Abstract
Objective
The current study reported a case series to illustrate the early computed tomography (CT) findings of coronavirus disease 2019 (COVID-19) in pediatric patients.
Materials and Methods
All pediatric patients who were diagnosed with COVID-19 and who underwent CT scan in Zhongnan Hospital of Wuhan University from January 20, 2020 to February 28, 2020 were included in the current study. Data on clinical and CT features were collected and analyzed.
Results
Four children were included in the current study. All of them were asymptomatic throughout the disease course (ranging from 7 days to 15 days), and none of them showed abnormalities in blood cell counts. Familial cluster was the main transmission pattern. Thin-section CT revealed abnormalities in three patients, and one patient did not present with any abnormal CT findings. Unilateral lung involvement was observed in two patients, and one patient showed bilateral lung involvement. In total, five small lesions were identified, including ground-glass opacity (n = 4) and consolidation (n = 1). All lesions had ill-defined margins with peripheral distribution and predilection of lower lobe.
Conclusion
Small patches of ground-glass opacity with subpleural distribution and unilateral lung involvement were common findings on CT scans of pediatric patients in the early stage of the disease.
Keywords: Coronavirus disease 2019, Pediatric pneumonia, Computed tomography
INTRODUCTION
Coronavirus disease 2019 (COVID-19) is caused by a novel coronavirus initially identified in Wuhan, China, in December 2019 (1). By March 11, 2020, the pathogen had been rapidly spread to 113 countries worldwide (2). COVID-19 has typical manifestations of acute pneumonia and severe complications such as acute respiratory distress syndrome, and its mortality rate was estimated to be approximately 2% (2,3,4). Since it is a highly infectious disease and transmission by asymptomatic patients has been proven (5), early detection and diagnosis are of significant importance in disease control and treatment. Radiological characteristics provide important evidence for the clinical diagnosis of COVID-19. According to previous studies (6,7,8,9,10,11), bilateral and peripheral predominant ground-glass opacity (GGO) or mixed GGO and consolidation with signs such as crazy paving, air bronchogram, and interstitial thickening were common findings in adult patients diagnosed with COVID-19. However, information regarding pediatric clinical and radiological features of COVID-19 is insufficient (12,13,14,15). This study aimed to describe a pediatric case series diagnosed with COVID-19 in detail to illustrate early computed tomography (CT) findings.
MATERIALS AND METHODS
The study was approved by the Institutional Review Board of Zhongnan Hospital of Wuhan University (approval number 2020004). The requirement for written informed consent was waived.
Patients
A total of 1574 patients were diagnosed with COVID-19 by reverse transcription-polymerase chain reaction (RT-PCR) tests in Zhongnan Hospital of Wuhan University from January 20, 2020 to February 28, 2020. Among all confirmed cases, six were pediatric patients, including one infant and five children aged less than 14 years. After excluding one child and one infant with no radiological examination, a total of four children (two boys and two girls; age range, 7–13 years) were included in the current study.
Clinical Information Collection
Data regarding demographics, laboratory findings, treatment, and prognosis were collected from the patients' electronic medical records by two independent researchers. Familial clustering information was collected by direct communication with patients and their families. Disease severity was evaluated according to the 7th edition of the diagnosis and treatment guidelines of COVID-19 pneumonia in China (16).
CT Protocol
CT scan (Discovery, GE Medical Systems, Milwaukee, USA) was performed on patients in the supine position under free breathing with the following parameters: 120 kV and automatic tube current (100–150 mA), 1-mm slice thickness with 1-mm gap, lung window setting with window center at −700 HU and window width at 1500 HU, and mediastinal window setting with window center at 40 HU and window width at 400 HU.
Image Analysis
CT features were evaluated by two experienced radiologists who were blinded to the RT-PCR results. The presence of specific CT signs was recorded including GGO, consolidation, mixed GGO and consolidation, crazy paving pattern, air bronchogram, interstitial thickening, parenchymal band, reticular pattern, and lymphadenopathy. Other signs including cystic changes, bronchiolectasis, tree-in-bud, halo sign, calcification, and pleural effusion were also evaluated. Lesion distribution was categorized as peripheral (outer 1/3 of the lung), central (inner 2/3 of the lung), or both. Lesion size was recorded as small (diameter < 1 cm), moderate (1 cm ≤ diameter ≤ 3 cm), or large (diameter > 3 cm). Infected lobes and bilateral or unilateral lung involvement were also recorded.
RESULTS
Clinical Characteristics
The four children were diagnosed with COVID-19 after close contact with infected family members. They were asymptomatic throughout the disease course (range, 7–15 days). Their blood cell counts and procalcitonin and C-reactive protein levels remained within the normal limits. Coinfection was not observed. A significant increase in alanine aminotransferase and aspartate aminotransferase levels was observed in one child without evidence for hepatitis. All reported children were discharged after obtaining at least two consecutive negative RT-PCR test results (three repeats for the two younger children). The time interval from confirmation to first negative RT-PCR result varied from 2 to 12 days (Table 1).
Table 1. Clinical and CT Features.
| Characteristics | Case 1 | Case 2 | Case 3 | Case 4 |
|---|---|---|---|---|
| Demographics | ||||
| Age (years) | 7 | 7 | 12 | 13 |
| Sex | Male | Female | Female | Male |
| Symptoms at onset | None | None | None | None |
| Symptoms during whole disease course | None | None | None | None |
| Epidemiologic history | ||||
| Family members infected | 3 | 3 | 1 | 1 |
| Severity of disease on admission | Mild | Mild | Mild | Mild |
| Laboratory findings | ||||
| White blood cell count (× 109/L) | 6.86 | 4.79 | 6.52 | 4.60 |
| Neutrophil count (× 109/L) | 1.47 | 2.23 | 3.48 | 2.28 |
| Lymphocyte count (× 109/L) | 4.66 | 2.18 | 2.33 | 1.85 |
| Alanine aminotransferase (U/L) | 16 | 520 | 15 | 39 |
| Aspartate aminotransferase (U/L) | 24 | 439 | 16 | 27 |
| Procalcitonin (mg/L) | < 0.05 | < 0.05 | < 0.05 | < 0.05 |
| C-reactive protein (mg/L) | 0.54 | 0.54 | 1.70 | 1.30 |
| Co-infection | None | None | None | None |
| CT features on admission | ||||
| GGO | None | Presence | Presence | Presence |
| Consolidation | None | Presence | None | None |
| Lesion distribution | None | Peripheral | Peripheral | Peripheral |
| Lesion size | None | Small | Small | Small |
| Infected lobe | None | Lower lobe | Lower lobe | Lower lobe |
| Unilateral or bilateral lung involvement | None | Unilateral | Bilateral | Unilateral |
| Treatment | ||||
| Intensive care unit | No | No | No | No |
| Severe complications | No | No | No | No |
| Medication | Vitamin C | Vitamin C | Arbidol | Arbidol |
| Time from confirmation to first negative RT-PCR result (days) | 2 | 4 | 3 | 12 |
| Time from confirmation to discharge (days) | 13 | 13 | 7 | 15 |
CT = computed tomography, GGO = ground glass opacity, RT-PCR = reverse transcription-polymerase chain reaction
CT Features on Admission
Three of the four pediatric patients showed abnormalities on thin-section CT scans, and the fourth patient had a negative CT scan result. Unilateral lung involvement was observed in two patients, and only one child had bilateral lung infection. In total, five lesions were identified in three patients (Figs. 1, 2, 3). All lesions were small (diameter < 1 cm) with peripheral distribution, and they were located in the lower lobes with predilection of the left lower lobe (n = 4).
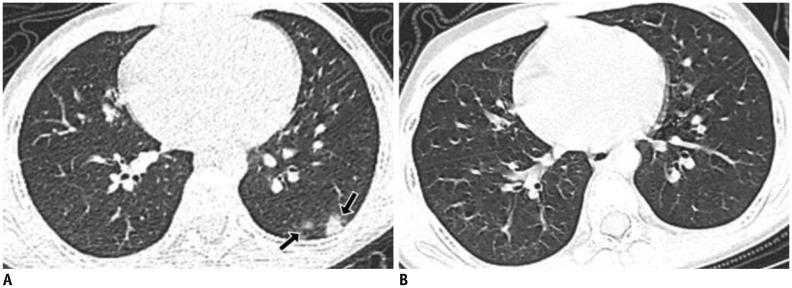
Fig. 1. 7-year-old twin girl diagnosed with COVID-19.
A. CT scan on admission (day 1) showed subpleural ground-glass opacity and consolidation in left lower lobe (arrows). B. On discharge (day 13), acute exudative lesions were substantially resolved after treatment. COVID-19 = coronavirus disease 2019, CT = computed tomography
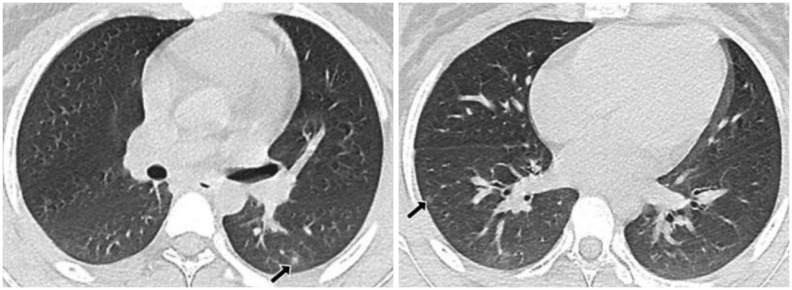
Fig. 2. 12-year-old girl diagnosed with COVID-19.
Small patches of ground-glass opacity were observed on CT scan, with subpleural distribution and bilateral lung involvement (arrows).
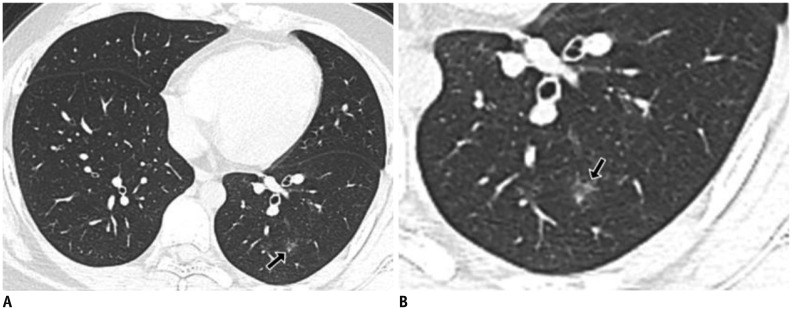
Fig. 3. 13-year-old boy diagnosed with COVID-19.
A. Patch of ground-glass opacity can be observed in left lower lobe (arrow). B. Delicate interstitial thickening was observed in zoom-in image (arrow) without formation of crazy paving pattern.
In a per-lesion analysis, GGO (n = 4) was more common, followed by consolidation (n = 1). Margins of all lesions were ill-defined. The halo sign could be observed surrounding the consolidation (Fig. 1). Of the four GGO lesions, one was mixed GGO or part-solid GGO (Fig. 2), while the other lesions (n = 3) were pure GGO. Delicate interstitial thickening was observed in one pure GGO lesion (Fig. 3). Crazy paving pattern or air bronchogram sign was not observed. Signs including cystic changes, bronchiolectasis, reticular pattern, tree-in-bud, calcification, lymphadenopathy, and pleural effusion were not observed.
CT Changes in Follow-Up Imaging
Regarding disease treatment, vitamin C was administered to the two younger patients, while arbidol was administered to the other two older patients. The follow-up CT imaging after treatment revealed that all the pulmonary exudative lesions were substantially resolved.
DISCUSSION
A low percentage (0.4%, 6 of the 1574 patients) of pediatric patients aged less than 14 years was diagnosed with COVID-19 in our center, which was consistent with the results previously reported by Guan et al. (17) (0.9%). According to previous studies (12,13,14,15,17), most pediatric cases of COVID-19 were mild and showed symptoms similar to those of adult cases. The reported four patients were subclinical cases and had good prognoses after a disease course ranging from 7 to 15 days. Notably, for Patient 4 with one lesion on CT images and no new lesion arising during treatment, a significantly longer time interval was observed from confirmation to first negative RT-PCR (12 days) compared with the other three patients. This suggested that the duration of viral shedding might not be associated with disease severity evaluated with CT scan.
Regarding laboratory findings, lymphopenia or leucopenia was not observed, although they were common findings in most adult patients diagnosed with COVID-19 (3,17). A remarkable increase in procalcitonin levels and a significant proportion of coinfection were observed among pediatric patients according to Xia et al.'s study (13), and this finding was not observed in the current four patients. One child had hepatic dysfunction upon admission and recovered quickly after treatment. After ruling out hepatitis, it was considered possible that the hepatic damage was caused by COVID-19, which had been previously reported in adult patients (18).
Considering that RT-PCR test was time consuming and showed high false-negative rate in China (19), radiological findings were considered important in infection detection and disease control. Although chest radiography is a regular examination, it was not recommended for COVID-19 due to its low sensitivity and nonspecific manifestation, which had been reported in several studies (10,15). As most pediatric patients were mild or moderate cases of COVID-19, the rate of misdiagnosis by radiography might be higher for children than for adults, leading to delayed isolation and treatment for at least a proportion of pediatric patients with initial false-negative RT-PCR results. Compared to radiography, thin-section CT was more sensitive to subtle changes in early infection and was recommended by the guidelines for imaging diagnosis of COVID-19 in China (20).
In adult patients, bilateral lung involvement was frequently observed in most patients; peripherally located GGO or mixed GGO and consolidation in CT images were typical findings, with or without crazy paving, interstitial thickening, or air bronchogram signs (7,9,10,11). These manifestations were similar but milder in pediatric patients. In the current study, unilateral involvement was observed in two of the four patients. Predilection of peripheral or subpleural distribution could be observed, and the lower lobes were more likely to be infected, which was observed in a previous study (12) and in adult patients (19). A majority of patients in this study showed small patches of GGO with ill-defined borders, and consolidation surrounded by the halo sign was not as common as had been reported previously (4). One possible explanation is that consolidation tends to develop in the progressive stage (7,21). CT signs such as crazy paving, interstitial thickening, and air bronchogram were infrequently observed due to the relatively smaller lesions in children (diameter < 1 cm). Reticular pattern, parenchymal band, pleural changes, lymphadenopathy, and pleural effusion were not observed in the current study.
All four children reported familial cluster transmission, which was consistent with the reported transmission pattern among infants (22). Thus, adult family members with high risk factors of COVID-19 infection should pay special attention when in direct contact with children. Additionally, since some pediatric infections have an asymptomatic or mild manifestation, attention should be paid to potential transmission by such cases as asymptomatic carrier transmission has already been proven (5).
The current study had a small sample size, which is a limitation. Hence, further investigation with a large cohort is required to understand the full disease spectrum among children with COVID-19. Additionally, radiography findings from the four children were not available because CT was the recommended examination for both adult and pediatric COVID-19 patients according to the guidelines for imaging diagnosis of COVID-19 in China (20). However, considering that pediatric COVID-19 tends to be mild and different from adult cases, the recommendation of CT as a routine radiological examination for pediatric patients awaits further evidence to carefully weigh the benefits and risks of CT.
In summary, a pediatric case series of COVID-19 was described. Although similar to adult patients, pediatric patients tended to experience mild manifestations of COVID-19. Regarding CT features, small patches of GGO with subpleural distribution and unilateral lung involvement were common findings in pediatric patients in the early stage of the disease. Consolidation surrounded by the halo sign could also be observed. Margins of lesions were ill-defined. Lower lobes were predominantly infected. All exudative lesions were substantially resolved after treatment, and patients had good prognoses. Additionally, familial cluster was the main transmission pattern of these pediatric infections. Potential asymptomatic carrier transmission by pediatric patients should be further studied.
Footnotes
This study was supported by the National Natural Science Foundation of China (Grants No.81771819), National key research and development plan of China (Grants No. 2017YFC0108803).
Conflicts of Interest: The authors have no potential conflicts of interest to disclose.
References
- 1.Zhu N, Zhang D, Wang W, Li X, Yang B, Song J, et al. A novel coronavirus from patients with pneumonia in China, 2019. N Engl J Med. 2020;382:727–733. doi: 10.1056/NEJMoa2001017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.World Health Organization. Coronavirus disease (COVID-2019) situation report. [Accessed March 12, 2020]. Available at: https://www.who.int/emergencies/diseases/novel-%ADcoronavirus-%AD2019/situation-%ADreports/
- 3.Wang D, Hu B, Hu C, Zhu F, Liu X, Zhang J, et al. Clinical characteristics of 138 hospitalized patients with 2019 novel coronavirus-infected pneumonia in Wuhan, China. JAMA. 2020 Feb 07; doi: 10.1001/jama.2020.1585. [Epub] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Huang C, Wang Y, Li X, Ren L, Zhao J, Hu Y, et al. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet. 2020;395:497–506. doi: 10.1016/S0140-6736(20)30183-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Bai Y, Yao L, Wei T, Tian F, Jin DY, Chen L, et al. Presumed asymptomatic carrier transmission of COVID-19. JAMA. 2020 Feb 21; doi: 10.1001/jama.2020.2565. [Epub] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Song F, Shi N, Shan F, Zhang Z, Shen J, Lu H, et al. Emerging 2019 novel coronavirus (2019-nCoV) pneumonia. Radiology. 2020;295:210–217. doi: 10.1148/radiol.2020200274. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Pan F, Ye T, Sun P, Gui S, Liang B, Li L, et al. Time course of lung changes on chest CT during recovery From 2019 novel coronavirus (COVID-19) pneumonia. Radiology. 2020 Feb 13; doi: 10.1148/radiol.2020200370. [Epub] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Xie X, Zhong Z, Zhao W, Zheng C, Wang F, Liu J. Chest CT for Typical 2019-nCoV pneumonia: relationship to negative RTPCR testing. Radiology. 2020 Feb 12; doi: 10.1148/radiol.2020200343. [Epub] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Bernheim A, Mei X, Huang M, Yang Y, Fayad ZA, Zhang N, et al. Chest CT findings in coronavirus disease-19 (COVID-19): relationship to duration of infection. Radiology. 2020 Feb 20; doi: 10.1148/radiol.2020200463. [Epub] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Yoon SH, Lee KH, Kim JY, Lee YK, Ko H, Kim KH, et al. Chest radiographic and CT findings of the 2019 novel coronavirus disease (COVID-19): analysis of nine patients treated in Korea. Korean J Radiol. 2020;21:494–500. doi: 10.3348/kjr.2020.0132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Wei J, Xu H, Xiong J, Shen Q, Fan B, Ye C, et al. 2019 novel coronavirus (COVID-19) pneumonia: serial computed tomography findings. Korean J Radiol. 2020;21:501–504. doi: 10.3348/kjr.2020.0112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Li W, Cui H, Li K, Fang Y, Li S. Chest computed tomography in children with COVID-19 respiratory infection. Pediatr Radiol. 2020 Mar 11; doi: 10.1007/s00247-020-04656-7. [Epub] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Xia W, Shao J, Guo Y, Peng X, Li Z, Hu D. Clinical and CT features in pediatric patients with COVID-19 infection: Different points from adults. Pediatr Pulmonol. 2020 Mar 05; doi: 10.1002/ppul.24718. [Epub] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Liu W, Zhang Q, Chen J, Xiang R, Song H, Shu S, et al. Detection of covid-19 in children in early January 2020 in Wuhan, China. N Engl J Med. 2020;382:1370–1371. doi: 10.1056/NEJMc2003717. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Xu Y, Li X, Zhu B, Liang H, Fang C, Gong Y, et al. Characteristics of pediatric SARS-CoV-2 infection and potential evidence for persistent fecal viral shedding. Nat Med. 2020 Mar 13; doi: 10.1038/s41591-020-0817-4. [Epub] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.China National Health Commission. Diagnosis and treatment of COVID-19 pneumonia in China (trial version 7) [Accessed March 4, 2020]. Available at: www.nhc.gov.cn/yzygj/s7652m/202003/a31191442e29474b98bfed5579d5af95.shtml.
- 17.Guan WJ, Ni ZY, Hu Y, Liang WH, Ou CQ, He JX, et al. Clinical characteristics of coronavirus disease 2019 in China. N Engl J Med. 2020 Feb 28; doi: 10.1056/NEJMoa2002032. [Epub] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Chen N, Zhou M, Dong X, Qu J, Gong F, Han Y, et al. Epidemiological and clinical characteristics of 99 cases of 2019 novel coronavirus pneumonia in Wuhan, China: a descriptive study. Lancet. 2020;395:507–513. doi: 10.1016/S0140-6736(20)30211-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Ai T, Yang Z, Hou H, Zhan C, Chen C, Lv W, et al. Correlation of chest CT and RT-PCR testing in coronavirus disease 2019 (COVID-19) in China: a report of 1014 cases. Radiology. 2020 Feb 26; doi: 10.1148/radiol.2020200642. [Epub] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.H Li, H Xu. Guidelines for imaging diagnosis of COVID-19 in China (2020, version 1) YI XUE XIN ZHI. 2020;30:22–34. [Google Scholar]
- 21.Shi H, Han X, Jiang N, Cao Y, Alwalid O, Gu J, et al. Radiological findings from 81 patients with COVID-19 pneumonia in Wuhan, China: a descriptive study. Lancet Infect Dis. 2020;20:425–434. doi: 10.1016/S1473-3099(20)30086-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Wei M, Yuan J, Liu Y, Fu T, Yu X, Zhang ZJ. Novel coronavirus infection in hospitalized infants under 1 year of age in China. JAMA. 2020 Feb 14; doi: 10.1001/jama.2020.2131. [Epub] [DOI] [PMC free article] [PubMed] [Google Scholar]