Rico-Sanz J., Rankinen T., Rice T., Leon A.S., Skinner J.S., Wilmore J.H., Rao D.C., Bouchard C. Quantitative trait loci for maximal exercise capacity phenotypes and their responses to training in the HERITAGE Family Study. Physiol. Genomics. 2004;16:256–260. doi: 10.1152/physiolgenomics.00035.2003. [DOI] [PubMed] [Google Scholar]
- 31.Carey R.M., Siragy H.M. Newly recognized components of the renin-angiotensin system: Potential roles in cardiovascular and renal regulation. Endocr. Rev. 2003;24:261–271. doi: 10.1210/er.2003-0001. [DOI] [PubMed] [Google Scholar]
- 32.Dietze G.J., Henriksen E.J. Angiotensin-converting enzyme in skeletal muscle: Sentinel of blood pressure control and glucose homeostasis. J. Renin. Angiotensin. Aldosterone. Syst. 2008;9:75–88. doi: 10.3317/jraas.2008.011. [DOI] [PubMed] [Google Scholar]
- 33.Brull D., Dhamrait S., Myerson S., Erdmann J., Regitz-Zagrosek V., World M., Pennell D., Humphries S.E., Montgomery H. Bradykinin B2BKR receptor polymorphism and left-ventricular growth response. Lancet. 2001;358:1155–1156. doi: 10.1016/S0140-6736(01)06273-0. [DOI] [PubMed] [Google Scholar]
- 34.Kaess B.M., Barnes T.A., Stark K., Charchar F.J., Waterworth D., Song K., Wang W.Y.S., Vollenweider P., Waeber G., Mooser V., et al. FGF21 signalling pathway and metabolic traits—genetic association analysis. Eur. J. Hum. Genet. 2010;18:1344–1348. doi: 10.1038/ejhg.2010.130. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Novelle M.G., Contreras C., Romero-Picó A., López M., Diéguez C. Irisin, two years later. Int. J. Endocrinol. 2013;2013 doi: 10.1155/2013/746281. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Pedersen B.K. A muscular twist on the fate of fat. N. Engl. J. Med. 2012;366:1544–1545. doi: 10.1056/NEJMcibr1201024. [DOI] [PubMed] [Google Scholar]
- 37.Vamvini M.T., Aronis K.N., Panagiotou G., Huh J.Y., Chamberland J.P., Brinkoetter M.T., Petrou M., Christophi C.A., Kales S.N., Christiani D.C., et al. Irisin mRNA and circulating levels in relation to other myokines in healthy and morbidly obese humans. Eur. J. Endocrinol. 2013;169:829–834. doi: 10.1530/EJE-13-0276. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Liu A.L., Xie H.J., Xie H.Y., Liu J., Yin J., Hu J.S., Peng C.Y. Association between fat mass and obesity associated (FTO) gene rs9939609 A/T polymorphism and polycystic ovary syndrome: A systematic review and meta-analysis. BMC Med. Genet. 2017;18:89. doi: 10.1186/s12881-017-0452-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Pan H., Ping X.C., Zhu H.J., Gong F.Y., Dong C.X., Li N.S., Wang L.J., Yang H.B. Association of myostatin gene polymorphisms with obesity in Chinese north Han human subjects. Gene. 2012;494:237–241. doi: 10.1016/j.gene.2011.10.045. [DOI] [PubMed] [Google Scholar]
- 40.Döring F., Onur S., Kürbitz C., Boulay M.R., Pérusse L., Rankinen T., Rauramaa R., Wolfarth B., Bouchard C. Single nucleotide polymorphisms in the myostatin (MSTN) and muscle creatine kinase (CKM) genes are not associated with elite endurance performance. Scand. J. Med. Sci. Sport. 2011;21:841–845. doi: 10.1111/j.1600-0838.2010.01131.x. [DOI] [PubMed] [Google Scholar]
- 41.Harvey N.R., Voisin S., Dunn P.J., Sutherland H., Yan X., Jacques M., Papadimitriou I.D., Haseler L.J., Ashton K.J., Haupt L.M., et al. Genetic variants associated with exercise performance in both moderately trained and highly trained individuals. Mol. Genet. Genomics. 2020;295:515–523. doi: 10.1007/s00438-019-01639-8. [DOI] [PubMed] [Google Scholar]
- 42.Riechman S.E., Balasekaran G., Roth S.M., Ferrell R.E. Association of interleukin-15 protein and interleukin-15 receptor genetic variation with resistance exercise training responses. J. Appl. Physiol. 2004;97:2214–2219. doi: 10.1152/japplphysiol.00491.2004. [DOI] [PubMed] [Google Scholar]
- 43.Nielsen A.R., Mounier R., Plomgaard P., Mortensen O.H., Penkowa M., Speerschneider T., Pilegaard H., Pedersen B.K. Expression of interleukin-15 in human skeletal muscle effect of exercise and muscle fibre type composition. J. Physiol. 2007;584:305–312. doi: 10.1113/jphysiol.2007.139618. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Huang C.-J., Slusher A.L., Whitehurst M., Wells M., Maharaj A., Shibata Y. The impact of acute aerobic exercise on chitinase 3-like protein 1 and intelectin-1 expression in obesity. Exp. Biol. Med. 2016;241:216–221. doi: 10.1177/1535370215602785. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.He Z.-H., Hu Y., Li Y.-C., Gong L.-J., Cieszczyk P., Maciejewska-Karlowska A., Leonska-Duniec A., Muniesa C.A., Marín-Peiro M., Santiago C., et al. PGC-related gene variants and elite endurance athletic status in a Chinese cohort: A functional study. Scand. J. Med. Sci. Sports. 2015;25:184–195. doi: 10.1111/sms.12188. [DOI] [PubMed] [Google Scholar]
- 46.Urano T., Shiraki M., Sasaki N., Ouchi Y., Inoue S. Large-scale analysis reveals a functional single-nucleotide polymorphism in the 5’-flanking region of PRDM16 gene associated with lean body mass. Aging Cell. 2014;13:739–743. doi: 10.1111/acel.12228. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Schubert M.M., Sabapathy S., Leveritt M., Desbrow B. Acute exercise and hormones related to appetite regulation: A meta-analysis. Sports Med. 2014;44:387–403. doi: 10.1007/s40279-013-0120-3. [DOI] [PubMed] [Google Scholar]
- 48.Gu D., Kelly T.N., Hixson J.E., Chen J., Liu D., Chen J., Rao D.C., Mu J., Ma J., Jaquish C.E., et al. Genetic variants in the renin-angiotensin-aldosterone system and salt sensitivity of blood pressure. J. Hypertens. 2010;28:1210–1220. doi: 10.1097/HJH.0b013e3283383655. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Bouchard L., Weisnagel S.J., Engert J.C., Hudson T.J., Bouchard C., Vohl M.C., Pérusse L. Human resistin gene polymorphism is associated with visceral obesity and fasting and oral glucose stimulated C-peptide in the Québec Family Study. J. Endocrinol. Invest. 2004;27:1003–1009. doi: 10.1007/BF03345301. [DOI] [PubMed] [Google Scholar]
- 50.He Z.-H., Hu Y., Li Y.-C., Yvert T., Santiago C., Gómez-Gallego F., Ruiz J.R., Lucia A. Are calcineurin genes associated with athletic status? A function, replication study. Med. Sci. Sports Exerc. 2011;43:1433–1440. doi: 10.1249/MSS.0b013e31820e7f38. [DOI] [PubMed] [Google Scholar]
- 51.Williams A.G., Folland J.P. Similarity of polygenic profiles limits the potential for elite human physical performance. J. Physiol. 2008;586:113–121. doi: 10.1113/jphysiol.2007.141887. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Kodama S., Saito K., Tanaka S., Maki M., Yachi Y., Asumi M., Sugawara A., Totsuka K., Shimano H., Ohashi Y., et al. Cardiorespiratory fitness as a quantitative predictor of all-cause mortality and cardiovascular events in healthy men and women: A meta-analysis. JAMA J. Am. Med. Assoc. 2009;301:2024–2035. doi: 10.1001/jama.2009.681. [DOI] [PubMed] [Google Scholar]
- 53.Strasser B., Burtscher M. Survival of the fittest: VO2max, a key predictor of longevity? Front. Biosci. Landmark. 2018;23:1505–1516. doi: 10.2741/4657. [DOI] [PubMed] [Google Scholar]
- 54.Bouchard C. DNA Sequence Variations Contribute to Variability in Fitness and Trainability. Med. Sci. Sports Exerc. 2019;51:1781–1785. doi: 10.1249/MSS.0000000000001976. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Joyner M.J. Limits to the Evidence that DNA Sequence Differences Contribute to Variability in Fitness and Trainability. Med. Sci. Sports Exerc. 2019;51:1786–1789. doi: 10.1249/MSS.0000000000001977. [DOI] [PubMed] [Google Scholar]
- 56.Barnes J.N., Joyner M.J. Physical activity and cardiovascular risk: 10 metabolic equivalents or bust. Mayo Clin. Proc. 2013;88:1353–1355. doi: 10.1016/j.mayocp.2013.10.015. [DOI] [PubMed] [Google Scholar]
- 57.Baghai T.C., Binder E.B., Schule C., Salyakina D., Eser D., Lucae S., Zwanzger P., Haberger C., Zill P., Ising M., et al. Polymorphisms in the angiotensin-converting enzyme gene are associated with unipolar depression, ACE activity and hypercortisolism. Mol. Psychiatry. 2006;11:1003–1015. doi: 10.1038/sj.mp.4001884. [DOI] [PubMed] [Google Scholar]
- 58.Ma F., Yang Y., Li X., Zhou F., Gao C., Li M., Gao L. The Association of Sport Performance with ACE and ACTN3 Genetic Polymorphisms: A Systematic Review and Meta-Analysis. PLoS ONE. 2013;8:e54685. doi: 10.1371/journal.pone.0054685. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Orysiak J., Zmijewski P., Klusiewicz A., Kaliszewski P., Malczewska-Lenczowska J., Gajewski J., Pokrywka A. The association between ace gene variation and aerobic capacity in winter endurance disciplines. Biol. Sport. 2013;30:249–253. doi: 10.5604/20831862.1077549. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Falahati A., Arazi H. Association of ACE gene polymorphism with cardiovascular determinants of trained and untrained Iranian men. Genes Environ. 2019;41:8. doi: 10.1186/s41021-019-0126-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Day S.H., Gohlke P., Dhamrait S.S., Williams A.G. No correlation between circulating ACE activity and VO2max or mechanical efficiency in women. Eur. J. Appl. Physiol. 2007;99:11–18. doi: 10.1007/s00421-006-0309-3. [DOI] [PubMed] [Google Scholar]
- 62.Qi Y., Niu W., Zhu T., Zhou W., Qiu C. Synergistic effect of the genetic polymorphisms of the renin-angiotensin- aldosterone system on high-altitude pulmonary edema: A study from Qinghai-Tibet altitude. Eur. J. Epidemiol. 2008;23:143–152. doi: 10.1007/s10654-007-9208-0. [DOI] [PubMed] [Google Scholar]
- 63.Jin T., Ren Y., Zhu X., Li X., Ouyang Y., He X., Zhang Z., Zhang Y., Kang L., Yuan D. Angiotensin II Receptor 1 gene variants are associated with high-altitude pulmonary edema risk. Oncotarget. 2016;7:77117–77123. doi: 10.18632/oncotarget.12489. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Morrell N.W., Morris K.G., Stenmark K.R. Role of angiotensin-converting enzyme and angiotensin II in development of hypoxic pulmonary hypertension. Am. J. Physiol. 1995;269:H1186–H1194. doi: 10.1152/ajpheart.1995.269.4.H1186. [DOI] [PubMed] [Google Scholar]
- 65.Mahmood S.S., Pinsky M.R. Heart-lung interactions during mechanical ventilation: The basics. Ann. Transl. Med. 2018;6:349. doi: 10.21037/atm.2018.04.29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.McPherron A.C., Lawler A.M., Lee S.J. Regulation of skeletal muscle mass in mice by a new TGF-β superfamily member. Nature. 1997;387:83–90. doi: 10.1038/387083a0. [DOI] [PubMed] [Google Scholar]
- 67.Mondal H., Mishra S.P. Effect of BMI, Body Fat Percentage and Fat Free Mass on Maximal Oxygen Consumption in Healthy Young Adults. J. Clin. Diagnostic Res. 2017;11:CC17–CC20. doi: 10.7860/JCDR/2017/25465.10039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Miyatani M., Kawano H., Masani K., Gando Y., Yamamoto K., Tanimoto M., Oh T., Usui C., Sanada K., Higuchi M., et al. Required muscle mass for preventing lifestyle-related diseases in Japanese women. BMC Public Health. 2008;8:291. doi: 10.1186/1471-2458-8-291. [DOI] [PMC free article] [PubMed] [Google Scholar]