COVID-19, the disease caused by the novel coronavirus SARS-CoV-2, was declared a pandemic on March 11, 2020. Although most patients (81%) develop mild illness, 14% develop severe illness, and 5% develop critical illness, including acute respiratory failure, septic shock, and multiorgan dysfunction.1
Point-of-care ultrasound (POCUS), or bedside ultrasound performed by a clinician caring for the patient, is being used to support the diagnosis and serially monitor patients with COVID-19. We performed a literature search of electronically discoverable peer-reviewed publications on POCUS use in COVID-19 from December 1, 2019, to April 10, 2020. We review key POCUS applications that are most relevant to front-line providers in the care of COVID-19 patients.
LUNG AND PLEURAL ULTRASOUND
Diagnosing COVID-19 disease by polymerase chain reaction is limited by availability of testing, delays in test positivity (mean 5.1 days), and high false-negative rate early in the course of the disease (sensitivity 81%).2 Chest computed tomography (CT) scans are often requested during the initial evaluation of suspected COVID-19, but the American College of Radiology has recommend against the routine use of CT scans for diagnosing COVID-19.3
The diagnostic accuracy of lung ultrasound (LUS) has been shown to be similar to chest CT scans in patients presenting with respiratory complaints, such as dyspnea and hypoxemia, caused by non–COVID-19 pneumonia (sensitivity, 85%; specificity, 93%).4 Normal LUS findings correlate well with CT chest scans showing absence of typical ground glass opacities. This negative predictive value is very important.5 However, early in the course of COVID-19, similar to CT scans, LUS may be normal during the first 5 days or in patients with mild disease.2 Unique advantages of LUS in COVID-19 include immediate availability of results, repeatability over time, and performance at the bedside, which avoids transportation of patients to radiology suites and disinfection of large imaging equipment.
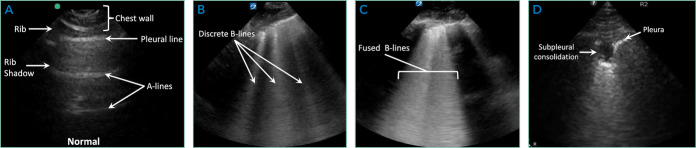
LUS findings in COVID-19 include (a) an irregular, thickened pleural line, (b) B-lines in various patterns (discrete and confluent), (c) small subpleural consolidations, and (d) absence of pleural effusions (Figure). Bilateral, multifocal disease is common, while lobar alveolar consolidation is less common.6,7 In addition to supporting the initial diagnosis, LUS is being used to serially monitor hospitalized COVID-19 patients. As lung interstitial fluid content increases, discrete B-lines become confluent, and the number of affected lung zones increases, which can guide decisions about escalation of care. LUS is often used to guide decisions about prone ventilation, extracorporeal membrane oxygenation, and weaning from mechanical ventilation in acute respiratory failure of non–COVID-19 patients,8 and these concepts are being applied to COVID-19 patients. During recovery, reappearance of A-lines can be seen, but normalization of the LUS pattern is gradual over several weeks based on our experience and one report.9 Multiple LUS protocols examining 6 to 12 lung zones have been published prior to the COVID-19 pandemic. We recommend continuing to use an institutional protocol and evaluating at least one to two rib interspaces on the anterior, lateral, and posterior chest wall.
FIG.
Lung Ultrasound in COVID-19. (A) Normal lung ultrasound is characterized by pleural sliding and A-lines. The following abnormal lung ultrasound findings are typical in COVID-19: (B) discrete B-lines are individual hyperechoic, laser-like artifacts that emanate from the pleural line because of increased interstitial fluid in the acute setting, (C) fused B-lines are seen when individual B-lines coalesce as interstitial fluid increases, (D) subpleural consolidations are small areas (< 3 cm) of consolidation seen just below the pleural line.
FOCUSED CARDIAC ULTRASOUND
Myriad cardiac complications have been described in COVID-19 – including acute coronary syndrome, myocarditis, cardiomyopathy with heart failure, and arrhythmias – secondary to increased cardiac stress from hypoxia, direct myocardial infection, or indirect injury from a hyperinflammatory response. Mortality is higher in patients with hypertension, diabetes, and coronary artery disease.10,11 Cardiac POCUS is being used to evaluate COVID-19 patients when troponin and B-type natriuretic peptide (BNP) are elevated or when there are hemodynamic or electrocardiogram changes. Given the high incidence of venous thromboembolism (VTE) in COVID-19,12 cardiac PO-CUS is being used to rapidly assess for right ventricular (RV) dysfunction and acute pulmonary hypertension.
The American Society of Echocardiography has recommended the use of cardiac POCUS by frontline providers for detection or characterization of preexisting cardiovascular disease, early identification of worsening cardiac function, serial monitoring and examination, and elucidation of cardiovascular pathologies associated with COVID-19.13 Sharing cardiac POCUS images in real time or through an image archive can reduce the need for consultative echocardiography, which ultimately reduces staff exposure, conserves personal protective equipment, and reduces need for decontamination of echocardiographic equipment.
The minimum cardiac POCUS views recommended in COVID-19 patients include the parasternal long-axis and short-axis views (midventricular level), either the apical or sub-costal four-chamber view, and the subcostal long-axis view of the inferior vena cava.13 The goal of a cardiac POCUS exam is to qualitatively assess left ventricular (LV) systolic function, RV size and contractility, gross valvular and regional wall motion abnormalities, and pericardial effusion. In prone position ventilation, the swimmer’s position with one arm elevated above the shoulder may permit acquisition of apical views. Finally, integrated cardiopulmonary ultrasonography, including evaluation for deep vein thrombosis (DVT; see below), is ideal for proper characterization of underlying LV and RV function, volume status, and titration of vasopressor and inotropic support.
VENOUS THROMBOEMBOLISM
COVID-19 has been associated with a proinflammatory and hypercoagulable state with elevated d-dimer and higher-than- expected incidence of VTE (27%) in critically ill patients.12,14 Previous studies have demonstrated that frontline providers, including hospitalists, can detect lower extremity (LE) DVTs with high diagnostic accuracy using POCUS.15 Given the high incidence of DVTs despite prophylactic anticoagulation, some reports have suggested screening or serially monitoring for LE DVT in hospitalized COVID-19 patients.16 In patients with suspected pulmonary embolism (PE), POCUS can rapidly detect venous thrombosis that justifies prompt initiation of anticoagulation (eg, finding DVT or clot-in-transit), supportive findings of PE (eg, acute RV dysfunction, pulmonary infarcts), or alternative diagnoses (eg, bacterial pneumonia). However, it is important to recognize POCUS cannot definitively rule out PE. Additionally, subpleural consolidations are common in COVID-19 patients and could be caused by either infection or infarction. The American Society of Hematology has endorsed the use of POCUS, LE compression ultrasonography, and echocardiography in COVID-19 patients with suspected PE when availability of CT pulmonary angiography or ventilation-perfusion lung scans is limited.14
A POCUS exam for LE DVT consists of two-dimensional venous compression alone and yields results similar to formal vascular studies in both critically ill and noncritically ill patients. Because proximal LE thrombi have the highest risk of embolization, evaluation of the common femoral vein, femoral vein, and popliteal vein is most important.15 Either inability to compress a vein completely with wall-to-wall apposition or visualization of echogenic thrombus within the vein is diagnostic of DVT. Acute thrombi are gelatinous and may appear anechoic, while subacute or chronic thrombi are echogenic, but all veins with a DVT will not compress completely.
VASCULAR ACCESS
Ultrasound guidance for central venous catheter (CVC) insertion has been shown to increase procedure success rates and decrease mechanical complications, primarily arterial puncture and pneumothorax. Similarly, higher success rates and fewer insertion attempts have been observed with ultrasound-guided peripheral intravenous line and arterial line placement.17 Ultrasound- guided PIV placement can reduce referrals for midlines and peripherally inserted central catheters in hospitalized patients.18
In COVID-19 patients, use of ultrasound guidance for vascular access has distinct advantages. First, given the high incidence of DVT in COVID-19 patients,12 POCUS allows preprocedural evaluation of the target vessel for thrombosis, as well as anatomic variations and stenosis. Second, visualizing the needle tip and guidewire within the target vein prior to dilation nearly eliminates the risk of arterial puncture and inadvertent arterial dilation, which is particularly important in COVID-19 patients receiving high-dose prophylactic or therapeutic anti-coagulation. Third, when inserting internal jugular and subclavian CVCs, visualization of normal lung sliding before and after the procedure safely rules out pneumothorax. However, if lung sliding is not seen before the procedure, it cannot be used to rule out pneumothorax afterward. Additionally, visualizing absence of the catheter tip in the right atrium and presence of a rapid atrial swirl sign within 2 seconds of briskly injecting 10 mL of saline confirms catheter tip placement near the superior vena cava/right atrial junction, which can eliminate the need for a postprocedure chest radiograph.17
ENDOTRACHEAL INTUBATION
POCUS can be used to rapidly confirm endotracheal tube (ETT) placement, which can reduce reliance on postintubation chest radiographs. A meta-analysis of prospective and randomized trials showed transtracheal ultrasonography had high sensitivity (98.7%) and specificity (97.1%) for confirming tracheal placement of ETTs.19 Confirming endotracheal intubation involves two steps: First, a linear transducer is placed transversely over the suprasternal notch to visualize the ETT passing through the trachea, and not the esophagus, during insertion. Second, after the ETT cuff has been inflated, bilateral lung sliding should be seen in sync with the respiratory cycle if the ETT is in the trachea. Absent lung sliding, but preserved lung pulse, on the anterior hemithorax is likely caused by main stem bronchial intubation, and withdrawing the ETT until bilateral lung sliding is seen confirms tracheal placement. Additionally, the following steps are recommended to reduce the risk of exposure to healthcare workers: minimizing use of bag-valve-mask ventilation, performing rapid sequence intubation using video laryngoscopy, and connecting the ETT to the ventilator immediately.
ULTRASOUND DEVICES AND DISINFECTION
Important considerations when selecting an ultrasound machine for use in COVID-19 patients include image quality, portability, functionality, and ease of disinfection. Advantages of handheld devices include portability and ease of disinfection, whereas cart-based systems generally have better image quality and functionality. To minimize the risk of cross contamination, an ultrasound machine should be dedicated exclusively for use on patients with confirmed COVID-19 and not shared with patients with suspected COVID-19.20 To minimize exposure to COVID-19 patients, frontline providers should perform POCUS exams only when findings may change management, and timing of the exam and views acquired should be selected deliberately.
Ultrasound machine disinfection should be integrated into routine donning and doffing procedures. When possible, both handheld and cart-based machines should be draped with protective covers during aerosol-generating procedures. Single use ultrasound gel packets are recommended in order to decrease the risk of nosocomial infection.20 After every use of an ultrasound machine on intact skin or for percutaneous procedures, low-level disinfection should be performed with an Environmental Protection Agency–recommended product that is effective against coronavirus.
Some ultrasound manufacturers have added teleultrasound software that allows remote training of novice POCUS users and remote guidance in actual patient care. Teleultrasound can be utilized to share images in real time with consultants or expert providers.
CONCLUSION
POCUS is uniquely poised to improve patient care during the COVID-19 pandemic. POCUS can be used to support the diagnosis of COVID-19 patients and monitor patients with confirmed disease. Common POCUS applications used in COVID-19 patients include evaluation of the lungs, heart, and deep veins, as well as performance of bedside procedures. Ultrasound machine portability and disinfection are important considerations in COVID-19 patients.
Footnotes
Disclosures: The authors have no potential conflict of interest to disclose.
Funding: Department of Veterans Affairs, Quality Enhancement Research Initiative (QUERI) Partnered Evaluation Initiative Grant (HX002263-01A1) to Dr Soni. The contents of this publication do not represent the views of the US Department of Veterans Affairs or the United States government.
References
- 1.Wu Z, McGoogan JM. Characteristics of and important lessons from the coronavirus disease 2019 (COVID-19) outbreak in China: summary of a report of 72 314 cases from the Chinese Center for Disease Control and Prevention. JAMA. 2020;323(13):1239–1242. doi: 10.1001/jama.2020.2648. doi: 10.1001/jama.2020.2648. [DOI] [PubMed] [Google Scholar]
- 2.Ai T, Yang Z, Hou H, et al. Correlation of chest CT and RT-PCR testing in coronavirus disease 2019 (COVID-19) in China: a report of 1014 cases. Radiology. 2020:200642. doi: 10.1148/radiol.2020200642. doi: 10.1148/radiol.2020200642. [DOI] [PMC free article] [PubMed]
- 3.American College of Radiology ACR Recommendations for the use of Chest Radiography and Computed Tomography (CT) for Suspected COVID-19. [Accessed April 10 2020];Infection March. 2020 11 https://www.acr.org/Advocacy-and-Economics/ACR-Position-Statements/Recommendations-for-Chest-Radiography-and-CT-for-Suspected-COVID19-Infection. [Google Scholar]
- 4.Alzahrani SA, Al-Salamah MA, Al-Madani WH, Elbarbary MA. Systematic review and meta-analysis for the use of ultrasound versus radiology in diagnosing of pneumonia. Crit Ultrasound J. 2017;9(1):6. doi: 10.1186/s13089-017-0059-y. doi: 10.1186/s13089-017-0059-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Hew M, Corcoran JP, Harriss EK, Rahman NM, Mallett S. The diagnostic accuracy of chest ultrasound for CT-detected radiographic consolidation in hospitalised adults with acute respiratory failure: a systematic review. BMJ Open. 2015;5(5):e007838. doi: 10.1136/bmjopen-2015-007838. doi: 10.1136/bmjopen-2015-007838. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Peng QY, Wang XT, Zhang LN, Chinese Critical Care Ultrasound Study Group Findings of lung ultrasonography of novel corona virus pneumonia during the 2019-2020 epidemic. Intensive Care Med. 2020 doi: 10.1007/s00134-020-05996-6. doi: 10.1007/s00134-020-05996-6. [DOI] [PMC free article] [PubMed]
- 7.Huang Y, Wang S, Liu Y, et al. A preliminary study on the ultrasonic manifestations of peripulmonary lesions of non-critical novel coronavirus pneumonia (COVID-19) Soc Sci Res Netw (SSRN) 2020 doi: 10.2139/ssrn.3544750. [DOI]
- 8.Mojoli F, Bouhemad B, Mongodi S, Lichtenstein D. Lung ultrasound for critically ill patients. Am J Respir Crit Care Med. 2019;199(6):701–714. doi: 10.1164/rccm.201802-0236ci. doi: 10.1164/rccm.201802-0236ci. [DOI] [PubMed] [Google Scholar]
- 9.Ji L, Cao C, Lv Q, Li Y, Xie M. Serial bedside lung ultrasonography in a critically ill COVID-19 patient. Qjm. 2020 doi: 10.1093/qjmed/hcaa141. doi: 10.1093/qjmed/hcaa141. [DOI] [PMC free article] [PubMed]
- 10.Madjid M, Safavi-Naeini P, Solomon SD, Vardeny O. Potential effects of coronaviruses on the cardiovascular system: a review. JAMA Cardiol. 2020 doi: 10.1001/jamacardio.2020.1286. doi: 10.1001/jamacardio.2020.1286. [DOI] [PubMed]
- 11.Guo T, Fan Y, Chen M, et al. Cardiovascular implications of fatal outcomes of patients with coronavirus disease 2019 (COVID-19) JAMA Cardiol. 2020:e201017. doi: 10.1001/jamacardio.2020.1017. [DOI] [PMC free article] [PubMed]
- 12.Klok F, Kruip M, van der Meer N, et al. Incidence of thrombotic complications in critically ill ICU patients with COVID-19. Throm Res. 2020 doi: 10.1016/j.thromres.2020.04.013. [DOI] [PMC free article] [PubMed]
- 13.Johri AM, Galen B, Kirkpatrick J, Lanspa M, Mulvagh S, Thamman R. ASE statement on point-of-care ultrasound (POCUS) during the 2019 novel coronavirus pandemic. J Am Soc Echocardiogr. 2020 doi: 10.1016/j.echo.2020.04.017. doi: 10.1016/j.echo.2020.04.017. [DOI] [PMC free article] [PubMed]
- 14.American Society of Hematology COVID-19 and Pulmonary Embolism: Frequently Asked Questions. [Accessed April 10 2020];2020 Apr 9; https://www.hematology.org/covid-19/covid-19-and-pulmonary-embolism.
- 15.Fischer EA, Kinnear B, Sall D, et al. Hospitalist-Operated Compression Ultrasonography: a Point-of-Care Ultrasound Study (HOCUS-POCUS) J Gen Intern Med. 2019;34(10):2062–2067. doi: 10.1007/s11606-019-05120-5. doi: 10.1007/s11606-019-05120-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Tavazzi G, Civardi L, Caneva L, Mongodi S, Mojoli F. Thrombotic events in SARS-CoV-2 patients: an urgent call for ultrasound screening. Intensive Care Med. 2020:1–3. doi: 10.1007/s00134-020-06040-3. [DOI] [PMC free article] [PubMed]
- 17.Franco-Sadud R, Schnobrich D, Mathews BK, et al. Recommendations on the use of ultrasound guidance for central and peripheral vascular access in adults: a position statement of the Society of Hospital Medicine. J Hosp Med. 2019;14:E1–E22. doi: 10.12788/jhm.3287. doi: 10.12788/jhm.3287. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Galen B, Baron S, Young S, Hall A, Berger-Spivack L, Southern W. Reducing peripherally inserted central catheters and midline catheters by training nurses in ultrasound-guided peripheral intravenous catheter placement. BMJ Qual Saf. 2020;29(3):245–249. doi: 10.1136/bmjqs-2019-009923. doi: 10.1136/bmjqs-2019-009923. [DOI] [PubMed] [Google Scholar]
- 19.Gottlieb M, Holladay D, Peksa GD. Ultrasonography for the confirmation of endotracheal tube intubation: a systematic review and meta-analysis. Ann Emerg Med. 2018;72(6):627–636. doi: 10.1016/j.annemergmed.2018.06.024. doi: 10.1016/j.annemergmed.2018.06.024. [DOI] [PubMed] [Google Scholar]
- 20.Abramowicz J, Basseal J. WFUMB Position Statement: how to perform a safe ultrasound examination and clean equipment in the context of COVID-19. Ultrasound Med Biol. 2020 doi: 10.1016/j.ultrasmedbio.2020.03.033. doi: 10.1016/j.ultrasmedbio.2020.03.033. [DOI] [PMC free article] [PubMed]