Abstract
Coronavirus disease 2019 (COVID-19) is a new infectious disease rapidly spreading around the world, raising global public health concerns. Radiological examinations play a crucial role in the early diagnosis and follow-up of COVID-19. Cross infection among patients and radiographers can occur in radiology departments due to the close and frequent contact of radiographers with confirmed or potentially infected patients in a relatively confined room during radiological workflow. This article outlines our experience in the emergency management procedure and infection control of the radiology department during the COVID-19 outbreak.
Keywords: COVID-19, Infection control, Radiology department, Radiographer
INTRODUCTION
In December 2019, coronavirus disease 2019 (COVID-19), a novel infectious disease, emerged in Wuhan, China (1,2,3). It rapidly spread across China and other countries in the following four months, raising global public health concerns (4,5). As of April 12th, 2020, the World Health Organization reported a total of 1696588 confirmed cases and 105952 deaths around the world (6). In a recent report from the Chinese Center for Disease Control and Prevention (Chinese CDC), more than 3000 health-care workers have been infected with COVID-19 (7). Radiology is the first-line service for COVID-19 patients, and radiographers are often directly exposed to confirmed patients in a relatively confined room during radiological examination (8,9,10). Thus, radiology departments face two great challenges while carrying out routine examinations; one is to control patient-to-patient cross infection, and the other is to protect our staff from infection.
Reverse transcription-polymerase chain reaction (RT-PCR) is regarded as the reference standard for diagnosing COVID-19 (11). However, several studies have reported that the sensitivity of initial RT-PCR tests were as low as 60–71%, which could be related to sampling errors, low virus load, or other factors (12,13). Furthermore, during the early stages of the outbreak, RT-PCR results must be confirmed by the Chinese CDC to make the final diagnosis in China (14). Thus, prompt diagnosis and early isolation were rather difficult. Radiological examinations could play a vital role in the control of COVID-19 through prompt diagnosis, monitoring disease progression, and guiding clinical decisions (15,16,17,18). Portable chest radiography is used as a first-line triage tool in Italy and the United Kingdom due to the reduced risk of cross infection and the ease of disinfection (19,20). However, several studies have reported that the sensitivity of chest radiography in detecting COVID-19 is as low as 56–69% (21,22). Chest computed tomography (CT) is fast and identify COVID-19 early with high sensitivity of 97–98% (12,13,23). Thus, in the early stage of the outbreak, chest CT was considered as a major modality for detecting COVID-19 in China. Considering the importance of CT in fighting against COVID-19 from the perspective of Wuhan, the epicenter in China, dedicated CT scanners were employed in the fever clinics of nearly all hospitals (15,24,25). Over the past two months, we have examined thousands of suspected cases of COVID-19 in the fever clinic and have successfully run with an infection rate of zero for our medical staff. As the COVID-19 epidemic is now widespread in the rest of the world outside China, an increasing number of radiologists are acting against the emerging infectious disease. Thus, we have timely summarized our experience in the management and infection control by the radiology department to help radiologists globally to minimize cross infection of COVID-19 among healthcare workers and patients. In addition, we have discussed the setup and workflow of our dedicated CT rooms for COVID-19 in our department.
Hospital Management of COVID-19
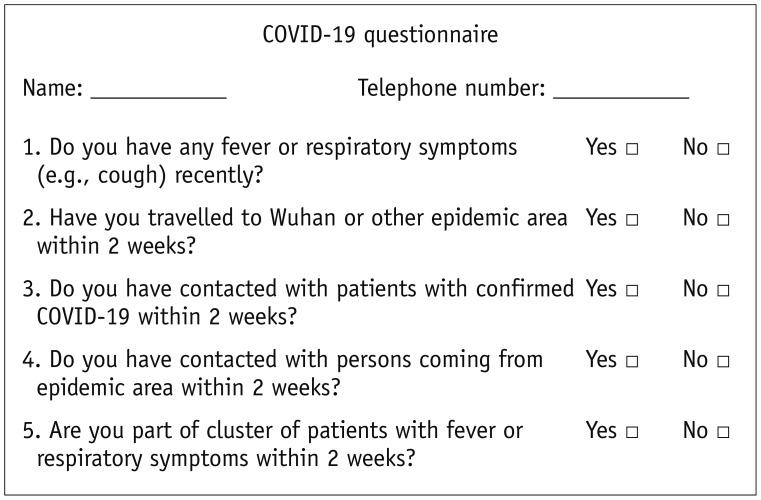
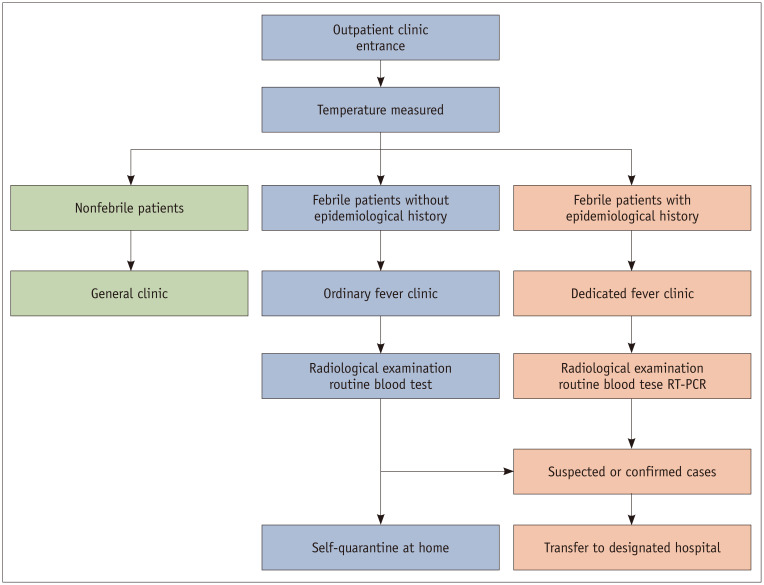
In response to the COVID-19 outbreak, more than 150000 hospitals in China established dedicated fever clinics, in both COVID-19-designated and non-designated hospitals. Enhanced management and infection control measures were enforced in each hospital to prevent nosocomial transmission of COVID-19. During the COVID-19 outbreak, an outdoor clinic in our hospital was set up outside the main outpatient building for the screening of incoming patients and any accompanying persons. All medical staff attended work through a designated passage. Everyone was required to wear masks with no breathing valve before entering the hospital. An infrared temperature detector was used to measure temperatures, which could be displayed on the computer screen instantly. A detailed questionnaire was also conducted by triage nurses (Fig. 1). The definition of the epidemic area in our hospital often changed and followed the Diagnosis and Treatment Program of 2019 New Coronavirus Pneumonia released by the Chinese Health Commission. Given that the seasonal influenza was still widely spread in the community, referral of all fever patients to the COVID-19 fever clinic could increase potential patient-to-patient cross infection. Our hospital divided patients with fever or respiratory symptoms into two groups. Fever patients with an epidemiological history were asked to consult to the COVID-19 fever clinic, while those without an epidemiological history were treated using the routine workflow in the ordinary fever clinic (Fig. 2). All fever patients were required to undergo radiological examinations and routine blood tests to help diagnosis COVID-19. Considering that results of an initial RT-PCR may be false-negative, patients with typical radiological manifestations were categorized as suspected cases. If the diagnosis of suspected or confirmed cases were made, patients were immediately transferred to designated hospitals for further management.
Fig. 1. Questionnaire on fever, travel, contact, and clustering.
COVID-19 = coronavirus disease 2019
Fig. 2. Flowchart of outpatient triage in our hospital.
Fever patients were asked to visit ordinary fever clinic or dedicated fever clinic according to epidemiological history. Patients were also required to undergo radiological examinations and routine blood tests. All suspected or confirmed cases were transferred to designated hospitals for further management. RT-PCR = reverse transcription-polymerase chain reaction
Emergency Management and Infection Control in the Radiology Department
Establish an Infection Control Team
During the early stages of the outbreak, we quickly set up an infection control team to ensure the department ran normally and efficiently. The infection control team members included the chief of radiology department, radiographer-in-charge, nurse-in-charge, and chief resident. The responsibility of each member was identified, as shown in Table 1. The team frequently reviewed the practices in our department and the CT rooms of the fever clinic to help reinforce infection control measures.
Table 1. Responsibilities of Infection Control Team Members.
| Team Member | Responsibility |
|---|---|
| Chief | Take overall responsibility for infection control team; coordinate with hospital infection control team |
| Deputy chief | Draft emergency management plan including urgency events such as infection of staff members |
| Radiographerin- charge | Reorganize working areas and radiological equipment; draft work schedule for radiographers |
| Nurse-in-charge | Staff education, training, and supervision |
| Chief resident | Disseminate up to date information of COVID-19; receive and distribute protective equipment |
COVID-19 = coronavirus disease 2019
Reorganize Working Areas
As we aimed to restrict movement to minimize the risk of potential transmission, the entire department was divided into clean areas, potential dirty areas, and dirty areas (26). Each area was marked with red, yellow, and green notice plates at a prominent location (Table 2). Staff who worked in different areas were not allowed to visit each other without reason. This allowed our department to provide an uninterrupted radiology service in the event of any staff being infected.
Table 2. Separation Areas of Radiology Department during COVID-19 Outbreak.
| Location | Clean Areas | Potential Dirty Areas | Dirty Areas |
|---|---|---|---|
| For patients from fever clinic | |||
| Examination room | √ | ||
| Control room | √ | ||
| Passage and waiting area | √ | ||
| For routine patients | |||
| Examination room | √ | ||
| Control room | √ | ||
| Passage and waiting area | √ | ||
| Registration | √ | ||
| Nurse’s station | √ | ||
| For medical staff | |||
| Diagnostic room | √ | ||
| Office | √ | ||
| Resting area | √ | ||
| Passage | √ |
At the start of the outbreak, the shortage of personal protective equipment (PPE) was a big challenge to the hospital and PPE was strictly distributed based on the risk of the working area. Here, PPE is divided into four levels (Table 3) (24). The staff were required to use general protection in clean areas, level 1 protection in potentially dirty areas, and level 2 or level 3 protection in dirty areas (27). Only radiographers who had frequent contact with fever patients used the highest level of PPE.
Table 3. Personal Protection Guidelines Checklist.
| Items | General Protection | Level 1 Protection | Level 2 Protection | Level 3 Protection |
|---|---|---|---|---|
| Working clothes | √ | √ | √ | √ |
| Mask | √ Surgical | √ N95 | √ N95 | √ N95 |
| Round hat | √ | √ | √ | |
| Gloves | √ | √ | √ | |
| Gown | √ | √ | √ | |
| Goggles/face guard | √ | √ | ||
| Shoe covers | √ | √ | ||
| Comprehensive respiratory apparatus | √ |
Reorganize Radiological Equipment
A lesson learnt from severe acute respiratory syndrome (SARS) was that dedicated facilities situated outside the main department should be employed for COVID-19 examination, if possible (28,29,30). This allows the segregation of patients with suspected COVID-19 from other patients, which can reduce the risk of cross infection and facilitate our routine radiology service. At the onset of the outbreak, a portable X-ray machine was designated to examine suspected COVID-19 patients in the fever clinic for several days. However, no positive findings were reported. Immediately after the recommendations from Chinese Healthy Commission and Hubei radiologists that chest thin slice CT could sensitively display the early-stage changes of COVID-19, such as subpleural patchy ground-glass opacity, one separate CT room in our radiotherapy department, near the fever clinic, was expropriated for patients with possible COVID-19. Meanwhile, a dedicated passage and waiting area were also established to minimize contact with other patients and health-care workers during transit. Barriers were placed to separate these areas, while precautions and directional signs were put up to guide patients and transporters to the examination room. For hospitals constrained by the amount or layout of equipment, we believe that the easiest way is to allocate dedicated time for suspected COVID-19 patients (28,29,31). However, this may be rather challenging to implement as the clinical conditions of a patient often determine the examination time.
Reorganize Radiology Staff
When facing the epidemic, many radiology colleagues showed great courage and volunteered to serve the dedicated examination room for COVID-19. Our two senior radiographers with experiences in fighting SARS in fever clinic in 2003 were firstly recalled to be on duty and were dispatched to Wuhan for medical assistance. Six radiographers in our department were divided into two teams with a work schedule allowing one person per shift, an 8-hour shift daily for a week, followed by 1 week of rest. This arrangement could lower their workload and stress both physically and mentally (28,32). The radiographers were required to report their health condition daily. Whenever the radiographers presented any symptoms of infection, such as fever, cough, or sore throat, they were quarantined. Another new team member was then employed. To date, no radiographer has been infected.
At the initial phase of the outbreak, all student radiographers and radiologists were immediately withdrawn from clinical work. Pregnant radiographers were exempted from all duties that possessed any potential risk of COVID-19. As we faced potential manpower shortages during the outbreak, some booked appointments and non-essential services were canceled, where possible. The value of requested examinations for patients was discussed between the referring physician and radiologists. Requests were only to be made only when the radiological results had a substantial impact on patient treatment. This allowed our staff to have sufficient time to undertake infection control procedures and reduce the workload.
Staff Education, Training, and Supervision
Many staff in our department experienced the SARS outbreak in 2003, with the impressive memory that the radiology department became a site of cross infection between patients and staff (33,34). At the start of the COVID-19 outbreak, we motivated every staff member to join the battle against the virus. All staff were included in the education program organized by the hospital and department. The hospital infection control team provided us the infection control training. The training lectures, documents, and videos were provided by Wechat. Personal hygiene was reinforced, especially the hand hygiene procedure, and alcohol-based hand rubs were placed across the department. All radiology staff were required to be proficient in the proper steps of donning and doffing PPE. A regular audit of staff was carried out on careful hand hygiene, correct use of PPE, and strict adherence to isolation precautions. Only the staff with confirmatory tests could go back on duty. Furthermore, staff were encouraged to remind each other to follow the stringent infection control procedures in all clinical areas.
In our department, diagnostic reports from dedicated facilities for COVID-19 test were requested within 30 minutes. Both radiographers and radiologists were familiarized with the typical and atypical imaging manifestations of COVID-19. A senior radiologist was assigned to collect the literature daily, summarize the imaging features of COVID-19, and provide training to other radiologists to improve their professional skills in diagnosing COVID-19 (15). Considering that some asymptomatic patients with later confirmed COVID-19 may undergo examinations in undedicated machines, radiographers were also required to be familiar with atypical imaging features of COVID-19. Whenever suspicious cases were found during CT scanning, radiographers were advised to contact radiologists immediately for further management.
Notably, all the education and training programs were not a single initiative but were continually updated to our staff through all available communication channels, such as a webchat group, to ensure the knowledge of infection control procedures could be fully implemented into daily practice.
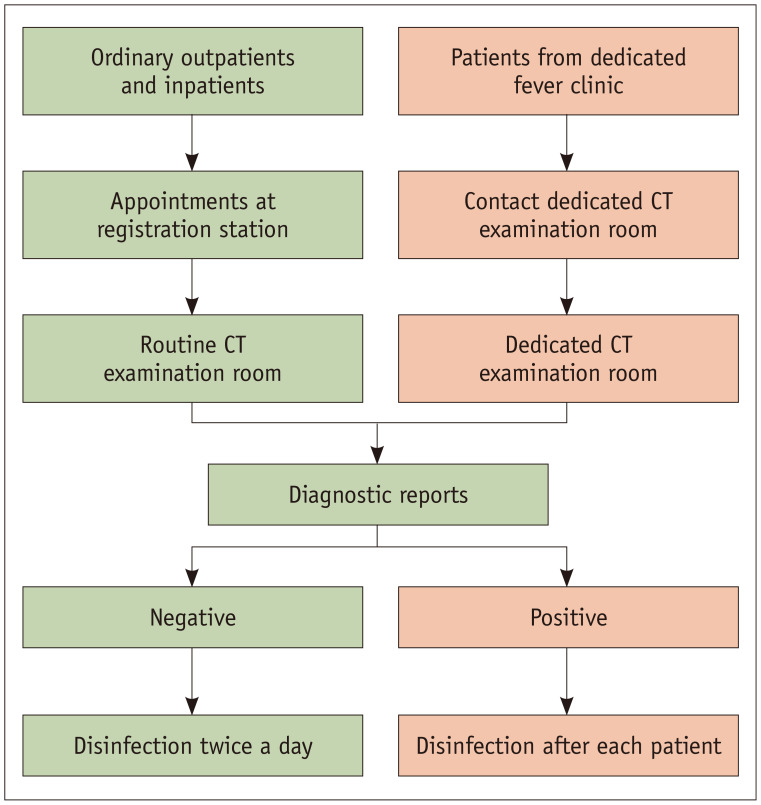
Procedures of Dedicated CT Examination for COVID-19
During the COVID-19 epidemic, we modified many of our daily radiographic practices, ranging from appointments to film distribution and report printing. For COVID-19 dedicated CT, a new workflow was implemented to ensure its validity and efficiency (Fig. 3).
Fig. 3. Workflow of CT examination room in our department.
Non-COVID-19 patients and suspected COVID-19 patients were examined in routine CT rooms or dedicated CT room, respectively. Dedicated CT examination room was disinfected after each patient, while routine CT examination rooms implemented strict disinfection before next patient's examination if COVID-19 was suspected, based on diagnostic reports. CT = computed tomography
Procedure for Allocating Appointments
As our hospital was a non-COVID-19-designated hospital, imaging requests to the dedicated examination room were all from the COVID-19 fever clinic. To facilitate the communication between the COVID-19 fever clinic and the dedicated examination room, examination requests were directly ordered by clinicians to the radiographers by telephone. Radiographers could then prepare prior to patient arrival. Meanwhile, electronic request forms, based on radiology information systems, were utilized to avoid potential transmission by paper request forms. Each request form included information about a patients' clinical symptoms and epidemiological history.
Procedure for Preparing Patients
Patients were instructed to disinfect their hands using hand sanitizer before entering the dedicated CT examination room and to wear a surgical mask throughout the examination. Any high-density objects on the neck and chest were required to be removed. All patients from the COVID-19 fever clinic were escorted by transporters through the dedicated passage. Accompanying persons and transporters were required to stay in the waiting area.
Procedure for Examining Patients
As most patients from the fever clinic could get on and off the examination table themselves, radiographers were advised to stay in the control room during the whole examination procedure. Radiographers could guide patients to place themselves in the correct position, train their respirator, and move the examination table through the control panel. If patients had trouble ambulating, radiographers used level 2 PPE to assist the patient and implement hand hygiene before and after patient contact. When the scanning was complete, patients were instructed to go back to the fever clinic immediately. The images were reconstructed into 1 mm slices and sent to the picture archiving and communication system automatically. Then, radiographers telephoned radiologists to write diagnostic reports which were finished with priority in 30 minutes. Meanwhile, the cleaning staff was called to disinfect the examination room thoroughly. Finally, the diagnostic reports and films were sent to the fever clinic by designated workers when available.
Special Attention for Routine Radiological Services
Some infected patients lacking clinical symptoms or epidemiological history may fail to be allocated to the COVID-19 fever clinic for further examination. Therefore, during routine examinations, radiographers were required to pay extra attention to images for any evidence of COVID-19 mentioned above. If suspicious cases were encountered, staff would directly contact radiologists to rapidly read, write, and sign the report. If the diagnosis of viral pneumonia was considered, radiographers contacted the COVID-19 fever clinic to collect the patient. Then, strict equipment and environment disinfection was performed before next patient's examination.
Disinfection of Equipment and Environment
It has been established that COVID-19 patients with mild upper respiratory tract involvement can cause extensive environmental contamination (35). For all equipment and surroundings in the radiology department, high-level disinfection is mandatory (26,27). We recommend routine disinfection to be implemented by a specially trained worker at least twice a day. All examination rooms for suspected or confirmed COVID-19 patients should be strictly cleaned and disinfected after each patient. The metal equipment can be wiped using 75% alcohol (26). Chlorine-containing disinfectant (2000 mg/L) was used for cleaning the floor, while 500 mg/L chlorine-containing disinfectant was used for exposed surfaces including the handle, wall switch, telephones, and other facilities. Ultraviolet-C light was employed to disinfect air for more than 30 minutes when nobody was present (27,36). The windows of the waiting area and control room were kept open to allow better ventilation. Vacuuming and mechanical buffing of floors were temporarily halted to prevent inadvertent aerosolization of COVID-19.
CONCLUSION
The outbreak of COVID-19 has posed a great challenge and threats to our radiology department. As a non-designated hospital for COVID-19, our hospital undertook the task of the preliminary screening of potentially infected patients. We reorganized our radiologic services and set up dedicated radiological equipment for COVID-19, which minimized the risk of transmission from infected patients. With meticulous planning, strict adherence to infection control approaches, so far, no radiographer has been infected in our department. Of note, the radiology preparedness proposed in this paper is preferentially applicable to non-designated hospitals in China. We hope our experience in infection control management in the radiology department for combating COVID-19 can help radiologists globally better prepare for the uprising epidemic.
Footnotes
This study was supported by The National Key Research and Development Program of China (2017YFC0113400 for L.J.Z.).
Conflicts of Interest: The authors have no potential conflicts of interest to disclose.
References
- 1.Zhu N, Zhang D, Wang W, Li X, Yang B, Song J, et al. China Novel Coronavirus Investigating and Research Team. A novel coronavirus from patients with pneumonia in China, 2019. N Engl J Med. 2020;382:727–733. doi: 10.1056/NEJMoa2001017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Lipsitch M, Swerdlow DL, Finelli L. Defining the epidemiology of Covid-19—Studies needed. N Engl J Med. 2020;382:1194–1196. doi: 10.1056/NEJMp2002125. [DOI] [PubMed] [Google Scholar]
- 3.Chan JF, Yuan S, Kok KH, To KK, Chu H, Yang J, et al. A familial cluster of pneumonia associated with the 2019 novel coronavirus indicating person-to-person transmission: a study of a family cluster. Lancet. 2020;395:514–523. doi: 10.1016/S0140-6736(20)30154-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Rothe C, Schunk M, Sothmann P, Bretzel G, Froeschl G, Wallrauch C, et al. Transmission of 2019-nCoV infection from an asymptomatic contact in Germany. N Engl J Med. 2020;382:970–971. doi: 10.1056/NEJMc2001468. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Heymann DL, Shindo N WHO Scientific and Technical Advisory Group for Infectious Hazards. COVID-19: what is next for public health? Lancet. 2020;395:542–545. doi: 10.1016/S0140-6736(20)30374-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.National authorities. Coronavirus disease 2019 (COVID-19) situation report–83. World Health Organization; 2020. [Accessed April 23, 2020]. Available at: https://www.who.int/docs/default-source/coronaviruse/situation-reports/20200412-sitrep-83-covid-19.pdf?sfvrsn=697ce98d_4. [Google Scholar]
- 7.Novel Coronavirus Pneumonia Emergency Response Epidemiology Team. [The epidemiological characteristics of an outbreak of 2019 novel coronavirus diseases (COVID-19) in China] Zhonghua Liu Xing Bing Xue Za Zhi. 2020;41:145–151. [Google Scholar]
- 8.Kooraki S, Hosseiny M, Myers L, Gholamrezanezhad A. Coronavirus (COVID-19) outbreak: what the department of radiology should know. J Am Coll Radiol. 2020;17:447–451. doi: 10.1016/j.jacr.2020.02.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Kim H. Outbreak of novel coronavirus (COVID-19): what is the role of radiologists? Eur Radiol. 2020 Feb 18; doi: 10.1007/s00330-020-06748-2. [Epub] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Ilyas F, Burbridge B, Babyn P. Health Care-Associated Infections and the radiology department. J Med Imaging Radiat Sci. 2019;50:596–606.e1. doi: 10.1016/j.jmir.2019.07.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Notice on the issuance of a programme for the diagnosis and treatment of novel coronavirus (2019-nCoV) infected pneumonia (trial seventh edition). Office of State Administration of Traditional Chinese Medicine Web site. [Accessed March 4, 2020]. http://bgs.satcm.gov.cn/zhengcewenjian/2020-03-04/13594.html. Published March 3, 2020.
- 12.Fang Y, Zhang H, Xie J, Lin M, Ying L, Pang P, et al. Sensitivity of chest CT for COVID-19: comparison to RT-PCR. Radiology. 2020 Feb 19; doi: 10.1148/radiol.2020200432. [Epub] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Ai T, Yang Z, Hou H, Zhan C, Chen C, Lv W, et al. Correlation of chest CT and RT-PCR testing in coronavirus disease 2019 (COVID-19) in China: a report of 1014 cases. Radiology. 2020 Feb 26; doi: 10.1148/radiol.2020200642. [Epub] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Yang Y, Lu Q, Liu M, Wang Y, Zhang A, Jalali N, et al. Epidemiological and clinical features of the 2019 novel coronavirus outbreak in China. medRxiv; 2020. [Accessed February 13, 2020]. Available at: [DOI] [Google Scholar]
- 15.Zu ZY, Jiang MD, Xu PP, Chen W, Ni QQ, Lu GM, et al. Coronavirus disease 2019 (COVID-19): a perspective from China. Radiology. 2020 Feb 21; doi: 10.1148/radiol.2020200490. [Epub] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Xie X, Zhong Z, Zhao W, Zheng C, Wang F, Liu J. Chest CT for typical 2019-nCoV pneumonia: relationship to negative RTPCR testing. Radiology. 2020 Feb 12; doi: 10.1148/radiol.2020200343. [Epub] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Li K, Wu J, Wu F, Guo D, Chen L, Fang Z, et al. The clinical and chest CT features associated with severe and critical COVID-19 pneumonia. Invest Radiol. 2020 Feb 29; doi: 10.1097/RLI.0000000000000672. [Epub] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Chung M, Bernheim A, Mei X, Zhang N, Huang M, Zeng X, et al. CT imaging features of 2019 novel coronavirus (2019-nCoV) Radiology. 2020;295:202–207. doi: 10.1148/radiol.2020200230. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Imaging the coronavirus disease COVID-19. healthcare-ineurope. com Web site. [Accessed March 23, 2020]. https://healthcare-in-europe.com/en/news/imaging-the-coronavirus-disease-covid-19.html. Published March 16, 2020.
- 20.Lessons from the frontline of the covid-19 outbreak. thebmj. com Web site. [Accessed March 22, 2020]. https://blogs.bmj.com/bmj/2020/03/20/lessons-from-the-frontline-of-the-covid-19-outbreak/?utm_campaign=shareaholic&utm_medium=twitter&utm_source=socialnetwork. Published March 20, 2020.
- 21.Yoon SH, Lee KH, Kim JY, Lee YK, Ko H, Kim KH, et al. Chest radiographic and CT findings of the 2019 novel coronavirus disease (COVID-19): analysis of nine patients treated in Korea. Korean J Radiol. 2020;21:494–500. doi: 10.3348/kjr.2020.0132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Wong HYF, Lam HYS, Fong AH, Leung ST, Chin TW, Lo CSY, et al. Frequency and distribution of chest radiographic findings in COVID-19 positive patients. Radiology. 2019 Mar 27; doi: 10.1148/radiol.2020201160. [Epub] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Long C, Xu H, Shen Q, Zhang X, Fan B, Wang C, et al. Diagnosis of the coronavirus disease (COVID-19): rRT-PCR or CT? Eur J Radiol. 2020;126:108961. doi: 10.1016/j.ejrad.2020.108961. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Zhang HW, Yu J, Xu HJ, Lei Y, Pu ZH, Dai WC, et al. Corona virus international public health emergencies: implications for radiology management. Acad Radiol. 2020;27:463–467. doi: 10.1016/j.acra.2020.02.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Fan L, Xiao Y, Wang C, Zhang C, Guan Y, Wu Y, et al. [Transformation of workflow facing the COVID-19 in the Department of Radiology.] Chin J Radiol. 2020 Feb 29; doi: 10.3760/cma.j.issn.1005-1201.2020.0013. [Epub] [DOI] [Google Scholar]
- 26.Chinese Society of Imaging Technology. [Infection prevention in radiological examination of novel coronavirus pneumonia: expert recommendation from the Chinese Society of Imaging Technology (First edition)] Chin J Radiol. 2020 Feb 15; doi: 10.3760/cma.j.issn.1005-1201.2020.0009. [Epub] [DOI] [Google Scholar]
- 27.Chinese Thoracic Society, Chinese Society of General Practice, Chinese Association of Chest Physican, Chinese Medical Doctor Association General Practitioners Sub-Association, Chinese Society of Infectious Disease, Chinese Alliance for Respiratory Diseases in Primary Care, et al. [Expert recommendations for the prevention and control of novel coronavirus infections in primary care (First Edition)] Chin J Gen Pract. 2020;19:175–192. [Google Scholar]
- 28.Tsou IY, Goh JS, Kaw GJ, Chee TS. Severe acute respiratory syndrome: management and reconfiguration of a radiology department in an infectious disease situation. Radiology. 2003;229:21–26. doi: 10.1148/radiol.2291030789. [DOI] [PubMed] [Google Scholar]
- 29.King AD, Ching AS, Chan PL, Cheng AY, Wong PK, Ho SS, et al. Severe acute respiratory syndrome: avoiding the spread of infection in a radiology department. AJR Am J Roentgenol. 2003;181:25–27. doi: 10.2214/ajr.181.1.1810025. [DOI] [PubMed] [Google Scholar]
- 30.Gogna A, Tay KH, Tan BS. Severe acute respiratory syndrome: 11 years later--a radiology perspective. AJR Am J Roentgenol. 2014;203:746–748. doi: 10.2214/AJR.14.13062. [DOI] [PubMed] [Google Scholar]
- 31.Nyirenda D, Williams R, Ten Ham-Baloyi W. Infection control recommendations for radiology departments in Malawi. Health SA. 2019;24:1035. doi: 10.4102/hsag.v24i0.1035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Lin YC, Dong SL, Yeh YH, Wu YS, Lan GY, Liu CM, et al. Emergency management and infection control in a radiology department during an outbreak of severe acute respiratory syndrome. Br J Radiol. 2005;78:606–611. doi: 10.1259/bjr/17161223. [DOI] [PubMed] [Google Scholar]
- 33.Yang S, Wu J, Ding C, Cui Y, Zhou Y, Li Y, et al. Epidemiological features of and changes in incidence of infectious diseases in China in the first decade after the SARS outbreak: an observational trend study. Lancet Infect Dis. 2017;17:716–725. doi: 10.1016/S1473-3099(17)30227-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Li L, Cheng S, Gu J. SARS infection among health care workers in Beijing, China. JAMA. 2003;290:2662–2663. doi: 10.1001/jama.290.20.2662. [DOI] [PubMed] [Google Scholar]
- 35.Ong SWX, Tan YK, Chia PY, Lee TH, Ng OT, Wong MSY, et al. Air, surface environmental, and personal protective equipment contamination by severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) from a symptomatic patient. JAMA. 2020 Mar 04; doi: 10.1001/jama.2020.3227. [Epub] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Dexter F, Parra MC, Brown JR, Loftus RW. Perioperative COVID-19 defense: an evidence-based approach for optimization of infection control and operating room management. Anesth Analg. 2020 Mar 26; doi: 10.1213/ANE.0000000000004829. [Epub] [DOI] [PMC free article] [PubMed] [Google Scholar]