Abstract
Diffuse alveolar hemorrhage (DAH) is a rare life-threatening condition in children. In this entity, the bleeding originates from the pulmonary microvasculature as a result of microvascular damage leading to blood leakage into the alveolar spaces. DAH can occur as an isolated medical entity or may be associated with other organ system injury or dysfunction. The classic triad of symptoms includes hemoptysis, anemia and diffuse pulmonary infiltrates. Hemoptysis is the usual presenting symptom but is not constant. A variety of diseases is associated with the development of DAH. Current classification organize the etiologies of diffuse alveolar hemorrhage based on the presence of severe immune disorders (such as systemic vasculitis and collagenosis) or non-immunodeficiency disorders (with an identified cardiac or non-cardiac origin, or idiopathic).
The five cases of DAH presented in this study were all diagnosed in full-term infants, four males and one female, with normal neonatal adaptation and without family history of notable diseases. In all cases the diagnosis was made between the age of three and eighteen weeks-old. Moreover, all five patients, at the time of diagnosis, presented with hemoptysis, mild or severe dyspnea, anemia and abnormal chest X-rays. Consequently, the diagnosis of DAH was strongly suspected and, eventually, confirmed by bronchoscopy. Additional laboratory tests, as well as selected serologic and radiographic studies were performed in order to identify a specific etiology. The final diagnoses reflect a variety of causes: infections, idiopathic pulmonary hemosiderosis, accidental suffocation and Heiner syndrome. Treatment included oral corticosteroids except from one patient that received antimicrobial therapy.
Keywords: Diffuse alveolar hemorrhage, Bronchoscopy, BAL, Golde score, Hemoptysis, Anemia
1. Background
DAH is a rare but potentially life-threatening condition in infants. In this entity, the bleeding originates from the pulmonary microvasculature (pulmonary arterioles, alveolar capillaries, and pulmonary venules) as a result of microvascular damage leading to blood leakage into the alveolar spaces [19,23].
Due to the lack of reported cases and cohorts described in the literature, the epidemiology and the incidence of the different causes of DAH in pediatric population remain imprecise.
A variety of diseases is associated with the development of the DAH. Current classification schemes organize the etiologies of DAH according to the association with severe immune disorders (such as systemic vasculitis and collagenosis [19]), the association with non-immune disorders, which may be of cardiac or non-cardiac origin, or idiopathic disorders [1,2]. In children, the most frequent non-immune causes of DAH are infections [22] and cardiovascular diseases.
Interestingly, a plethora of cases of DAH in children have been identified as idiopathic pulmonary hemosiderosis (IPH). IPH is a diagnosis of exclusion, and its pathogenesis remains controversial [10,23]. Various hypotheses have been proposed to explain the pathophysiology of IPH; allergic, environmental, genetic and autoimmune [9,10]. The allergic theory is based on the frequent association between IPH and cow's milk hypersensitivity (Heiner syndrome).
Published data associating pulmonary hemosiderosis with the exposure to a toxigenic fungus provides some evidence that environmental factors may play a role in DAH [11]. IPH has also been described in a small number of familial cases, leading to the discussion of a genetic theory; however, no gene has been identified yet [12]. Finally, considering the frequent association with autoimmune diseases, the autoimmune theory is recognized as the most probable. It is important to mention that alveolar hemorrhage may be the first manifestation occurring well before (months to a year) the development of an immunological disorders [14,19,24]. Table 1 demonstrates the current classification scheme for the causes of DAH.
Table 1.
Classification of diffuse alveolar hemorrhage in young infants.
| Classification | Disorders |
|---|---|
| Immune Disorders (Not Common) | Idiopathic pulmonary capillaritis Wegener's granulomatosis Microscopic polyangiitis Behcet's syndrome Goodpasture's syndrome Henoch-Schönlein purpura Churg-Strauss syndrome Cryoglobulinemia Systemic lupus erythematosus Polyarteritis nodosa Sclerodermitis IgA nephropathy Antiphospholipid antibody syndrome Polymyositis |
| Non-immune Disorders (More Common) Non-cardiovascular Origins: |
Idiopathic pulmonary hemosiderosis Heiner syndrome Celiac disease (Lane-Hamilton syndrome) Infections Coagulation disorders Infanticide Drugs and toxines |
| Cardiovascular Causes: | Mitral stenosis Pulmonary veno-occlusive disease Arteriovenous malformations Pulmonary hypertension Pulmonary capillary hemangiomatosis Chronic right heart failure |
2. Clinical manifestations, laboratory findings and imaging
The clinical presentation of DAH can vary from acute respiratory distress syndrome to a more insidious presentation with minimal symptoms such as cough. The classic triad of symptoms includes hemoptysis, anemia and diffuse pulmonary infiltrates [21]. Hemoptysis is the usual presenting symptom, but is not constant, as young children may not expectorate [2,10].
3. Diagnostic approach
The most useful investigation to confirm the diagnosis of DAH consists of bronchial fibroscopy and BAL [1,21]. Bronchoscopy is the most direct way to evaluate hemoptysis and determine the site of bleeding (if there is an active bleeding) or another obvious cause, such as inhalation of a foreign body. A macroscopically hemorrhagic BAL fluid, especially with increase blood content on successive aliquots, is considered as a diagnostic of acute alveolar hemorrhage (AH). However, the demonstration of hemosiderin-laden macrophages (HLMs) is a good evidence of sub-acute AH. After a bleeding episode into the lungs, hemoglobin is converted to hemosiderin by alveolar macrophages. In a mice model, Epstein et al. [14] showed that HLMs and hemosiderin appear within 48–72h after the initial bleeding, reach a maximal concentration at day 6 and then remains within the lungs for 4–8 weeks [4]. The Golde score is a semi-quantitative assessment of HLMs, after a Prussian blue stain, which evaluates both the percentage of macrophages containing hemosiderin (evaluating 100 macrophages), and the intensity of staining on a scale between 0 and 4. The score can therefore vary from 0 to 400. An AH is confirmed for a score above 100 [3].
Further investigations of DAH include a search for infectious agents and for both precipitating antibodies to cow's milk proteins and milk-specific immunoglobulin E (IgE). Complete work-up should also include evaluation for coagulation disorders, screening for a cardiac etiology as well as for possible pulmonary-renal syndromes [17,18], including urine analysis and renal function, as well as specific serologic testing for antinuclear antibodies (ANA) and their components, anti-glomerular basement membrane (GBM) antibodies, and antineutrophil cytoplasmic antibodies (ANCA) to detect immune-mediated lung disease [18,23]. As the diagnosis of DAH can be performed by less invasive procedures, lung biopsy is not justified [21].
4. Presentation of the cases
4.1. Case 1
A seven-week-old male was admitted to the Pediatric Emergency Department after an episode of hemoptysis and epistaxis. He was born full term, eutrophic, with normal neonatal adaptation. He was fed with cow milk (CM) formula from birth on. No other symptoms preceding the hemorrhage were reported by the parents. At the admission, the patient presented a bloody nasal discharge. Clothes were stained with blood. He was pale and hypotonic. He presented a moderate tachypnea varying from 40 to 50 bpm but without associated hypoxemia (SpO2 95% on room air). There was no fever, no central cyanosis, the capillary refill time was normal, and there were no actively hemorrhagic skin or mucous lesions. The infant was dyspneic with chest retractions and presented a grunting. The pulmonary auscultation was normal, there were neither crackles nor wheezes. The cardiovascular exam and the systemic examination were unremarkable. Family and patient history was not contributive. Exposure to tobacco smoke or abnormal humidity at home were denied.
Initial routine laboratory results revealed a hemoglobin level of 10.5 g/dL, a hematocrit value of 22%, a white blood cell count (WBC) of 13.9 x 10*9/L, a platelet count of 360 x 10*9/L, with normal coagulation profile (prothrombin time: 16.6 seconds, activated partial thromboplastin time: 39 seconds, fibrinogen: 2.2 g/L and D-dimers: 760ng/mL). C-reactive protein level, renal function, electrolytes, and aminotransferases were normal. Central venous blood gases showed a moderate respiratory acidosis (pH of 7.17, partial pressure of carbon dioxide of 68 mm Hg). Toxicology screen was negative, and urinalysis was normal.
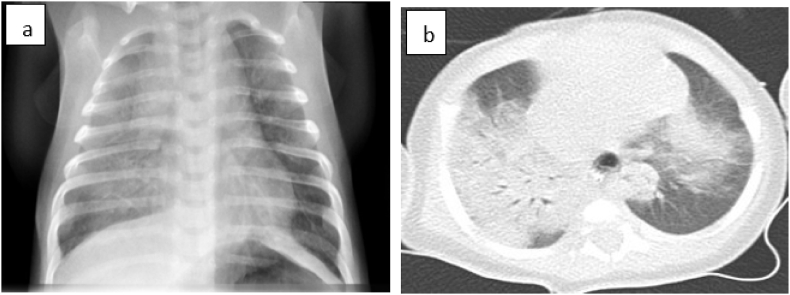
The chest radiograph showed diffuse alveolar infiltrates mostly in the right lung (Fig. 1a). Chest computed tomography (CT) showed consolidated opacities mainly in the right lung (Fig. 1b).
Fig. 1.
(a) Chest radiography showed diffuse alveolar infiltrates mostly in the right pulmonary hemi-field. (b) Chest computed tomography scan showed, within the right upper lobe, complete consolidation in the posterior segment and nearly complete consolidation in the anterior segment.
Within the first hour of hospitalization, the oxygen saturation decreased (SpO2 75%), and the anemia worsened(hemoglobin of 8,5 g/dL); therefore, a supportive therapy including volume expansion, ventilatory support, and transfusion of packed red blood cells at a dose of 20ml/kg was necessary. The infant was intubated and transported to our Pediatric Intensive Care Unit (PICU) under initial antibiotic coverage.
The infant underwent emergency bronchial fibroscopy, and diffuse active bleeding [diffuse alveolar hemorrhage (DAH)] was spotted. There were large amounts of blood and clots present in the whole airway. Unfortunately, it was not possible to perform a bronchoalveolar lavage (BAL) because of the hemodynamic instability of the patient. Full etiologic assessment was done and was not contributive (see Table 1). The diagnosis of idiopathic hemosiderosis was proposed.
The immunosuppressive therapy was prescribed using 2 mg/kg of prednisolone daily. The infant was extubated on day 2, and discharged 7 days after admission. The infant returned home on steroid therapy (2mg/kg/day during one month and followed by a gradual dose reduction), with hypoallergenic amino acid-based milk and under home cardio-respiratory monitoring. The patient is regularly followed in the respiratory outpatient clinic, and he is doing very well. At 3 months of age, the chest radiograph and the CT were normalized.
4.2. Case 2
A 3-month-old male infant, born at full term, eutrophic, with normal neonatal adaptation, presented at the emergency department for cough followed by several episodes of hemoptysis.
History included hospitalization at the age of two and a half months for tachypnea, cough and upper airways congestion accompanied by oral bloody secretions. The initial diagnosis was gastroesophageal reflux and the patient was discharged from hospital with a proton pump inhibitor and a strict cow's milk elimination.
On admission, the infant was well perfused, and not hypoxic (SpO2 98% on room air). Physical examination showed nasal congestion and bilateral lung crackles on pulmonary auscultation. No dyspnea was noted. Central venous blood gases showed a pH of 7.3 and partial pressure of carbon dioxide of 54 mm Hg. Laboratory studies showed anemia (hemoglobin level: 8.1 g/dL, hematocrit value: 24%). WBCs and platelet count, coagulation profile, quantitative immunoglobulins, and complement studies were normal. Urine analysis was normal.
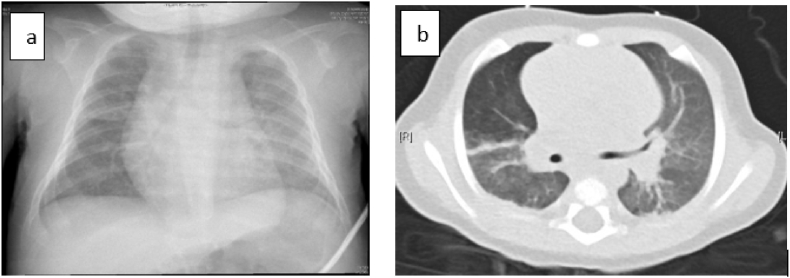
Chest x-ray revealed bilateral alveolo-interstitial opacities and left lower lobe parenchymal consolidation (Fig. 2a). Chest CT showed diffuse bilateral alveolar and ground-glass opacities (Fig. 2b).
Fig. 2.
(a) Chest radiograph demonstrated bilateral alveolo-interstitial opacities. (b) Chest computed tomography scan showed diffuse bilateral alveolar and ground-glass opacities.
The infant received packed red cells but no ventilatory support was necessary. A bronchial fibroscopy was performed early after admission that active diffuse bleeding was objectified. Due to the precocity of BAL, hemosiderin-laden macrophages were not demonstrated in the cytological analysis. Etiologic assessment was done and was not contributive except the presence of Chlamydia Trachomatis on BAL culture (see Table 1). The diagnosis of an interstitial pneumonitis with subsequent diffuse alveolar hemorrhage was made. Antimicrobial therapy using oral clarithromycin 15mg/kg/day for 21 days was given, while the systemic corticotherapy initiated at admission was stopped. The patient's symptoms completely resolved shortly after the start of treatment and he was discharged from the hospital on the 8th day on hypoallergenic amino acid-based milk and with a cardio-respiratory monitor.
4.3. Case 3
A two-month-old female infant, born at 37 weeks of gestation from consanguineous parents, eutrophic, needed prolonged hospitalization in the Neonatal Intensive Care Unit (NICU) for polymalformative syndrome including a common atrium, rectovulvar fistula, alopecia, and dysmorphic features. Initial adaptation at birth was marginal but she quickly stabilize after birth, and a non-invasive ventilatory support was needed for mild apneic syndrome. She was found unconscious, apneic, bradycardic with a heart rate of 60–70 beats per minute and cyanotic (SpO2 40% on room air), with foamy bloody secretions in her mouth and nose. No history of trauma, fever or bleeding from any other site was noted.
The acute situation required emergency tracheal intubation and fresh blood was aspirated from the endotracheal tube. Heart rate and oxygen saturation quickly improved with conventional mechanical ventilation. High ventilatory pressures were needed to achieve adequate tidal volumes. Physical examination showed normal skin, bilateral lung crackles and a systolic murmur already known. Chest radiograph showed cardiomegaly with diffuse alveolar infiltrates mostly in the right lung. Complete blood count showed normal WBCs count (8500/mm3 with 22% neutrophils, 69% lymphocytes), a hemoglobin level of 10 g/dl, a hematocrit value of 30.4%, a platelet count of 247,000/mm3, and a normal coagulation profile. Central venous blood gases showed mild respiratory acidosis and elevated lactate level (50mg/dL). Screening for common causes of DAH (see Table 1) was performed but was not contributive.
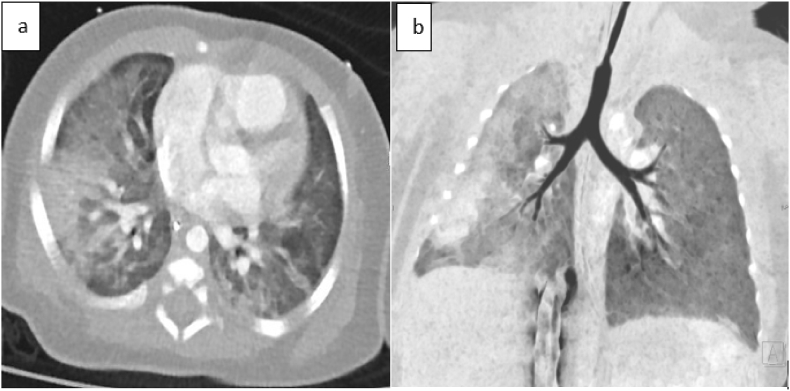
Two days later, packed red blood cells were transfused for anemia and intravenous antibiotics were administered for suspected infection (fever and raised inflammatory markers). Blood culture and nasopharyngeal aspiration were obtained for viral and bacterial screening. Thoracic angiography scan showed consolidated opacities mainly within the right lung, and arteriovenous malformation were excluded (Fig. 3a, b). The echocardiography confirmed large inter-atrial left-to-right shunt. A bronchial fibroscopy was performed 6 days after admission, excluding active bleeding. BAL was not performed because of the patient's respiratory instability.
Fig. 3.
(a,b) Thoracic angiography scan showed consolidated opacities mainly within the right lung.
The first extubation attempt was done on day 3, but reintubation was necessary due to the recurrent bleeding episode and respiratory distress.
The patient initially continued to present fresh blood and clots aspirated from her endotracheal tube and then slowly improved from day 4 after the first bleeding episode. Her ventilatory support was weaned and she was successfully extubated on day 6. Her chest radiograph showed significant clearance of the initial haziness. Respiratory virus PCR panel from nasopharyngeal aspiration and tracheal secretions was positive for coronavirus NL63. Bacterial cultures from respiratory secretions and blood were negative. Antimicrobial therapy was stopped after 48 hours and the infant received oral corticosteroid treatment.
4.4. Case 4
A three-week-old male, born at full term, eutrophic with normal neonatal adaptation, was admitted to the emergency department for a severe episode of loss of consciousness accompanied by hypotonia and cyanosis. The infant, was found unconscious in bed 1 hour after feeding on his stomach, surrounded by soft toys and pillows. His mother noticed some foamy red secretions on his lips.
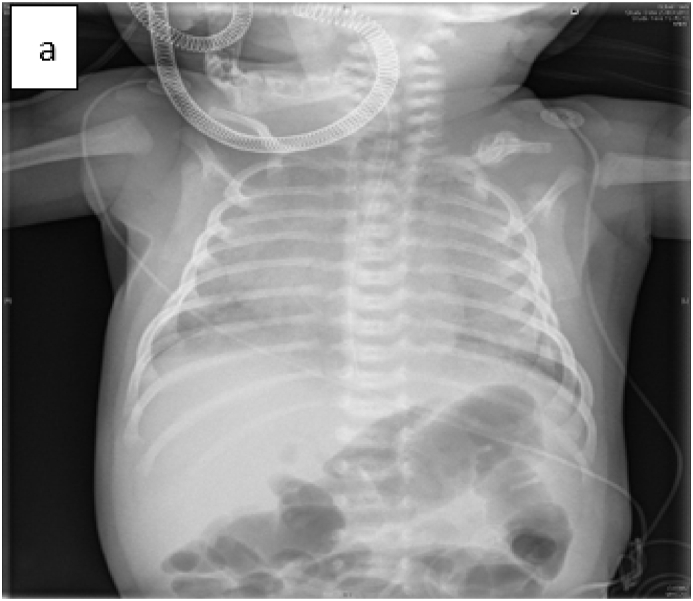
At admission, he was pale, capillary refill time was prolonged (4 seconds), central temperature was 35.5 °C. He showed nasal flaring and retractions, a respiratory rate of 40–50 bpm, and SpO2 at room air of 85%. The pulmonary auscultation revealed bilateral crackles. A venous blood gas showed a severe metabolic acidosis (pH: 7.08, partial pressure of carbon dioxide: 38 mmHg, bicarbonate: 10 mmol/L and base excess: 18 mmol/L). Hemoglobin level was normal (16 g/d). Further routine laboratory results including markers of inflammation and infection, of hemostasis, of renal and hepatic function were normal. Urinalysis was also normal. Chest x-ray revealed diffuse and bilateral opacities (Fig. 4a). The cardiac evaluation, including echocardiogram, revealed a physiologic patent foramen ovale.
Fig. 4.
(a) Chest x-ray showed diffuse alveolar infiltrates.
The infant was admitted to the Intensive Care Unit under initial triple intravenous antibiotic coverage, non-invasive ventilatory support and supplemental oxygen. The first 48 hours of hospitalization, he presented a sudden drop of 4 g/dL of the hemoglobin levels. A bronchial fibroscopy and a BAL were performed on day 4. No active bleeding was noted. Hemosiderin-laden macrophages (siderophages) at 68%, and a positive Golde score at 129% were demonstrated in the BAL confirming the DAH. Etiologic assessment for DAH was done and was not contributive (see Table 1). During hospitalization, he received prednisone 2mg/kg/day and he was discharged after one week with the diagnosis of AH probably due to accidental suffocation, as he was found lying with his face against the mattress. The patient was on steroid treatment with gradual dose reduction, with hypoallergenic amino acid-based milk and under cardio-respiratory monitoring.
4.5. Case 5
A 3-month-old male infant, born at full term, eutrophic, with a history of transient tachypnea of the newborn after birth, was admitted at the emergency department for brutal cough and hemoptysis while sleeping. He was described hypotonic during this episode. No symptoms were reported by parents preceding the hemorrhage. He was fed with cow milk (CM) formula from birth on.
On admission, the infant was eupneic and normoxic (SpO2 98% on room air). Physical examination and in particular the pulmonary auscultation was normal. One hour later, he developed dyspnea with moderate chest retractions. Central venous blood gases showed a respiratory acidosis (pH of 7.08 and partial pressure of carbon dioxide of 71 mm Hg). Initial laboratory study showed anemia (hemoglobin level: 9.4 g/dL, hematocrit value: 29.3%), thrombocytosis (platelet count: 595.000/mm³), hyperleukocytosis (WBC count: 18.530/mm3, 54% lymphocytes, 39% neutrophils) but normal C-reactive protein levels. Further routine laboratory results including septic, hemostatic, renal, and hepatic profile returned normal. Urinalysis was also normal.
Chest x-ray revealed diffuse interstitial opacities in the right lung (Fig. 5a), Thoracic angiography scan confirmed diffuse interstitial opacities in the right lung and excluded vascular malformation .
Fig. 5.
(a) Chest radiography showed diffuse alveolar infiltrates at the right pulmonary hemifield.
A bronchial fibroscopy was performed on day 4 after the episode of bleeding and did not demonstrate any active bleeding. Hemosiderin-laden macrophages (siderophages) at 89%, and a positive Golde score at 212% were demonstrated in the BAL, confirming DAH. The infant received prednisone 2mg/kg/day. A complete etiologic assessment for DAH (see Table 1) was done and was not contributive except for the positivity of precipitins against cow's milk proteins (see Table 3). The diagnosis of Heiner syndrome was made. Hypoallergenic amino acid-based milk diet was proposed.
Table 3.
Demographic data, clinical presentation, etiology assessment and diagnosis.
| Case 1 | Case 2 | Case 3 | Case 4 | Case 5 | |
|---|---|---|---|---|---|
| Sex | M | M | F | M | M |
| Age at onset | 7-w | 12-w | 8-w | 3-w | 18-w |
| Hemoptysis | Acute hemoptysis | 2-w history of intermittent hemoptysis | Acute hemoptysis | Acute hemoptysis | Acute hemoptysis |
| Anemia | + | + | + | + | + |
| Venous blood gases | RA | RA | RA | MA | RA |
| Chest X-Ray | AI | AI | AI | AI | AI |
| CT scan | CO | ILD | CO | ND | CO |
| BAL | + | + | ND | + | + |
| HLMs | – | – | ND | + | + |
| Golde score | ND | ND | ND | + | + |
| Microbiologic culture in BAL | N | Chlamydia trachomatis | N | N | N |
| Respiratory virus PCR panel | N | N | COV | N | N |
| Immunologic abnormalities | N | N | N | N | N |
| Milk RAST | N | N | N | N | N |
| Milk precipitin test | ND | ND | ND | ND | + |
| Blood transfusion | + | + | + | – | – |
| Ventilatory support | + | – | + | + | – |
| Corticosteroid therapy | + | – | + | + | + |
| Antimicrobial therapy | – | + | – | – | – |
| Diagnosis | Idiopathic pulmonary hemosiderosis | DAH due to Chlamydia trachomatis infection | DAH due to coronavirus infection | DAH due to accidental suffocation | Heiner syndrome |
BAL = bronchoscopic alveolar lavage, HLMs = hemosiderin laden macrophages, RA = respiratory acidosis, MA = metabolic acidosis, AI = alveolo-interstitial pattern, ILD = interstitial lung disease, CO = consolidative opacities, ND = not done, N = normal, COV= Coronavirus NL63, DAH = Diffuse alveolar hemorrhage.
The patient's evolution during the hospitalization was favorable and no subsequent hemoptysis was noted. The patient was discharged from hospital with amino acid-based milk and systemic corticosteroid. During regular outpatient visits, the patient presented a favorable respiratory evolution without any recurrent hemoptysis. The corticosteroid treatment was stopped after three months.
5. Discussion
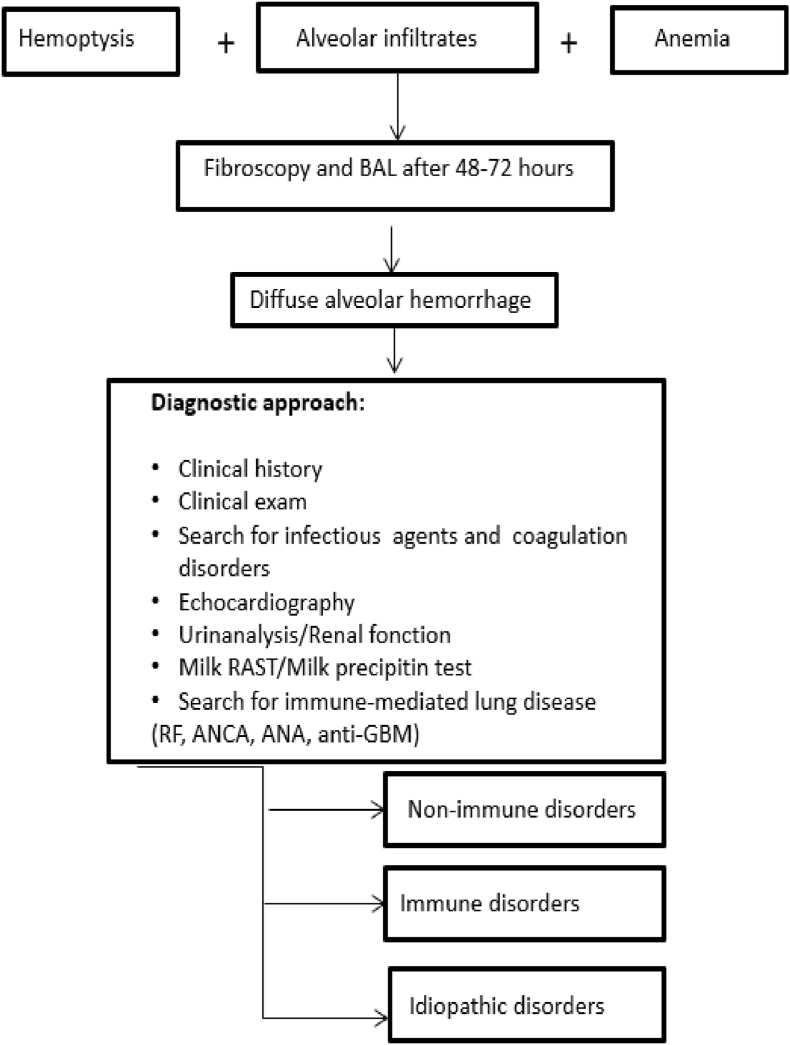
Five cases of DAH are described in this report. Our five patients presented episodes of hemoptysis, anemia of varying degrees, and their chest radiographs showed diffuse bilateral interstitial infiltrates consistent with pulmonary hemorrhage. Consequently a diagnosis of DAH was strongly suspected (Fig. 6). In three of the five cases, the severity of the initial pulmonary hemorrhage was sufficient to cause acute pulmonary distress, requiring adequate ventilatory support and to cause severe anemia requiring packed red blood cell transfusion. In all our cases, due to young age, systemic vasculitis and collagen vascular disorders were unlikely.
Fig. 6.
Algorithm for management of intra-alveolar haemorrhage
BAL: bronchoscopic alveolar lavage; RF: rheumatic factor; ANCA: Antineutrophil Cytoplasmic Antibodies; ANA: Antinuclear Antibodies; GBM: Glomerular Basement Membrane.
In all cases, pediatric pulmonologists performed a bronchial fibroscopy in order to look for active bleeding in the airways. In the absence of obvious cause of the bleeding, BAL was performed. Hemosiderin-laden macrophages were found in BAL only in 2 of our 5 patients, either due to early performance of the BAL within 24 hours from hemoptysis or due to limitations of the bronchoscopy procedure because of hemodynamic instability of the patients. As previously mentioned, HLMs were not demonstrated in the cytological analysis until 48–72 hours after the acute phase. However, the visualization of areas of active bleeding, and the aspiration of fresh blood confirmed the pulmonary hemorrhage in these cases.
Table 2 presents bronchoalveolar lavage results for these five cases.
Table 2.
Bronchoalveolar lavage results.
| Red blood cells, mm3 | White blood cells, mm3 | Neutrophils, % | Lymphocytes, % | Macrophages, % | Hemosiderin-laden macrophages, %, | Golde score | |
|---|---|---|---|---|---|---|---|
| Case 1 | 510 | 450 | ND | ND | ND | ND | ND |
| Case 2 | 1910 | 400 | 73 | 4 | 23 | ND | ND |
| Case 3 | 1540 | 110 | ND | ND | ND | ND | ND |
| Case 4 | 280 | 450 | 1.3 | 1.9 | 96 | 69 | 129 |
| Case 5 | 80 | 460 | 33 | 3 | 63 | 89 | 212 |
ND: not done.
In all cases, the diagnosis of DAH was confirmed by the bronchoscopy. Subsequently and in order to identify a specific etiology, we proceeded to additional laboratory tests, as well as selected serologic and radiographic studies.
In our first case, as no underlying pathology was found, the diagnosis of idiopathic pulmonary hemosiderosis was retained. As previously mentioned pulmonary hemosiderosis is a diagnosis of exclusion, based on an association of anemia, chest X-ray pulmonary infiltrates and the presence of hemosiderin-laden macrophages in the bronchoalveolar lavage. Further investigation was non contributive for this infant.
The next two cases of DAH were due to infectious causes. In our second case, culture analysis of tracheal aspirate samples identified the presence of Chlamydia Trachomatis. Infants born vaginally from infected mothers are at risk of acquiring Chlamydia trachomatis, which can lead to severe tracheobronchial or pneumonic infection and DAH. In our third case, polymerase chain reaction of tracheal aspirate samples identified the presence of Coronavirus NL63. Coronavirus is a common cause of upper respiratory tract infection in children and has also been occasionally associated with lower respiratory tract infections (such as bronchiolitis and pneumonia) and with pulmonary hemorrhage [8]. At present, there are seven coronaviruses recognized as human pathogens (HCoV): HCoV-OC43, HCoV-299E, HCoV-HKU1, HCoV-NL63, SARS CoV, MERS-CoV and the newly identified SARS COV-2 [25]. The use of reverse transcriptase polymerase chain reaction helps in the rapid and reliable detection of these viruses. It is noteworthy, that pulmonary hemorrhage in children has been mainly associated with bacterial infections, such as Staphylococcus aureus, in relation to necrotizing pneumonia [6], by fungi, such as Stachybotrys Chartarum [11] and occasionally by virus such as H1N1 influenza [7]. To our knowledge, our patients are the second reported cases of pulmonary hemorrhage in infants associated with chlamydia trachomatis [5] and coronavirus infection [8], respectively.
In our fourth case, mainly according to detailed anamnestic data, accidental suffocation and asphyxia were probably the causes of the DAH. It is worth mentioning that the infant received an objective evaluation including ophthalmologic examination and head imaging because of initial suspicion of abuse. Suffocation and shaken baby syndrome are the most difficult components to exclude in the differential diagnosis of pulmonary hemorrhage.
In our last case, serum immunoglobulin levels (IgG, IgA, IgM, IgE) and milk-specific serum IgE were normal but interestingly high precipitating cow's milk proteins antibodies titers was found and Heiner syndrome (HS) was diagnosed. Heiner syndrome (HS) is a cow's milk (CM) hypersensitivity pulmonary disease that affects primarily infants. Moissidis et al., recently reported a series of infants with recurrent respiratory symptoms and iron deficiency anemia. All of these children presented symptomatic and radiologic improvement with the eviction of cow's milk proteins [2,13].
The immunologic mechanism in milk-induced pulmonary disease is incompletely clear. The formation of immune complexes (Gell and Coombs' type III) or cell-mediated reaction (Gell and Coombs' type IV) may have a role. Patients with HS characteristically have high titers of milk-specific IgG antibodies (which is not pathognomic of the disease) and some of them may have high serum total IgE levels and milk-specific IgE antibodies. Although this syndrome remains a controversial entity which has been rarely reported in the medical literature, it should be particularly suspected in pediatric pulmonary practices. Insufficient awareness about this disease is probably a major factor in its misdiagnosis and its morbidity.
Table 3 presents data regarding assessments, diagnosis, and treatment for the five cases presented.
6. Treatment and prognosis
In our five cases, none had elevated milk-specific IgE antibodies and only one had positive IgG antibodies against CM proteins. However, considering the young age of our five patients and the immaturity of the infant's immune system, our policy was to remove cow's milk from the diet of infants and control the serum immunoglobulins levels later in life.
In acute phase, the treatment was symptomatic (transfusion, oxygen therapy and, if needed, ventilatory support) for all the patients. For the second case we concluded to interstitial pneumonitis and a diffuse alveolar hemorrhage due to an infectious agent for which the patient received antimicrobial therapy by oral clarithromycin 15mg/kg/day for 21 days. For all the other cases, the first-line curative treatment was oral corticosteroids. Corticosteroids have been reported to be associated with decreased pulmonary bleeding relapses and pulmonary fibrosis progression, as well as with higher survival rates [10]. Since the recommended duration of corticosteroids treatment is variable among the patients based on clinical, radiological, and biological evolution, our patients received prolonged treatment for 3–6 months [23]. In small case series of severe DAH, which does not improve with intravenous corticosteroids, the use of intrapulmonary recombinant factor VII a, has been described to obtain good results [20]. In chronic cases of pulmonary hemorrhage with poor response to steroids, or in cases associated with systemic diseases, immunosuppressive agents such as azathioprine, methotrexate, and cyclophosphamide have been used with variable results [10,16].
All of our five cases are followed up closely in respiratory outpatient clinic and none of them has had further episodes of pulmonary bleeding up to 12 months after discharge.
Recent retrospective case studies have shown significantly better survival, with five-year survival rates above 80%. Prolonged remission is possible; however, later death from the disease remains a possibility [9]. The cause of death is generally terminal chronic respiratory failure but may also be massive hemoptysis. Sometimes DAH is immune-mediated and the prognosis of these patients in terms of morbidity and mortality may be affected by the extent of involvement in other organs [19].
7. Conclusion
This article focuses on diffuse alveolar hemorrhage in infancy. In childhood and mostly in infancy, diffuse alveolar hemorrhage present as a rare but serious medical emergency. The differential diagnosis in infants includes cardiopulmonary vascular malformations, infection, coagulation disorders, food hypersensitivity syndromes and idiopathic pulmonary hemosiderosis. Vasculitis and collagenosis are extremely rare in infancy. An early diagnosis is crucial. As highlighted by these case reports, high index of suspicion, adequate etiologic screening and appropriate treatment are mandatory to improve survival.
Declaration of competing interest
The authors declare that they have no competing interests.
Acknowledgements
Not applicable.
Abbreviations
- DAH
Diffuse Alveolar Hemorrhage
- CM
Cow Milk
- CT
Computed tomography
- WBC
White Blood Cells
- BAL
Bronchoscopic Alveolar Lavage
- NICU
Neonatal intensive Care Unit
- PDA
Patent Ductus Arteriosus
- VSD
Ventricular Septal Defect
- SIDS
Sudden Infant Death Syndrome
- IPH
Idiopathic Pulmonary Hemosiderosis
- AH
Alveolar Hemorrhage
- HLMs
Hemosiderin Laden Macrophages
- ANA
Antinuclear Antibodies
- GBM
Glomerular Basement Membrane
- ANCA
Antineutrophil Cytoplasmic Antibodies
- bpm
beats per minute
Authors' contributions
EG and MM were involved in writing, reading and editing the manuscript. All authors read and approved the final manuscript.
Funding
The authors thank the University of Liege for the support and funding of this publication.
References
- 1.Parrot A., Picard C., Fartoukh M., Vincent F., Mayaud C. Hémorragies intra-alvéolaires. Diagnostic et traitement. Reanimation. 2005;14(7):614–620. [Google Scholar]
- 2.Godfrey S. Pulmonary hemorrhage/hemoptysis in children. Pediatr. Pulmonol. 2004;37(6):476–484. doi: 10.1002/ppul.20020. [DOI] [PubMed] [Google Scholar]
- 3.Sherman J.M., Winnie G., Thomassen M.J., Abdul-Karim F.W., Boat T.F. Time course of hemosiderin production and clearance by human pulmonary macrophages. Chest. 1984;86(3):409–411. doi: 10.1378/chest.86.3.409. [DOI] [PubMed] [Google Scholar]
- 4.Epstein C.E., Elidemir O., Colasurdo G.N., Fan L.L. Time course of hemosiderin production by alveolar macrophages in a murine model. Chest. 2001;120(6):2013–2020. doi: 10.1378/chest.120.6.2013. [DOI] [PubMed] [Google Scholar]
- 5.Thompson J.W., Nguyen C.D., Schoumacher R.A., Lazar R.H., Hamdan F., Stocks R.M., Van Nguyen K. Evaluation and management of hemoptysis in infants and children a report of nine cases. Ann. Otol. Rhinol. Laryngol. 1996;105(7):516–520. doi: 10.1177/000348949610500704. [DOI] [PubMed] [Google Scholar]
- 6.Boussaud V., Parrot A., Mayaud C., Wislez M., Antoine M., Picard C., Cadranel J. Life-threatening hemoptysis in adults with community-acquired pneumonia due to Panton-Valentine leukocidin-secreting Staphylococcus aureus. Intensive Care Med. 2003;29(10):1840–1843. doi: 10.1007/s00134-003-1918-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Gilbert C.R., Vipul K., Baram M. Novel H1N1 influenza A viral infection complicated by alveolar hemorrhage. Respir. Care. 2010;55(5):623–625. [PubMed] [Google Scholar]
- 8.Agarwal P., Arora H., Abdulhamid I., Asmar B., Natarajan G., Chawla S. Pulmonary hemorrhage in an infant with coronavirus infection. J. Neonatal Biol. 2015;4(175) 2167-0987. [Google Scholar]
- 9.Le L.C., Le M.B., Fauroux B., Forenza N., Dommergues J.P., Desbois J.C.…Pin I. Long-term outcome of idiopathic pulmonary hemosiderosis in children. Medicine. 2000;79(5):318–326. doi: 10.1097/00005792-200009000-00005. [DOI] [PubMed] [Google Scholar]
- 10.Taytard J., Nathan N., De Blic J., Fayon M., Epaud R., Deschildre A., Cros P. New insights into pediatric idiopathic pulmonary hemosiderosis: the French RespiRare® cohort. Orphanet J. Rare Dis. 2013;8(1):161. doi: 10.1186/1750-1172-8-161. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Dearborn D.G., Smith P.G., Dahms B.B., Allan T.M., Sorenson W.G., Montana E., Etzel R.A. Clinical profile of 30 infants with acute pulmonary hemorrhage in Cleveland. Pediatrics. 2002;110(3):627–637. doi: 10.1542/peds.110.3.627. [DOI] [PubMed] [Google Scholar]
- 12.Gencer M., Ceylan E., Bitiren M., Koc A. Two sisters with idiopathic pulmonary hemosiderosis. Can. Respir. J. J. Can. Thorac. Soc. 2007;14(8):490–493. doi: 10.1155/2007/150926. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Moissidis I., Chaidaroon D., Vichyanond P., Bahna S.L. Milk‐induced pulmonary disease in infants (Heiner syndrome) Pediatr. Allergy Immunol. 2005;16(6):545–552. doi: 10.1111/j.1399-3038.2005.00291.x. [DOI] [PubMed] [Google Scholar]
- 14.Jacanamijoy A.B., Silva D.C.G., Méndez J.C.B., Roa J.D., Vásquez P. Acute idiopathic pulmonary hemorrhage in infants. Report of two cases and literature review. Case Rep. 2016;2(2):19–29. [Google Scholar]
- 16.Fullmer J.J., Langston C., Dishop M.K., Fan L.L. Pulmonary capillaritis in children: a review of eight cases with comparison to other alveolar hemorrhage syndromes. J. Pediatr. 2005;146(3):376–381. doi: 10.1016/j.jpeds.2004.10.025. [DOI] [PubMed] [Google Scholar]
- 17.Von Vigier R.O., Trummler S.A., Laux‐End R., Sauvain M.J., Truttmann A.C., Bianchetti M.G. Pulmonary renal syndrome in childhood: a report of twenty‐one cases and a review of the literature. Pediatr. Pulmonol. 2000;29(5):382–388. doi: 10.1002/(sici)1099-0496(200005)29:5<382::aid-ppul7>3.0.co;2-d. [DOI] [PubMed] [Google Scholar]
- 18.Harris N.L.M.D., McNeely W.F.M.D. Case records of the Massachusetts general hospital: case 30-2002. N. Engl. J. Med. 2002;347(13):1009–1017. doi: 10.1056/NEJMcpc020022. [DOI] [PubMed] [Google Scholar]
- 19.Susarla S.C., Fan L.L. Diffuse alveolar hemorrhage syndromes in children. Curr. Opin. Pediatr. 2007;19(3):314–320. doi: 10.1097/MOP.0b013e3280dd8c4a. [DOI] [PubMed] [Google Scholar]
- 20.Park J.A., Kim B.J. Intrapulmonary recombinant factor VIIa for diffuse alveolar hemorrhage in children. Pediatrics. 2015;135(1):216–220. doi: 10.1542/peds.2014-1782. [DOI] [PubMed] [Google Scholar]
- 21.Lazor R. Alveolar hemorrhage syndromes. Orphan lung diseases. Eur. Respir. Monogr. 2011;54:15–31. [Google Scholar]
- 22.Coss-Bu J.A., Sachdeva R.C., Bricker J.T., Harrison G.M., Jefferson L.S. Hemoptysis: a 10-year retrospective study. Pediatr. Engl. Ed. 1997;100(3):e7. doi: 10.1542/peds.100.3.e7. [DOI] [PubMed] [Google Scholar]
- 23.Schwarz M.I. Wolters Kluwer; 2015. The Diffuse Alveolar Hemorrhage Syndromes. Alphen Aan Den Rijn. [Google Scholar]
- 24.Milman N., Pedersen F.M. 2013. Idiopathic Pulmonary Hemosiderosis. UpToDate Oct. 2017. [PubMed] [Google Scholar]
- 25.Teramoto S. Clinical significance of aspiration pneumonia and diffuse aspiration bronchiolitis in the elderly. J. Gerontol. Geriatr. Res. 2014;3(142) [Google Scholar]