Abstract
Background:
The supracondylar nonunion of femur in elderly individuals is rare and challenging to manage. Nothing in English literatures or guidelines is available regarding this particular fracture characterized by osteoporosis, soft-tissue contracture, shortening, and joint stiffness. We report a case of an elderly patient with a supracondylar nonunion of the femur, which was successfully treated using staged Ilizarov techniques and dual plating.
Case Presentation:
An 84-year-old female patient was admitted to our orthopedic department for her pain and soft-tissue swelling around the right knee with claudication and shortening deformity of the affected extremity. She denied any specific history of trauma and had sought traditional Chinese medical attention for 6 months before she presented to our hospital. Diagnosis of the right femoral supracondylar nonunion was made based on the X-ray and computed tomography. Ilizarov external fixator was carried out for successive and slow distraction and gradual correction of the shortening deformity, in consideration of the nonunion was still present. Subsequently, internal fixation with dual plating of the distal femur was performed. Excellent function and patient satisfaction were observed at 6 months of follow-up.
Conclusion:
The protocol of Ilizarov technique with subsequent internal fixation of dual plating seems to be an efficient solution to the supracondylar nonunion of femur in elderly patients with osteoporosis. The advantage of the protocol is that it allows knee joint motion, avoids neurovascular complications, and gentle correction of soft-tissue contractures.
Keywords: old fracture, nonunion, elderly patients, supracondylar fracture of femur, Ilizarov technique, osteoporosis, dual plating, internal fixation
Introduction
Misdiagnosis or missed diagnosis of fractures can be more likely to happen in developing countries. In China, the most common cause of neglected fractures is initial diagnosis and treatment done by traditional Chinese medicine (TCM) physicians. Most of the patients in China must pay for medical cost out of pocket, especially if they are not covered by government medical insurance and commercial insurance. The elderly individuals usually prefer TCM for the common symptoms such as swelling and pain. In China, traditional Chinese treatment is cheap, readily available, and widely accepted but often lacks X-ray, does not always identify acute fracture, and trends toward nonoperative treatment. Fractures without proper treatment for more than few weeks will allow muscles, vessels, and nerves to contract as well as predispose to disuse osteopenia. At present, there is no English literature regarding guidelines for treating the supracondylar nonunion of femur in elderly patients with osteoporosis as the condition is very rare in the world, especially in developed countries. Ilizarov technique offering the effect of gradual distraction has been proven to yield satisfactory results in various difficult situations like severe trauma, nonunions, limb length discrepancies, deformities, and osteomyelitis. We had the opportunity to treat the case of a missed geriatric supracondylar fracture of femur with Ilizarov technique followed by a second stage—consisting of internal fixation with dual plating. It appears to be the only case report in English literature.
Case Presentation
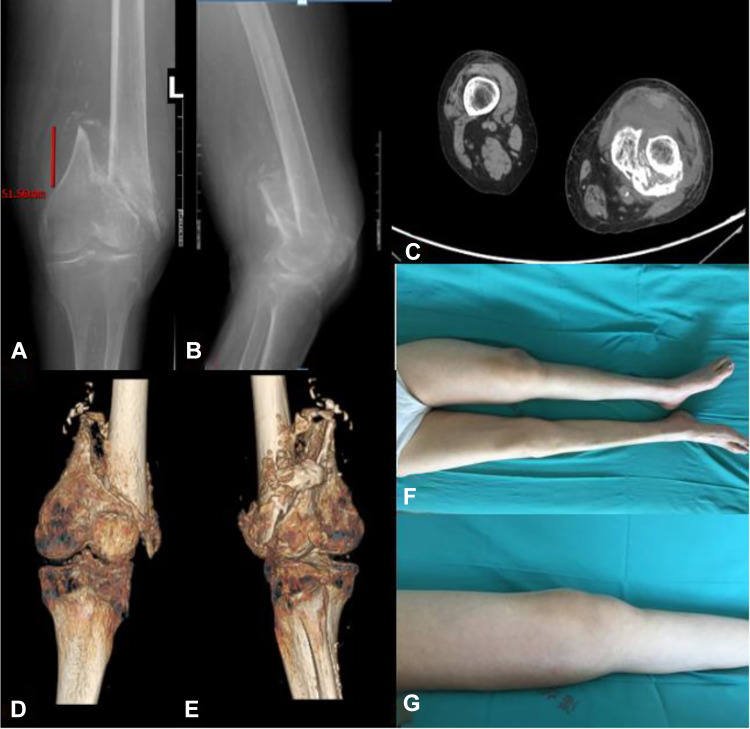
An 84-year-old female patient with a history of osteoporosis presented with pain and soft-tissue swelling of her right distal femur and with claudication and shortening deformity of the affected extremity for 6 months before she presented to our hospital. The patient’s clinical history was inaccurate, but there was no specific trauma or any known injury. Her activities of daily were initially unaffected. She first sought help from a traditional bone setter and was diagnosed with osteoporosis and knee osteoarthritis without any radiographs once symptoms worsened. The patient was treated conservatively with traditional Chinese plaster and herbal medicine and referred to a local physical therapy clinic for thermal modalities and therapeutic exercises. However, she failed to show any improvement despite a period of conservative treatment. The author examined the patient when she came to our orthopedic clinic 6 months later and suspected the presence of a possible fracture. Subsequent radiographic imaging examinations including X-ray and computed tomography scan revealed the left femoral supracondylar nonunion. Imaging and physical examination revealed the following challenges: osteoporosis, shortening about 5 cm, soft-tissue contracture, muscle atrophy, and joint stiffness (Figure 1).
Figure 1.
Anteroposterior and lateral radiograph (A and B), CT scan and 3D reconstruction images (C, D, E), and clinical picture (F and G) of the left lower extremity on presentation before operation. And (A) show the shortening is about 5 cm, and (D) and (E) show rotation deformity. CT indicates computed tomography.
In anticipation of the expected difficulties in reducing the fracture, distracting the soft tissue contractures and preventing neurovascular complications in this patient, a 2-stage procedure was planned and discussed with the patient. In the first stage, the Ilizarov external fixator installation was applied to the patient in a supine position on the fracture table under epidural anesthesia. Entire injured extremity was prepared and draped. Then application of the 2 preassembled circular frames of the femur and tibia was done, which was connected with 3 hinges distributing equally and flexing centrally around the knee. The femoral frame consisted of proximal blocs of 2 femoral arches connected together with rods, 1 complete ring proximal to the fracture, and 1 intermediate five-eighths ring between the fracture and knee. The five-eighths ring was connected to the complete ring with 4 rods, and the concavity of the five-eighths ring was directly behind the thigh. Then, the proximal arches were connected to the complete ring with 1 oblique support (an anterolateral rod) and 1 longitudinal support (a lateral rod). One reference Schanz pin and one wire were used to help frame application on the femur. The Schanz pin was inserted laterally at the level of the proximal fracture and attached to the complete ring. The wire was inserted transversely into the level of femoral condyle and attached to the five-eighths ring. The tibial frame consisted of 1 five-eighths ring and 1 complete ring, which was connected with 4 rods, and the concavity of the five-eighths ring was directly behind the leg. One reference Schanz pin and one wire were used to help frame application on the tibia. The Schanz pin was inserted anteriorly into the level under the tibial platform and attached to the five-eighths ring. The wire was inserted transversely into the level of middle tibia and attached to the complete ring. The 2 frames will center on the thigh and leg, respectively, and all the different aspects of the femoral and tibial frames should be parallel to the corresponding aspects of the thigh and leg, respectively. At the same time, adequate space presenting between the frame and the skin all around should be verified (Figure 2). When the hinges were locked, as a motion unit, the Ilizarov fixator could restrict knee movement and provide greater stability and allow the patient to stand and move freely with the help of her family. And when the patients lie on her bed, the hinges were allowed to unlock and the knee to flex 0 to 30°. Gradual distraction at the fracture site started 3 days postoperatively for 3 weeks until the shortening and deformity were corrected (Figure 3). In the second stage, the surgery of internal fixation with dual plating was done at a translucent orthopedic table in supine position and under combined spinal epidural anesthesia with tourniquet applied whenever feasible and with a bolster below the affected knee. After standard sterilization and draping in entire injured extremity and ipsilateral iliac crest, lateral incision was made beginning at the Gerdy tubercle and extending proximally far enough to facilitate adjustment of the lateral plate position and the medial plate insertion. Then minimally stripping of soft tissue necessary for application of the plates, the debridement of fibrotic and sclerotic areas, and the freshening of the end of the fracture were done. The subsequent reduction of the fracture was carried out first with preliminary K-wires followed by cancellous autograft obtained from iliac crest placed in the fracture site. Afterward, fixation of the lateral column was completed using locking lateral distal femoral plate and at last, under direct vision with neurovascular protection: A relatively small reconstructive plate was arranged in the anteromedial area of distal femur for the medial column using the single incision with percutaneous screws (Figure 4). Alignment was checked under X-ray image intensification.
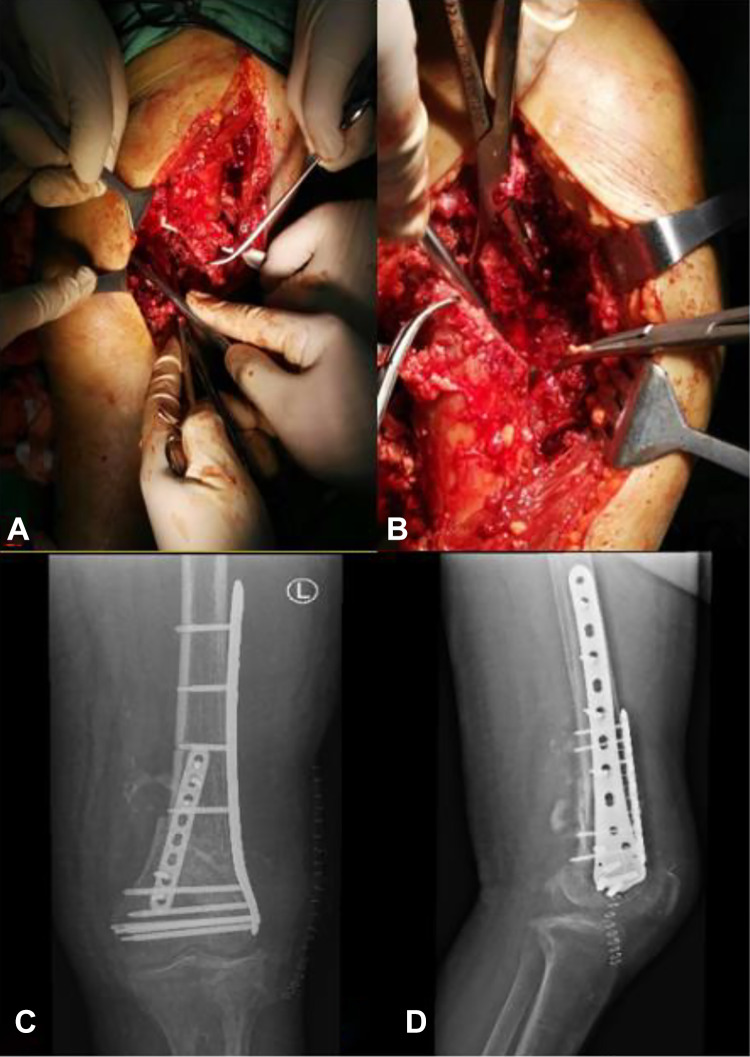
Figure 2.
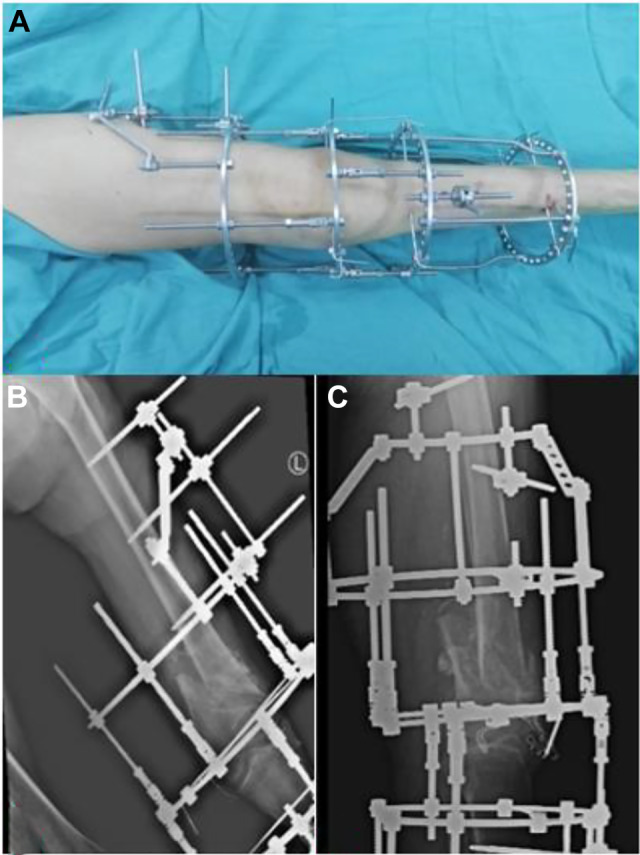
Clinical picture (A) and anteroposterior and lateral radiograph (B and C) of Ilizarov external fixator during and after the first stage operation.
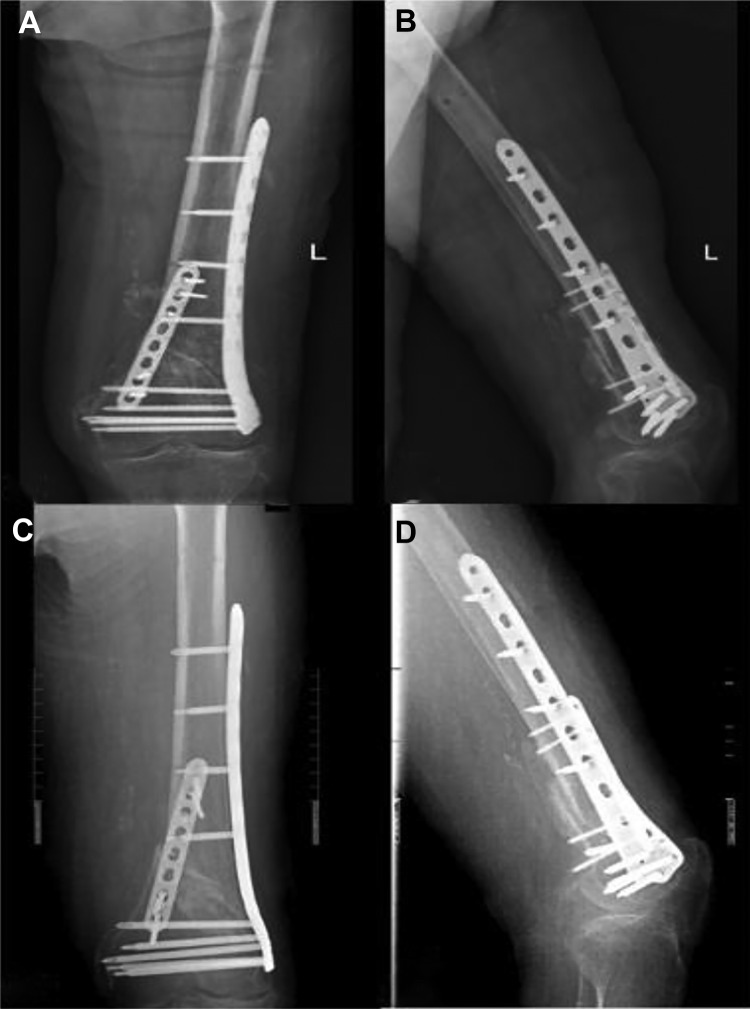
Figure 3.
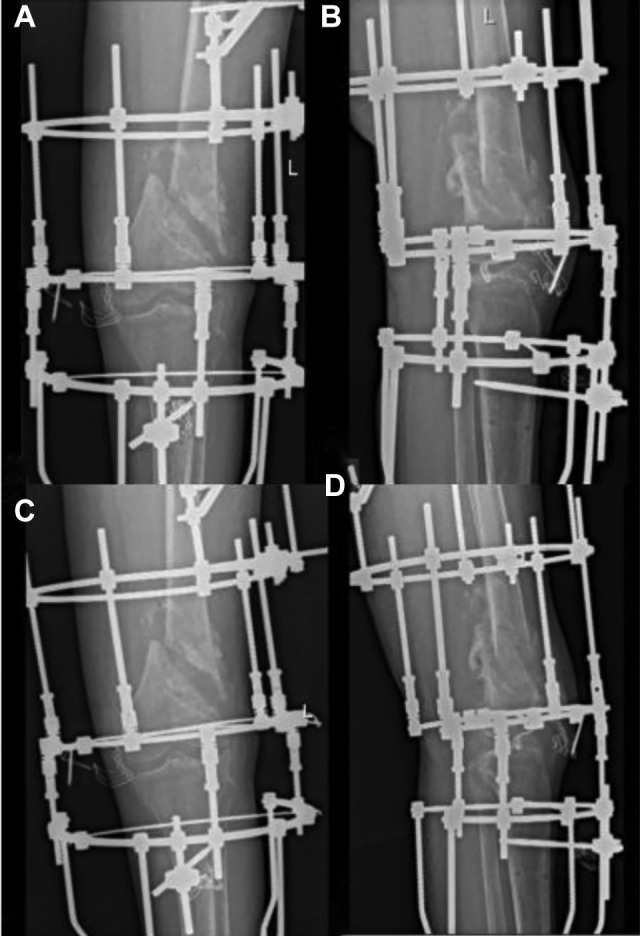
Anteroposterior and lateral radiograph (A and B) of Ilizarov external fixator when the shortening deformity was being corrected 3 days after the first stage and radiograph (C and D) of the shortening deformity had been corrected 3 weeks after the first stage.
Figure 4.
Clinical pictures (A and B) presenting fibrous nonunion and endosclerosis during the second stage. Anteroposterior and lateral radiograph (C and D) of femoral condyle 1 week after the second stage.
Rehabilitation exercises were begun from the first postoperative day for both stages. During the distraction, the patient could stand and move for a short period with the help of doctors and nurses or her family and flex her affected knee when lying in bed everyday. The continuous passive motion machine was used after the second stage with the flexion slowly increased from 0° to 60°. Then weight bearing was done gradually based on the clinical and radiological improvements. Bony union was documented on a radiograph at 3 months after operation (Figure 5). In the follow-up afterward, the patient stubbornly refused X-ray examination but she had returned to her routine life without pain and other symptoms at 6 months after operation (Figure 6).
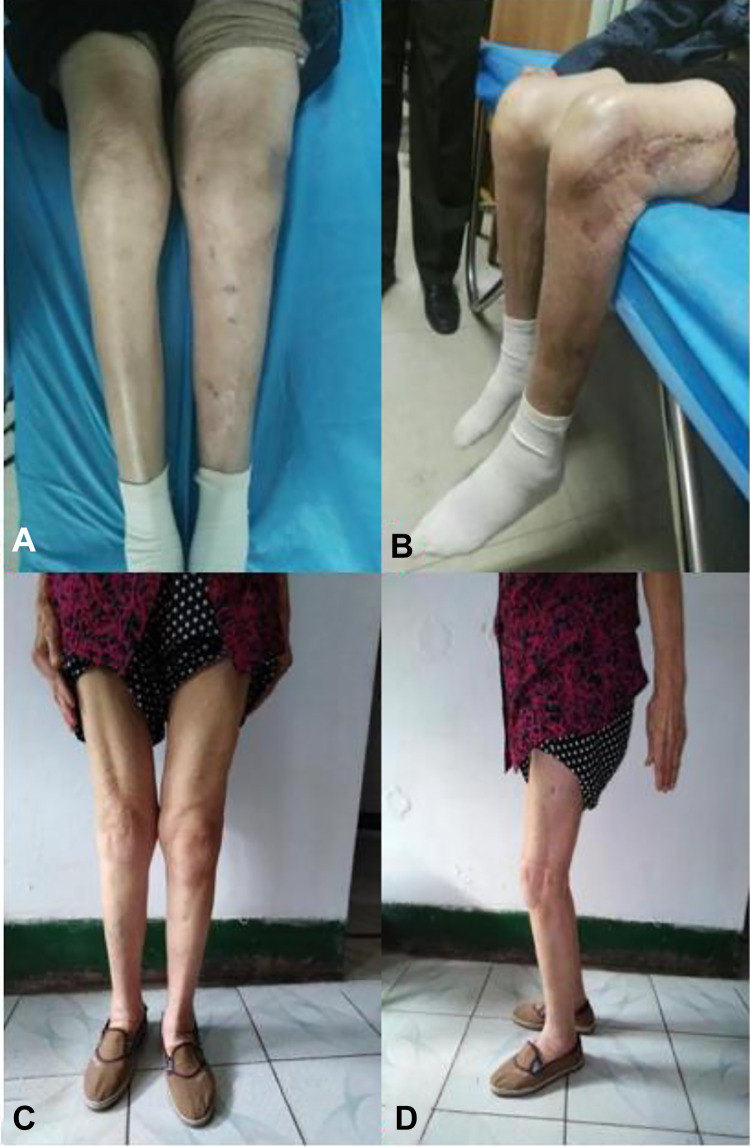
Figure 5.
Partially callus formation of AP and lateral radiograph (A and B) 1 month after the second stage. Basically bony union of AP and lateral radiograph (C and D) 3 months after the second stage. AP indicates anteroposterior.
Figure 6.
Clinical pictures (A and B) of 2 months after the second stage presenting partial weight bearing and an excellent motion of knee. Clinical pictures (C and D) of 6 months after the second stage presenting full weight bearing and returned to her routine life.
Discussion
Neglected fractures are more common in developing countries, like this patient. Various reasons for misdiagnosis and missed diagnosis include complex conditions, poverty, illiteracy, skepticism of Western medicine, and availability of traditional treatments. We speculate that the patient had a low-energy trauma and developed an incomplete fracture. Due to her low weight (40 kg), the patient could maintain normal activities with only minimal pain and swelling. Unfortunately, the traditional care provider did not give her accurate physical and radiographic examination or correct diagnosis. Initial treatments for osteoarthritis and osteoporosis allowed this insufficiency fracture to gradually develop into a complete fracture. The shortening deformity and symptoms of the nonunion worsened progressively. At last, when the patient came to our treatment center, it had been 6 months after visiting at Traditional Chinese physician and the fracture care became complex.
We considered all possible difficulties and complications of the nonunion in this patient with osteoporosis, like neurovascular palsies, pathological refracture, fixation options, joint stiffness, malunion or nonunion, and deformity correction. Kempf et al1 concluded that more than 4 cm of limb lengthening is associated with nerve palsies. Yadav2 described 6 to 16 cm lengthened of shortening limb should be obtained in duration of 3 to 6 weeks by skeletal traction, and the traction weight should gradually increase up to 30 kg to avoid neurovascular complications. In the treatment of neglected fracture of the shaft of femur, Krishnakumar et al3 performed definitive surgeries if overlapping was less than 1 cm, but if overlapping was more than 1 cm, skeletal traction with periodical increase of weights with neurovascular monitoring was done before definitive surgery. Because he holds that 1 cm overlapping can be overcome without undue tension under anesthesia with muscles relaxation and careful subperiosteal elevation, and when the overlapping more than 1 cm, correction of overlapping was possible with gradually increased traction weights. However, when the overlapping of lower extremity more than 5 cm, a surgery should be performed to help removing adhesions and using traction effectively to correction the shortening deformity before definitive surgery. In our case, the overlapping of the old supercondylar fracture of the femur was more than 5 cm accompanied by osteoporosis and unhealthy soft tissues, in which sustained activities of the affected limb while stretching the contraction of soft tissue and correcting deformity was therefore desired. The options for such deformity include surgery to remove adhesions, cutaneous or skeletal traction. Surgical release and lengthening of the shortening deformity require extensive soft-tissue dissection which inevitably resulting in extensive operative trauma and extra soft-tissue injuries, moreover, could not correct the gross shortening deformity at the same time on account of neurovascular complications.4 In the elderly patient with osteoporosis and aging skin, cutaneous traction or skeletal traction demanding long-term bedridden were also not suitable because of the risk of muscular atrophy, pin cut out, joint stiffness, deep venous thrombosis, and cardiopulmonary complications. We have been accumulating experience by using Ilizarov technique in various situations such as infection, pseudarthrosis, bone defects and deformity, and feel comfortable with this method. We felt that gradually docking with slow stretching of shortening limb without any dissection would be the perfect choice for the case, so we considered Ilizarov technique to mend the difficult situation. Through frame, the nonunion was distracted at the rate of 1 mm from the third postoperative day for 1 week and 2 mm for 2 weeks until the desired length was achieved. The Ilizarov technique is not aggressive and do not require massive intensive care measures postoperatively for geriatric patients. But the use of a simple circular frame construct with less number of wires and pins is also significant for geriatric patients with osteoporosis which could minimize the incidence of pathological fracture, pin-tract infection, and improve the patient compliance. The configuration allows and we encourage the moderate activities with partial weight bearing when standing and the knee movement when in bed, which could also minimize the incidence of complications such as deep vein thrombosis, disuse osteoporosis and stiffness of the knee. Mobilization could improve limb circulation and enhance the healing process based the fact that the speed of healing is usually proportionally determined by the amount of available circulation.5 The drop in physical fitness with aging is an unavoidable fact, and simultaneously body and bone strength deteriorate rapidly when the patient is confined to a bed, but all these could be minimized by early functional activities through Ilizarov external fixator.
Another difficulty we encountered was fixation options in consideration of osteoporosis, bone resorption, and poor stabilization. It necessitates a safe fracture fixation and an adequate rehabilitation for the immediate re-establishment in view of this patient’s functional status. It was noted that the bone ends were highly sclerotic and massive osteoporosis, and the Ilizarov external fixator could not provide sufficient compression to the fracture site with osteoporosis to avoid pins cutting out. Therefore, this Ilizarov construct was initially planned as a temporary measure till shortening deformity corrected. Although an osteotomy at sclerotic bone and subsequent gradual distraction could allow for new bone regeneration, but the long period required for consolidation of the newly formed bone is the major disadvantage. The consolidation phase may be 3 to 4 times longer than the distraction phase, which may increase the incidence of complications and make the patient eager to have the external fixator removed.6 In addition, the use of Ilizarov external fixator can be psychologically stressful and creates sleeping problems because of its long duration and many other complications. Yiildiz et al7 has reported that there was at least 1 psychiatric symptom in 52.5% of the individuals treated with a circular external fixator in his study. Furthermore, wires and pins of Ilizarov external fixator in the femur invariably transfix quadriceps8 even though we had passed all the wires and the pins in some degrees of knee flexion which inevitably cause discomfort. Total knee arthroplasty (TKA) with a revision component or megaprosthesis is another surgical option for patients with severe osteoporosis. However, TKA can cause various complications such as aseptic loosening, infection, and periprosthetic fractures that are particularly in elderly patients.8-10 More importantly, El-Galaly et al11 has found that previous fractures in the distal femur and/or proximal tibia can increase the risk of early and medium-term revision of TKAs inserted, and the revision due to instability occurred more frequently in TKAs performed as a result of previous fractures. New retrograde nails have developed to increase stability, and biomechanical cadaveric studies showed that they even had a better performance in terms of fatigue resistance in younger patients, however, in elderly individuals with poor bone quality, it’s unsuccessful because such patients have reduced bone volumes and weaker bones as well as joint distortion due to arthritis, in the condition their bones offer little purchase to nails.12,13 Locked plating technique currently remains the standard for osteoporotic fractures of the distal femur and could provide increased stability and resistance to failure compared to retrograde nails in elderly patients with poor bone stock, but hardware breakage and nonunion were often detected by a single-side plate which may be assumed having a sizeable cutting effect upon the loosening bone and lead to failure in the treatment of supracondylar fracture of femur with osteoporosis.14,15 Whereas we preferred the use of the dual plating for the case, which can increase the fracture stabilization similar to the other 2-column fracture types like tibial plateau, distal humerus and plafond fractures.16,17 In our case, surgery was done by 1 incision lateral to femur. Fibrotic areas and bone sequesters were debrided completely, obtained cancellous bone graft from iliac crest placed in the fracture site, direct reduction done followed by temporary fixation with K-wires, and long-locked lateral distal femoral plate used for the lateral column, then, under direct vision with neurovascular protection, a relatively small reconstructive plate was used at anteromedial distal femur for the medial column. At this condition, dual plating could provide rigid fixation in the condylar region of the femur, where thin cortices and frequently poor bone stock make fixation difficult and decrease the lever arm that acts on the femoral axis thereby reduce the load applied at the fracture site and finally overcome these complications such as loosening, breakage, and rotational malposition and allow a greater range of motion of knee achieved by early mobilization immediately after operation. Simultaneously, single incision can significantly lead less periosteal stripping and soft-tissue exposure for plate placement which is required for union and less complications combined with dual plating and cancellous autograft.18-20 At last, in the present case, the patient made satisfactory progress postoperatively without any complications. In the follow-up 2 months after operation, the patient could flex the knee from 0° to 90° and perform partial weight-bearing activities without help of others. Six months after operation, clinical bone healing was achieved and daily activity restores the level before fracture without any pain, swelling, and other complications.
Conclusion
The supracondylar nonunion of femur in elderly patients with osteoporosis is very rare clinically and there is no consensus with regard to the best option of treatment. We deemed the protocol that primarily gradual correction of shortening deformity and soft-tissue contractures with Ilizarov external fixator and subsequently open reduction and fixation using single lateral approach with dual plating as being the most conducive to manage the supracondylar nonunion of femur in elderly patients with osteoporosis. The advantages of the protocol were allowing the patients to move the affected limb and flex the knee, which can prevent limb length discrepancy, neurovascular spasm, and the other complications effectively.
Footnotes
Authors’ Note: The study was approved by the institutional ethics committee.
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
ORCID iD: Nianzong Hou  https://orcid.org/0000-0001-5520-2847
https://orcid.org/0000-0001-5520-2847
References
- 1. Kempf I, Grosse A, Abalo C. Locked intramedullary nailing. Its application to femoral and tibial axial, rotational, lengthening, and shortening osteotomies. Clin Orthop Relat Res. 1986;212:165–173. [PubMed] [Google Scholar]
- 2. Yadav SS. Double oblique diaphyseal osteotomy. A new technique for lengthening deformed and short lower limbs. J Bone Joint Surg Br. 1993;75(6):962–966. [DOI] [PubMed] [Google Scholar]
- 3. Krishnakumar R, Thiruvenkitaprasad G, Kaliaperumal D, Sundaram N. Supracondylar skeletal traction and open interlocking nailing for neglected fracture of the shaft of femur-retrospective study. J Clin Orthop Trauma. 2013;4(3):110–114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Bhave A, Shabtai L, Ong PH, Standard SC, Paley D, Herzenberg JE. Custom knee device for knee contractures after internal femoral lengthening. Orthopedics. 2015, 38(7): e567–e572. [DOI] [PubMed] [Google Scholar]
- 5. El-Sayed M, Atef A. Management of simple (types A and B) closed tibial shaft fractures using percutaneous lag-screw fixation and Ilizarov external fixation in adults. Int Orthop. 2012;36(10):2133–2138. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Kumar R, Mohapatra SS, Joshi N, Goyal SK, Kumar K, Gora R. Primary Ilizarov external fixation in open grade III type C distal femur fractures: our experience. J Clin Orthop Trauma. 2019;10(5):928–933. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Yildiz C, Uzun O, Sinici E, Sabri AA, Ozşahin A, Başbozkurt M. Psychiatric symptoms in patients treated with an Ilizarov external fixator (in Turkish). Acta Orthop Traumatol Turc. 2005;39(1):59–63. [PubMed] [Google Scholar]
- 8. Leino OK, Lempainen L, Virolainen P, Sarimo J, Pölönen T, Mäkelä KT. Operative results of periprosthetic fractures of the distal femur in a single academic unit. Scand J Surg. 2015;104(3):200–207. [DOI] [PubMed] [Google Scholar]
- 9. Loosen A, Fritz Y, Dietrich M. Surgical treatment of distal femur fractures in geriatric patients. Geriatr Orthopc Surg Rehabil. 2019;10:2151459319860723 doi:10.1177/2151459319860723 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Marsland D, Mears SC. A review of periprosthetic femoral fractures associated with total hip arthroplasty. Geriatr Orthop Surg Rehabil. 2012;3(3):107–120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. El-Galaly A, Haldrup S, Pedersen AB, Kappel A, Jensen MU, Nielsen PT. Increased risk of early and medium-term revision after post-fracture total knee arthroplasty. Acta Orthopaedica. 2017;88(3):263–268. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Assari S, Kaufmann A, Darvish K, et al. Biomechanical comparison of locked plating and spiral blade retrograde nailing of supracondylar femur fractures. Injury. 2013;44(10):1340–1345. [DOI] [PubMed] [Google Scholar]
- 13. Yamauchi K, Fushimi K, Shirai G, Fukuta M. Comparison of functional recovery in the very early period after surgery between plate and nail fixation for correction of stable femoral intertrochanteric fractures. Geriatr Orthop Surg Rehabil. 2014;5(2):63–68. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Ricci WM, Streubel PN, Morshed S, Collinge CA, Nork SE, Gardner MJ. Risk factors for failure of locked plate fixation of distal. Femur fractures: An analysis of 335 Cases. J Orthop Trauma. 2014;28(2):83–89. [DOI] [PubMed] [Google Scholar]
- 15. Metwaly RG, Zakaria ZM. Single-incision double-plating approach in the management of isolated, closed osteoporotic distal femoral fractures. Geriatr Orthop Surg Rehabil. 2018;9:2151459318799856 doi:10.1177/2151459318799856 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Leigey DF, Farrell DJ, Siska PA, Tarkin IS. Bicolumnar 90-90 plating of low-energy distal humeral fractures in the elderly patient. Geriatr Orthop Surg Rehabil. 2014;5(3):122–126. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. J James IB, Farrell DJ, Evans AR, Siska PA, Tarkin IS. Open reconstruction of complex proximal metadiaphyseal fragility fractures of the humerus. Geriatr Orthop Surg Rehabil. 2014;5(1):9–13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Doshi HK, Wenxian P, Burgula MV, Murphy DP. Clinical outcomes of distal femoral fractures in the geriatric population using locking plates with a minimally invasive approach. Geriatr Orthop Surg Rehabil. 2013;4(1):16–20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Taormina DP, Shulman BS, Karia R, Spitzer AB, Konda SR, Egol AK. Older age does not affect healing time and functional outcomes after fracture nonunion surgery. Geriatr Orthop Surg Rehabil. 2014;5(3):116–121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Shulman BS, Patsalos-Fox B, Lopez N, Konda SR, Tejwani NC, Egol KA. Do elderly patients fare worse following operative treatment of distal femur fractures using modern techniques? Geriatr Orthop Surg Rehabil. 2014;5(1):27–30. [DOI] [PMC free article] [PubMed] [Google Scholar]