Abstract
Background:
In response to COVID-19, American medical centers have enacted elective case restrictions, markedly affecting the training of orthopaedic residents. Residencies must develop new strategies to provide patient care while ensuring the health and continued education of trainees. We aimed to describe the evolving impact of COVID-19 on orthopaedic surgery residents.
Methods:
We surveyed five Accreditation Council for Graduate Medical Education-accredited orthopaedic residency programs within cities highly affected by the COVID-19 pandemic about clinical and curricular changes. An online questionnaire surveyed individual resident experiences related to COVID-19.
Results:
One hundred twenty-one resident survey responses were collected. Sixty-five percent of the respondents have cared for a COVID-19-positive patient. One in three reported being unable to obtain institutionally recommended personal protective equipment during routine clinical work. All programs have discontinued elective orthopaedic cases and restructured resident rotations. Most have shifted schedules to periods of active clinical duty followed by periods of remote work and self-isolation. Didactic education has continued via videoconferencing.
Discussion:
COVID-19 has caused unprecedented changes to orthopaedic training; however, residents remain on the front lines of inpatient care. Exposures to COVID-19 are prevalent and residents have fallen ill. Programs currently use a variety of strategies to provide essential orthopaedic care. We recommend continued prioritization of resident safety and necessary training accommodations.
Cases of the viral illness COVID-19 first emerged from Wuhan, China, in December 2019.1 On March 11, 2020, the World Health Organization declared the COVID-19 virus a pandemic.2 The United States now leads in the number of diagnosed cases.3 In response to this health crisis, medical centers across the country have instituted major policy changes to meet growing patient volume, slow disease transmission, and protect healthcare workers from infection. These policies include suspension of elective cases and reduced outpatient visits, which have markedly affected all surgical specialties, including orthopaedic surgery.4 The COVID-19 crisis has had unprecedented consequences to not only surgeons and patients but also orthopaedic surgery trainees.
There are over 3,500 orthopaedic surgery residents in 171 programs across the country.5,6 Most orthopaedic residencies are associated with level 1 or 2 trauma centers. Residents are crucially responsible 24/7 as firstline responders to manage acute traumatic injuries and evaluate musculoskeletal reports in the emergency department. They also provide inpatient care for perioperative orthopaedic patients. However, the operating room is the keystone of orthopaedic residency training, where residents both provide valuable assistance and gain necessary skills for future practice.
In response to institutional changes, orthopaedic programs have restructured resident work schedules and transitioned to web-based didactics. Many clinical strategies are aimed at decreasing viral transmission by dividing residents into insulated teams and limiting unnecessary exposure. Nevertheless, as residents continue to perform essential patient care during the evolving COVID-19 crisis, they will undoubtedly face both daily challenges to personal health and longer term questions about their training experience.
Currently, epicenters of COVID-19 in the United States include New York, Los Angeles, Seattle, and New Orleans.3 Many orthopaedic residencies are part of tertiary medical centers at the front lines of the pandemic in these metropolitan areas. Despite similar challenges facing all residencies, information and resource sharing between programs have been limited. We aimed to describe the experiences of residents and the strategies of several orthopaedic residency programs within COVID-19 epicenters to promote continued safety, education, and quality patient care.
Methods
As of April 2, 2020, the leading epicenters of COVID-19 in the United States are New York City (52,948 cases), Los Angeles County (4,045 cases), New Orleans (3,476 cases), and Seattle-King County (2,787 cases).3 Five Accreditation Council for Graduate Medical Education (ACGME)-accredited orthopaedic residency programs associated with tertiary medical centers in each of the abovementioned cities were identified and surveyed. Programs included Hospital for Special Surgery (HSS) in New York City, NY; University of Washington in Seattle, WA; Tulane University in New Orleans, LA; and University of California-Los Angeles (UCLA) and Cedars-Sinai in Los Angeles, CA.
One resident member of each program was asked to describe any clinical structure changes in response to COVID-19, including the number of clinically active residents, sites, specific responsibilities, and details related to the ongoing orthopaedic cases. A summary of educational curriculum included the types and frequency of didactics and supplemental resources. Health and wellness of the residency detailed cases of confirmed or suspected COVID-19 infection among residents, testing, self-isolation protocols, and available resources for mental health. All descriptions reflect official policies in place as of April 2, unless otherwise specified. A 12-item electronic survey related to resident experiences with COVID-19 exposure, testing, and safety was administered to trainees at each participating program.
Results
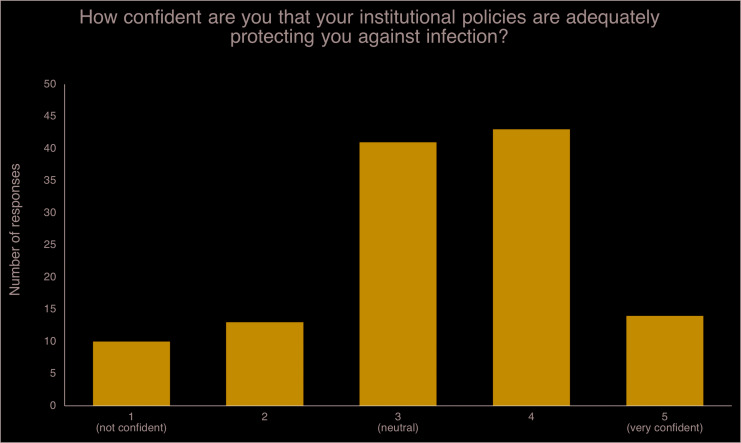
The resident survey response rate was 82% (121 of 148). Of 115 who reported active clinical duties since the pandemic policy changes, 65% have had clinical contact with and 29% have operated on a COVID-19-positive patient, respectively. Most trainees have received training on the proper use of personal protective equipment (PPE) via in-person sessions (52.5%) or electronic materials (26.7%). Despite this, 35% of residents reported experiencing situations in which they were unable to access institutionally recommended PPE necessary for patient care. Testing protocols for COVID-19 vary, with 74% of residents able to obtain testing if exhibiting symptoms, but only 14% were able to obtain testing for the history of high-risk exposure. Of the programs surveyed, only HSS in NYC has tasked residents to nonorthopaedic care of patients with COVID-19, but contingency plans also exist at other programs. On a 1 to 5 scale (5 = very confident), residents reported an average score of 3.3 (SD 1.1), representing neutral confidence that their institutional policies adequately protect them from disease transmission (Figure 1). Twenty percent of residents surveyed are using mental health resources to support their well-being.
Figure 1.
Chart illustrating the resident survey responses to “How confident are you that your institutional policies are adequately protecting you against infection?” N = 121, mean (SD) rating 3.3 (1.1).
Table 1 describes the demographic characteristics and COVID-19-related policies at participating institutions. Among all programs, primary indications for ongoing orthopaedic cases included acute traumatic fractures, infections, and musculoskeletal tumors. In the case that a resident had a positive COVID-19 polymerase chain reaction (PCR) test, all institutions required a minimum of 7 days of self-isolation and 72 hours without symptoms before returning to work. Symptomatic residents with a negative test were allowed to return to work within 24 hours of improving symptoms.
Table 1.
Demographic Characteristics and COVID-19-related Data From Five Metropolitan Orthopaedic Residency Programs
| Factors | Hospital for Special Surgery | University of Washington | Cedar-Sinai | UCLA | Tulane University |
| New York City, NY | Seattle, WA | Los Angeles, CA | Los Angeles, CA | New Orleans, LA | |
| No. of residents total (per class) | 45 (9) | 39 (8) | 20 (4) | 29 (6) | 15 (3) |
| No. of attending faculty | >130 | 55 | 41 | 34 | 17 |
| Hospital sites (institutions in italics do not have continued resident coverage) | HSS NYP Cornell* NYP Queens* VA Memorial Sloan Kettering Cancer Center | Harborview Medical Center* UWashington Medical Center Seattle Children's Hospital UWashington Medical Center-Northwest VA | Cedars-Sinai Medical Center* Children's Hospital of Los Angeles Kerlan-Jobe Institute Shriner's Hospital for Children | Ronald Reagan Hospital* UCLA Santa Monica VA Olive View Medical Center Orthopaedic Institute for Children | University Medical Center of New Orleans* Tulane Medical Center VA Lakeside Hospital East Jefferson West Jefferson New Orleans Children's Hospital |
| Institution-wide suspension of elective cases | March 16, 17 | March 16 | March 17 | March 17 | March 10 |
| Implementation of residency program changes | March 17, Reassignment April 4b | March 23 | March 17 | March 17 | March 10 |
| Residents involved in clinics? | No | Yes | No | No | Yes—trauma clinic only |
| Availability of COVID-19 testing for residents? Type of testing |
Yes, if symptomatic PCR |
Yes, if symptomatic PCR |
Yes, if symptomaticc PCR |
Yes, if symptomatic PCR |
Yes, if symptomatic PCR |
| Residents suspended from clinical duty with suspected or diagnosed COVID-19 | Yes, 6 suspected, 5 confirmed | Yes, 4 suspected, negative testing | Yes, 1 suspected, negative testing | Yes, 1 suspected, negative testing | Yes, 1 suspected, negative testing |
PCR = polymerase chain reaction
Level 1 trauma center.
Reassignment of residents occurring after the Accreditation Council for Graduate Medical Education Pandemic Status III Declaration.
Testing not initially available, mandated self-quarantine protocol if symptomatic.
VA = Veteran's affairs; UCLA = University of California-Los Angeles
Hospital for Special Surgery (HSS) (New York, NY)
Clinical Structure
A COVID-19 leadership group was established with representatives from each class to facilitate communication and logistics. From March 17 to April 4, teams of 12 and 16 residents covered acute inpatient care for each of the level 1 trauma centers, with smaller teams dedicated to other hospital sites for essential cases and orthopaedic inpatient care. No residents participated in outpatient clinics. After the declaration of the ACGME Stage 3 Pandemic Emergency Status, all core competencies were suspended. Starting April 4, 22 residents were reassigned to caring for critical patients with COVID-19 in intensive care (ICU) settings. For both phases of program restructuring, each resident team remained insulated from others and alternated between 1 week on-service and 1 week of self-isolation.
Education
Attending-led didactics from each orthopaedic subspecialty offered 1 to 5 hours weekly of educational material for residents and fellows via videoconferencing. Residents were also encouraged to continue self-directed learning via the HSS eAcademy, a database of video-based lectures.
Health and Wellness
As of April 2, at least six residents tested positive or were presumed positive for COVID-19. These residents were self-quarantined for a minimum 1 week. Residents were allowed to return to work after 72 hours without symptoms but were required to wear a face mask for 2 weeks. All healthcare providers were required to wear a surgical mask in regular patient encounters. Daily wellness communications were provided by the residency program, with content such as home physical and meditation exercises. Residents were also able access to confidential counseling with the hospital psychologist and infectious disease/internal medicine consultation if needed.
University of Washington (Seattle, WA)
Clinical Structure
At University of Washington Medical Center, residents remained fully involved in both surgical cases and clinics. The trauma service of 12 residents was largely maintained to manage the high volume of essential cases averaging 6 per day. However, clinical time was decreased by alternating on and off days for each resident. An alternate-week system was implemented for hand surgery, the pediatric service, and Veteran's Affairs (VA) service. The spine service was unchanged because of the consistent volume of spine trauma. Eleven residents on elective services were assigned to 1 week on and 2 weeks off to cover call cases at the remaining hospitals. Residents not on clinical duty were available as backup if a working resident fell ill. Although not yet implemented, contingency plans are in place to assign orthopaedic residents to frontline COVID-19 teams in anticipation of a surge in patients.
Educational Curriculum
Previously, the didactic curriculum involved a weekly all-resident conference, with additional conferences and journal clubs at each hospital site. Since March 6, conferences and journal clubs have continued via videoconferencing at their usual times at all sites, allowing all residents to take part in education previously limited by location.
Health and Wellness
There have been no diagnosed cases of COVID-19 reported within the residency. At least four residents developed flulike symptoms and were temporarily suspended from duty until test results returned negative. Free wellness services are provided through the University of Washington.
Tulane University (New Orleans, LA)
Clinical Structure
Orthopaedic administrators and residents came together in advance of institutional changes to develop a COVID-19 strategy. The residency was organized into two 7-person teams, each assigned to clinical duties for one week followed by 1 week of self-isolation. One resident was assigned to the pediatric hospital. Cross coverage between hospitals was minimized. All consults not requiring a reduction or acute management were discussed with the chief resident on call to decide if an in-person consult was required. Resident clinic coverage was limited to the trauma clinic to manage only preoperative and postoperative patients with time-sensitive issues.
Educational Curriculum
Since March 3, all morning fracture conferences and weekly grand rounds have moved online using Zoom videoconferencing. Other activities include weekly resident team conference calls and faculty-led journal clubs for a total of 7 hours per week, supplemented by online resources and self-study. Grand rounds were adapted into a forum discussing appropriate patient management during the pandemic.
Health and Wellness
There has been one suspected case of COVID-19 reported among the residency group, with eventual negative test results. Residents receive daily updates on COVID-19 case counts and the status of hospital resources. Tulane Medical Center offers virtual mental health support programs and hot meals for providers.
University of California-Los Angeles (UCLA) (Los Angeles, CA)
Clinical Structure
The residency transitioned to a rotating schedule composed of two teams that alternated between 2 weeks of clinical duty and 2 weeks of self-isolation. Cross-coverage between different hospital sites was restricted. Each clinical site was assigned residents according to expected surgical volume. Resident duties have been limited to emergency department consults, inpatient care, and surgical cases only, without coverage of outpatient clinics. Case volume has averaged 3 to 4 cases per day at the level 1 and level 2 trauma centers.
Educational Curriculum
Starting March 10, in-person lectures were replaced by twice daily (am and pm) faculty-led educational conferences from Monday to Thursday and journal club each Friday via Zoom videoconferencing. Instructional time totaled 9 hours per week.
Health and Wellness
There have been no cases of COVID-19 reported among the residency. One resident developed respiratory symptoms and received a negative COVID-19 PCR test result within 12 hours. UCLA offers professional mental health services to all residents via videoconferencing. Free childcare and pet-sitting for residents have been provided by student volunteers and private organizations.
Cedars-Sinai (Los Angeles, CA)
Clinical Structure
The resident body was organized into four 4-person teams, each assigned to clinical duties at the primary level 1 trauma center for four consecutive days, followed by 12 days of “remote work.” The goal of this strategy was to prophylactically isolate residents during the early infectious period if an inadvertent COVID-19 exposure were to occur. Two to 5 cases were performed per day.
Educational Curriculum
Daily in-person fracture conference was held between the on-service resident team and on-call attending. A new didactic schedule was instituted, consisting of 14 hours per week of attending-led lectures via teleconference and required daily in-training study questions. A weekly hour-long conference is dedicated to briefing the residency on new policy changes.
Health and Wellness
There have been no diagnosed cases of COVID-19 reported within the residency. One resident developed symptoms, but testing proved negative. Up until March 27, without adequate testing available, 7-day self-quarantine was default for symptomatic individuals. Subsequently, rapid PCR testing has become available. Cedars-Sinai offers a professional wellness service with eight sessions of free counseling available.
Discussion
As a World Health Organization-designated pandemic, the COVID-19 crisis has prompted 38 American states to implement stay-at-home policies in efforts to slow transmission.2,7,8 With the same goal, tertiary medical centers within highly affected metropolitan cities suspended elective surgical procedures in mid-March.9,10 This policy profoundly affected orthopaedic surgery which features high volumes of elective cases. Although surgeons in the United States are still adjusting to these changes, Chang Liang et al11 reported on the Singapore experience, which advocated for orthopaedic surgeons to step up as role models in health safety and to adopt innovative uses of technology for patient care and medical education. The impact of COVID-19 on orthopaedic surgery residency training in the United States has been tremendous yet difficult to quantify. With little guidance, residency programs have been challenged with developing independent strategies to continue delivering quality patient care and medical education while protecting the health of their trainees.
In metropolitan outbreak centers of New York, Seattle, Los Angeles, and New Orleans, residency structures have changed dramatically. Residents were divided into insulated teams focused on acute inpatient orthopaedic care and essential cases including acute fractures, infections, and tumors. Most programs eliminated resident involvement in outpatient clinics. Resident teams spent 4 to 14 days on clinical duties before self-isolating for 7 to 14 days. One program required every other day inpatient coverage to satisfy patient volumes. Epidemiologic evidence suggests that the viral incubation period is 3 to 9 days and viral shedding is the highest in the early infection period, occurring at or before the onset of symptoms.12 The duration of clinical duties may best be guided on these estimates, although the number of clinical sites and available residents pose practical limitations.
Residents of all specialties, including those in orthopaedics, are on the front lines of treating patients during this crisis. Despite reduced case volumes, the demand for orthopaedic inpatient care continues. Our survey yielded a strong response rate of 82%. Residents indicated that clinical exposure to patients with COVID-19 in the workplace was high. PPE protocols among institutions differ; however, 35% of residents encountered situations in which the recommended PPE was not available. Residents also expressed limited confidence that their institutional policies were providing adequate protection from infection. As this disease becomes more prevalent and hospitalizations increase, it is crucial that appropriate PPE is accessible and properly used in every clinical situation. Close communication between residents, program directors, and hospital administrators may help promote confidence that provider safety is a top priority.
New York City is the most severely affected metropolitan area by the pandemic. Thus far, 6 of 45 orthopaedic residents at HSS have been ill and restricted from work duties. Owing to the overwhelming volumes, HSS has declared ACGME Pandemic Stage III.13 This declaration suspends all educational requirements in an effort to make residents and fellows available for clinical care. Orthopaedic residents are now reassigned to nonorthopaedic clinical duties including intensive care of COVID-19-positive patients. Programs in the other metropolitan areas surveyed have not experienced emergency reassignment but should be prepared for this possibility if patient volumes surge.
The educational component of residency has largely transitioned to a digital format. Limited surgical volume has led to more opportunities for didactic instruction.14 The ACGME and American Board of Orthopaedic Surgery have issued statements acknowledging the extreme pandemic circumstances but have not made any specific policy changes.13,15-17 Minimum rotation and case requirements exist to standardize training; however, the ACGME leaves the ultimate decision of resident graduation to each program director. Therefore, programs have the flexibility to adapt residents' training to encourage on-time graduation. The American Board of Orthopaedic Surgery dictates that academic leave cannot exceed 6 weeks per year averaged over five years. For a typical program with 4 weeks of vacation per year, time off secondary to COVID-19 can be up to 10 weeks.
This study is limited by the rapidly evolving clinical situation and changing policies. We attempted to provide a glimpse of early strategies, approximately 3 weeks into institutional cancellation of elective cases. Standardized guidelines are limited, but as more evidence emerges, institutions should readily review and update their policies. Regarding residency training, it is difficult to quantify the educational opportunities lost and impossible to predict how long circumstances may persist. Although there is marked reduction in surgical volumes, programs are all increasing didactics and digital education. In addition, these experiences only depict a handful of residency programs but are by no means unique. In particular, the overwhelming case volume in New York is a scenario for which other regions must be prepared. The select programs represented here vary considerably in class size, number of clinical sites, and case volume. Their response strategies may provide valuable insight for other programs.
Orthopaedic residency training continues amidst the evolving pandemic. Residents remain active in inpatient duties at tertiary centers that currently face the greatest burden of patients with COVID-19 care around the country. Programs have responded by limiting resident time within the hospital and implementing schedules that allow for self-isolation, but exposures are inevitable. It is critical that residents have access to appropriate PPE and up-to-date information. All residency programs should maintain open communication and remain flexible in an ever-changing environment. Orthopaedic education has successfully continued with rapid adoption of digital technologies, but the consequences of lost surgical experiences remain unclear. In the end, this generation of residents will be uniquely trained not only as orthopaedic surgeons but also as doctors who contributed to the fight against COVID-19.
Footnotes
None of the following authors or any immediate family member has received anything of value from or has stock or stock options held in a commercial company or institution related directly or indirectly to the subject of this article: Dr. An, Dr. Igboechi, Dr. Wang, Dr. Yerrapragada, Dr. Lin, and Dr. Paiement.
References
- References printed in bold type are those published within the past 5 years.
- 1.Wu Z, McGoogan JM: Characteristics of and important lessons from the coronavirus disease 2019 (COVID-19) outbreak in China: Summary of a report of 72314 cases from the Chinese center for disease control and prevention. JAMA 2020;323:1239-1242. [DOI] [PubMed] [Google Scholar]
- 2.World Health Organization: WHO Director-General's Opening Remarks at the Media Briefing on COVID-19-11 March 2020. Available at: https://www.who.int/dg/speeches/detail/who-director-general-s-opening-remarks-at-the-media-briefing-on-covid-19---11-march-2020. Accessed April 7, 2020. [Google Scholar]
- 3.Johns Hopkins University: Coronavirus COVID-19 Global Cases by the Center for Systems Science and Engineering (CSSE) at Johns Hopkins University (JHU). Available at: https://coronavirus.jhu.edu. Accessed April 6, 2020. [Google Scholar]
- 4.Centers for Medicare and Medicaid Services: Non-emergent, Elective Medical Services, and Treatment recommendations. Available at: https://www.cms.gov/files/document/31820-cms-adult-elective-surgery-and-procedures-recommendations.pdf. Accessed March 30, 2020 [Google Scholar]
- 5.Trikha R, Keswani A, Ishmael CR, Greig D, Kelley BV, Bernthal NM: Current trends in orthopaedic surgery residency applications and match rates. J Bone Joint Surg Am 2020;102:e24. [DOI] [PubMed] [Google Scholar]
- 6.Nasreddine AY, Gallo R: Applying to orthopaedic residency and matching rates: Analysis and review of the past 25 years. J Bone Joint Surg Am 2019;101:e134. [DOI] [PubMed] [Google Scholar]
- 7.State of California: Executive Order N-33-20. Available at: https://www.gov.ca.gov/wp-content/uploads/2020/03/3.19.20-attested-EO-N-33-20-COVID-19-HEALTH-ORDER.pdf. Accessed April 7, 2020. [Google Scholar]
- 8.New York State: Novel Coronavirus. Available at: https://coronavirus.health.ny.gov/. Accessed April 7, 2020. [Google Scholar]
- 9.NYP: CORONAVIRUS (COVID-19): WHAT TO KNOW. Available at: https://www.nyp.org/coronavirus-information. Accessed April 7, 2020. [Google Scholar]
- 10.HSS: HSS Suspends Nonessential Onsite Care. Available at: https://www.hss.edu/essential-surgeries-and-care.asp. Accessed April 7, 2020. [Google Scholar]
- 11.Chang Liang Z, Wang W, Murphy D, Po Hui JH: Novel coronavirus and orthopaedic surgery. J Bone Joint Surg 2020;1:1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Lauer SA, Grantz KH, Bi Q, et al. : The incubation period of coronavirus disease 2019 (COVID-19) from publicly reported confirmed cases: Estimation and application. Ann Intern Med 2020. doi: 10.7326/M20-0504. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.ACGME: ACGME Response to Pandemic Crisis. Available at: https://acgme.org/covid-19. Published 2020. Accessed March 30, 2020. [Google Scholar]
- 14.Stella JJ, Lamb DL, Stain SC, Termuhlen PM: Understanding ACGME scholarly activity requirements for general surgery programs in the era of single accreditation and the next accreditation system. Am Surg 2018;84:e40-43. [PubMed] [Google Scholar]
- 15.ACGME: ACGME Statement on Early Graduation from US Medical Schools and Early Appointment to the Clinical Learning Environment. Available at: https://www.acgme.org/Newsroom/Newsroom-Details/ArticleID/10184/ACGME-Statement-on-Early-Graduation-from-US-Medical-Schools-and-Early-Appointment-to-the-Clinical-Learning-Environment. Published 2020. Accessed March 30, 2020. [Google Scholar]
- 16.ACGME: ACGME Response to the Coronavirus. Available at: https://acgme.org/Newsroom/Newsroom-Details/ArticleID/10111/ACGME-Response-to-the-Coronavirus-COVID-19. Accessed March 18, 2020. [Google Scholar]
- 17.ABOS: ABOS Statements on Coronavirus (3/25/20). Available at: https://www.abos.org/2194-2/. Accessed April 6, 2020. [Google Scholar]