1. Background
The outbreak of 2019 novel coronavirus disease (Covid-19) is deeply weakening the healthcare systems all along the world. This unprecedented crisis impacts the healthcare systems and particularly affects all the geriatric organisations, from the hospital ward to nursing homes.
After two months of pandemic, France has more than 29,000 dead people due to the Covid-19 and, older adults are paying a heavy price [1]. Indeed, 89% of hospital deaths are among people aged 65 and over [1]. Also, deaths in nursing homes account for almost 40% of all deaths [1], while nursing homes residents represent only 1% of the French population [2]. The mortality of nursing home residents is probably underestimated because when they die in hospital, they are counted as hospital deaths, according to the French organisation. These points indicate how Covid-19 is a major geriatric issue [3], [4]. French hospital geriatric departments are mobilized to make the patient flow easier, ensuring continuity of care and coordinating all healthcare professionals.
Covid-19 often causes respiratory syndromes such as hemodynamic or respiratory insufficiency, dyspnea, or chest pain [5]. Clinical data show a modified clinical presentation (diarrhoea, unusual falls, confusion, etc.) in older adults, making the evocation of diagnosis more difficult [6], [7], [8]. In older adults, without a clear respiratory presentation, the symptoms listed above should make one think about Covid-19. Elderly patients then find themselves exposed to new infectious history in a context of major frailty that can lead to decompensation linked to the geriatric syndromes [9]. In this context, it is therefore fundamental to consider not only Covid-19 infection management but also global geriatric care lessening the risk of this cascading decompensation [10]. This pandemic required a major and rapid reorganisation of all the healthcare offer in general and in geriatrics in particular, to optimize the patient flow [11].
This article reports the impact of the pandemic of Covid-19 on geriatric wards and describes the whole reorganisation implemented to be able to receive Covid patients, as to maintain the usual care of non-Covid patients. Tools already used in practice, such as the telephone hotline and hospital mobile teams have been transformed into special Covid tools to optimize the patient flow.
2. Geriatric ecosystem
The Geriatric Department of the University Hospital of Saint-Etienne covers all the need for older patients care, with short-stay geriatric units, rehabilitation care units and healthcare teams working as out of the hospital teams. In the city of Saint-Etienne and its metropolitan area, there are around forty nursing homes. Before the Covid-19 epidemic, the University Hospital of Saint-Etienne proposed hotline designed to enhance general practitioner (GP) clinic-hospital interactions by phone [9]. This system has shown a positive effect on the number of emergency department visits, whose deleterious effects are described in the literature and provide support to GPs in caring for older adults.
3. Reorganisation of wards
Consequently, geriatric hospitalization wards have been reorganized to continue to receive their usual patients in dedicated sectors (Covid−). Elderly Covid+ patients, coming from home or nursing homes, are now cared in dedicated units. The organization of this patient flow allows having two distinct sectors:
A high viral density sector enables medical care and/or to avoid contamination of those fragile close of the hospitalized patient (partner, or other nursing homes residents), until Day 21 of symptoms.
A second sector with a lower viral density after Day 21. This sector enables to anticipate the return home or to nursing homes in complete safety with adapted precautions (hygiene). Collaboration is thus initiated with external contributors (home hospitalization team, private nurses, home help structures) to optimize patient care and any future complications.
During hospitalization, a standardized geriatric assessment is performed to assess the patient's physical and cognitive abilities. Thus, it enables to fight indirectly against the contagiousness by adapting as well as possible the recommendations for barrier gestures.
Our teams were able to design complete flow for older Covid+ patients in just a few weeks with the creation of dedicated services, geriatric Covid-19 telephone hotlines, dedicated beds for patients from nursing homes and mobile geriatric teams visiting nursing homes. This specific organization was possible through the measures of the French government following the consensus of the French geriatric and gerontological structures [12], [13].
Extensive knowledge of the geriatric ecosystem and a major investment by all the involved structures and professionals facilitated reaching this result. This organization enabled to offer geriatric care both within hospital structures and within nursing homes. Moreover, it has strengthened and improved patient care provision. One of the difficulties encountered has been the ability to sectorize and isolate patients. In the future, architectural projects construction of care facilities will have to take into account the risk of epidemics and the necessity to build additional single rooms to isolate the patients. We believe that it will be necessary to work with hygienists to make these projects feasible.
4. Modification of city/hospital link tools
The creation of a specific Covid-19 telephone hotline allowed a direct link between structures such as nursing homes and the hospital centre. These telephone hotlines, which are a specific plan between GP and nursing homes to hospital geriatricians, are endowed with mobile teams to assess and assist in the care of residents in these structures. Also initiated via the Covid-19 telephone hotline, establishment of mass screening is an important new central element in reorganisation and patient orientation (Fig. 1 ). Our choice of screening strategy in nursing homes is also shared by other researchers [14], [15].
Fig. 1.
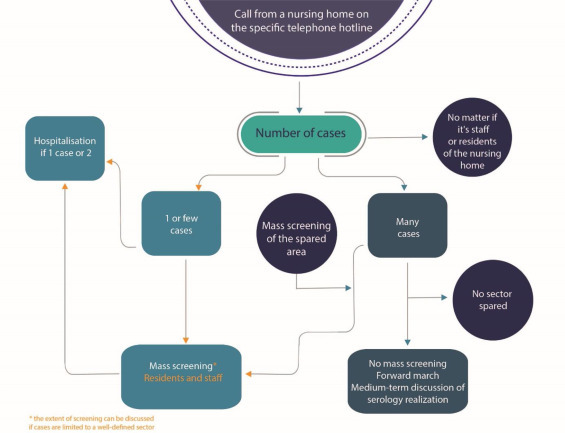
Decision process for care management and mass screening for patients with Covid-19 in nursing homes.
Source: own creation.
Associated with this new organization, mobile teams propose medical care to nursing home patients at their places of residence and, if necessary, in coordination with the palliative care and/or home hospitalization teams [16], [17]. The mobile teams have also dedicated beds at their disposal to hospitalize residents of nursing homes requiring it, or to hospitalize the first cases of Covid-19 to try to avoid any epidemic within the nursing homes. No epidemics have been noticed following the eviction of patients with Covid-19 from nursing homes. This organization allows the hospital to be as close as possible to the actors of the city. It also makes it possible to propose direct and rapid hospital care, without going through an emergency department, sometimes responsible for hospital iatrogeny [7].
Many people tested positive to Covid-19 were asymptomatic and certainly contributed to transmission [14]. Mass screening is a key element in the global reorganization. Thus, its repetition appears logical in nursing homes in the event of new cases. Moreover, the close city/hospital link, via mobile hygiene teams, enables to reduce the risk of epidemics in nursing homes through training interventions, particularly on the barrier gestures to adopt during this epidemic.
This global care provision, trying to take into account the pressure on the health care system but also the risk of contamination of the patient's entourage, is probably not only a factor of good medical care but also a fundamental element in breaking the chain of contamination.
The Covid-19 epidemic and the urgency induced by this situation contributed to improving our model of health organizations. We believe that based on this experience and framework, this organization can be sustainable to face a new wave of Covid-19 but also in case of seasonal flu or other infectious diseases.
5. Conclusion
Hospitalization of older adults living in nursing homes and infected with Covid-19 was not a situation envisaged initially. Given the situation and particularly in nursing homes, an adaptation of dedicated hotlines and mobile hospital teams improved the management of the patient's flow. Indeed, through to the coordination that these tools allow, patients can be directly orientated to the appropriate sector. Our system highlighted the interest of these tools that promote the city/hospital link. Sustainability of these services seems necessary.
Sponsor's role
Not applicable.
Disclosure of interest
The authors declare that they have no competing interest.
Acknowledgments
We acknowledge Dr. L. Bertoletti who prodived language help and proofed read the article.
References
- 1.Santé Publique France. Infection au nouveau Coronavirus (SARS-CoV-2), COVID-19, France et Monde [Internet]. [cité 25 mars 2020 ; disponible sur : https://www.santepubliquefrance.fr/maladies-et-traumatismes/maladies-et-infections-respiratoires/infection-a-coronavirus/articles/infection-au-nouveau-coronavirus-sars-cov-2-covid-19-france-et-monde].
- 2.Ministère des Solidarités et de la Santé. Infographie : L’hébergement des personnes âgées en établissement — Les chiffres clés [Internet]. [cité 26 avr 2020 ; disponible sur : https://www.drees.solidarites-sante.gouv.fr/etudes-et-statistiques/publications/infographies/article/infographie-l-hebergement-des-personnes-agees-en-etablissement-les-chiffres].
- 3.Applegate W.B., Ouslander J.G. COVID-19 presents high risk to older persons. J Am Geriatr Soc. 2020;68:681. doi: 10.1111/jgs.16426. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Promislow D.E.L. A geroscience perspective on COVID-19 mortality. J Gerontol A Biol Sci Med Sci. 2020 doi: 10.1093/gerona/glaa094. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Lechien J.R., Chiesa-Estomba C.M., Place S., Van Laethem Y., Cabaraux P., Mat Q., et al. Clinical and epidemiological characteristics of 1420 European patients with mild-to-moderate coronavirus disease. J Intern Med. 2019:2020. doi: 10.1111/joim.13089. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Liu K., Chen Y., Lin R., Han K. Clinical features of COVID-19 in elderly patients: a comparison with young and middle-aged patients. J Infect. 2020 doi: 10.1016/j.jinf.2020.03.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Niu S., Tian S., Lou J., Kang X., Zhang L., Lian H., et al. Clinical characteristics of older patients infected with COVID-19: a descriptive study. Arch Gerontol Geriatr. 2020;89:104058. doi: 10.1016/j.archger.2020.104058. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Godaert L., Proye E., Demoustier-Tampere D., Coulibaly P.S., Hequet F., Dramé M. Clinical characteristics of older patients: the experience of a geriatric short-stay unit dedicated to patients with COVID-19 in France. J Infect. 2020 doi: 10.1016/j.jinf.2020.04.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Martinez L., Lacour N., Gonthier R., Bonnefoy M., Goethals L., Annweiler C., et al. Impact of geriatric hotlines on health care pathways and health status in patients aged 75 years and older: protocol for a French Multicenter Observational Study. JMIR Res Protoc. 2020;9:e15423. doi: 10.2196/15423. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Preventing chaos in a crisis strategies for damage limitation by Patrick Lagadec — AbeBooks [Internet]. [cité 26 avr 2020 ; disponible sur : https://www.abebooks.co.uk/book-search/title/preventing-chaos-in-a-crisis-strategies-for-damage-limitation/author/patrick-lagadec/].
- 11.Koeberle S, Tannou T, Bouiller K, Becoulet N, Outrey J, Chirouze C, et al. COVID 19 outbreak: organisation of a geriatric assessment and coordination unit. A French example. Age Ageing [Internet]. [cité 24 mai 2020 ; disponible sur : https://www.academic.oup.com/ageing/advance-article/doi/10.1093/ageing/afaa092/5831132]. [DOI] [PMC free article] [PubMed]
- 12.Jeandel C. Olivier Véran; 2020. Lettre ouverte au ministre des Solidarités et de la Santé. [Google Scholar]
- 13.Info Coronavirus COVID-19. Gouvernement.fr.
- 14.Arons M.M., Hatfield K.M., Reddy S.C., Kimball A., James A., Jacobs J.R., et al. Presymptomatic SARS-CoV-2 infections and transmission in a skilled nursing facility. N Engl J Med. 2020 doi: 10.1056/NEJMoa2008457. [0:null] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Asymptomatic transmission, the Achilles’ heel of current strategies to control Covid-19 | NEJM [Internet]. [cité 26 avr 2020 ; disponible sur :https://www.nejm.org/doi/full/10.1056/NEJMe2009758]. [DOI] [PMC free article] [PubMed]
- 16.Borasio G.D., Gamondi C., Obrist M., Jox R. For the Covid-Task Force of palliative ch null. COVID-19: decision making and palliative care. Swiss Med Wkly. 2020;150:w20233. doi: 10.4414/smw.2020.20233. [DOI] [PubMed] [Google Scholar]
- 17.Powell V.D., Silveira M.J. What should palliative care's response be to the COVID-19 pandemic? J Pain Symptom Manage. 2020 doi: 10.1016/j.jpainsymman.2020.03.013. [DOI] [PMC free article] [PubMed] [Google Scholar]


