Twin pregnancies have increased significantly over recent decades, mainly due to the growing rate of such pregnancies that have been achieved via assisted reproductive techniques. Twin pregnancies are associated with high infant morbidity and mortality. Maternal obesity has been found to be significantly related to an increased risk of pre-eclampsia and other adverse outcomes. Maternal weight gains during pregnancy may have important implications for maternal and fetus health. Women with excessive gestational weight gains (GWG) are more likely to increase their risk of gestational diabetes mellitus (GDM), macrosomia, preterm birth, and fetal growth restriction. As with singletons, GDM is also expected to be more frequent in pre-gravid obese mothers of twins.[1] Although there are some guides for twin pregnancies, few researches are focused on the systematic management of twin pregnancies. The main goal of this study was to assess the benefits of systematic management of twin pregnancies, especially GDM-like diet and exercise management models.
This research examined the data of all twin pregnancies in this hospital from January 1, 2013 to December 31, 2017. This study was approved by the Ethics Committee of International Peace Maternity and Child Health Hospital (No. GKLW 2015-62). All study subjects gave written informed consents before the study. As the focus of obstetric management, twin pregnancies have a high rate of pregnancy complications. In mid-2014, a specialist clinic for twin pregnancies was established, we began to give systematic guidance to twin pregnancies, including diet, physical activity, weight control, sleep, and mentality. The weight control was made according to the recommendation of the Institute of Medicine in 2009. The research population were the twin pregnancies delivered in 2015 to 2017, with those delivered in 2013 to 2014 as a control group. The inclusion criteria were all twins delivered after 26 weeks of pregnancy in this hospital. Exclusion criteria were: (1) gestational age at delivery of <26 weeks, (2) stillbirth before labor, and (3) fetal reduction for congenital fetal anomalies. The research compared twin pregnancy complications to assess the benefits of systematic management.
Data were examined for missing and extreme values, with logics checked. Descriptive statistics included the numbers and percentages for categorical variables. Prenatal weight gain data were presented as the mean ± standard deviation. The differences in ages and pre-pregnancy body mass index (BMI) between the two groups were assessed with the independent-sample t test, and χ2 tests were made for dichotomous outcomes. Logistic regression was used to determine the risk ratio (RR) and 95% confidence intervals (CIs) of pregnancy complications. All data were analyzed with SPSS software (version 21; IBM Corp., Armonk, NY, USA). A P value of <0.05 was considered statistically significant.
After restricting the sample according to the inclusion and exclusion criteria, this research abstracted data on 1994 twin pregnancy mothers who delivered from 2013 to 2017 at International Peace Maternity and Child Health Hospital (China), which is one of the largest labor centers in Shanghai, with 11,000 to 17,000 annual deliveries. And 710 twin pregnancy women were in control group, with a total of deliveries of 32,269 (710/32,269, or 2.20%); and 1284 twin pregnancy women were in the intervention group, with a total of deliveries of 48,986 (1284/48,986, or 2.62%). Two hundred and sixty-three women were excluded due to fetal reduction for congenital fetal anomalies, with gestational age <26 weeks at delivery, or stillbirth.
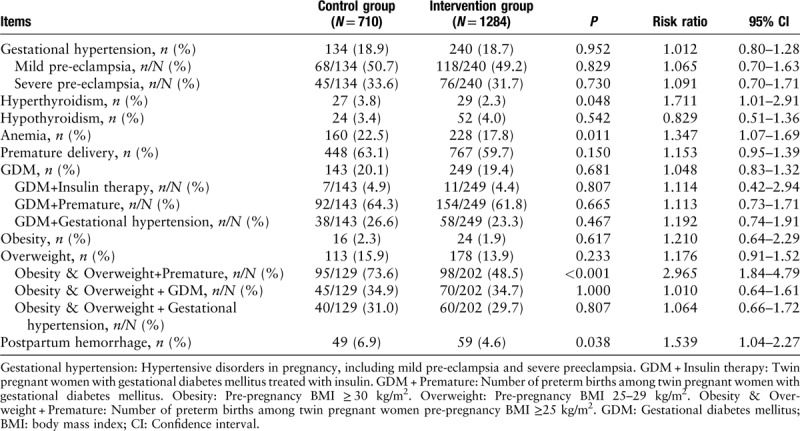
Table 1 demonstrated the rates of maternal complications of the twin pregnancies. The pregnant women with obesity & overweight who received comprehensive management guidance had been obviously lowered their rate of preterm birth (73.6% vs. 45.8%, P < 0.01, RR: 2.965, 95% CI: 1.84–4.79). And it showed a dramatic decline in the rates of hyperthyroidism (3.8% vs. 2.3%, P < 0.05, RR: 1.711, 95% CI: 1.01–2.91), anemia (22.5% vs. 17.8%, P < 0.05, RR: 1.347, 95% CI: 1.07–1.69), and postpartum hemorrhage (6.9% vs. 4.6%, P < 0.05, RR: 1.539, 95% CI: 1.04–2.27). The rates of gestational hypertension (18.9% vs. 18.7%), GDM (20.1% vs. 19.4%), GDM & insulin therapy (4.9% vs. 4.4%), GDM & premature (64.3% vs. 61.8%), GDM & gestational hypertension (26.6% vs. 23.3%), obesity/overweight & GDM (34.9% vs. 34.7%), and obesity/overweight & gestational hypertension (31.0% vs. 29.7%) declined in the intervention group. But this research observed no significant difference between the two groups.
Table 1.
Maternal complications in the twin pregnancy.
The theoretical basis of the management plan under this research includes the following aspects. First, the pregnancy is defined as a diabetogenic event determined by the hormones produced by placenta, having an effect of the insulin resistance. The fact that the weight of placenta is higher in women with diabetes is more frequently found. In twins, the placenta is larger, hormones are more abundant, and diabetes is more common. Second, due to the metabolic rate and dietary habits, it is easier to be morbid obesity (BMI ≥40 kg/m2) for obese or overweight pregnant women, and then it will increase the mortality of maternal and fetal.[2] Lastly, many twin pregnant women are unwilling to do physical activities, which is harmful to the cardio-pulmonary functions and disadvantageous to maintaining uterine muscle tension. There are few researches on twin pregnant women's exercises and diets.
The comorbidity of obesity and GDM is important to the prognosis of twin pregnancies. A study assessing the effectiveness of regular physical activities for preventing GDM has demonstrated a high ability of exercises to reduce GDM risks and improve glucose metabolism.[3] According to this research, the relationship between GDM and preterm birth was not significant. These results are consistent with a meta-analysis that finds no difference in gestational ages at delivery in GDM vs. non-GDM twins.[4] The physiological differences between twin pregnancies and singletons should be considered when assessing glucose tolerance in twin pregnancies.
Several studies have shown that maternal anemia of pregnant women may lead to premature birth.[5] This research found a dramatic decline in the rates of anemia (P < 0.05) and obesity & overweight in connection with premature (P < 0.01) in the intervention group. And it also found that the incidence of the total premature birth rate decreased in the intervention group. But there was no significant difference compared with the control group.
Through comprehensive management, including dietary guidance, the weight of pregnant women was under control, and the incidence of GDM and gestational hypertension also significantly decreased in twin pregnant women who had been diagnosed with obesity. Pregnant women with high BMI index often belong to the high-risk group of premature birth, but in this study, twin pregnancies were arranged with a certain amount of exercises, combined with dietary guidance. As a result, the incidence of preterm labor was significantly decreased.
These findings highlight the importance of systematic management, especially GDM-like diet and exercise management, for twin pregnancies. Regular physical activities, nutrition guidance, and psychological counseling during pregnancy are helpful in reducing the perinatal complications of twin pregnancies. And regular physical activities do not increase the rate of premature of twins. Instead, they are possibly associated with reduced postpartum hemorrhage. Future studies are needed to further analyze the impact of system management on complex twins.
Funding
This work was supported by the National Natural Science Foundation of China (No. 81971401), Chinese Academy of Medical Sciences Research Unit (No. 2019RU056), CAMS Innovation Fund for Medical Sciences (No. 2019-I2M-5-064), the Western Medicine Guide Project of Shanghai Science and Technology Commission (No. 19411960900), and the Project of Translational Medicine Cross-research Fund, Shanghai JiaoTong University (No. ZH2018QNB14).
Conflict of interest
None.
Footnotes
How to cite this article: Gao L, Lyu SP, Zhao XR, Wu Y, Hua RY, Wang S, Zhang Y, Wang YL. Systematic management of twin pregnancies to reduce pregnancy complications. Chin Med J 2020;133:1355–1357. doi: 10.1097/CM9.0000000000000808
References
- 1.Lucovnik M, Blickstein I, Verdenik I, Trojner-Bregar A, Tul N. Maternal obesity in singleton versus twin gestations: a population-based matched casecontrol study. J Matern Fetal Neonatal Med 2015; 28:623–625. doi: 10.3109/14767058.2014.928854. [DOI] [PubMed] [Google Scholar]
- 2.Dolin CD, Kominiarek MA. Pregnancy in women with obesity. Obstet Gynecol Clin North Am 2018; 45:217–232. doi: 10.1016/j.ogc.2018.01.005. [DOI] [PubMed] [Google Scholar]
- 3.Mottola MF, Nagpal TS, Begeginski R, Davenport MH, Poitras VJ, Gray CE, et al. Is supine exercise associated with adverse maternal and fetal outcomes? A systematic review. Br J Sports Med 2019; 53:82–89. doi: 10.1136/bjsports-2018-099919. [DOI] [PubMed] [Google Scholar]
- 4.McGrath RT, Hocking SL, Scott ES, Seeho SK, Fulcher GR, Glastras SJ. Outcomes of twin pregnancies complicated by gestational diabetes: a meta-analysis of observational studies. J Perinatol 2017; 37:360–368. doi: 10.1038/jp.2016.254. [DOI] [PubMed] [Google Scholar]
- 5.Zhang Y, Li Z, Li H, Jin L, Zhang Y, Zhang L, et al. Maternal haemoglobin concentration and risk of preterm birth in a Chinese population. J Obstet Gynaecol 2018; 38:32–37. doi: 10.1080/01443615.2017.1325454. [DOI] [PubMed] [Google Scholar]


