Abstract
Since January 2020, there has been a worldwide pandemic of COVID-19, caused by a novel coronavirus–severe acute respiratory syndrome coronavirus 2. The United States has been particularly affected, with the largest number of confirmed cases in a single country in the world. Healthcare systems for adults as well as children have dealt with challenges. This article will reflect on the experiences of selected children’s hospitals in Seattle, New York City, and New Orleans, three of the “hotspots” in the US and share common aspects and lessons learned from these experiences. This article discusses testing and cohorting of patients, personal protective equipment utilization, limiting workplace exposure, and information sharing.
Keywords: COVID-19, United States, Children’s Hospitals
Introduction
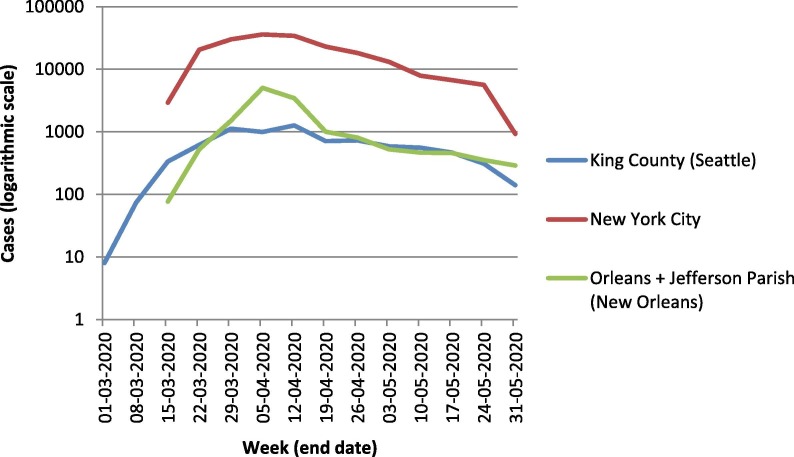
In January 2020, a novel coronavirus–severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) [1]—was identified, and by March 11th the disease it causes, COVID-19, was declared a worldwide pandemic [2]. The United States has been particularly affected, with more than 1.7 million cases as of the end of May, the largest number of confirmed cases in a single country in the world [3]. The country has been in a state of emergency since the 13th of March [4], and by mid-March all fifty states, the District of Columbia, and four U.S. territories had reported cases of COVID-19 [5]. Although the majority of severe illness has been seen in adults, leading to immense challenges for hospitals and healthcare systems, COVID-19 also has profound impact on the healthcare systems for children as well. Seattle, New York City, and New Orleans were three “hotspots” of COVID-19 infections in the US [Table1 ], each with unique epidemiologic features contributing to their case rate [Fig. 1 ].
Table 1.
Epidemiology of COVID-19, as of May 28, 2020.
Fig. 1.
In this review, we reflect on the experiences of selected children’s hospitals (Seattle Children’s, Children’s Hospital at Montefiore in New York, and Children’s Hospital New Orleans) in each of these cities, with the aim of identifying commonalities and lessons learned that might be applicable to future health crises.
Seattle
On January 21, 2020, a 35 year old man who had returned to Washington a few days prior after traveling to Wuhan, China became the first confirmed case of COVID-19 in the Seattle area [9], [10]. In late February, the Seattle Flu Study identified COVID-19 in a 15 year old evaluated for influenza-like illness, and using sequence data, linked this case to the first adult case [11], [12], demonstrating ongoing community transmission. Also in late February, a large ongoing outbreak was reported by an area nursing home, further reflecting and contributing to community spread. In response, regional hospitals braced for patient surges and planned for overwhelmed healthcare systems and alternate standards of care. By the end of March, approximately 200 new cases were being identified per day in King County (the Seattle region).
At Seattle Children’s Hospital, a multidisciplinary group began meeting regularly at the end of January to plan the response to COVID-19, and by the end of February an incident command structure was erected in order to provide for centralized decision-making and rapid escalation of questions and concerns. The experience in China suggested that children accounted for a very small proportion of COVID-19 cases and that their symptoms and signs were relatively mild compared to adults. Thus, while the hospital planned for a surge of pediatric patients out of caution, they also planned to care for the region’s children who would otherwise be cared for at mixed adult-pediatric hospitals and prepared to admit sick young adults in the event the adult hospitals reached their capacity. In the end, perhaps in part due to suspension of all elective visits and surgeries, and the ‘shelter in place’ strategies employed as of March 23rd, [13] the adult hospitals avoided exceeding their capacity and Seattle Children’s maintained available beds.
New York City
Nearly six weeks after the Seattle area saw its first case, the first case of COVID-19 in New York State was confirmed on March 1st: a woman who had returned home to New York City (NYC) after travel to Iran [14]. By March 15th, there were nearly 3000 identified cases in NYC and by the end of March, 3500–6000 new cases were being identified each day [7]. Multiple factors may have contributed to this huge increase, including high population density and reliance on crowded public transportation, in addition to the more than two-week period from when the first cases were reported until the official NYC shutdown began, and three week period until the definitive ‘stay at home’ order on March 22nd [15]. Given NYC’s accelerated rate of transmission, hospitals feared that a surge of pediatric patients in the emergency department, including the “worried well”, would lead to admissions. There was particular concern in the Bronx, the borough in which our hospital system is primarily located, given that it is one of the poorest areas of the state and the rates of obesity, asthma, and other co-morbidities thought to exacerbate COVID-19 are very high [16], [17]. Although ultimately the Bronx did experience a disproportionate number of cases and death in adults [7], pediatric ED visits and admissions remained low, and dropped even further after NYC public schools closed and non-urgent procedures were cancelled. Efforts were made in the Bronx to consolidate pediatric admissions at the Children’s Hospital at Montefiore in anticipation of the need to increase capacity for adult patients across NYC [18].
The Children’s Hospital at Montefiore (CHAM) is a part of a large health system and is situated within the main Montefiore Hospital campus. In order to help alleviate some of the burden on our adult colleagues and in preparation for an anticipated peak in the first two weeks of April, pediatric leadership met with institutional leadership regularly, and surge plans were put into place. Pediatric providers, nurses and staff employed a “surge in place” model, creating and staffing an adult COVID-19 unit [19]; increased the age limit on pediatric med-surg units to 30 years; and deployed multiple providers and staff to units run by adult providers.
New Orleans
The first case of presumptive COVID-19 in the greater metropolitan area of New Orleans was identified on March 9th, approximately one week after the first case in NYC. Over the next week, several more cases were identified in individuals who had no significant travel history and were unrelated to each other, suggesting that there was previously unrecognized existence of disease and presence of community transmission in the area. New Orleans had recently celebrated Mardi Gras during the last two weeks of February, when nearly one million visitors from around the country and world visited the area. It has been suggested that the Mardi Gras celebration may have significantly accelerated transmission within the community and possibly led to the virus’s spread around the country [20]. Currently available sequencing data [21] indicate that a small number of closely related strains were introduced, likely in late February or early March, and those strains spread rapidly within the New Orleans community.
Within a week of the first case, state and local officials moved to decrease transmission. Schools were closed on March 20th, 2020 and restrictions on business activities followed shortly thereafter, leading to a predictable decline in visits to the pediatric Emergency Room at Children’s Hospital New Orleans (CHNOLA). As a part of a hospital system with four adult hospital partners, CHNOLA leaders were acutely aware of the stressors that colleagues across the system faced, and set up an Incident Command team on March 11th with broad representation. A subset of this group met twice a day with leaders from across the system so that decisions made at CHNOLA were based on the real-time activities at adult partner facilities. Pediatric acute and critical care units were consolidated in anticipation of the need to accommodate adult patients during the predicted surge. However, their adult partners expanded their own capacity to absorb the surge which peaked in the last week of March through the first week of April, and CHNOLA did not care for any adult patients. However, CHNOLA clinical and non-clinical team members were deployed to adult facilities to assist in a variety of ways. In addition, supplies including ventilators, medications, and personal protective equipment (PPE) were shared to meet the needs of each facility in the health system as dictated by clinical volumes.
Discussion
As COVID-19 spread across the United States, there were factors unique to each city which influenced the individual experiences. Seattle was the first major US city to experience COVID-19, and therefore faced the need to implement COVID-19 policies immediately. New York City, with its high population density and delayed implementation of strict social distancing, had a rate of spread and acute surge that challenged hospitals and healthcare systems to an extent not seen in other US cities. New Orleans hosted a highly attended event in February before the threat of transmission in the US was fully appreciated, and thus likely had an increase in community spread that may have been initially under-recognized [5]. Despite these different starting points, the three children’s hospitals shared many similar experiences.
Testing and cohorting patients
All three institutions faced limited testing capabilities [22]. Each region initially relied on testing through local Public Health or Department of Health (DoH) centers, which pragmatically prevented widespread testing. When testing capability was expanded to include in-hospital and commercial laboratories, limited supplies of reagent and swabs threatened testing ability. Each institution employed strict criteria aimed to allow testing of patients most at risk for severe disease or of transmitting disease. Although each site used a different algorithm, initial criteria at all three included fever, cough/shortness of breath, and risk of exposure (travel to certain areas, known exposure to someone with confirmed or highly suspected disease). Children with certain chronic medical illnesses who presented with respiratory symptoms were given preference for testing as well. As the understanding of disease transmission and the recognition of the possible constellation of presenting symptoms evolved, and availability of rapid testing improved, criteria for testing were expanded. Currently, all three institutions are performing COVID-19 testing on a broader population, including all patients presenting for surgeries or those requiring aerosol-generating procedures, admitted patients, and a subset of patients presenting to the emergency room. Patients are prioritized to either in-house or commercial-based tests, depending on urgency of need for results. The number of patients being tested remains highly variable between the three sites [Table 2 ].
Table 2.
COVID-19 testing in each children’s hospital, March 1 to May 27, 2020.
| Seattle | New York City | New Orleans | |
|---|---|---|---|
| Number of tests sent | 3985 | 577 | 1126 |
| Number of positive | 40 | 131 | 29 |
| % positive | 1% | 22.7% | 2.6% |
The evolving ability to test and definitively diagnose COVID-19 drove the need for novel considerations regarding bed assignments and cohorting pediatric inpatients. At Seattle Children’s, a Special Isolation Unit for patients under investigation (PUIs) or with confirmed COVID-19 was created, with controlled access and specially trained staff. At CHNOLA, one of the acute care floors was designated. Because of limited testing initially, every patient with respiratory symptoms was treated as a PUI, despite the fact that RSV and flu were still relatively prevalent and may have accounted for observed symptoms. Once testing became more available, COVID-positive patients could be more exclusively cohorted on the single unit. At CHAM, the initial plan was to house all PUIs and patients with confirmed COVID-19 in an isolated hallway with a single team of nurses and providers. However, because test results initially were only available 48–72 h after admission, and because of the increasing prevalence of disease in the community, there were more pediatric patients who met the definition of PUI than could be accommodated. Expansion of the space designated for COVID-positive or suspected patients, as well as availability of in-house testing with a reduction in time to results availability, allowed for rational cohorting of patients.
Personal protective equipment
As an understanding of how the SARS-CoV-2 virus transmission improved, Center for Diseases Control (CDC) recommendations regarding the use of PPE evolved over time [23]. Simultaneous with rapidly changing recommendations, all three institutions also faced concern over supply shortages, an effect of both increased utilization and a shrinking pipeline. Each institution employed different strategies to ensure adequate protection [22]. First, Seattle Children’s had previously switched from routine use of N95 masks to multi-use powered air purifying respirators (PAPRs) as the primary source of respirators. With a shortage of isolation masks, PAPRs were preferentially used for care of patients with any respiratory symptoms or signs. In addition, re-use strategies for PAPR shields and face shields were employed, and extended use strategies were initiated for PAPRs, face shields, and isolation masks. CHNOLA implemented similar PPE conservation measures nearly immediately during the first week of local disease recognition in order to preserve their supply. At CHAM, PPE inventory information across the health system was shared at the leadership level on a regular basis, and both re-use and multi-use strategies were employed. At the unit level, critical items including N95 masks and face shields, were stored in a central location with controlled access.
Through the three hospitals’ experiences, several strategies for managing PPE shortages emerged as promising: controlling access immediately, monitoring supply closely including tracking utilization, and implementing conservation strategies that may need to change frequently to reflect degree and type of shortages. In addition, capitalizing on appropriate opportunities for PPE discontinuation was recognized as an important strategy [24]. In order to ensure effective use of available supplies, all three sites made PPE references, including donning and doffing protocols [24], easily accessible and interpretable by all frontline clinicians. Once adequate PPE supplies were ensured, each site was able to successfully implement universal masking.
Limiting exposure
Limiting workplace and nosocomial exposure to COVID-19 required a coordinated institutional response [25]. For example, in order to identify potentially infected people quickly and contain the risk of transmission, strategies for screening all staff prior to entering the hospital were implemented at each hospital. All three centers also implemented institutional policies to limit those at the bedside of admitted pediatric patients, in alignment with official recommendations [26] to one parent or primary caretaker. All three institutions suspended team rounds at the bedside, which had previously been a daily part of the workflow, in order to limit staff and patient exposure, and to maintain social distancing [25]. Technology was increasingly utilized, for example calling or face-timing patients and families to obtain histories and answer questions so that PPE could be conserved and movement in and out of patient rooms limited [27]. To minimize overall crowding in buildings and offices, institutions changed prior policies to allow a work-from-home option for non-clinical work. Ambulatory settings in each hospital have seen a marked increase in the use of telemedicine in an attempt to limit unnecessary visits to the hospital campus; this is a strategy that merits further exploration in the inpatient setting.
Information sharing and communication
Timely and accurate communication was crucial within each hospital to avoid any confusion or misinformation that might be potentially generated by the multiple streams of information existing within a complex hospital. All three institutions mitigated this risk by using a centralized system to collect and disseminate information such as treatment protocols, clinical trial information, and epidemiologic data. This allowed each hospital to maintain alignment throughout the organization, and ensure all staff was informed as protocols and policies changed. In addition, in-person communication was key to real-time response. At CHNOLA, members of the Incident Command team made regular rounds in all units to address any questions, concerns and misconceptions, and about PPE conservation in particular. At CHAM, leadership walk rounds and institution-wide virtual town halls occurred daily, allowing staff to interact with leadership and share concerns and successes directly. Pediatric leadership meetings were held twice weekly, to ensure information sharing and to address local issues. At Seattle Children’s, an incident command structure was used for escalation of problems and centralized decision-making. Organization-wide communications happened almost daily and leaders rounded to ensure uptake of the information and to answer questions. In addition, virtual town halls occurred on a regular cadence.
Communication between institutions and providers proved to be equally as important as communication within institutions. The internet and multiple means of electronic communications conferred an ability to disseminate information at a pace unprecedented in any previous health crisis. Federal, state and local agencies provided real-time updates via electronic posts and bulletins to wide audiences in order to ensure that both providers and the public had accurate information about all aspects of the emerging pandemic. Physician group “listservs” [an electronic mailing list] provided timely discussion of new findings as well as information to those in areas which had yet to experience a surge. Indeed, when Seattle Children’s circulated a summary of their experiences and protocols on numerous listservs in early March to members of the pediatric community across the country, CHAM and CHNOLA reaped the benefit of their experience, which enabled a more informed response and an incorporation of their lessons learned into their early planning. Webinars allow for rapid, widespread learning about a novel disease without needing to gather large groups of individuals together. In fact, institutions continue to use these channels to share information about the evolving clinical picture and treatment of the newly recognized covid-19 associated Multi-system Inflammatory Syndrome in Children (MIS-C). Lastly, social media platforms allow for sharing of reflections, provision of emotional support and communal mourning as well as celebration, which may be comforting to providers navigating the myriad challenges of the pandemic.
Conclusion
During the winter and spring of 2020, the three selected children’s hospitals in Seattle, New York City, and New Orleans initially experienced the COVID-19 pandemic differently because of unique contextual factors. However, all three institutions faced the challenges of addressing the needs of their communities with a strong spirit of cooperation, resilience, and adaptability among the pediatric staff, which allowed for the flexibility necessary to respond to the fluid nature of the situation. With emerging knowledge about the virus and by accumulating experience managing it, the three institutions independently developed solutions which, taken together, can inform our understanding and can drive responses to future recurrences or new pandemics should they arise.
Directions for future research
-
•
Determine the impact of transmission mitigation strategies on the inpatient experience for patients and their families.
-
•
Identify which of the PPE conservation strategies utilized are most effective in maintaining adequate supply.
-
•
Characterize effective use of telemedicine and other electronic communication with patients in the inpatient setting.
Funding
None.
Acknowledgements
The authors would like to thank Dr. Margaret Aldrich for providing data regarding COVID-19 testing at CHAM.
References
- 1.Centers for Disease Control and Prevention. Coronavirus Disease 2019, Cases in the U.S. https://www.cdc.gov/coronavirus/2019-ncov/cases-updates/cases-in-us.html. Accessed May 20, 2020.
- 2.World Health Organization. Rolling updates on coronavirus disease (COVID-19). 2020; https://www.who.int/emergencies/diseases/novel-coronavirus-2019/events-as-they-happen. Accessed May 31, 2020.
- 3.Coronavirus Resource Center. https://coronavirus.jhu.edu/. Accessed May 15, 2020.
- 4.Federal Emergency Management Agency. Bringing resources to state, local, tribal & territorial governments. https://www.fema.gov/coronavirus/governments. Accessed May 16, 2020.
- 5.Geographic Differences in COVID-19 Cases, Deaths, and Incidence – United States, February 12-April 7, 2020. MMWR. Morbidity Mortality Weekly Report 2020;69(15):465–71. [DOI] [PMC free article] [PubMed]
- 6.King County Department of Health. Daily COVID-19 outbreak summary. 2020; https://www.kingcounty.gov/depts/health/covid-19/data/daily-summary.aspx. Accessed May 31, 2020.
- 7.New York City Department of Health. COVID-19: Data. 2020; https://www1.nyc.gov/site/doh/covid/covid-19-data.page. Accessed May 28, 2020.
- 8.Louisiana Department of Health. COVID-19. 2020; http://ldh.la.gov/Coronavirus/. Accessed May 29, 2020.
- 9.Holshue M.L., DeBolt C., Lindquist S. First case of 2019 novel coronavirus in the United States. N Engl J Med. 2020;382(10):929–936. doi: 10.1056/NEJMoa2001191. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Centers for Disease Control and Prevention. First Travel-related Case of 2019 Novel Coronavirus Detected in United States. https://www.cdc.gov/media/releases/2020/p0121-novel-coronavirus-travel-case.html. Accessed May 20, 2020.
- 11.Chu HY, Englund JA, Starita LM, et al. Early Detection of Covid-19 through a Citywide Pandemic Surveillance Platform. N Engl J Med. Published online ahead of print, May 1, 2020. [DOI] [PMC free article] [PubMed]
- 12.Bedford T. Cryptic transmission of novel coronavirus revealed by genomic epidemiology. 2020; https://bedford.io/blog/ncov-cryptic-transmission/. Accessed May 20, 2020.
- 13.Inslee J. Stay Home-Stay Healthy. Proclamation by the Governor 2020; https://www.governor.wa.gov/sites/default/files/proclamations/20-25%20Coronovirus%20Stay%20Safe-Stay%20Healthy%20%28tmp%29%20%28002%29.pdf. Accessed May 31, 2020.
- 14.Goldstein J, McKinley J. Coronavirus in N.Y.: Manhattan Woman Is First Confirmed Case in State. New York Times. March 1, 2020.
- 15.New York State. New York State on PAUSE. 2020; https://coronavirus.health.ny.gov/new-york-state-pause. Accessed May 31, 2020.
- 16.Warman K., Silver E.J., Wood P.R. Modifiable risk factors for asthma morbidity in Bronx versus other inner-city children. J Asthma. 2009;46(10):995–1000. doi: 10.3109/02770900903350481. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Franki R. Comorbidities the rule in New York’s COVID-19 deaths. The Hospitalist. 2020 [Google Scholar]
- 18.Amid Ongoing COVID-19 Pandemic, Governor Cuomo Announces Initial Delivery of Equipment and Supplies for Javits Center Temporary Hospital [press release]. March 23, 2020 2020.
- 19.Philips K, Uong A, Buckenmyer T, et al. Rapid Implementation of an Adult Coronavirus Disease 2019 Unit in a Children's Hospital. J Pediatrics. Published online ahead of print, May 4, 2020. [DOI] [PMC free article] [PubMed]
- 20.Reckdahl K, Robertson C, Fausset R. New Orleans Coronavirus: City Faces a Nightmare, and Mardi Gras May Be Why. The New York Times. March 26, 2020.
- 21.Nextstrain. Genomic epidemiology of novel coronavirus – Global subsampling. 2020; https://nextstrain.org/ncov/global. Accessed May 25, 2020.
- 22.Nathavitharana R.R., Patel P.K., Tierney D.B. Innovation and knowledge sharing can transform COVID-19 infection prevention response. J Hospital Med. 2020;5:299–301. doi: 10.12788/jhm.3439. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Centers for Disease Control and Prevention. Strategies to Optimize the Supply of PPE and Equipment. 2020; https://www.cdc.gov/coronavirus/2019-ncov/hcp/healthcare-supply-ppe.html. Accessed May 26, 2020.
- 24.Steuart R., Huang F.S., Schaffzin J.K., Thomson J. Finding the value in personal protective equipment for hospitalized patients during a pandemic and beyond. J Hospital Med. 2020;15(5):295–298. doi: 10.12788/jhm.3429. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Arora V.M., Chivu M., Schram A., Meltzer D. Implementing physical distancing in the hospital: a key strategy to prevent nosocomial transmission of COVID-19. J Hospital Med. 2020;15(5):290–291. doi: 10.12788/jhm.3434. [DOI] [PubMed] [Google Scholar]
- 26.Centers for Disease Control and Prevention. Interim Infection Prevention and Control Recommendations for Patients with Suspected or Confirmed Coronavirus Disease 2019 (COVID-19) in Healthcare Settings. 2020. https://www.cdc.gov/coronavirus/2019-ncov/hcp/infection-control-recommendations.html. Accessed May 31, 2020.
- 27.Cho H.J., Feldman L.S., Keller S., Hoffman A., Pahwa A.K., Krouss M. Choosing wisely in the COVID-19 era: preventing harm to healthcare workers. J Hospital Med. 2020;6:360–362. doi: 10.12788/jhm.3457. [DOI] [PMC free article] [PubMed] [Google Scholar]