Abstract
BACKGROUND:
The cellular immune system is of pivotal importance with regard to the response to severe infections. Monocytes/macrophages are considered key immune cells in infections and downregulation of the surface expression of monocytic human leukocyte antigen-DR (mHLA-DR) within the major histocompatibility complex class II reflects a state of immunosuppression, also referred to as injury-associated immunosuppression. As the role of immunosuppression in coronavirus disease 2019 (COVID-19) is currently unclear, we seek to explore the level of mHLA-DR expression in COVID-19 patients.
METHODS:
In a preliminary prospective monocentric observational study, 16 COVID-19–positive patients (75% male, median age: 68 [interquartile range 59–75]) requiring hospitalization were included. The median Acute Physiology and Chronic Health Evaluation-II (APACHE-II) score in 9 intensive care unit (ICU) patients with acute respiratory failure was 30 (interquartile range 25–32). Standardized quantitative assessment of HLA-DR on monocytes (cluster of differentiation 14+ cells) was performed using calibrated flow cytometry at baseline (ICU/hospital admission) and at days 3 and 5 after ICU admission. Baseline data were compared to hospitalized noncritically ill COVID-19 patients.
RESULTS:
While normal mHLA-DR expression was observed in all hospitalized noncritically ill patients (n = 7), 89% (8 of 9) critically ill patients with COVID-19–induced acute respiratory failure showed signs of downregulation of mHLA-DR at ICU admission. mHLA-DR expression at admission was significantly lower in critically ill patients (median, [quartiles]: 9280 antibodies/cell [6114, 16,567]) as compared to the noncritically ill patients (30,900 antibodies/cell [26,777, 52,251]), with a median difference of 21,508 antibodies/cell (95% confidence interval [CI], 14,118–42,971), P = .002. Reduced mHLA-DR expression was observed to persist until day 5 after ICU admission.
CONCLUSIONS:
When compared to noncritically ill hospitalized COVID-19 patients, ICU patients with severe COVID-19 disease showed reduced mHLA-DR expression on circulating CD14+ monocytes at ICU admission, indicating a dysfunctional immune response. This immunosuppressive (monocytic) phenotype remained unchanged over the ensuing days after ICU admission. Strategies aiming for immunomodulation in this population of critically ill patients should be guided by an immune-monitoring program in an effort to determine who might benefit best from a given immunological intervention.
See Article, p 989
KEY POINTS.
Question: Is severe coronavirus disease 2019 (COVID-19) associated with an immunosuppressive phenotype of key innate immune cells?
Findings: We observed considerable reduction of monocytic human leukocyte antigen-DR (mHLA-DR), a key marker of monocytic immune function, in critically ill COVID-19 patients with acute respiratory failure and this effect remained unchanged over the first days on the intensive care unit (ICU).
Meaning: Severe COVID-19 disease is associated with reduced human leukocyte antigen (HLA-DR) expression on circulating cluster of differentiation 14+ cells, indicating a dysfunctional immune response. Future strategies aiming for immunomodulation in this population of ICU patients should be guided by an immune-monitoring program in an effort to determine who might potentially benefit from a targeted immunological intervention.
In higher life forms, the immune system is organized in complex social network architecture-like structures,1 and its dysfunction is associated with adverse outcomes in various clinical scenarios. Although detection and monitoring of various organ dysfunctions is a key challenge for physicians involved in the care for the critically ill, the immune system may currently be regarded somewhat overlooked as it is typically not monitored within the clinical routines of most intensive care units (ICUs). This may be of particular importance in critically ill patients with severe infections (eg, patients with bacterial septic shock).2–7
Data show that monocytes/macrophages play key roles in critically ill patients with severe infections and constitute a first-line cellular response that initiates and promotes a targeted, adaptive, immune response.2,3,8 In this regard, flow cytometry–based standardized assessment of the surface expression of monocytic human leukocyte antigen-DR (mHLA-DR) was proposed by us and others2,9,10 to serve as a global marker of (monocytic) immune function as it reflects key cell–mediated immune functions including major histocompatibility complex (MHC) class II–mediated antigen-presentation, ex-vivo cytokine release, and phagocytosis.2,3,6,8,10 mHLA-DR expression can be assessed in a quantitative fashion using a standardized assay (coefficient of variation <4% intralab and 15% interlab),11 allowing for multicenter data comparison.9 Importantly, mounting data from critically ill patients with (bacterial) sepsis/septic shock show that reduced mHLA-DR expression (indicating “injury-associated immunosuppression”3) is associated with adverse clinical outcomes in ICU patients, including increased rates of secondary infections and increased mortality.2,12–15 Further, mHLA-DR previously served to guide targeted immunological interventions, for example, using immunostimulatory approaches16–18 or via reduction of inhibitory factors.19 Such biomarker enrichment20 may allow for identification of which patient might benefit best from a given immunomodulatory intervention.2,6,7,14
From an epidemiological perspective, coronavirus disease 2019 (COVID-19; severe acquired respiratory syndrome coronavirus-2 [SARS-CoV-2]) patients appear (clinically) well characterized.21–24 However, the role of virus-induced immunosuppression remains incompletely understood.25 We therefore embarked to investigate the role and course of mHLA-DR expression in ICU patients with severe COVID-19 disease, that is, critically ill patients. This is performed as understanding of the immunologic phenotype will be important when immunomodulatory immunotherapies are evaluated.
METHODS
In a preliminary prospective monocentric observational study, patients with confirmed COVID-19 disease were included from March to April 2020 and followed up until ICU-/hospital discharge and/or death. Patients were initially assessed for eligibility in the emergency rooms (noncritically ill patients) or at the ICU (in cases of direct ICU admission). The study was performed in a 900+ bed tertiary care academic medical center (Inselspital, Bern University Hospital, Switzerland). In this center, the Department of Intensive Care Medicine is the sole provider of intensive care medicine for adults.
Adult (aged ≥18 years) patients with confirmed SARS-CoV-2 infection (detected by polymerase chain reaction [PCR] in nasopharyngeal swabs) were consecutively included in the study after provision of informed consent (in case of lack of capacity and/or inability to provide consent, consent followed the local procedures for research projects in emergency situations). Screening of patients was performed in daily clinical practice by the research team. The following exclusion criteria applied: no confirmed SARS-CoV-2 infection or confirmed SARS-CoV-2 infection >3 days before inclusion, age <18 years, lack of consent. No financial compensation applied for participants. Hospitalized patients and ICU patients were followed up until ICU or hospital discharge or death (while in hospital). Laboratory data were recorded with missing data indicated. Laboratory samples were drawn at the scheduled visits within ±36 hours. Data available until April 30, 2020 (censor date) were included. The study was performed in accordance with the “Declaration of Helsinki” and approved by the Kantonale Ethikkommission KEK, Bern, Switzerland, Nr. 2020-00877.
Flow Cytometric Assessment of mHLA-DR Expression
Flow cytometric assessment of mHLA-DR expression (primary outcome) was performed from ethylenediaminetetraacetic acid (EDTA) samples within 4 hours, as previously reported11 (discussed in references 3, 9). In brief, a mixture that contains beads with predefined amounts of conjugated antibodies (phycoerythrin molecules [PE]) is measured using the same flow cytometer instrument settings (as the cells of interest) using a mixture of antihuman HLA-DR-PE, antihuman CD14-PerCP-Cy5.5, and an inhibitor of HLA-DR turnover (Quantibrite HLA-DR/Monocyte reagent, Becton Dickinson, Franklin Lakes, NJ).11 The known ratio of PE to anti-HLA-DR antibody is applied to convert PE molecules/cell into antibodies/cell3,9,11 with the anti-CD14 antibody detecting all monocytes (CD14 bright and weak positive).11 The gating strategy is given in Figure 1.
Figure 1.
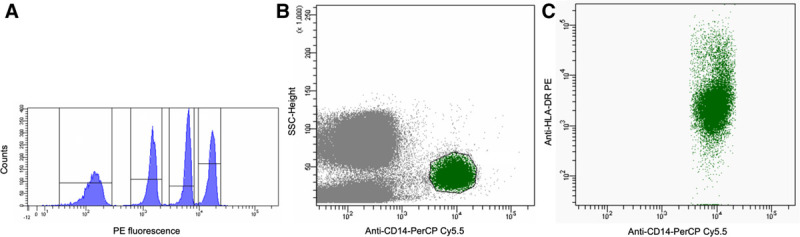
Flow cytometric analysis of HLA-DR expression in COVID-19 patients. Gating strategy: key steps in measurement of monocytic HLA-DR expression using standardized assessment. Beads are gated on their SSC and FSC characteristics (not shown), and PE fluorescence is plotted (A). Patient’s monocytes are gated by CD14-binding and SSC properties (B), mHLA-DR expression is plotted against CD14 to calculate the median HLA-DR expression (C). CD14 indicates cluster of differentiation (14); COVID-19, coronavirus disease 2019; FSC, forward scatter; HLA-DR, human leukocyte antigen-DR; mHLA-DR, monocytic human leukocyte antigen-DR; PE, phycoerythrin; SSC, side scatter.
Statistics
Data were analyzed with Stata 16.1 (StataCorp, College Station, TX). The distribution of continuous data was assessed with histograms, Q-Q plots, and Shapiro-Wilk tests. All continuous data departed from the normal distribution and are presented as median [quartiles]. Baseline demographic data, laboratory data, and follow-up data were compared between the groups with Mann-Whitney U tests (continuous data) or with Fisher exact test (categorical data; all had expected counts <5 in ≥25% of cells).
The primary outcome, mHLA-DR expression at admission, was compared between the groups (patients admitted to the general ward versus patients admitted to the ICU) using a Mann-Whitney U test.26 The median difference between the groups and its 95% confidence interval (CI) were estimated with the Hodges-Lehmann estimator. Being aware that our small dataset does not lend itself to multiple regression modeling, we yet performed explorative analyses to gauge potential confounding due to differences in baseline characteristics between groups.27,28 We used quantile (median) regression, as well as linear regression with bootstrapped standard errors (10,000 replications), to adjust for age, sex, and body mass index (BMI).
One patient was first admitted to the normal ward and subsequently to the ICU after clinical deterioration. According to the primary admission, this patient is considered a noncritically ill patient for the comparison of mHLA-DR expression at admission. We also performed a sensitivity analysis in which the patient was analyzed as being an ICU patient.
In ICU patients, follow-up data for mHLA-DR expression were obtained at days 3 and 5 of their ICU admission. Differences over time were tested with the Skillings-Mack test. This test is an extension of the Friedman test (nonparametric equivalent to 1-way repeated-measures analysis of variance) that allows for missing data. Two-sided P < .05 was considered statistically significant. For this preliminary investigation, a formal a priori power analysis/sample size calculation was not performed, and the sample size is based on the available number of patients.
Results
Sixteen patients (12 male, median age 68 years) were included in this preliminary observational study, of which 9 were primarily admitted to the ICU for mechanical ventilation, and 7 with primary hospitalization at the general ward. The Table shows demographic data, comorbidities, laboratory data, as well as follow-up data for both patient groups. While the Table suggests clinically relevant differences in terms of infection parameters and length of hospital stay in our sample of patients, there was insufficient evidence to claim a significant difference in the population of patients from which the data were sampled (all P values >.05).
Table.
Baseline Demographics, Disease Severity, and Clinical Outcome
| ICU Patients With COVID-19 (n = 9) | Hospitalized COVID-19 Patients (n = 7) | Total Cohort (n = 16) | Between-Group P Value | |
|---|---|---|---|---|
| Demographics | ||||
| Age (y) | 66 [62, 77] | 71 [55, 73] | 68 [59, 75] | .98 |
| Gender (male, %) | 6 (67) | 6 (86) | 12 (75) | .59 |
| Body mass index | 26.9 [26.0, 27.8] | 26.3 [24.4, 27.9] | 26.6 [25.1, 27.9] | .59 |
| APACHE-II score (first 24 h) | 30 [25, 32] | - | - | - |
| SAPS II score (first 24 h) | 69 [66, 78] | - | - | - |
| SOFA score (baseline) | 13 [13, 15] | - | - | - |
| Comorbidity data | ||||
| Charlson comorbidity index (total score) | 3 [2, 6] | - | - | - |
| Myocardial infarction (no./%) | 1 (11%) | - | - | - |
| Chronic heart failure (no./%) | 0 (0%) | - | - | - |
| Peripheral vascular disease (no./%) | 1 (11%) | - | - | - |
| Cerebrovascular accident (no./%) | 1 (11%) | - | - | - |
| Dementia (no./%) | 0 (0%) | - | - | - |
| COPD (no./%) | 3 (33%) | - | - | - |
| Connective tissue disease (no./%) | 0 (0%) | - | - | - |
| Peptic ulcer disease (no./%) | 0 (0%) | - | - | - |
| Liver disease (0–3) (no./%) | 0 (0%) | - | - | - |
| Diabetes (0–2) (no./%) | 2 (22%) | - | - | - |
| Hemiplegia (no./%) | 0 (0%) | - | - | - |
| Moderate to severe CKD (no./%) | 2 (22%) | - | - | - |
| Solid tumor (0–6) (no./%) | 0 (0%) | - | - | - |
| Leukemia (no./%) | 0 (0%) | - | - | - |
| Lymphoma (no./%) | 0 (0%) | - | - | - |
| HIV/AIDS (no./%) | 0 (0%) | - | - | - |
| Laboratory data | ||||
| C-reactive protein (mg/L) | 149 [96, 243] | 43 [7, 126] | 120 [31, 197] | .07 |
| Procalcitonin levels (ng/mL) | 0.4 [0.2, 1.2] | 0.2 [0.1, 0.3] | 0.3 [0.2, 0.5] | .09 |
| Total leukocyte count (G/L) | 7.0 [4.7, 7.7] | 6.9 [5.2, 8.5] | 6.9 [5.0, 8.1] | .92 |
| Total lymphocyte count (G/L) | 0.8 [0.6, 0.9] | 1.2 [1.0, 1.9] | 1.0 [0.8, 1.7] | .06 |
| Platelet count (G/L) | 192 [143, 225] | 185 [174, 267] | 189 [166; 234] | .47 |
| Serum potassium (mmol/L) | 3.9 [3.6, 4.2] | 3.7 [3.6, 4.2] | 3.8 [3.6, 4.2] | .42 |
| Serum creatinine (µmol/L) | 102 [76, 134] | 79 [62, 97] | 95 [67, 105] | .14 |
| D-dimers (µg/L) | 1340 [982, 1973] | 490 [428, 2062] | 1233 [574, 2062] | .28 |
| Follow-up | ||||
| Days on ICU | 11.8 [8.3, 23.0] | - | - | - |
| Days in hospital | 17 [9, 24] | 6 [4, 14] | 10.5 [4.5, 20.0] | .07 |
| Total days on antibiotics | 6 [4, 8] | 4 [1, 12] | 4.5 [1.5, 9.0] | .49 |
| Total days on mechanical ventilation | 9 [5, 23] | - | - | - |
| Renal replacement at any time (no./%) | 3 (33%) | - | - | - |
| On vasopressors at any time (no./%) | 8 (89%) | - | - | - |
| Total norepinephrine dose (cumulative dose/ICU days; mg) | 3.4 [1.3, 6.8] | - | - | - |
| ICU mortality (no./%) | 2/9 (22%)a | - | - | - |
| Hospital mortality (no./%) | 2/9 (22%)a | 0/7 (0%) | 2/16 (13%) | .50 |
Demographical data, baseline comorbidities, laboratory data, and clinical follow-up are given for patients with primary admission to ICU versus normal ward (until censor date). Numbers (No.) with percentages are given, as indicated. Continuous data are reported as median [quartiles]. Between-group P values from Mann-Whitney U tests and Fisher exact tests are given for ICU versus non–ICU (normal ward) populations.
Abbreviations: AIDS, acquired immunodeficiency syndrome; APACHE-II, Acute Physiology and Chronic Health Evaluation-II score; CKD, chronic kidney disease; COPD, chronic obstructive pulmonary disease; COVID-19, coronavirus disease 2019; HIV, human immunodeficiency virus; ICU, intensive care unit; SAPS II, Simplified Acute Physiology Score II; SOFA, sepsis-related organ failure assessment score.
aMortality data are available until censor date. Between-group P values are given for ICU versus non–ICU (normal ward) populations.
mHLA-DR expression at admission was significantly lower in the ICU group (9280 antibodies/cell [6114, 16,567]) as compared to the non–ICU group (30,900 antibodies/cell [26,777, 52,251]), with a median difference of 21,508 antibodies/cell (95% CI, 14,118–42,971), P = .002 (Figure 2). Similarly, the adjusted quantile regression and linear regression provided evidence for a significant between-group difference (P = .001 and P < .001, respectively).
Figure 2.
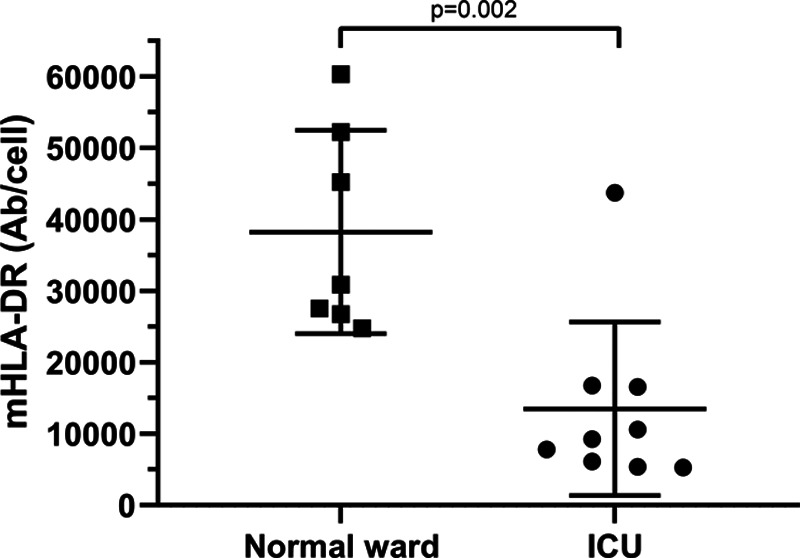
mHLA-DR expression in hospitalized patients with COVID-19. mHLA-DR expression (given in Ab/cell) at normal ward (n = 7) versus primary ICU admission (n = 9), P = .002 in Mann-Whitney U test. Ab/cell indicates antibodies/cell; COVID-19, coronavirus disease 2019; ICU, intensive care unit; mHLA-DR, monocytic human leukocyte antigen-DR.
The sensitivity analysis, in which 1 patient of the non–ICU group was counted toward the ICU group as described above, provides consistent results in the unadjusted analysis (median difference 19,419 antibodies/cell, 95% CI, 8487–43,578, P = .016) as well as in the adjusted analyses (P = .001 and P = .007, respectively).
In ICU patients, median mHLA-DR expression was 9280 antibodies/cell [6114, 16,567] at admission (N = 9), 9672 antibodies/cell [8253, 10,511] at 3 days (N = 9), and 7334 antibodies/cell [5241, 11,022] at 5 days (N = 6), without evidence for a change over time (P = .33, Figure 3). Including the admission measurement of the patient who was initially admitted to the normal ward and who was later admitted to the ICU, median HLA-DR expression was 9944 antibodies/cell [6114, 16,782] at admission (N = 10), still without evidence for a change over time (P = .19).
Figure 3.
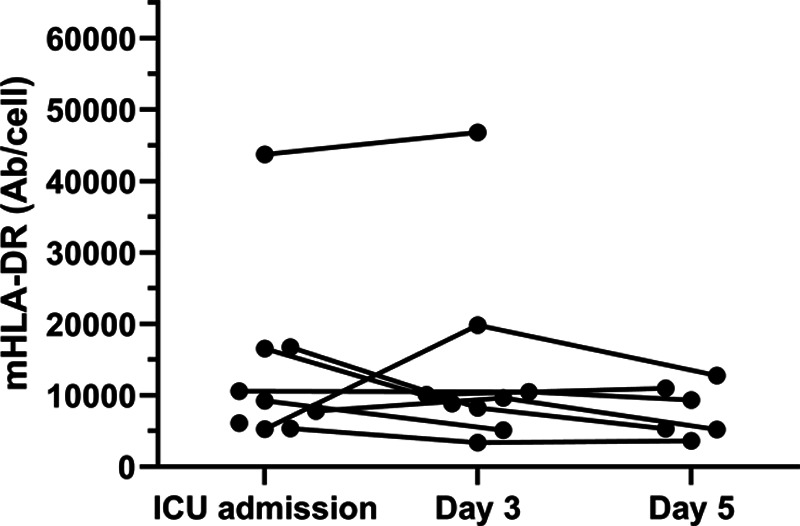
Expression of monocytic HLA-DR over time in patients hospitalized in the ICU. Available data (presented in Ab/cell) are given at ICU admission, and days 3 and 5. Discharge from ICU (until day 5) and transfer from the normal ward to ICU are included. Ab/cell indicates antibodies/cell; HLA-DR, human leukocyte antigen-DR; ICU, intensive care unit.
Discussion
We demonstrate immunosuppression of key innate immune cells in critically ill patients with (severe) COVID-19. mHLA-DR expression was reduced on circulating CD14+ cells, and this was not observed in hospitalized COVID-19 patients without critical illness. Importantly, this initial effect persisted over the ensuing days of ICU treatment (until day 5). Of note, all study individuals were treatment-naive regarding immunomodulatory agents and/or high-dose corticosteroids. In the light of the current multiple immunomodulatory interventional approaches tested in COVID-19,25 it seems essential that patients are adequately immunologically characterized using immunological read-outs in an effort to determine which patient might benefit best from a given immunomodulatory intervention. Thus, injury-associated immunosuppression should be taken into account when novel immunomodulatory interventions are designed and tested in critically ill patients with COVID-19.
Our current data show that immunosuppression presented as early as at ICU admission and the observed downregulation of mHLA-DR did not change significantly over the ensuing days of ICU treatment (ie, at least until day 5 after ICU admission). This seems of particular interest, as when compared to ICU patients with (bacterial) septic shock, decreased mHLA-DR expression is mostly observed after a few days following ICU admission and may be most prominent after about 72 hours (reviewed in reference 3). Although the exact onset of disease can mostly not be elucidated in critically ill patients, it is known that the median incubation period of SARS-CoV-2 is about 4–5 days21–24 and about 97.5% of patients diagnosed with COVID-19 develop symptoms within the first 11.5 days.22 In the light of the specific disease investigated, it thus seems tempting to speculate that downregulation of mHLA-DR would typically occur before development of acute respiratory failure, that is, before ICU admission in severe COVID-19 disease and mHLA-DR assessment could theoretically provide early prognostic information. Moreover, and importantly, the immunosuppression reflected in decreased mHLA-DR might theoretically be a relevant contributor to progression of increased viral replication and/or the severity of the viral disease. Previous data from ICU patients with bacterial septic shock show that secondary infection rates are increased in patients with persistent downregulation of mHLA-DR, that is, injury-associated immunosuppression (reviewed in references 3, 6). Thus, as secondary infections contribute to increased morbidity and mortality in ICU patients with COVID-19 disease, the potential association of mHLA-DR downregulation with secondary infection rates should be investigated in subsequent investigations. Importantly, however, in the current analysis, we are unable to conclude back on causality and/or effects on secondary infection rates due to the limited sample size and the preliminary, observational nature of the investigation.
Further, our observations might challenge the concept of a general macrophage activation syndrome as being a primary driver of severe COVID-19 disease. In the current observational study, we observed macrophage “deactivation” as indicated by reduced expression of MHC class II (human leukocyte antigen-DR [HLA-DR]) on CD14+ cells, rather than macrophage activation. However, due to the limited sample size and monocentric character of the investigation, this awaits confirmation in subsequent larger analyses.
A number of additional limitations of this analysis deserve discussion. First, consecutive patients were included in a single-center observational study and all respective limitations (driven by study design) apply. Second, the sample size was limited and results await confirmation in subsequent larger cohorts. However, the limited sample size was partly due to the fact that informed consent cannot easily be achieved during a pandemic in the cohort investigated. Nevertheless, observed effects on mHLA-DR expression were consistent and strong, likely pointing to an important disease-immanent process. Third, final outcome data were not available for 3 patients with long-term ICU stay. However, although a final data set might have been preferable, it may underline the relevance of immunosuppression in this context. Fourth, follow-up data at days 3 and 5 of noncritically ill hospitalized patients would have been interesting, but were unavailable (also for the fact that patients improved rapidly) to obtain such samples as patients were discharged from our institution. Fifth, longer follow-up, that is, until all ICU patients have recovered, would have been preferable; however, this was initially deemed not possible and out of the scope of the current investigation. Nevertheless, we are therefore unable to conclude on the potential recovery slope of mHLA-DR in survivors of critical illness and suppose that this should be investigated in subsequent larger studies. Sixth, one might speculate whether monocyte deactivation would be a phenomenon of the blood compartment, rather than to reflect monocytic immune function in “solid immune organs.” However, it was previously shown in patients with bacterial sepsis, that HLA-DR downregulation would not only be observed in the blood compartment but would rather be paralleled in respective “solid immune organs.”15
In conclusion, in a prospective monocentric study with a limited sample size, we observed that severe COVID-19 disease is associated with considerable and sustained immunosuppression of key innate immune cells (monocytes/macrophages), indicating a dysfunctional immune response in a majority of critically ill patients. This phenotype persisted over the initial days of ICU treatment and may underline the urgent need for an adequate immunological characterization (using appropriate immunological read-outs) when targeted immunomodulatory interventions are tested in respective critically ill patients.
DISCLOSURES
Name: Thibaud Spinetti, PhD.
Contribution: This author helped with the conception and design of the study, analysis and interpretation of data, drafting the article, and approved the final version to be submitted.
Conflicts of Interest: T. Spinetti declares that the Department of Intensive Care Medicine, Inselspital, Bern, has received research or other grants from (full departmental disclosure): Orion Pharma, Abbott Nutrition International, B. Braun Medical, CSEM, Edwards Lifesciences Services, Kenta Biotech, Maquet Critical Care, Omnicare Clinical Research, Nestle, Pierre Fabre Pharma, Pfizer, Bard Medica, Abbott, Anandic Medical Systems, Pan Gas Healthcare, Bracco, Hamilton Medical, Fresenius Kabi, Getinge Group Maquet, Dräger, Teleflex Medical, Glaxo Smith Kline, Merck Sharp and Dohme, Eli Lilly and Company, Baxter, Astellas, Astra Zeneca, CSL Behring, Novartis, Covidien, Hemotune, Phagenesis, and Nycomed outside the submitted work. The money was paid into departmental funds.
Name: Cedric Hirzel, MD.
Contribution: This author helped with the conception and design of the study, analysis and interpretation of data, drafting the article, and approved the final version to be submitted.
Conflicts of Interest: None.
Name: Michaela Fux, PhD.
Contribution: This author helped with the conception and design of the study, analysis and interpretation of data, drafting the article, and approved the final version to be submitted.
Conflicts of Interest: None.
Name: Laura N. Walti, MD.
Contribution: This author helped with the conception and design of the study, analysis and interpretation of data, drafting the article, and approved the final version to be submitted.
Conflicts of Interest: None.
Name: Patrick Schober, MD, PhD, MMedStat.
Contribution: This author helped with the conception and design of the study, analysis and interpretation of data, drafting the article, and approved the final version to be submitted.
Conflicts of Interest: None.
Name: Frank Stueber, MD.
Contribution: This author helped with the conception and design of the study, analysis and interpretation of data, drafting the article, and approved the final version to be submitted.
Conflicts of Interest: None.
Name: Markus M. Luedi, MD, MBA.
Contribution: This author helped with the conception and design of the study, analysis and interpretation of data, drafting the article, and approved the final version to be submitted.
Conflicts of Interest: None.
Name: Joerg C. Schefold, MD.
Contribution: This author helped with the conception and design of the study, analysis and interpretation of data, drafting the article, and approved the final version to be submitted.
Conflicts of Interest: J. C. Schefold declares that the Department of Intensive Care Medicine, Inselspital, Bern, has received research or other grants from (full departmental disclosure): Orion Pharma, Abbott Nutrition International, B. Braun Medical, CSEM, Edwards Lifesciences Services, Kenta Biotech, Maquet Critical Care, Omnicare Clinical Research, Nestle, Pierre Fabre Pharma, Pfizer, Bard Medica, Abbott, Anandic Medical Systems, Pan Gas Healthcare, Bracco, Hamilton Medical, Fresenius Kabi, Getinge Group Maquet, Dräger, Teleflex Medical, Glaxo Smith Kline, Merck Sharp and Dohme, Eli Lilly and Company, Baxter, Astellas, Astra Zeneca, CSL Behring, Novartis, Covidien, Hemotune, Phagenesis, and Nycomed outside the submitted work. The money was paid into departmental funds.
This manuscript was handled by: Jean-Francois Pittet, MD.
FOOTNOTES
GLOSSARY
- Ab/cell
- antibodies/cell
- AIDS
- acquired immunodeficiency syndrome
- APACHE-II
- Acute Physiology and Chronic Health Evaluation-II score
- BMI
- body mass index
- CD14+
- cluster of differentiation (14+)
- CI
- confidence interval
- CKD
- chronic kidney disease
- COPD
- chronic obstructive pulmonary disease
- COVID-19
- coronavirus disease 2019
- EDTA
- ethylenediaminetetraacetic acid
- FACS
- fluorescence-activated cell sorting
- FSC
- forward scatter
- HIV
- human immunodeficiency virus
- HLA-DR
- human leukocyte antigen-DR
- ICU
- intensive care unit
- MHC
- major histocompatibility complex
- mHLA-DR
- monocytic human leukocyte antigen-DR
- PCR
- polymerase chain reaction
- PE
- phycoerythrin
- SAPS II
- Simplified Acute Physiology Score II
- SARS-CoV-2
- severe acquired respiratory syndrome coronavirus-2
- SOFA
- sepsis-related organ failure assessment score
- SSC
- side scatter
Published ahead of print 4 June 2020.
Funding: None.
Conflicts of Interest: See Disclosures at the end of the article.
T. Spinetti and C. Hirzel contributed equally and share first authorship.
All available data and materials are available on reasonable noncommercial request to the corresponding author. All software application or custom code are available on request to the corresponding author.
Reprints will not be available from the authors.
REFERENCES
- 1.Rieckmann JC, Geiger R, Hornburg D. Social network architecture of human immune cells unveiled by quantitative proteomics. Nat Immunol. 2017;18:583–593. [DOI] [PubMed] [Google Scholar]
- 2.Hotchkiss RS, Monneret G, Payen D. Sepsis-induced immunosuppression: from cellular dysfunctions to immunotherapy. Nat Rev Immunol. 2013;13:862–874. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Pfortmueller CA, Meisel C, Fux M, Schefold JC. Assessment of immune organ dysfunction in critical illness: utility of innate immune response markers. Intensive Care Med Exp. 2017;5:49. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Rubio I, Osuchowski MF, Shankar-Hari M. Current gaps in sepsis immunology: new opportunities for translational research. Lancet Infect Dis. 2019;19:e422–e436. [DOI] [PubMed] [Google Scholar]
- 5.Schefold JC, Hasper D, Reinke P, Monneret G, Volk HD. Consider delayed immunosuppression into the concept of sepsis. Crit Care Med. 2008;36:3118. [DOI] [PubMed] [Google Scholar]
- 6.Venet F, Monneret G. Advances in the understanding and treatment of sepsis-induced immunosuppression. Nat Rev Nephrol. 2018;14:121–137. [DOI] [PubMed] [Google Scholar]
- 7.Schefold JC, Hasper D, Volk HD, Reinke P. Sepsis: time has come to focus on the later stages. Med Hypotheses. 2008;71:203–208. [DOI] [PubMed] [Google Scholar]
- 8.Roche PA, Furuta K. The ins and outs of MHC class II-mediated antigen processing and presentation. Nat Rev Immunol. 2015;15:203–216. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Monneret G, Venet F, Meisel C, Schefold JC. Assessment of monocytic HLA-DR expression in ICU patients: analytical issues for multicentric flow cytometry studies. Crit Care. 2010;14:432. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Schefold JC. Measurement of monocytic HLA-DR (mHLA-DR) expression in patients with severe sepsis and septic shock: assessment of immune organ failure. Intensive Care Med. 2010;36:1810–1812. [DOI] [PubMed] [Google Scholar]
- 11.Döcke WD, Höflich C, Davis KA. Monitoring temporary immunodepression by flow cytometric measurement of monocytic HLA-DR expression: a multicenter standardized study. Clin Chem. 2005;51:2341–2347. [DOI] [PubMed] [Google Scholar]
- 12.Chéron A, Monneret G, Landelle C, Floccard B, Allaouchiche B. Low monocytic HLA-DR expression and risk of secondary infection. Ann Fr Anesth Reanim. 2010;29:368–376. [DOI] [PubMed] [Google Scholar]
- 13.Monneret G, Lepape A, Voirin N. Persisting low monocyte human leukocyte antigen-DR expression predicts mortality in septic shock. Intensive Care Med. 2006;32:1175–1183. [DOI] [PubMed] [Google Scholar]
- 14.Venet F, Lukaszewicz AC, Payen D, Hotchkiss R, Monneret G. Monitoring the immune response in sepsis: a rational approach to administration of immunoadjuvant therapies. Curr Opin Immunol. 2013;25:477–483. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Boomer JS, To K, Chang KC. Immunosuppression in patients who die of sepsis and multiple organ failure. JAMA. 2011;306:2594–2605. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Nierhaus A, Montag B, Timmler N. Reversal of immunoparalysis by recombinant human granulocyte-macrophage colony-stimulating factor in patients with severe sepsis. Intensive Care Med. 2003;29:646–651. [DOI] [PubMed] [Google Scholar]
- 17.Meisel C, Schefold JC, Pschowski R. Granulocyte-macrophage colony-stimulating factor to reverse sepsis-associated immunosuppression: a double-blind, randomized, placebo-controlled multicenter trial. Am J Respir Crit Care Med. 2009;180:640–648. [DOI] [PubMed] [Google Scholar]
- 18.Payen D, Faivre V, Miatello J. Multicentric experience with interferon gamma therapy in sepsis induced immunosuppression. A case series. BMC Infect Dis. 2019;19:931. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Schefold JC, von Haehling S, Corsepius M. A novel selective extracorporeal intervention in sepsis: immunoadsorption of endotoxin, interleukin 6, and complement-activating product 5a. Shock. 2007;28:418–425. [DOI] [PubMed] [Google Scholar]
- 20.Spinetti T, Meisel C, von Gunten S, Schefold JC. Immune biomarker-based enrichment in sepsis trials. Crit Care. 2020;24:58. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Guan WJ, Ni ZY, Hu Y; China Medical Treatment Expert Group for Covid-19. Clinical characteristics of coronavirus disease 2019 in China. N Engl J Med. 2020;382:1708–1720. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Lauer SA, Grantz KH, Bi Q, et al. The incubation period of coronavirus disease 2019 (COVID-19) from publicly reported confirmed cases: estimation and application. Ann Intern Med. 2020;172:577–582. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Li Q, Guan X, Wu P. Early transmission dynamics in Wuhan, China, of novel coronavirus-infected pneumonia. N Engl J Med. 2020;382:1199–1207. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Pung R, Chiew CJ, Young BE; Singapore 2019 Novel Coronavirus Outbreak Research Team. Investigation of three clusters of COVID-19 in Singapore: implications for surveillance and response measures. Lancet. 2020;395:1039–1046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Tay MZ, Poh CM, Rénia L, MacAry PA, Ng LFP. The trinity of COVID-19: immunity, inflammation and intervention. Nat Rev Immunol. 2020;20:363–374. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Schober P, Vetter TR. Two-sample unpaired t tests in medical research. Anesth Analg. 2019;129:911. [DOI] [PubMed] [Google Scholar]
- 27.Vetter TR, Schober P. Regression: the apple does not fall far from the tree. Anesth Analg. 2018;127:277–283. [DOI] [PubMed] [Google Scholar]
- 28.Schober P, Vetter TR. Confounding in observational research. Anesth Analg. 2020;130:635. [DOI] [PubMed] [Google Scholar]


