INTRODUCTION
The Coronavirus Disease 2019 (COVID-19) caused by severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) is currently circulating in the world. Available data have revealed that a significant proportion of patients with COVID-19 present not only with pneumonia but with various gastrointestinal diseases as well. To date, the guidelines for managing pneumonia in patients with COVID-19 have already been established. However, there is currently no guideline or consensus for the management of digestive disorders associated with COVID-19. The Chinese Gastroenterology Expert Group, comprising experts from the gastroenterology units and national medical aid teams of the epidemic region of Wuhan, along with the Chinese Society of Gastroenterology introduce and recommend this management consensus for digestive disorders in patients with COVID-19.
DIGESTIVE MANIFESTATIONS AND PATHOPHYSIOLOGY
COVID-19 commonly occurs in the middle-aged and elderly population. The median ages were 47.0 (1), 55.5 (2), and 56.0 (3) years. Digestive symptoms were present in 16.0% (4), 34.8% (5), 50.5% (6), 56.8% (7), and 61.1% (8) of patients with COVID-19. Diarrhea was a common complaint in 2.0%–49.5% (1–7,9). Other symptoms included anorexia in 15.8%–50.2% (3,4,6,7,9), nausea and/or vomiting in 2.0%–22.7% (1,3–6), and abdominal pain in 0.1%–4.4% (3,4,6,7) of the patients. In some cases, diarrhea was the initial symptom; it may have even occurred before pyrexia (4,6,7). In a cohort of COVID-19 with low severity, 23.3% of patients presented with digestive symptoms alone, whereas 33.5% had both digestive and respiratory symptoms (7). Diarrhea presented initially before respiratory symptoms in 2.9%–6.3% of patients (6,7). Diarrhea was reportedly induced by the antiviral medications Oseltamivir and Arbidol in 55.2% of patients (9). Excluding drug-related diarrhea, this symptom was prevalent in 22.2% of COVID-19 patients (9). Diarrhea often occurred within 1–8 days (median of 3.3 days) after the onset of disease (9) and lasted for 1–14 days (7,9). Bowel movements were as frequent as 18 episodes (median of 4.3 ± 2.2 episodes) per day (7). On admission, 6.9% of patients were found positive for leukocytes or fecal occult blood in the stool analysis (9).
Patients with COVID-19 showed liver injury with an elevated alanine aminotransferase (ALT) level in 5.3%–28.3% (1,2,8,9). Levels of aspartate aminotransferase (AST) and bilirubin were also increased in 4.2%–35.4% and 10.5%–23.2% of COVID-19 patients, respectively (1,2,8,9). In a few individuals, the ALT and AST reached the high levels of 7590 U/L and 1445 U/L (2). Patients with severe COVID-19 were more likely to have higher rates of liver dysfunction (9).
Pathologic findings from the available autopsy and biopsy specimens of patients with COVID-19 showed degeneration, necrosis, and exfoliation of the esophageal, gastric, and intestinal epithelium. Other notable features included hepatomegaly, stem cell degeneration, focal necrosis with neutrophilic infiltration, hepatic sinus congestion, and infiltration of lymphocytes and mononuclear cells into the portal area (10). The exact mechanism of digestive damage associated with COVID-19 remains unknown. Angiotensin-converting enzyme 2 has been identified as a SARS-CoV-2 receptor (11). This enzyme is highly expressed in the lungs, upper esophagus, colon, and cholangiocytes (12,13). Thus, theoretically, digestive organs might also be vulnerable targets of SARS-CoV-2.
MANAGEMENT OF UPPER GASTROINTESTINAL DISORDERS
Anorexia is common, especially in critical COVID-19 patients (3). Nausea and vomiting are often mild and transient. These symptoms may be caused by a gastrointestinal response to the SARS-CoV-2 infection or to antiviral medication. Recommended treatments include fever control, management of drug side effects, liver support, and psychotherapy. Metoclopramide, domperidone, or 5-hydroxytryptamine receptor antagonists can be used for nausea and vomiting.
There are many risk factors that can cause stress-induced gastric mucosal damage in patients with severe COVID-19. These include disease severity, hypoxia, acute respiratory distress syndrome, mechanical ventilation, multiple organ failure, and psychological stress. It has been reported that the incidence of gastrointestinal bleeding in patients with SARS-CoV-2 pneumonia was 4% (14). Theoretically, the incidence of stress-induced gastric mucosal damage should be higher than this rate. Proton pump inhibitors are the preferred options for the prevention of stress gastritis erosion in COVID-19 patients who possess more than one of the aforementioned high-risk factors. In addition, enteral nutrition and mucosal protective agents will benefit the gastrointestinal mucosa.
MANAGEMENT OF DIARRHEA
COVID-19–associated diarrhea is generally mild or moderate and persists for only a short time. Antiviral drug-induced diarrhea often resolves spontaneously without treatment. Frequent diarrhea (>4 times/day) or drug intolerance should be treated by adjusting the dosage of the antiviral agents. There is no specific therapy for the diarrhea caused by SARS-CoV-2. However, dioctahedral montmorillonite and probiotics may be beneficial. Some Lactobacillus probiotics were effective in relieving animal coronavirus-associated diarrhea (15). The effectiveness of these probiotics on human coronavirus-associated diarrhea, however, is still unknown. Probiotic preparations containing Lactobacillus can be used for clinical trials in patients with COVID-19 diarrhea.
Antibiotic-associated diarrhea or Clostridium difficile infection (CDI) may occur in critical COVID-19 patients. Thus, clinicians should be vigilant for both conditions. CDI tests should be performed and probiotics should be given to prevent or control the occurrence of CDI in patients with severe COVID-19.
MANAGEMENT OF LIVER INJURY
Liver injury in patients with COVID-19 may be caused by either systemic inflammation or direct effects of SARS-CoV-2 on the angiotensin-converting enzyme 22 of cholangiocytes (13). Furthermore, a variety of drugs to treat COVID-19 may induce liver injuries. Examples of these are as antivirals (lopinavir, ribavirin), antipyretic analgesics, antibiotics, and herbal products. In most cases with COVID-19, the liver injuries are mild (AST/ALT elevation <2 times the normal value). Dynamic observation without special treatment is warranted for such cases. However, for those with severe (AST/ALT elevation >2 times the normal value) or continuous liver damage, the use of antiviral drugs should be re-evaluated or suspended. Hepatoprotective agents such as glutathione, polyene phosphatidylcholine, and glycyrrhizic acid derivatives may be administered.
OUTPATIENT MANAGEMENT
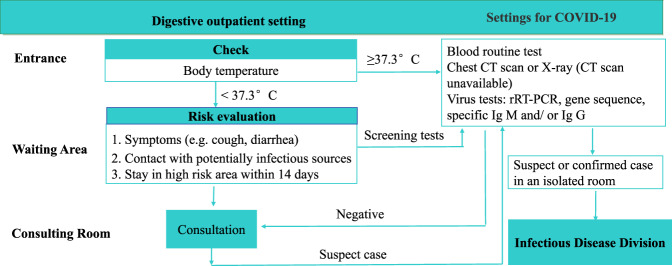
SARS-CoV-2 is primarily transmitted through respiratory droplets or direct contact. Even then, the viral RNA has been detected in stool specimens (7,8). The gastrointestinal fluids or fecal material of patients with COVID-19 are highly risky contaminants. Protective measures must be taken during gastroenterological practice in clinics. Patients with COVID-19 are likely to visit physicians for digestive complaints. A telephone interview is recommended to divert unessential counseling of outpatients and to screen for COVID-19 patients before they arrive at the clinic. In epidemic regions, all patients in the clinics should receive checks for body temperature, assessment for respiratory symptoms, and questioning for travel and contact history. Based on these preliminary screening measures, outpatients can be stratified according to different risk levels. A confirmed or suspected case needs to be treated in an isolated room or transferred to an infectious disease division (Figure 1).
Figure 1.
Workflow of digestive outpatient setting during SARS-CoV-2 epidemic. SARS-CoV-2, severe acute respiratory syndrome coronavirus 2.
DIGESTIVE PROCEDURES
To prevent or control the transmission of SARS-CoV-2 in epidemic communities, gastroenterological procedures such as esophageal pH test, gastrointestinal motility, hydrogen breath test, fecal microbiota transplantation, Helicobacter pylori breath test, and stool antigen detection are recommended for suspension or postponement until the epidemic is under control.
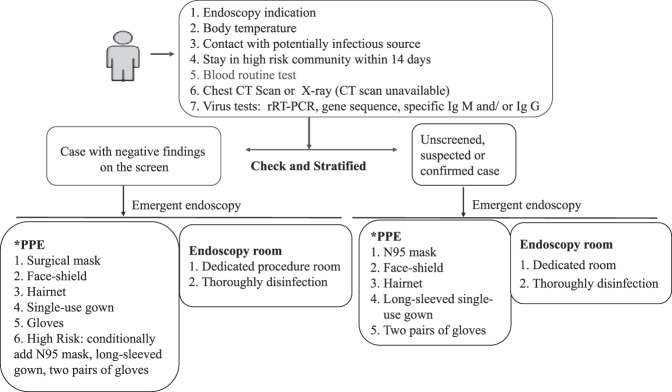
Digestive endoscopy is regarded as a risky procedure because of the potential contact or air transmission. It is recommended to cancel or postpone all elective procedures in communities with an ongoing transmission. Emergent endoscopy, whenever indicated for acute gastrointestinal massive hemorrhage, removal of foreign bodies in the gastrointestinal tract, infectious cholangitis, and biliary pancreatitis, should be available. The screening of COVID-19 should be undertaken before digestive endoscopy is performed in communities with an ongoing transmission. The screening measures include temperature checks, laboratory testing, and lung CT scanning. If necessary and available, SARS-CoV-2 nucleic acid or specific antibody detection must also be performed (Figure 2). Carbon dioxide insufflation during endoscopy is conditionally recommended to reduce gastrointestinal tract distention and gas water splash. This may be potentially helpful in lessening contamination from the gut.
Figure 2.
Risk stratification and PPE for endoscopy procedure during SARS-CoV-2 epidemic. *PPE, Personal protect equipment; SARS-CoV-2, severe acute respiratory syndrome coronavirus 2.
Capsule or disposable endoscopies are recommended as the preferred options for patients with emergent endoscopy indications in epidemic regions because of less contamination.
SUMMARY
Although patients with COVID-19 mainly present with pneumonia, they may also have various digestive symptoms. In fact, some patients initially present with digestive symptoms, whereas others manifest with gastrointestinal symptoms alone. Management revolving around symptomatic and protective treatments are recommended for digestive disorders associated with COVID-19. SARS-CoV-2 is transmitted primarily through respiratory droplets and close contact. Gastrointestinal fluids and fecal material from patients with COVID-19 may contain live viruses. Thus, these are considered highly risky contaminants. Protective flow and measures have been suggested in gastroenterological practice to reduce the transmission. Elective gastrointestinal procedures are recommended for suspension or postponement. Emergent endoscopy, on the other hand, should be available. Implementers are suggested to wear personal protective equipment according to the high-risk standards during operation.
Because SARS-CoV-2 is an emerging infection, most reports on COVID-19 are fairly recent. Many aspects including the pathogenicity to the digestive organs, clearance of the viruses from the digestive tract, specific detection modalities, and specific therapies for digestive disorders associated with COVID-19 remain unclear. Further research and updated management in gastroenterology are needed to effectively control the COVID-19 pandemic.
CONFLICTS OF INTEREST
Guarantor of the article: Yunsheng Yang, MD, and Chengwei Tang, MD.
Specific author contributions: Y.Y. was responsible for the idea, outlined and prepared the initial and final drafts of the manuscript. All authors were involved in drafting or critically revising the manuscript. All authors approved the final draft submitted.
Financial support: None to report.
Potential competing interests: None to report.
Ethics: None to report.
ACKNOWLEDGMENTS
We would like to extend our sincere gratitude to Chinese Gastroenterology Expert Group Against COVID-19. The experts in alphabetical order are Bin Lv, Dongfeng Chen, Jingnan Li, Jingyuan Fang, Jiyao Wang, Junping Wang, Liya Zhou, Lu Xia, Nonghua Lv, Rui Li, Shiming Yang, Wei Lu, Weifen Xie, Weiguo Dong, Xin Wang, Yanqing Li, Ye Chen, Yongquan Shi, Yu Lan, Yulan Liu and Zhen Ding. For English language editing, we would like to thank Ms. Yan Zhang and Mr Peter Chiang in the drafting and Editage (www.editage.com) in the final revision.
REFERENCES
- 1.Guan WJ, Ni ZY, Hu Y, et al. Clinical characteristics of coronavirus disease 2019 in China. N Engl J Med 2020;382(18):1708–20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Chen N, Zhou M, Dong X, et al. Epidemiological and clinical characteristics of 99 cases of 2019 novel coronavirus pneumonia in Wuhan, China: A descriptive study. Lancet 2020;395(10223):507–13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Wang D, Hu B, Hu C, et al. Clinical characteristics of 138 hospitalized patients with 2019 novel coronavirus-infected pneumonia in Wuhan, China. JAMA 2020;323(11):1061–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Luo S, Zhang X, Xu H. Don't overlook digestive symptoms in patients with 2019 novel coronavirus disease (COVID-19). Clin Gastroenterol Hepatol 2020. doi: 10.1016/j.cgh.2020.03.043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Nobel YR, Phipps M, Zucker J, et al. Gastrointestinal symptoms and COVID-19: Case-control study from the United States. Gastroenterology 2020. doi: 10.1053/j.gastro.2020.04.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Pan L, Mu M, Yang P, et al. Clinical characteristics of COVID-19 patients with digestive symptoms in Hubei, China: A descriptive, cross-sectional, multicenter study. Am J Gastroenterol 2020;115(5):766–73. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Han C, Duan C, Zhang S, et al. Digestive symptoms in COVID-19 patients with mild disease severity: Clinical presentation, stool viral RNA testing, and outcomes. Am J Gastroenterol 2020. doi: 10.14309/ajg.0000000000000664. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Lin L, Jiang X, Zhang Z, et al. Gastrointestinal symptoms of 95 cases with SARS-CoV-2 infection. Gut 2020;69(6):997–1001. [DOI] [PubMed] [Google Scholar]
- 9.Fang D, Ma JD, Guan JL, et al. Manifestations of digestive system in hospitalized patients with novel coronavirus pneumonia in Wuhan, China: A single-center, descriptive study. Chin J Dig 2020;40(3):151–6. [Google Scholar]
- 10.Liu X, Wang RS, Qu GQ, et al. Autopsy report of a dead patient with novel coronavirus pneumonia (COVID-19). J Forensic Med 2020;36(1):21–3. [Google Scholar]
- 11.Lu R, Zhao X, Li J, et al. Genomic characterisation and epidemiology of 2019 novel coronavirus: Implications for virus origins and receptor binding. Lancet 2020;395(10224):565–74. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Zhang H, Kang Z, Gong H, et al. The digestive system is a potential route of SARS-CoV-2 infection: A bioinformatics analysis based on single-cell transcriptomes. bioRxiv 2020. doi: 10.1101/2020.01.30.927806. [DOI] [Google Scholar]
- 13.Chai XQ, Hu LF, Zhang Y, et al. Specific ACE2 expression in cholangiocytes may cause liver damage after SARS-CoV-2 infection. bioRxiv 2020. doi: 10.1101/2020.02.03.931766. [DOI] [Google Scholar]
- 14.Yang X, Yu Y, Xu J, et al. Clinical course and outcomes of critically ill patients with SARS-CoV-2 pneumonia in Wuhan, China: A single-centered, retrospective, observational study. Lancet Respir Med 2020;8(5):475–81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Kumar R, Seo BJ, Mun MR, et al. Putative probiotic Lactobacillus spp. from porcine gastrointestinal tract inhibit transmissible gastroenteritis coronavirus and enteric bacterial pathogens. Trop Anim Health Prod 2010;42(8):1855–60. [DOI] [PMC free article] [PubMed] [Google Scholar]