1. Introduction
Though the exact etiology of autoimmune diseases still remains unknown, there are various factors which are believed to contribute to the emergence of an autoimmune disease in a host including the genetic predisposition, the environmental triggers such as bacterial infections, including the gut microbiota, viral fungal and parasitic infections, as well as physical and environmental agents, hormonal factors and the hosts immune system dysregulation. All these factors interplay was coined by Shoenfeld et al., many years ago “The Mosaic of Autoimmunity” [[1], [2], [3], [4]]. The most prominent pathogenic viruses which have been proposed in the triggering and initiation of autoimmune diseases include: Parvovirus B19, Epstein-Barr-virus (EBV), Cytomegalovirus (CMV), Herpes virus-6, HTLV-1, Hepatitis A and C virus, and Rubella virus [[5], [6], [7], [8], [9], [10], [11]]. These viruses have been implicated in the initiation of chronic inflammatory or autoimmune diseases such as rheumatoid arthritis, systemic lupus erythematosus, Sjogren's syndrome, primary billiary cholangitis, multiple sclerosis, polymoysitis, uveitis, Henoch Schonlein Puprpura, Systemic Juvenile Idiopathic arthritis, systemic sclerosis, Hashimoto thyroiditis and autoimmune hepatitis [12,13]. Suggested mechanisms of induction of the autoimmunity include both molecular mimicry [14] as well as “bystander activation” whereby the infection may lead to activation of antigen presenting cells that may in turn activate pre-primed auto-reactive T-cells, thus leading to the production of pro-inflammatory mediators, which in turn may lead to tissue damage [15]. Alternative suggested mechanisms include epitope spreading as well as presentation of cryptic antigens [16].
Corona viruses represent a major group of viruses mostly affecting human beings through zoonotic transmission. In the past two decades, this is the third instance of the emergence of a novel coronavirus, after the severe acute respiratory syndrome (SARS) in 2003 and the Middle East respiratory syndrome coronavirus (MERS-CoV) in 2012 [17,18]. In December 2019 a novel outbreak of a new strain of coronavirus infection emerged in Wuhan, China the SARS-CoV-2 or the Covid-19. The disease which was declared as a pandemic in early March 2020, is characterized by fever, dry cough, myalgia and or extreme fatigue, may be asymptomatic or with minimal flu-like constitutional symptoms leading to a favorable outcome in many instances. However, some of the patients encounter a severe pneumonia with sepsis leading to an acute respiratory distress syndrome (ARDS) with respiratory failure requiring mechanical ventilation, and at times accompanied by hyperferritinemia and multiple organ involvement including hematological, gastrointestinal, neurological and cardiovascular complications leading to death [[19], [20], [21], [22], [23]]. The ARDS described in up to 20% of Covid-19 cases, is reminiscent of the cytokine release syndrome-induced ARDS and secondary hemophagocytic lymphohistiocytosis (sHLH) observed in patients with SARS-CoV and MERS-CoV as well as in leukemia patients receiving engineered T cell therapy. These cases with Covid-19 are those who develop through the excessive cytokine release and the uncontrolled immune activation, the multiorgan failure with a grave prognosis [24,25].
2. Autoimmune diseases / syndromes potentially associated with Covid-19 described so far
It has been suggested that the shared pathogenetic mechanisms and clinical-radiological aspects between the hyper-inflammatory diseases and Covid-19 may suggest that SARS-CoV-2 could act as a triggering factor for the development of a rapid autoimmune and/or autoinflammatory dysregulation, leading to the severe interstitial pneumonia, in genetic predisposed individuals [26]. Furthermore, in an online pre-published study from Germany the authors studied prospectively a group of 22 patients for the possible role of autoimmunity in SARS-CoV-2 -associated respiratory failure. Based on serological, radiological and histomorphological similarities between Covid-19-associated ARDS and acute exacerbation of connective tissue disease induced interstitial lung disease, the authors suggest that SARS-CoV-2 infection might trigger or simulate a form of organ specific autoimmunity in predisposed patients [27]. In a similar retrospective study from China of 21 patients with critical SARS-CoV-2 pneumonia, the authors showed a prevalence of between 20 and 50% of autoimmune disease related autoantibodies, suggesting the rational for immunosupression in such cases of Covid-19 [28].
3. Immune thrombocytopenic purpura – ITP secondary to COVID-19
Immune thrombocytopaenic purpura (ITP) is an autoimmune systemic disease manifested by the presence of low blood platelets count (<10 [5]/μl) and the production of autoantibodies against glycoproteins expressed on the platelet surface. The clinical course is often acute, and life-threatening events may occur especially in children, with 52% of pediatric patients recovering either spontaneously or after treatment. A chronic ITP evolution is observed in 64% of adults, of whom 12% will develop an overlapping autoimmune disease. Several microbial infections as well as viruses including CMV, EBV parvovirus, rubella, measles or HIV can potentially trigger ITP through molecular mimicry [29,30].. The association between ITP and Covid-19 has been suggested in a single case report of a 65-year-old female patient with a background history of hypertension, autoimmune hypothyroidism, and positive swab for Covid-19 who presented with fever, dry cough and signs of pneumonia. Laboratory studies were within normal limits and she was treated by intra-venous amoxicillin–clavulanic acid, low-molecular weight heparin and oxygen. The normal platelet count on admission had gradually dropped to 66,000 and later to 8000 per cubic millimeter on day seven accompanied by classical lower-extremity purpura and epistaxis. Both heparin and the antibiotics were discontinued. She was treated by two rounds of IVIG while the platelets had drooped even further to 1000 per cubic millimeter followed by the onset of right frontal headache, with a CT of the head demonstrating subarachnoid microhemorrhage. A platelet transfusion was administered with concurrent starting of 100 mg of prednisolone. On day 10, the headache had resolved with no new neurologic findings, and the platelet count had gradually increased to 139,000 on day 13 with a complete resolution of the purpura. The temporal sequence in this case suggests, but does not prove, that the ITP was triggered by the Covid-19 especially in view of the history of autoimmune hypothyroidism which is often associated with ITP. There are however other potential causes for the thrombocytopenia in this case such as the treatment with amoxicillin–clavulanic acid as well as the known heparin-induced-thrombocytopenia (HIT) [31,32]. Another report by Tsao et al. currently online, describes a case of SARS-CoV-2 positive pediatric patient with ITP and raises the awareness of ITP as a possible pediatric presentation of the virus [33].
4. Guillian-Barrė syndrome (GBS) secondary to COVID-19
GBS is a progressive, ascending, symmetrical flaccid limbs paralysis, along with areflexia or hyporeflexia with or without cranial nerve involvement which can progress over days to weeks. The disease may be triggered by respiratory or intestinal infections or vaccinations. The known triggering infections include Influenza; Chlamydia; CMV; varicella; mumps; rubella; HIV; Polio; Hepatitis E; Borrelia; Mycoplasma pneumonia as well as Campilobacter Jejuni. GBS is an immune-mediated disorder with molecular mimicry playing an important role in its autoimmune disorder in which the immune system attacks gangliosides on the peripheral nervous system [34,35]. There are so far 2 reports of GBS associated with Covid-19 infection [36,37]. It is yet unclear whether Covid-19 induces the production of antibodies against these specific gangliosides. The first is a report of five out of 1200 patients hospitalized between February 28th and March 21st, 2020 in Northern Italy hospitals. The onset of neurological symptoms began 7–10 days after the initial respiratory symptoms. Four out of the 5 patients had lower-limb weakness and paresthesia and one was with facial diplegia followed by ataxia and paresthesia. Generalized, flaccid tetraparesis or tetraplegia evolved over a period of 36 h to 4 days in 4 of the patients. Three of them required mechanical ventilation. Anti-ganglioside antibodies were either negative or not done. All patients received IVIG (1 of then required 2 cycles) and one had started plasma exchange. The second report from Iran describes a 65 year old male patient admitted to hospital because of acute progressive symmetric ascending quadriparesis, two weeks after a history of cough, fever and dyspnea. Covid-19 was diagnosed by RT-PCR. The patient was treated by hydroxychloroquine, Lopinavir/Ritonavir, and Azithromycin. GBS was confirmed by EMG. The patient was treated by IVIG for 5 days. Another early report of a single GBS patient came from China during the SARS-CoV-2 epidemic, although there is some concern regarding the causality in this particular case [38].
5. Miller Fisher syndrome (MFS) secondary to COVID-19
MFS is a rare, acquired disease that is considered to be a mild variant of Guillain-Barré syndrome, and is observed in about 5% of all cases of GBS. It is characterized by a triad of ataxia, areflexia, and ophthalmoplegia. Acute onset of external ophthalmoplegia is a cardinal feature. Ataxia tends to be out of proportion to the degree of sensory loss. Patients may also have mild limb weakness, ptosis, facial palsy, or bulbar palsy. Occasionally generalized muscle weakness and respiratory failure may develop. Patients have reduced or absent sensory nerve action potentials and absent tibial H reflex. Like GBS, symptoms may be preceded by a viral illness. The majority of individuals with MFS have unique antibodies that characterize the disorder, which are Anti-GQ1b and anti-GD1b antibodies. Dense concentrations of GQ1b ganglioside are found in the oculomotor, trochlear, and abducens nerves, which may explain the relationship between anti-GQ1b antibodies and ophthalmoplegia. Treatment for MFS is identical to treatment for GBS: intravenous immunoglobulin (IVIG) or plasmapheresis. A group from Spain reported of two patients infected with SARS-CoV-2 who acutely presented with MFS and polyneuritis cranialis respectively. Both patients presented with the typical neurological symptoms. One of the two patients was found to be positive for anti-GD1b-IgG antibodies and was treated with IVIG and the second patient with acetaminophen. Two weeks later, both patients made a complete neurological recovery, except for residual anosmia and ageusia in the first case [39].
6. Antiphospholipid antibodies and thrombosis secondary to COVID-19
Deep vein thrombosis, pulmonary embolism and stroke have been observed in patients affected by severe forms of COVID-19 [40,41]. These vascular events, particularly strokes, were mostly recorded in elderly patients [41]. However, 5 cases of stroke were recently reported in relatively young patients (age range: 33–49 years), in association with prolonged activated partial-thromboplastin time (aPTT) in 2 cases [42].
Vascular manifestations of COVID-19 comprise either venous or arterial thrombosis or stroke in subjects under the age of 50, sometimes with a severe phenotype that can resemble the “catastrophic” clinical picture associated with antiphospholipid antibodies (aPL). In patients with systemic autoimmune diseases such as Systemic Lupus Erythematosus (SLE), aPL represent the major cause of thrombosis (either arterial or venous or microangiopathic) and pregnancy morbidity. aPL are pathogenic autoantibodies that can cause the same vascular and obstetric manifestations also in subjects without any other autoimmune disease, suffering from the so called Primary Antiphospholipid Syndrome (APS) [43]. The more severe form of APS (the “catastrophic” APS, CAPS) is characterized by a rapidly occurring multiorgan thrombotic damage with histopathological evidence of microangiopathy [44], recalling pictures described in patients with COVID-19. CAPS is usually preceded by a precipitating factor, which is an infection in the majority of the cases [45]. The link between infection and aPL was first observed when patients with different autoimmune conditions were found to be positive for the serological test of syphilis, whose antigen was described as a mixture of phospholipids, including cardiolipin [46]. Nowadays, the detection of aPL is performed by anticardiolipin (aCL) and anti-beta2glicoprotein I (anti-b2GPI) immunoassays and by the functional coagulation test lupus anticoagulant (LA), according to the international consensus APS classification criteria [47].
Three cases of COVID-19 patients with severe thrombotic events associated with aCL and anti-b2GPI were recently reported [48]. Specifically, aCL of IgA isotype and anti-b2GPI of IgG and IgA isotype were detected, raising the hypothesis that the mucosal damage induced by SARS-CoV-2 could preferentially stimulate the IgA immune response. LA was found to be negative in these 3 patients.
On the other hand, LA was found to be positive in 25 out of 56 (44.6%) consecutive COVID-19 patients, while IgG/IgM aCL and/or anti-b2GPI were positive only in 5 (8.9%). No specific relation with thrombosis was mentioned in this cohort [49].
In addition, LA was studied in patients with prolonged aPTT, a finding that has been frequently reported in COVID-19. More than 90% of patients with prolonged aPTT, with or without clinical evidence of thrombosis, resulted positive for LA [50].
Another study investigated patients with acute respiratory distress syndrome and COVID-19 from intensive care units. In this study, 50 out of 59 (84.7%) tested patients had LA positive, strongly associated with high D-dimers and thrombosis, particularly if the test was performed early in the disease course. In this series only one patient had positive aCL of IgM isotype [51].
Therefore, we can assume that aPL can be frequently detected in patients with SARS-CoV-2 infection. Certainly, this finding is not surprising [52]. In fact, the occurrence of transient aPL was described in patients affected by several viral infections such as human immunodeficiency virus (HIV), varicella zoster, hepatitis C virus, cytomegalovirus (CMV), Epstein–Barr virus (EBV), adenovirus, parvovirus B19 [53]. In addition, aPL were also detected in patients with infections of different origin (bacterial, parasitic, etc) and an infection was often reported just before the clinical onset of APS [54]. These observations suggest the possible existence of molecular mimicry due to similarity between the peptide regions identified in the b2GPI molecule (and recognized by anti-b2GPI) and membrane proteins of several virus and bacteria [55]. Animals immunized with different viruses or bacteria (or proteins derived from them) developed anti-b2GPI antibodies that in some cases were associated with the occurrence of thrombosis [56]. The different pathogenic potential of antibodies can be attributed to the fine specificity that they acquire after immunization with different antigens. It is in fact known that antibodies directed to domain 1 of the b2GPI molecule are associated with an increased risk of thrombosis (in systemic autoimmune diseases and APS) [57] while antibodies directed to other parts of the molecule, such as domain 4/5, can be regarded as “innocent” [58]. On the other hand, the features of the host can also be important, since genetic background is recognized as one of the determinant factors in the induction of autoimmunity and can be the driver which turns aPL from being transient to persistent and pathogenic [59].
The above considerations widely justify why aPL, detected with different assays, can be found in patients affected by COVID-19, sometimes associated with thrombosis but not always. To our knowledge, no increased rate of miscarriages or fetal loss have been reported during SARS-CoV-2 pandemic so far, although some severe pregnancy complication, like those linked to aPL, such as HELLP syndrome were occasionally seen (A. Lojacono, personal communication). Whether pregnant women with COVID-19 have an increased rate of positive aPL during pregnancy is not known yet nor it is defined their possible impact on pregnancy outcome. COVID-19 is a novel infectious disease. The true relationship between this infection and aPL need to be further investigated. However, according to the “second hit hypothesis” [60], the thrombogenic potential of aPL is magnified in the presence of an infection or a severe inflammatory state, which is often associated with COVID-19. Therefore, the search for aPL may be considered in the management of COVID-19 patients with vascular manifestations, as the detection of positive aPL would allow of the indication for an early adequate anticoagulant treatment. In the case of aPL positivity, a follow-up testing after at least 12 weeks is warranted, in order to verify the persistence of aPL, which would suggest the post-infectious occurrence of APS. In fact, APS is currently considered as a systemic autoimmune disease which is not limited to thrombosis and pregnancy morbidity and deserves specific long-term management including anticoagulation and immunomodulation.
7. Kawasaki like disease secondary to COVID-19
Kawasaki disease (KD) is a systemic vasculitis that usually affects children less than 5 years old. Soon after the first description by Tomisaku Kawasaki in 1967, it was clear that the disease, although self-limiting, might cause coronary artery aneurism (CAA) in a high percentage of cases [61]. KD is nowadays considered as the first cause of acquired heart disease in children from developed countries [62]. The disease is far more common in eastern countries, and in children of eastern origin living in western countries. For example, the 2010 annual incidence for KD was 222.9 cases/100000 children <5 y/o in Japan, compared to 20/100000 in the USA [63,64]. Since no specific test is available, diagnosis relies on the recognition of the cardinal clinical features and the exclusion of other mimickers. The mainstay of treatment is the administration of intravenous immunoglobulins (IVIG) at 2 g/kg of body weight, as soon as the diagnosis is established, and possibly within 10 days from the onset of fever. IVIG have been demonstrated to reduce the risk of CAA [65]. A subgroup of patients, accounting for nearly 5% of those with KD, has been described to have a very severe disease onset with systolic hypotension or shock (Kawasaki Shock Syndrome-KSS). The shock may be caused by a capillary leak syndrome or by poor perfusion due to inflammatory myocarditis. KSS patients are more likely to be females and to have earlier onset, incomplete presentations, and more severe laboratory abnormalities (lower platelet counts, higher serum CRP levels, hyponatremia, increased transaminases, metabolic acidosis, consumptive coagulopathy, and lower serum albumin levels). Patients with KSS are often resistant to IVIG treatment and have a higher incidence of coronary artery aneurysms, mitral regurgitation, and prolonged myocardial dysfunction [66].
Northern Italy was the first European region to be severely hit by the SARS-COV2 epidemic after the original outbreak in China [67]. Although the data on the clinical presentation of COVID-19 in children is still scarce, lower rates of infection and milder forms of disease seem to be typical of this age group [68,69]. Since the end of March 2020, we observed and treated or received information from all over Italy about an abnormally elevated number of critically ill patients with clinical characteristics consistent with Kawasaki Shock Syndrome (KSS). The common features were: “middle-aged” children (6–9 y/o) with a history of persistent high spiking fever in the previous days, abdominal pain, diarrhea, skin rash, and rapidly deteriorating clinical conditions with the onset of shock, without clear signs of dehydration. Other less common features were arthralgia, cough, meningism, conjunctivitis and reddened, cracked lips. Labworks usually showed high inflammatory markers, low lymphocyte count, low sodium, and high troponin and pro-BNP levels. Echocardiography was consistent with myocarditis in the majority of patients instead of classical coronary artery abnormalities. Patients were diagnosed as Kawasaki disease (typical or incomplete) and treated accordingly with IVIG and/or steroids. One patient refractory to such treatments responded successfully to intravenous anakinra. Althoug all the patients had family contacts consistent with COVID-19, serology and nasopharyngeal swabs were inconsistently positive both in the single patients and among all children. To date we are aware of at least 10 cases of KSS possibly related to COVID-19. Given the unprecedented cluster of patients we decided to launch a nationwide alert for pediatricians and start a national registry. Few days after the diagnosis of our first cases, news from all over Europe first, and Eastern USA thereafter, reported on the identification of patients with remarkably the same characteristics we have observed. Some children with a less severe picture, without shock at the onset, but with clinical characteristics of systemic inflammation and some features of KD have also been seen by us and others (personal communications). These observations lead to a variety of nationwide alerts in the respective countries [70,71]. On May 7, 2020, Riphagen et al. published on 8 patients treated at the South Thames Retrieval Service for a severe acute illness similar to KSS [72]. Age at presentation was between 4 and 14 years, 6 out of 8 children were of Afro-Caribbean descent and 5 were boys. All the children had a similar disease onset with persistent fever, skin rash, conjunctivitis, peripheral oedema, and extremity pain. Gastrointestinal symptoms were frequent and severe, all children developed shock requiring ICU admission and vasopressors. Another key feature described in those patients was the cardiac involvement, as testified by very elevated cardiac enzymes, and echo-bright coronary vessels. One patient developed a giant coronary aneurism. Lab works typically showed high C-reactive protein, procalcitonin, ferritin, triglycerides, and D-dimers. All children were treated with IVIG (2 g/kg) and 6 also received aspirin (50 mg/kg). Broncho-alveolar lavage or nasopharyngeal aspirates were negative for SARS-COV-2 in all children; some of the patients had histories of familial contact with the virus. The authors stated that, at the time they were writing their report, another ICU in London managed 20 patients with similar characteristics. As per the Royal College of Pediatrics and Child Health (RCPCH) alert, some of these patients resulted to be positive for SARS-CoV-2 infection, by either nasopharyngeal swab, serology, or both [69]. The New York State Department of Health reported sixty-four cases as of May 5th 2020. For the purpose of this review we will refer to this clinical entity as Pediatric COVID-19 Hyperinflammatory Syndrome (PeCOHS), while the English authorities refers to it as Pediatric inflammatory multisystem syndrome temporally associated with SARS-CoV-2 infection (PIMS-TS).
Verdoni et al. published the first Italian experience on 10 patients admitted to their hospital for Kawasaki-like disease from February 18th to April 20th, 2020 (during the peak of COVID19 epidemic in Italy). Very nicely, the authors compared these children (group 2) to the historical cohort of KD patients seen in the last 5 years (group 1, 19 patients). Half of the children in group 2 presented with classic KD, while half were diagnosed as incomplete KD. Half of the patients showed hypotension and signs of hypoperfusion at onset, and were interpreted as KSS, and half had signs of myocarditis at echocardiogram. Pro-BNP was above normal values in all the patients. Half of the patients satisfied the PRINTO laboratory criteria for Macrophage Activation Syndrome (MAS) [73]. Two patients developed CAAs. Patients in group 2 displayed older age, a higher frequency of gastrointestinal and respiratory symptoms, meningeal signs, myocarditis, shock syndrome, and MAS criteria as compared with group 1. Nasopharyngeal swab for SARS-CoV-2 was positive in 2 patients only, 8 patients had positive IgG while 3 patients had positive IgM (all of whom were positive also for IgG) for SARS-CoV-2. All patients from group 2 were treated with IVIG and steroids, with good clinical outcome [74].
The occurrence of such cases with a stereotyped clinical picture, which is rarely seen in children, during the peak of SARS-CoV2 infection in highly epidemic areas, points to a causative link. One hypothesis is that these children were suffering from actual KD triggered by the SARS-CoV-2 virus. Indeed, a microbial etiology has been long advocated as a possible cause for KD. Many viruses (HHV-6, Epstein Barr virus, Cytomegalovirus, Coronavirus other than SARS-CoV-2, Parvovirus B19 etc.) but also bacterial infections (such as staphylococci, streptococci, Bartonella, and Yersinia) have been linked to KD. Interestingly enough, a case of classic KD has been recently reported in a 6 months-old child who tested positive for SARS-CoV-2, although this could be just coincidental [75]. The clinical and laboratory characteristics of the patients recently described are strikingly similar to the KSS typical picture, except for the older age, male predominance and relatively low frequency of coronary artery aneurysms [65]. Given these differences, it can be speculated that this COVID-19 Hyperinflammatory Syndrome is indeed a systemic vasculitis peculiar of the pediatric age and caused by SARS-CoV-2 infection.
How SARS-CoV-2 infection may cause a hyperinflammatory syndrome? At this point we can only formulate hypotheses, based on the clinical picture of the observed patients and using other diseases with overlapping manifestations, such as KD and Toxic Shock Syndrome (TSS), as models. The delay between the pandemic peak of COVID-19 and the occurrence of this hyperinflammatory syndrome in children does not point to a direct effect of the infection, but rather towards an immune-mediated disease. This seems to be confirmed also by the observation of Verdoni et al. that the majority of their patients had positive SARS-CoV-2 IgG, but negative IgM and swabs. Staphylococcal or Streptococcal TSS are the result of T cells induction by superantigens TSST-1, enterotoxins B or C (staphylococci), or pyrogenic exotoxin A or B (streptococci). Superantigens can stimulate clonal T cell proliferation and this leads to the production of massive amounts of pro-inflammatory cytokines, as IL-1, IL-6, and IFN-γ in a so-called cytokine storm [76]. There is a body of evidence suggesting that KD may be caused by a superantigen response, and recent data demonstrated that KSS is characterized by a massive pro-inflammatory cytokine release that differentiate those patients from the “regular” KD patients [77]. This cytokine storm could be the underlying mechanism leading to the clinical picture similar of that of TSS, KSS, and PeCOHS.
Other possible mechanisms by which SARS-CoV-2 could induce a hyperinflammatory syndrome are: i) the autoantibodies formation through “molecular mimicry”, as in Acute Rheumatic Fever (although this mechanism would not justify the occurrence of shock); ii) a vascular damage secondary to the deposition of immune-complexes as in acute serum sickness; iii) an antibody-dependent enhancement (ADE) with IgG immune complexes that enhance virus infection in Fc-receptor-bearing cells. Intriguingly, this phenomenon is the cause of Dengue vascular permeability syndrome, which, again, shares some similarities with PeCOHS [78]. ADE were demonstrated in SARS-CoV infection years ago, mediated by antibodies directed to the envelope spike proteins [79].
Children with SARS-CoV-2 infection usually have a benign course [67]. Differently from what we usually see in Kawasaki Disease, which has a predilection for asian countries, PeCOHS has not been described so far in those countries, suggesting that both the genetic predisposition of the host and differences in the viral genome may play a role in this disease.
To our knowledge, the majority of patients with PeCOHS respond to a variable combination of steroids and IVIG. The discussion about the immunomodulatory effects of both steroids and IVIG is beyond the scope of this review, but it is interesting to highlight that one of the many effects of IVIG is the down modulation of superantigens [80]. Of note, IVIG is the therapy of choice in the capillary leak syndrome, whose main features are similar to KSS and PeCOHS [81]. Finally, the efficacy of anti-IL-1 treatment as “rescue therapy” for cases resistant to IVIG+steroids points out the relevance of this pro-inflammatory cytokine in the hyperinflammatory state, similar to what already shown in adults with COVID-19 and hyperinflammation [82].
In conclusion, although SARS-CoV-2 infection appears to occur as a oligo-symptomatic form in the majority of children, there is mounting evidence that it can cause a systemic hyperinflammatory syndrome that mimics KSS, but has some peculiar features. The role of host and virus genetics and the exact immune mechanisms leading to the disease are far from been understood, and case collection would help us in better characterization of the clinical phenotype. As light has been shed on the interaction between SARS-CoV-2 and the immune system, we will gain hints also at Kawasaki Disease pathogenesis, almost 50 years from its first description by Tomisaku Kawasaki.
8. Preexisting autoimmune rheumatic diseases and COVID-19 infection
Since the breakout of the Covid-19 in late 2019 in China, many unresolved issues regarding both dealing with the fate of the preexisting autoimmune rheumatic diseases in patients who are affected by the virus including those under immunosuppressive and biologic therapy, as well as the impact of these therapies on the severity of the viral disease itself. Early reports in the course of the pandemia suggested that based on the data recovered from other and previous viral infections, there would be an increased probability for patients with rheumatic diseases to acquire the Covid-19 disease or are they prone to an increased severity of the infection if they do acquire it. On the contrary, however, early on, there was some evidence regarding the potential benefit of some of the drugs which have been used in the therapy of rheumatic disease [83,84].
Patients with SLE had posed a serious concern during the Covid-19 pandemia. This group of patients is well known to bear an increased risk of severe infections, due to both their immune system and the related organ damage as well as due to the therapies used including immunosuppressive drugs. In a report of 19 SLE patients from France who were clinically quiescent on a long-term treatment with Hydroxychloroquine (HCQ) and were infected by the Covid-19 virus, the authors were able to conclude that the clinical course of these lupus patients did not show any signs of the disease exacerbation, except for a single case of tenosynovitis [85]. A preliminary analysis of patients included in the COVID-19 Global Rheumatology Alliance registry, showed that 17% of 110 patients with rheumatic diseases who have been diagnosed with COVID-19 as of April the 1st, 2020- were patients with lupus [86]. Thus the frequency of patients with lupus who have been diagnosed with COVID-19 was over-represented, at about twice as compared to rheumatoid arthritis which is a much commoner rheumatic disease among the adult population. In a recent small report from northern Italy of SLE patients with either swab confirmed Covid-19 infection (n = 4) or a clinical diagnosis, based on 3 out of 4 symptoms of the viral infection (n = 8), the authors stated that the disease course was generally mild and self-resolving although one of the four patients who was on haemodialysis due to end-stage renal disease, needed intensive care for the development of acute respiratory distress syndrome [87]. Based on the clinical information published to date from the new and previous outbreaks caused by the coronaviruses, there is no overwhelming evidence that patients with rheumatic disease are at an increased risk compared with other comorbidities [[88], [89], [90]]. In a rather larger prospective report from New York, the authors reviewed a group of 86 patients with immune-mediated inflammatory disease including 59 cases of inflammatory arthritides (rheumatoid arthritis, psoriatic arthritis, ankylosing spondylitis, psoriasis and inflammatory bowel disease) with confirmed Covid-19, and 27 additional patients with suspected Covid-19 [91]. Two-thirds of the patients were on biologics or other immunomodulatory drugs. Hospitalized patients, as compared to those who were only followed on an out-patient basis, had more classical Covid-19 comorbidities. Conventional DMARDs were used more frequently in the hospitalized group of patients, whereas biologics were more often used in the ambulatory group of patients. The authors suggest that based on their findings the baseline use of biologics was not associated with worse Covid-19 outcomes. In another small report from China five patients with rheumatic disease and Covid-19 are described [92]. Four had rheumatoid arthritis and one with systemic sclerosis. All 5 patients had chest CT showing patchy ground glass opacities in the lungs. All 5 patients were treated with antiviral agents, antibiotics and the immunomodulatory agents for their rheumatic disease. Two of the 5 patients remained in stable condition in the course of the hospitalization, 2 progressed to severe Covid-19 and one was critically ill, though all patients recovered and were discharged from hospital. Similarly, a report by Monti et al. [93] suggested that patients with rheumatoid arthritis treated with biological DMARDs or targeted synthetic DMARDs did not seem to be at increased risk of life-threatening complications from Covid-19 compared with the general population. Another recent study from Italy supports the approach of encouraging connective tissue disease patients to maintain the ongoing rheumatologic therapy as well as adhere to the measures of infection prevention, thus avoiding relapse of the rheumatic disease without increasing the risk of Covid-19 [94]. Their study population included 123 adult patients (110 females) with systemic lupus erythematosus (n = 61), systemic sclerosis (n = 43), undifferentiated connective tissue disease (n = 9) and Sjogren syndrome (n = 10). About 60% of the patients were treated with conventional DMARDs, with a similar percentage of patients taking corticosteroids as well. Twenty five of the 110 patients received biologics. Only one rather young female patient with systemic sclerosis was found to be positive for Covid-19 and developed a critical course with interstitial pneumonia leading to her death despite intubation and an attempt with tocilizumab. A further 14 patients reported mild respiratory symptoms compatible with a viral infection but did not have access to a swab test and showed a rapid recovery of their symptoms. The authors concluded that only 5 out of their 123 patients had discontinued their current rheumatological therapy, with none of the rest 115 patients experiencing flare-ups of their disease. Similarly, Conticini et al recently reported of a large cohort of 859 patients from Italy affected by different rheumatic diseases, which were treated by biological DMARDs or by targeted synthetic DMARDs [95]. Only 2 patients who were both on biologics (rituximab or tocilizumab), were diagnosed with COVID-19, one of which even with bilateral diffuse interstitial pneumonia. Both patients had a complete recovery without interruption of the biological treatment. Similar favorable outcome has been reported for few cases with large-vessel vasculitis and granulomatosis with polyangiitis associated with Covid-19 infection [96,97]. Thus it seems that baseline use of biologics is not associated with worse Covid-19 outcomes. The situation might be different with patients suffering from systemic sclerosis, where the typical interstitial lung disease (ILD) could share some CT features with Covid-19 associated pneumonia [[98], [99], [100]]. Currently the impact of pre-existing systemic sclerosis associated with pulmonary and cardiac involvement, on the course of Covid-19 is yet unknown. Such a single case with scleroderma associated ILD and polyarthritis, who had been previously treated with anti-interleukin-6 receptor blocker (Tocilizumab) with a favorable response, was recently reported [101]. In the course of this therapy, 4 weeks after the last tocilizumab infusion, she reported a contact with Covid-19 and was found to be positive for the virus by a nasopharyngeal swab. Her condition remained stable during the course of the acute disease and following a negative swab and cure, she had received the next scheduled tocilizumab injection. It should be noted that early reports from China during the outbreak of the SARS-Cov2 were able to demonstrate increased levels of IL-6 and CRP, suggesting that this subgroup of patients may develop the Covid19 related cytokine storm. Randomized trials using anti-IL-6 receptor monoclonal antibody are currently ongoing. Recently many countries and organizations have set up registries incorporating patients with pre-existing rheumatic and autoimmune diseases who had encountered a Covid-19 infection. The largest international registries include The Global Rheumatology Alliance of Covid-19 and the Eular Covid-19 database.
9. Therapy - using rheumatologic drugs in COVID-19 infection
Many countries and organizations have published guidelines for treatment of the COVID-19 pandemic. Of note are the Treatment Guidelines of the National Institutes of Health and the American College of Rheumatology guidance for the management of adult patients with rheumatic disease during the COVID-19 pandemic [102,103].
Chloroquine and Hydroxychloroquine, are anti malarial drugs, used to treat autoimmune diseases, such as systemic lupus erythematosus (SLE) and rheumatoid arthritis (RA). Both chloroquine and hydroxychloroquine (HCQ) have immunomodulatory effects. In general, HCQ has fewer and less severe toxicities (including fewer propensities to prolong the QTc interval) and fewer drug-drug interactions than chloroquine. The proposed mechanisms of action and rationale for use for COVID-19 of both drugs have to do with the increase of the endosomal pH, inhibiting fusion of the severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) and the host cell membranes. Furthermore, Chloroquine inhibits glycosylation of the cellular angiotensin-converting enzyme 2 receptor, which may interfere with binding of SARS-CoV to the cell receptor. In vitro, both chloroquine and HCQ may block the transport of SARS-CoV-2 from early endosomes to endolysosomes, which may be required for release of the viral genome, and several studies have demonstrated in vitro activity of chloroquine against SARS-CoV [104,105]. Though HCQ has been administered to patients with Covid-19 there are to date no robust evidence supporting its use. In a retrospective computerized database of 1317 positive subjects for Covid-19 out of a sample size of 14,520, a comparison was conducted between those who tested positive versus those who were found negative, in terms of the rate of administration of HCQ or colchicine. The authors did not find any significant difference in terms of the rates of usage of either drug, thus they concluded that their findings raise doubts regarding the protective role of both these medication in the battle against SARS-CoV-2 infection [106]. Similar results were drawn by a study from a large medical center in New York. The authors examined the association between HCQ use and intubation or death among a group of 1446 consecutive patients. HCQ administration was not associated with either a greatly lowered or an increased risk of intubation or death [107]. Many similar reports came to the same conclusions [[108], [109], [110]], to the extent that the FDA has issued a safety alert and the American College of Physicians has as well recommended against the use of chloroquine or HCQ for COVID-19 [111,112]. Furthermore, an attempt to evaluate HCQ serum or plasma levels from various rheumatic disease patients receiving this treatment, found that these plasma or serum levels were unlikely to achieve the concentration shown to inhibit SARS-CoV-2 in vitro (average target 0.48 mg/L as opposed to the antiviral target of 4/1 mg/L) [113].
10. Anti-IL-6 receptor antibodies – Tocilizumab and Sarilumab
IL-6 is a pleiotropic, pro-inflammatory cytokine produced by a variety of cell types, including lymphocytes, monocytes, and fibroblasts. Infection by the related SARS-CoV induces a dose-dependent production of IL-6 from bronchial epithelial cells. Elevations in IL-6 levels may be an important mediator when severe systemic inflammatory responses occur in patients with SARS-CoV-2 infection. COVID-19-associated systemic inflammation and hypoxic respiratory failure is associated with an acute cytokine release, as indicated by elevated blood levels of IL-6, C-reactive protein (CRP), D-dimer, and ferritin [[114], [115], [116]]. Few clinical studies aiming to evaluate the efficacy of anti-IL-6 receptor blocker have been published so far. In a report from China by Xu et al. the authors were able to show that tocilizumab effectively improved clinical symptoms as well as reversed the deterioration of sever Covid-19 patients [117]. Within 5 days after tocilizumab, 15 of the 20 patients had lowered their oxygen intake and 19 of the 20 showed a noticeable improvement in the CT of the lungs, as well as a significant reduction in CRP levels which was noted in 16 of the 19 patients. All patients have been discharged on an average of 15 days after the tocilizumab dosing. Even though this is a small and uncontrolled study, the results seem to be impressive. Over 20 randomized controlled trials with tocilizumab, or sarilumab as well as JAK-inhibitors as baricitinib, are underway.
11. Interleukin-1 (IL-1) inhibitors – Anakinra
Anakinra is a recombinant human IL-1 receptor antagonist. It is approved to treat rheumatoid arthritis and cryopyrin-associated periodic syndromes, and it is also used off-label for a variety of inflammatory conditions and severe chimeric antigen receptor T cell (CAR-T)-mediated cytokine release syndrome (CRS) and macrophage activation syndrome (MAS)/secondary hemophagocytic lymphohistiocytosis. A case series of anakinra use in moderate to severe COVID-19 pneumonia has recently been published [118]. This small study of 9 patients with moderate to severe Covid-19 pneumonia, who did not reach respiratory failure and were given anakinra (Anti-IL-1), serves as a proof of concept since all 9 patients had dropped their fever,
CRP levels had dropped and normalized in 5 out of 8 patients at day 11. CT scans did not deteriorate and all were alive at the last follow up. Similar results were reached in a retrospective study from Italy of 16 patients with Covid-19 and adult respiratory distress syndrome who were managed with non-invasive ventilation outside of the ICU. Treatment with high-dose anakinra was found to be safe and associated with clinical improvement in 72% of the patients [119].
12. Covid-19 and autoimmunity: The role of molecular mimicry
Notwithstanding the current wave of intensive worldwide research, the ethiopathology of the diseases induced by the SARS-CoV-2 infection is the central question that remains obscure. One likely explanation is that the heterogeneity and multitude of the disorders induced by the current pandemic derive from molecular mimicry phenomena between the virus and human proteins. The scientific rationale is that, following the infection, the immune responses raised against SARS-CoV-2 may cross-react with human proteins that share peptide sequences with the virus, in this way leading to autoimmune pathologic sequelae [120]. Actually, a recent report [121] militates in this direction and likely explains lungs and airways dysfunctions through the sharing of peptides between SARS-CoV-2 glycoprotein and alveolar lung surfactant proteins [121]. Moreover, in the clinical context exposed above, it is of note to report that Sars.CoV-2 shares 6 minimal immune determinants (KTVLK, TPEEH, RETMS, PFVVS, GLEAP, ICLLQ) with the Kawasaki antigen Inositol-trisphosphate 3-kinase C [122], thus highlighting as likely cross-reactions and consequent autoimmune Kawasaki disease in predisposed subjects. Even more impressing it appears the heptapeptide sharing between the human proteome and the viral spike glycoprotein shown in Table 1 . The clinical scenario that emerges is upsetting. Indeed, the list of proteins reported in the table – when altered – configurate almost all the diseases that have been described in association with SARS-CoV-2. Two examples from the table are 1) Histone-lysine N-methyltransferase 2C that may associate with neurodevelopmental disorders., seizures, behavioral abnormalities [123], and 2) Interleukin-7 that plays a central, critical role in the regulation of the immune system and associates with severe lymphopenia when deficient [124].
Table 1.
Heptapeptide sharing between SARS-CoV-2 spike glycoprotein and the human proteins.
| Peptide | Human Protein Name |
|---|---|
| SSTASAL | 40S ribosomal protein S13 |
| KLNDLCF | Interleukin-7 |
| FLPFFSN | OTU domain-containing protein 6A |
| EIDRLNE | Protein SET |
| IGAGICA | Hepatitis A virus cellular receptor 2 |
| EIDRLNE | Protein SETSIP |
| LDKYFKN | Follistatin-related protein 1 |
| VSGTNGT | Lysosome-associated membrane glycoprotein 1 |
| FKNLREF | Isovaleryl-CoA dehydrogenase, mitochondrial |
| LPPLLTD | Maestro heat-like repeat-containing protein family member 9 |
| DKVFRSS | Zinc finger protein 528 |
| LVKQLSS | E3 SUMO-protein ligase PIAS1 |
| VTLADAG | Non-receptor tyrosine-protein kinase TNK1 |
| RRARSVAS | Amiloride-sensitive sodium channel subunit alpha |
| SPRRARS | Hermansky-Pudlak syndrome 1 protein |
| KVEAEVQ | EMILIN-3 |
| TRFQTLL | Disheveled-associated activator of morphogenesis 2 |
| VYSTGSN | Neural cell adhesion molecule L1-like protein |
| GLTVLPP | FH1/FH2 domain-containing protein 3 |
| SLLIVNN | ATP-binding cassette sub-family A member 10 |
| DEDDSEPV | Unconventional myosin-XVI |
| NASVVNI | Thyroid adenoma-associated protein |
| LIRAAEI | Unconventional myosin-XVIIIa |
| TGRLQSL | Neuron navigator 3 |
| DEVRQIA | Histone-lysine N-methyltransferase 2C |
| SSSGWTA | Transmembrane protein KIAA1109 |
Data on protein function/disease from Uniprot (https://www.uniprot.org/).
Sequential overlapping heptapeptides are given bold.
13. The Covid-19 vaccine and the constraint of molecular mimicry
The extent of the molecular mimicry between SARS-CoV-2 and the human proteome should be carefully analyzed as a mandatory step preliminarily to any vaccine formulation As a matter of fact, because of the pathogen–host peptide commonality, a potential consequence of vaccination might consist of a specific autoimmune reactions hitting self-antigens such as the already analyzed alveolar surfactant protein [121]. Only peptide sequences uniquely belonging to the virus can represent the basis for safe and specific vaccinations protocols [[125], [126], [127]].
14. Probable histopathological signs of autoimmune reactions in COVID-19
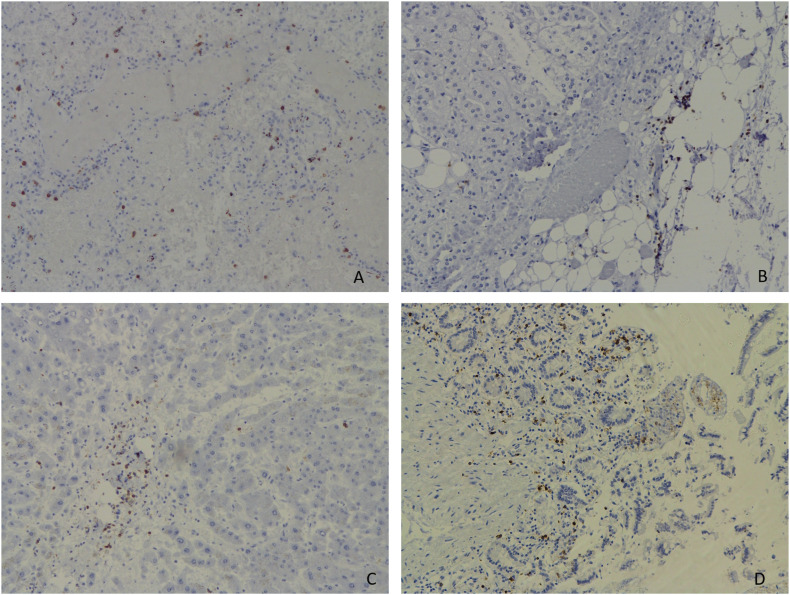
Based upon the possibility to detect autoimmune reactions by morphological methods we analyzed autopsies from 18 deceased patients from COVID-19. The pathological investigation was done by using bright lineage of immunohistochemistry (CD2, 3, 5, 7, 8, 20, 31, 34, 69). Our study allowed us to demonstrate the role of different mechanisms of death [128]. Of special interest was the diffuse infiltration of the lungs, along with focal infiltration of the kidney, liver, intestine, adrenals, pancreas and pericard by lymphocytes, which were seen in different grade in all our cases. In order to understand its nature we were able to prove that the infiltrate was dominated by T lymphocytes (CD3+), and the most numerous of them were CD8+ suppressors, observed in the lungs (Fig. 1a), adrenals (Fig. 1b), liver (Fig. 1c), intestine (Fig. 1d) and other organs partly accompanied by tissue lesions. Taking in to consideration that one of the most important mechanisms of autoimmune reactions is CD8+ T Cell mediated cytotoxicity, we assumed that the findings confirm an autoimmune process. Further complex studies will hopefully allow us to optimize the strategy of treatment as well.
Fig. 1.
Infiltration by CD8+ suppressor T-cells of different organs. IHC. Magnification 100. A-Lungs, B -Adrenal gland, C-liver, D- intestine.
References
- 1.Shoenfeld Y., Isenberg D.A. Elsevier; Holland: 1989. The mosaic of autoimmunity. [p.523] [DOI] [PubMed] [Google Scholar]
- 2.Amital H., Gershwin E.M., Shoenfeld Y. Reshaping the mosaic of autoimmunity. Semin Arthritis Rheum. 2006;35:341–343. doi: 10.1016/j.semarthrit.2005.09.002. [DOI] [PubMed] [Google Scholar]
- 3.Buskila D., Sikuler E., Shoenfeld Y. Hepatitis C virus, autoimmunity and rheumatic disease. Lupus. 1997;6:685–690. doi: 10.1177/096120339700600902. [DOI] [PubMed] [Google Scholar]
- 4.Cohen A., Shoenfeld Y. The viral autoimmunity relationship. Viral Immunol. 1995;8:1–9. doi: 10.1089/vim.1995.8.1. [DOI] [PubMed] [Google Scholar]
- 5.Barzilai O., Ram M., Shoenfeld Y. Viral infection can induce the production of autoantibodies. Curr Opin Rheumatol. 2007;19:636–643. doi: 10.1097/BOR.0b013e3282f0ad25. [DOI] [PubMed] [Google Scholar]
- 6.Watad A., Amital H., Shoenfeld Y. The environment in autoimmune diseases. Harefuah. 2015;154:308–311. [PubMed] [Google Scholar]
- 7.Barzilai O., Sherer Y., Ram M. Epstein–Barr virus and cytomegalovirus in autoimmune diseases are they truly notorious? A preliminary report. Ann N Y Acad Sci. 2007;1108:567–577. doi: 10.1196/annals.1422.059. [DOI] [PubMed] [Google Scholar]
- 8.Ram M., Gershwin M.E., Shoenfeld Y. Hepatitis B virus (HBV) and autoimmune disease. Clin Rev Allergy Immunol. 2008;34:85–102. doi: 10.1007/s12016-007-8013-6. [DOI] [PubMed] [Google Scholar]
- 9.Pablobic M., Kats A., Carvall M., Shoenfeld Y. Clinical and molecular evidence for association of SLE with parvovirus B19. Lupus. 2010;19:783–792. doi: 10.1177/0961203310365715. [DOI] [PubMed] [Google Scholar]
- 10.Li Sakkas, Bogdanos D.P. Infections as a cause of autoimmune rheumatic diseases. Auto Immun Highlights. 2016;7:13. doi: 10.1007/s13317-016-0086-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Shoenfeld Y., Selmi C., Zimlichman E., Gershwin M.E. The autoimmunologist: geoepidemiology, a new center of gravity, and prime time for autoimmunity. J Autoimmun. 2008;31:425–430. doi: 10.1016/j.jaut.2008.08.004. [DOI] [PubMed] [Google Scholar]
- 12.Selmi C., Leung P.S. Sherr DH et al; mechanisms of environmental influence on human autoimmunity: a National Institute of Environmental Health Sciences expert panel workshop. J Autoimmun. 2012;39:272–284. doi: 10.1016/j.jaut.2012.05.007. [DOI] [PubMed] [Google Scholar]
- 13.Floreani A., Leung P.S.C., Gershwin M.E. Environmental basis of autoimmunity. Cinic Rev Allerg Immunol. 2016;50:287–300. doi: 10.1007/s12016-015-8493-8. [DOI] [PubMed] [Google Scholar]
- 14.Ercolini A.M., Miller S.D. The role of infections in autoimmune diseases. Clin Exp Immunol. 2009;155:1–15. doi: 10.1111/j.1365-2249.2008.03834.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Fujinami R.S., von Herrath M.G., Christen U. Molecular mimicry, bystander activation, or viral persistence: infections and autoimmune disease. Clin Microbiol Rev. 2006;19:80–94. doi: 10.1128/CMR.19.1.80-94.2006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Hussein H.M., Rahal E.A. The role of viral infections in the development of autoimmune diseases. Crit Rev Microbiol. 2019;45:394–412. doi: 10.1080/1040841X.2019.1614904. [DOI] [PubMed] [Google Scholar]
- 17.Zhong N.S., Zheng B.J., Li Y.M. Epidemiology and cause of severe respiratory syndrome (SARS) in Guangdong, People’s Republic of China in February 2003. Lancet. 2003;362:1353–1358. doi: 10.1016/S0140-6736(03)14630-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Ramadan N., Shaib H. Middle East respiratory syndrome coronavirus (MERS-CoV): a review. Germs. 2019;9:35042. doi: 10.18683/germs.2019.1155. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Guan W.J., Ni Z.Y., Hu Y. Clinical characteristics of coronavirus disease 2019 in China. NEJM. 2020;382:1708–1720. doi: 10.1056/NEJMoa2002032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Wang L., Wang Y., Ye D. Review of the 2019 novel coronavirus (SARS-CoV-2) based on current evidence. Int J Antimicrob Agents. 2020;105948 doi: 10.1016/j.ijantimicag.2020.105948. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Zandman-Goddard G., Shoenfeld Y. Hyperferritinemia in autoimmunity. IMAJ. 2008;10:83–84. [PubMed] [Google Scholar]
- 22.Shoenfeld Y. COVID-19 Corona virus- disease of year 2019. Harefuah. 2020;159:224–225. [PubMed] [Google Scholar]
- 23.Colafrancesco S., Alessandri C., Conti F. Covid-19 gone bad: a new character in the spectrum of the hyperferritinemic syndrome? Autoimmun Rev. 2020 doi: 10.1016/j.autrev.2020.102573. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Moore J.B., June C.H. Cytokine release syndrome in severe COVID-19. Science. 2020 doi: 10.1126/science.abb8925. [DOI] [PubMed] [Google Scholar]
- 25.Henderson L.A., Schulert G.S., Carricchio R. 2020. On the alert for cytokine storm: Immunopathology in COVID-19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Caso F., Costa L., Ruscitti P. Could Sars-coronavirus-2 trigger autoimmune and / or autoinflammatory mechanisms in genetically predisposed subjects? Autoimmun Rev. 2020 doi: 10.1016/j.autrev.2020.102523. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Gagiannis D., Steinestel J., Hackenbroch C. 2020. COVID-19-induced acute respiratory failure-an exacerbation of organ-specific autoimmunity? [DOI] [Google Scholar]
- 28.Zhou Y., Han T., Chen J. Clinical and autoimmune characteristics of severe and critical cases with COVID-19. Clin Translat Sci. 2020 doi: 10.1111/CTS.12805. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Rinaldi M., Perricone C., Ortega-Hernandez O.-D. Immune Thrombocytopaenic Purpura: an autoimmune cross-link between infections and vaccines. Lupus. 2014;23:554–567. doi: 10.1177/0961203313499959. [DOI] [PubMed] [Google Scholar]
- 30.Elalfy M.S., Nugent D. Viruses, anti-viral therapy and viral vaccines in children with immune thrombocytopenia. Semin Hematol. 2016;53(Suppl. 1):S70–S72. doi: 10.1053/j.seminhematol.2016.04.021. [DOI] [PubMed] [Google Scholar]
- 31.Zulfiqar A.-A., Lorenzo-Villalba N.-L., Hassler P. Immune thrombocytopenic purpura in a patient with Covid-19. NEJM. 2020 doi: 10.1056/NEJMc2010472. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Lippi G., Plebani M., Henry B.M. Thrombocytopenia is associated with severe coronavirus disease 2019 (COVID-19) infections: a meta-analysis. Clin Chim Acta. 2020;506:145–148. doi: 10.1016/j.cca.2020.03.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Tsao H.S., Chason H.M., Fearon D.M. Immune thrombocytopenia (ITP) in a SARS-CoV-2 positive pediatric patient. Pediatrics. 2020 doi: 10.1542/peds.2020-1419. [DOI] [PubMed] [Google Scholar]
- 34.Israeli E., Agmon-Levin N., Blank M. Guillain-Barrė syndrome- a classical autoimmune disease triggered by infection or vaccination. Clin Rev Allergy Immunol. 2012;42:121–130. doi: 10.1007/s12016-010-8213-3. [DOI] [PubMed] [Google Scholar]
- 35.Shoenfeld Y., George J., Peter J.B. Guillain-Barre as an autoimmune disease. Int Arch Allergy Immunol. 1996;109:318–326. doi: 10.1159/000237258. [DOI] [PubMed] [Google Scholar]
- 36.Toscano G., Palmerini F., Ravaglia S. Guillain-Barrė syndrome associated with SARS-CoV-2. NEJM. 2020 doi: 10.1056/NEJMc2009191. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Seaghat Z., Karimi N. Guillain-Barrė syndrome associated with COVID-19 infection: A case report. J Clin Neurosci. 2020 doi: 10.1016/j.jocn.2020.04.062. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Zhao H., Shen D., Zhou H. Guillain-Barrė syndrome associated with SARS-CoV-2 infection: causality or coincidence? Lancet Neurol. 2020;19:383–384. doi: 10.1016/S1474-4422(20)30109-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Gutiėrrez-Ortiz C., Mėndez A., Rodrigo-Ray S. Miller Fisher syndrome and polyneuritis cranialis in COVID-19. Neurology. 2020 doi: 10.1212/WNL.0000000000009619. [DOI] [PubMed] [Google Scholar]
- 40.Xie Y., Wang X., Yang P., Zhang S. COVID-19 complicated by acute pulmonary embolism. Radiology: Cardiothoracic Imaging. 2020;2 doi: 10.1148/ryct.2020200067. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Li Y., Wang M., Zhou Y., Chang J., Xian Y., Mao L. 2020. Acute Cerebrovascular Disease Following COVID-19: A Single Center, Retrospective, Observational Study. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Thomas J., Oxley J. Mocco, Majidi Shahram. Large-Vessel Stroke as a Presenting Feature of Covid-19 in the Young. NEJM. April 28, 2020 doi: 10.1056/NEJMc2009787. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Khamashta M., Taraborelli M., Sciascia S., Tincani A. Antiphospholipid syndrome. Best Pract Res Clin Rheumatol. 2016 Feb;30(1):133–148. doi: 10.1016/j.berh.2016.04.002. [DOI] [PubMed] [Google Scholar]
- 44.Espinosa G., Rodríguez-Pintó I., Cervera R. Catastrophic antiphospholipid syndrome: an update. Panminerva Med. 2017 Sep;59(3):254–268. doi: 10.23736/S0031-0808.17.03324-9. [DOI] [PubMed] [Google Scholar]
- 45.Cervera R., Bucciarelli S., Espinosa G., Gómez-Puerta J.A., Ramos-Casals M., Shoenfeld Y. Catastrophic antiphospholipid syndrome: lessons from the ‘CAPS registry’ a tribute to the late Josep Font. Ann N Y Acad Sci. 2007;1108:448–456. doi: 10.1196/annals.1422.047. [DOI] [PubMed] [Google Scholar]
- 46.Pangborn M.C. A new serologically active phospholipid from beef heart. Proc Soc Exp Biol. 1941;48:484–486. [Google Scholar]
- 47.Miyakis S., Lockshin M.D., Atsumi T. International consensus statement on an update of the classification criteria for definite antiphospholipid syndrome (APS) J Thromb Haemost. 2006;4(2):295–306. doi: 10.1111/j.1538-7836.2006.01753.x. [DOI] [PubMed] [Google Scholar]
- 48.Zhang Yan, Xiao Meng, Zhang Shulan. 2020. Coagulopathy and antiphospholipid antibodies in patients with Covid-19 NEJM April 8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Harzallah I., Debliquis A., Drénou B. Lupus anticoagulant is frequent in patients with Covid-19. J Thromb Haemost. 2020 Apr 23 doi: 10.1111/jth.14867. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Bowles L., Platton S., Yartey N., Dave M., Lee K., Hart D.P. Lupus anticoagulant and abnormal coagulation tests in patients with Covid-19. N Engl J Med. 2020 May 5 doi: 10.1056/NEJMc2013656. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Helms J., Tacquard C., Severac F., Leonard-Lorant I., Ohana M., Delabranche X. High risk of thrombosis in patients with severe SARS-CoV-2 infection: a multicenter prospective cohort study. Intensive Care Med. 2020 May 4 doi: 10.1007/s00134-020-06062-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Sène D., Piette J.C., Cacoub P. Antiphospholipid antibodies, antiphospholipid syndrome and infections. Autoimmun Rev. 2008;7(4):272–277. doi: 10.1016/j.autrev.2007.10.001. [DOI] [PubMed] [Google Scholar]
- 53.Uthman I.W., Gharavi A.E. Viral infections and antiphospholipid antibodies. Semin Arthritis Rheum. 2002;31:256–263. doi: 10.1053/sarh.2002.28303. [DOI] [PubMed] [Google Scholar]
- 54.Torres Ruiza J., Blank M., Zandman-Goddardc G., Sherer Y., Shoenfeld Y. Antiphospholipid antibodies and their relationship with infections, vaccines, and drugs. In: Cervera R., Espinosa G., Khamashta M., editors. Antiphospholipid Syndrome in Systemic Autoimmune Diseases. Vol. 10. The Netherlands: Elsevier Publisher; Amsterdam: 2016. pp. 167–179. [Google Scholar]
- 55.Blank M., Krause I., Fridkin M., Keller N., Kopolovic J., Goldberg I. Bacterial induction of autoantibodies to beta-2-glycoprotein-I accounts for the infectious etiology of antiphospholipid syndrome. J Clin Invest. 2002;109(6):797–804. doi: 10.1172/JCI12337. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Pierangeli S.S., Blank M., Liu X., Espinola R., Fridkin M., Ostertag M.V. A peptide that shares similarity with bacterial antigens reverses thrombogenic properties of antiphospholipid antibodies in vivo. J Autoimmun. 2004;22(3):217–225. doi: 10.1016/j.jaut.2004.01.002. [DOI] [PubMed] [Google Scholar]
- 57.Pengo V., Ruffatti A., Tonello M., Cuffaro S., Banzato A., Bison E. Antiphospholipid syndrome: antibodies to domain 1 of β2-glycoprotein 1 correctly classify patients at risk. J Thromb Haemost. 2015 May;13(5):782–787. doi: 10.1111/jth.12865. [DOI] [PubMed] [Google Scholar]
- 58.Andreoli L., Chighizola C.B., Nalli C. Clinical characterization of antiphospholipid syndrome by detection of IgG antibodies against β2 -glycoprotein i domain 1 and domain 4/5: ratio of anti-domain 1 to anti-domain 4/5 as a useful new biomarker for antiphospholipid syndrome. Arthritis Rheum. 2015 May;67(8):2196–2204. doi: 10.1002/art.39187. [DOI] [PubMed] [Google Scholar]
- 59.Soriano A., Blank M., Shoenfeld Y. Genetics and origin of antiphospholipid syndrome. In: Meroni P.L., editor. Antiphospholipid antibody syndrome. From bench to bedside. Cham: Springer I; 2014. pp. 1–12. [Google Scholar]
- 60.Shoenfeld Y., Blank M., Cervera R., Font J., Raschi E., Meroni P.L. Infectious origin of the antiphospholipid syndrome. Ann Rheum Dis. 2006;65:2–6. doi: 10.1136/ard.2005.045443. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Burns J.C. Commentary: translation of Dr. Tomisaku Kawasaki’s original report of fifty patients in 1967. Pediatr Infect Dis J. 2002;21:993–995. doi: 10.1097/00006454-200211000-00002. [DOI] [PubMed] [Google Scholar]
- 62.McCrindle B.W., Rowley A.H., Newburger J.W. Diagnosis, treatment, and long-term management of Kawasaki disease: a scientific statement for health professionals from the American Heart Association. Circulation. 2017;135:e927–e999. doi: 10.1161/CIR.0000000000000484. [DOI] [PubMed] [Google Scholar]
- 63.Nakamura Y., Yashiro M., Uehara R. Epidemiologic features of Kawasaki disease in Japan: results of the 2009-2010 nationwide survey. J Epidemiol. 2012;22:216–221. doi: 10.2188/jea.JE20110126. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Holman R.C., Belay E.D., Christensen K.Y. Hospitalizations for Kawasaki syndrome among children in the United States, 1997-2007. Pediatr Infect Dis J. 2010;29:483–488. doi: 10.1097/INF.0b013e3181cf8705. [DOI] [PubMed] [Google Scholar]
- 65.Furusho K., Nakano H., Shinomiya K. High-dose intravenous gammaglobulin for kawasaki disease. Lancet. 1984;324:1055–1058. doi: 10.1016/S0140-6736(84)91504-6. [DOI] [PubMed] [Google Scholar]
- 66.Taddio A., Rossi E.D., Monasta L. Describing Kawasaki shock syndrome: results from a retrospective study and literature review. Clin Rheumatol. 2017;36:223–228. doi: 10.1007/s10067-016-3316-8. [DOI] [PubMed] [Google Scholar]
- 67.Covid-19 situation in Italy. http://www.salute.gov.it/portale/nuovocoronavirus/dettaglioContenutiNuovoCoronavirus.jsp?lingua=english&id=5367&area=nuovoCoronavirus&menu=vuoto Accessed 27 Apr 2020.
- 68.Jiatong S., lanqin L., Wenjun L. COVID-19 epidemic: disease characteristics in children. J Med Virol. 2020 doi: 10.1002/jmv.25807. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Carsetti R., Quintarelli C., Quinti I. The immune system of children: the key to understanding SARS-CoV-2 susceptibility? Lancet Child Adolesc Heal. 2020 doi: 10.1016/S2352-4642(20)30135-8. 0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Royal College of Pediatrics and Child Health Guidance Paediatric multisystem inflammatory syndrome temporally associated with COVID-19. https://www.rcpch.ac.uk/sites/default/files/2020-05/COVID-19-Paediatric-multisystem-inflammatory syndrome-20200501.pdf Accessed 8 May 2020.
- 71.Pediatric Intensive Care Society PICS Statement Increased number of reported cases of novel presentation of multisystem inflammatory disease. https://picsociety.uk/wp-content/uploads/2020/04/PICS-statement-re-novel-KD-C19-presentation-v2-27042020.pdf
- 72.Riphagen S., Gomez X., Gonzalez-Martinez C. Hyperinflammatory shock in children during COVID-19 pandemic. Lancet. 2020 doi: 10.1016/S0140-6736(20)31094-1. 0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Ravelli A., Minoia F., Davì S. 2016 classification criteria for macrophage activation syndrome complicating systemic juvenile idiopathic arthritis: a European league against rheumatism/American college of rheumatology/Paediatric rheumatology international trials organisation collaborative initiative. Ann Rheum Dis. 2016;75:481–489. doi: 10.1136/annrheumdis-2015-208982. [DOI] [PubMed] [Google Scholar]
- 74.Verdoni L., Mazza A., Gervasoni A. An outbreak of severe Kawasaki-like disease at the Italian epicentre of the SARS-CoV-2 epidemic: an observational cohort study. Lancet. 2020 doi: 10.1016/S0140-6736(20)31103-X. 0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Jones V.G., Mills M., Suarez D. COVID-19 and Kawasaki disease: novel virus and novel case. Hosp Pediatr. 2020 doi: 10.1542/hpeds.2020-0123. [DOI] [PubMed] [Google Scholar]
- 76.Burnham J.P., Kollef M.H. Understanding toxic shock syndrome. Intensive Care Med. 2015;41:1707–1710. doi: 10.1007/s00134-015-3861-7. [DOI] [PubMed] [Google Scholar]
- 77.Li Y., Zheng Q., Zou L. Kawasaki disease shock syndrome: clinical characteristics and possible use of IL-6, IL-10 and IFN-γ as biomarkers for early recognition. Pediatr Rheumatol. 2019;17 doi: 10.1186/s12969-018-0303-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Halstead S.B. Dengue antibody-dependent enhancement: knowns and unknowns. Microbiol Spectr. 2014;2 doi: 10.1128/microbiolspec.aid-0022-2014. [DOI] [PubMed] [Google Scholar]
- 79.Wang S.F., Tseng S.P., Yen C.H. Antibody-dependent SARS coronavirus infection is mediated by antibodies against spike proteins. Biochem Biophys Res Commun. 2014;451:208–214. doi: 10.1016/j.bbrc.2014.07.090. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Lindquist M.E., Hicar M.D. B cells and antibodies in Kawasaki disease. Int J Mol Sci. 2019;20 doi: 10.3390/ijms20081834. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Asmundsson A.S.E., Bjorklund A.R., Fisher G.A. Diagnosis of systemic capillary leak syndrome in a young child treated with intravenous immunoglobulin in the acute phase. J Pediatr intensive care. 2018;7:94–96. doi: 10.1055/s-0037-1607342. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Cavalli G., De Luca G., Campochiaro C. Interleukin-1 blockade with high-dose anakinra in patients with COVID-19, acute respiratory distress syndrome, and hyperinflammation: a retrospective cohort study. Lancet Rheumatol. 2020 doi: 10.1016/S2665-9913(20)30127-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Figueroa-Parra G., Aguirre-Garcia G.M., Gamboa-Alonso C.M. Are my patients with rheumatic diseases at higher risk of COVID-19? Ann Rheum Dis. 2020 doi: 10.1136/annrheudis-2020-217322. [DOI] [PubMed] [Google Scholar]
- 84.Pope J.E. What does the COVID-19 pandemic mean for rheumatology patients? Curr Treat Options in Rheum. 2020 doi: 10.1007/s40674-020-00145-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Lu C., Li S., Liu Y. Role of immunosuppressive therapy in rheumatic diseases concurrent with covid-19. Ann Rheum Dis. 2020 doi: 10.1136/annrheumdis-2020-21460. [DOI] [PubMed] [Google Scholar]
- 86.Mathian A., Mahevas M., Rohmer J. Clinical course of coronavirus disease 2019 (COVID-19) in a series of 17 patients with systemic lupus erythematosus under long-term treatment with hydroxychloroquine. Ann Rheum Dis. 2020 doi: 10.1136/annrheumdis-2020-217566. [DOI] [PubMed] [Google Scholar]
- 87.Gianfrancesco M.A., Hyrich K.L., Gossec L. Rheumatic disease and COVID-19: initial data from the COVID-19 global rheumatology alliance provider registries. Lancet Rheumatol. 2020 doi: 10.1016/s2665-9913(20)30095-. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Cassione E.B., Zanframundo G., Biglia A. Covid-19 infection in a northern-Italian cohort of systemic lupus erythematosus assessed by telemedicine. Ann Rheum Dis. 2020 doi: 10.1136/annrheumdis-2020-217717. [DOI] [PubMed] [Google Scholar]
- 89.Wu Z., McGoogan J.M. Characteristics of and important lessons from the coronavirus disease 2019 (COVID-19) outbreak in China: summary of a report of 72314 cases from the Chinese center for disease control and prevention. JAMA. 2020;323:1239–1242. doi: 10.1001/jama.2020.2648. [DOI] [PubMed] [Google Scholar]
- 90.W-jie Guan, Ni Z-yi Hu Y. Clinical characteristics of coronavirus disease 2019 in China. New Eng J Med. 2020;382:1708–1720. doi: 10.1056/NEJMoa2002032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Haberman R., Axelrad J., Chen A. Covid-19 in immune-mediated inflammatory diseases- case series from New York. New Eng J Med. 2020 doi: 10.1056/NEJMc2009567. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Cheng C., Li C., Zhao T. COVID-19 with rheumatic diseases: a report of 5 cases. Clin Rheumatol. 2020 doi: 10.1007/s10067-020-05160-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Monti S., Balduzzi S., Delvino P. Clinical course of Covid-19 in a series of patients with chronic arthritis treated with immunosuppressive targeted therapies. Ann Rheum Dis. 2020 doi: 10.1136/annrheumdis-2020-217424. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Favalli E.G., Agape E., Caporali R. Incidence and clinical course of COVID-19 in patients with connective tissue diseases: a descriptive observational analysis. J Rheumatol. 2020 doi: 10.3899/jrheum.200507. [DOI] [PubMed] [Google Scholar]
- 95.Conticini E., Bargagli E., Bardelli M. COVID-19 pneumonia in a large cohort of patients with biological and targeted synthetic antirheumatic drugs. Ann Rheum Dis. 2020 doi: 10.1136/annrheumdis-2020-217681. [DOI] [PubMed] [Google Scholar]
- 96.Guilpain P., Le Bihan C., Foulonge V. Rituximab for granulomatosis with polyangiitis in the pandemic of covid-19: lessons from a case with severe pneumonia. Ann Rheum Dis. 2020 doi: 10.1136/annrheumdis-2020-217549. [DOI] [PubMed] [Google Scholar]
- 97.Tomelleri A., Sartorelli S., Campochiaro C. Impact of COVID-19 pandemic on patients with large-vessel vasculitis in Italy: a moncentric survey. Ann Rheum Dis. 2020 doi: 10.1136/annrheumdis-2020-217600. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Ai T., Yang Z., Hou H. Correlation of chest CT and RT-PCR testing in coronavirus disease 2019 (COVID-19) in China: a report of 1014 cases. Radiology. 2020;200642 doi: 10.1148/radiol.2020200642. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Del Papa N., Sambataro G., Minniti A. Novel COrona Virus Disease 2019 (COVID-19) epidemic: What are the risks for systemic sclerosis patients. Autoimmun Rev. 2020 doi: 10.1016/j.autrev.2020.102558. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Matucci-Cerini M., Bruni C., Allanore Y. Systemic sclerosis and the COVID-19 pandemic: world Scleroderma Foundation preliminary advice for patient management. Ann Rheum Dis. 2020 doi: 10.1136/annrheumdis-2020-217407. [DOI] [PubMed] [Google Scholar]
- 101.Mihai C., Dobrota R., Schroder M. COVID-19 in a patient with systemic sclerosis treated with tocilizumab for SSc-ILD. Ann Rheum Dis. 2020 doi: 10.1136/annrheumdis-2020-217442. [DOI] [PubMed] [Google Scholar]
- 102.COVID-19 Treatment Guidelines Panel. Coronavirus Disease . National Institutes of Health; 2019. (COVID-19) Treatment Guidelines.https://covid19treatmentguidelines.nih.gov/ Available from: [PubMed] [Google Scholar]
- 103.Mikuls T.R., Johnson S.R., Fraenkel L. American College of Rheumatology guidance for the management of adult patients with rheumatic disease during the COVID-19 pandemic. Arthritis Rheum. 2020 doi: 10.1002/ART.41301. [DOI] [PubMed] [Google Scholar]
- 104.Wang M., Cao R., Zhang L. Remdesivir and chloroquine effectively inhibit the recently emerged novel coronavirus (2019-nCoV) in vitro. Cell Res. 2020;30(3):269–271. doi: 10.1038/s41422-020-0282-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Vincent M.J., Bergeron E., Benjannet S. Chloroquine is a potent inhibitor of SARS coronavirus infection and spread. Virol J. 2005;2:69. doi: 10.1186/1743-422X-2-69. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Liu J., Cao R., Xu M. Hydroxychloroquine, a less toxic derivative of chloroquine, is effective in inhibiting SARS-CoV-2 infection in vitro. Cell Discov. 2020;6:16. doi: 10.1038/s41421-020-0156-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.Gendelman O., Amital H., Bragazzi N.L. Continuous hydroxychloroquine or colchicines therapy does not prevent infection with SARS-CoV-2: Insights from a large healthcare database analysis. Autoimmun Rev. 2020 doi: 10.1016/j.autrev.2020.102566. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.Geleris J., Sun Y., Platt J. Observational study of hydroxychloroquine in hospitalized patients with Covid-19. N Engl J Med. 2020 doi: 10.1056/NEJMoa2012410. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Rubin E.J., Harrington D.P., Hogan J.W. The urgency of care during the Covid-19 pandemic-learning as we go. New Eng J Med. 2020 doi: 10.1056/NEJMe2015903. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110.Rosenberg E.S., Dufort E.M., Udo T. Association of treatment with hydroxychloroquione or azithromycin with in-hospital mortality in patients with Covid-19 in New York state. JAMA. 2020 doi: 10.1001/jama.2020.8630. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.FDA Drug Safety Communication . 04-24-2020. Safety Announcement. [Google Scholar]
- 112.Qaseem A., Yost J., Etxeandia-Ikobaltzeta I. Should clinicians use chloroquine or hydroxychloroquine alone or in combination with azithromycin for the prophylaxis or treatment of COVID-19? Living practice points from the American College of Physicians (Version 1) Ann Intern Med. 2020 doi: 10.7326/M20-1998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113.Balevic S.J., Hornik C.P., Green T.P. Hydroxychloroquine in patients with rheumatic disease complicated by COVID-19: clarifying target exposures and the need for clinical trials. J Rheumatol. 2020 doi: 10.3899/jrheum.200493. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114.Zhou F., Yu T., Du R. Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: a retrospective cohort study. Lancet. 2020;395(10229):1054–1062. doi: 10.1016/S0140-6736(20)30566-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115.Huang C., Wang Y., Li X. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet. 2020;395(10223):497–506. doi: 10.1016/S0140-6736(20)30183-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116.Wang Z., Yang B., Li Q., Wen L., Zhang R. Clinical features of 69 cases with coronavirus disease 2019 in Wuhan, China. Clin Infect Dis. 2020 doi: 10.1093/cid/ciaa272. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 117.Xu X., Han M., Li T. Effective treatment of severe COVID-19 patients with tocilizumab. PNAS. 2020 doi: 10.1073/pnas.2005615117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 118.Aouba A., Baldolli A., Geffray L. Targeting the inflammatory cascade with anakinra in moderate to severe Covid-19 pneumonia: case series. Ann Rheum Dis. 2020 doi: 10.1136/annrheumdis-2020-217706. [DOI] [PubMed] [Google Scholar]
- 119.Cavalli G., De Luca G., Campochiaro C. Interleukin-1 blockade with high-dose anakinra in patients with Covid-19, acute respiratory distress syndrome, and hyperinflammation: a retrospective cohort study. Lancet. 2020 doi: 10.1016/s2665-9913(20)30127-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 120.Oldstone M.B. Molecular mimicry: its evolution from concept to mechanism as a cause of autoimmune diseases. Monoclon Antib Immunodiagn Immunother. 2014;33(3):158–165. doi: 10.1089/mab.2013.0090. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 121.Kanduc D., Shoenfeld Y. On the molecular determinants of the SARS-CoV-2 attack. Clin Immunol. 2020;215:108426. doi: 10.1016/j.clim.2020.108426. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 122.Onouchi Y., Gunji T., Burns J.C. ITPKC functional polymorphism associated with Kawasaki disease susceptibility and formation of coronary artery aneurysms. Nat Genet. 2008;40(1):35–42. doi: 10.1038/ng.2007.59. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 123.Vallianatos C.N., Iwase S. Disrupted intricacy of histone H3K4 methylation in neurodevelopmental disorders. Epigenomics. 2015;7:503–519. doi: 10.2217/epi.15.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 124.Ponchel F., Cuthbert R.J., Goëb V. IL-7 and lymphopenia. Clin Chim Acta. 2011;412(1–2):7–16. doi: 10.1016/j.cca.2010.09.002. [Epub 2010 Sep 17] [DOI] [PubMed] [Google Scholar]
- 125.Kanduc D. Peptide cross-reactivity: the original sin of vaccines. Front Biosci. 2012;4:1393–1401. doi: 10.2741/s341. [DOI] [PubMed] [Google Scholar]
- 126.Kanduc D. “Self-nonself” peptides in the design of vaccines. Curr Pharm Des. 2009;15:3283–3289. doi: 10.2174/138161209789105135. [DOI] [PubMed] [Google Scholar]
- 127.Kanduc D., Shoenfeld Y. From HBV to HPV: designing vaccines for extensive and intensive vaccination campaigns worldwide. Autoimmun Rev. 2016;15:1054–1061. doi: 10.1016/j.autrev.2016.07.030. [DOI] [PubMed] [Google Scholar]
- 128.Zinserling V.A., Vashukova M.A., Vasilyeva M.V., Isakov A.N. Issues of pathology of a new coronavirus infection COVID-19. Jurnal infectologii. 2020;12(2):5–11. doi: 10.22625/2072-6732-2020-12-2-5-11. Rus. [DOI] [Google Scholar]
Addendum: Following this submission the enclosed references were published (129–143).
- 129.Colafrancesco S., Alessandri C., Conti F. COVID-19 gone bad: A new character in the spectrum of hyperferritinemic syndrome? Autoimun Rev. 2020 doi: 10.1016/j.autrev.2020.102573. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 130.Alijotas-Reig J., Esteve-Valverde E., Belizna C. Immunomodulatory therapy for the management of severe COVID-19. Beyond the anti-viral therapy: A comprehensive review. Autoimmun Rev. 2020 doi: 10.1016/j.autrev.2020.102569. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 131.Segal G., Mevorach D., Elis A. Clinical Insights and Management Recommendations for COVID-19 Patients Hospitalized in Internal Medicine Departments: Recommendations by the Corona Department Heads in Israel. Isr Med Assoc J. 2020;22:275–277. [PubMed] [Google Scholar]
- 132.Itelman E., Wasserstrum Y., Segev A. Clinical Characterization of 162 COVID-19 patients in Israel: Preliminary Report from a Large Tertiary Center. Isr Med Assoc J. 2020;22:271–274. [PubMed] [Google Scholar]
- 133.Jamilloux Y., Henry T., Belot A. Should we stimulate or suppress immune responses in COVID-19? Cytokine and anti-cytokine interventions. Autoimmune Rev. 2020 doi: 10.1016/j.autrev.2020.102567. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 134.Favalli E.G., Monti S., Ingegnoli F. Incidence of COVID-19 in patients with rheumatic diseases treated with targeted immunosuppressive drugs: what can we learn from observational data? Arthritis Rheum. 2020 doi: 10.1002/ART.41388. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 135.Favalli E.G., Ingegnoli F., De Lucia O. 2020. COVID-19 infection and rheumatoid arthritis: Faraway, so close! Autoimmune Rev. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 136.Karpel A., Nissan N., Klug M. Imaging findings in four COVID-19 patients. Isr J Med Sci. 2020;22:214–215. [PubMed] [Google Scholar]
- 137.Toniati P., Piva S., Cattalini M. Tocilizumab for the treatment of severe COVID-19 pneumonia with hyperinflammatory syndrome and acute respiratory failure: A single center study of 100 patients in Brescia. Italy. Autoimmune Rev. 2020 doi: 10.1016/j.autrev.2020.102568. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 138.McGonagle D., Sharif K., O’Regan A. The Role of Cytokines including Interleukin-6 in COVID-19 induced Pneumonia and Macrophage Activation Syndrome-Like Disease. Autoimmune Rev. 2020 doi: 10.1016/j.autrev.2020.102537. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 139.Cunningham L., Kimber L.I., Basketter D.A. Why judiciously timed anti-IL 6 therapy may be of benefit in severe COVID-19 infection. Autoimmune Rev. 2020 doi: 10.1016/j.autrev.2020.102563. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 140.Ruscitti P., Berardicurti O., Iagnocco A. Cytokine storm syndrome in severe COVID-19. Autoimmune Rev. 2020 doi: 10.1016/j.autrev.2020.102562. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 141.Angileri F., Legare S., Gammazza A.M. Molecular mimicry may explain multi-organ damage in COVID-19. Autoimmune Rev. 2020 doi: 10.1016/j.autrev.2020.102591. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 142.Marotto D., Sarzi-Puttini P. What is the role of rheumatologists in the era of COVID-19? Autoimmune Rev. 2020 doi: 10.1016/j.autrev.2020.102539. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 143.Emmi G., Bettiol A., Mattioli I. SARS-CoV-2 infection among patients with systemic autoimmune diseases. Autoimmune Rev. 2020 doi: 10.1016/j.autrev.2020.102575. [DOI] [PMC free article] [PubMed] [Google Scholar]