Highlights
-
•
Effective reproductive numbers (R t) for COVID-19 are linked to dates of interventions.
-
•
From 3.98 before lockdown, R t declined to below 1 by the second week of February 2020.
-
•
Declines follow “early detection, early report, early quarantine and early treatment”.
-
•
Evaluations of interventions provide lessons for others.
Keywords: Effective reproductive number, Intervention timing, COVID-19, Lockdown
Abstract
Effective reproductive numbers (Rt) were calculated from data on the COVID-19 outbreak in China and linked to dates in 2020 when different interventions were enacted. From a maximum of 3.98 before the lockdown in Wuhan City, the values of Rt declined to below 1 by the second week of February, after the construction of hospitals dedicated to COVID-19 patients. The Rt continued to decline following additional measures in line with the policy of “early detection, early report, early quarantine, and early treatment.” The results provide quantitative evaluations of how intervention measures and their timings succeeded, from which lessons can be learned by other countries dealing with future outbreaks.
On 11 March 2020 the World Health Organization (WHO) classified the COVID-19 outbreak as a “pandemic” when there were more than 118 000 confirmed cases in 114 countries, and 4291 people had died; more than 90% of the cases were in China, Italy, South Korea, and Iran, with 80 793 in mainland China, of whom 62 793 recovered and were discharged (National Health Commission of the People's Republic of China, 2020). Since the Wuhan city lockdown on 23 January, China's prevention and control measures showed considerable progress, and the daily number of newly confirmed cases declined from thousands to 15 on 11 March (Cohen and Normile, 2020, Li et al., 2020). This success led to two questions, which we address: (1) How did China's government effectively control the spread of the epidemic within less than two months? (2) What lessons can other countries learn from the implemented containment and mitigation strategies? To do this, we linked the timings of key interventions to rapid declines of the COVID-19 effective reproductive number to quantify lessons from mainland China. We initially estimated the daily number of cases with illness onset (Tang et al., 2020). We then estimated the effective reproduction number (R t) based on the number of daily confirmed cases by using the renewal equation with a mean serial interval of four days (Nishiura and Chowell, 2009, Nishiura et al., 2020).
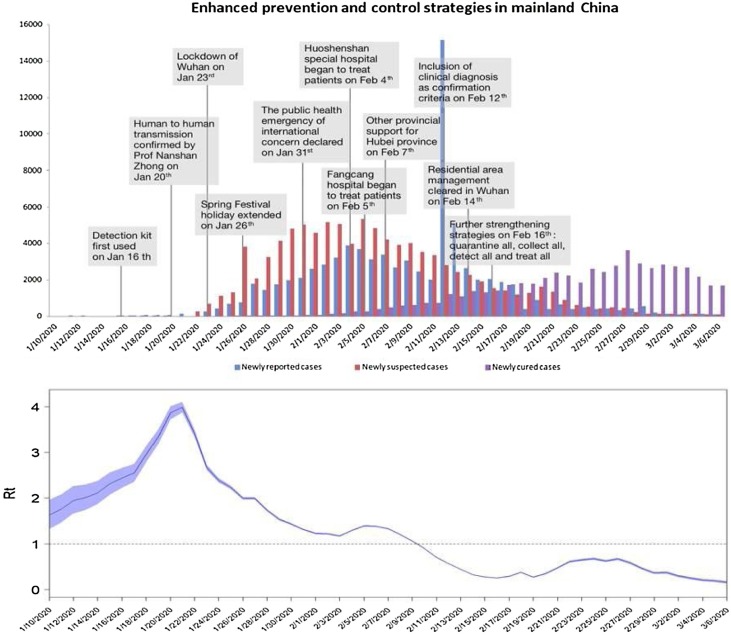
Before 23 January, the traditional Chinese Spring Festival holiday markedly increased crowding and population mobility, leading to an increase in the transmission risk of COVID-19. During this stage, our estimations (Tang et al., 2020) showed that R t increased almost exponentially, reaching a maximum of 3.98 on 21 January before the Wuhan lockdown (Fig. 1 ). Subsequently, a series of comprehensive measures were adopted nationwide, including travel restrictions, contact tracing, quarantine, extending the holiday, and improving the public health response level, after which R t decreased rapidly, and the spread of COVID-19 was curbed. Earlier, the number of confirmed cases quickly increased, but the number of suspected cases remained at a plateau (Fig. 1), which implied that contact tracing and quarantine measures were being strengthened, and the detection rate was increasing; thus, R t continued to decline. On 31 January, WHO identified the COVID-19 outbreak as a public health emergency, prompting the Chinese government to reinforce containment and mitigation strategies.
Fig. 1.
Time series of the number of newly reported cases, newly suspected cases and newly cured cases with times of implementation of enhanced containment and mitigation interventions (upper panel), and the estimated effective reproductive number Rt, with blue shading showing 95% confidence interval (lower panel).
More and more (suspected) patients needed to be treated with the evolution of the pandemic, but R t remained almost stable, apart from a minor peak around 5 February. However, the rapidly built Huoshenshan hospital and the innovative Fangcang (shelter) hospital started treating patients on 4 and 5 February, respectively, as medical teams from 16 provinces rushed to Hubei province. Strict implementation of prevention and control strategies and high compliance of individual self-isolation in other provinces quickly caused R t to decrease to below 1 after 9 February. New infections then decreased, so the comprehensive prevention and control measures had achieved initial success.
The Chinese government continued to foster publicity and education, people's awareness of self-isolation grew, and the resumption of work and opening of schools has been gradual, all of which effectively reduced the risk of a second outbreak. To consolidate this declining trend, public health sectors continued implementing the policy of “early detection, early report, early quarantine, and early treatment.” In particular, on 12 February, Hubei province started to include clinically diagnosed cases in the category of confirmed cases to enhance its quarantine/isolation measures. On 14 February, Wuhan refined its management protocol for residential quarters and, on 16 February, the National Health Commission of the People's Republic of China revised its New Coronavirus Pneumonia Prevention and Control Plan to further clarify and enhance the public health interventions as much as possible in four key areas: Quarantine high-risk individuals; Test suspected individuals; Treat patients and Receive and cure all patients. Consequently, these strategies effectively cut off transmission, kept the epidemic at a low level, and steadily increased the number of cured individuals (Fig. 1).
Analyses by fitting our model with multiple data sets (Tang et al., 2020), revealed that the epidemic situation in mainland China depends mainly on the cumulative number of quarantined and suspected cases (as of 24:00 on 11 March, 677 243 persons had been tracked and quarantined, with 97 141 suspected cases). The detection rate of suspected cases is a critical factor affecting the epidemic, the eventual development of which will depend on the coordinated implementation of prevention and control strategies and strengthening of community and individual self-isolation measures. These have been key to the rapid mitigation of COVID-19 in mainland China. Note that the COVID-19 infections in Hubei Province largely represented the situation for the whole country (Tang et al., 2020); the rest of China exhibited less severe infection rates, due to adequate medical resources and intense interventions, and hence we did not stratify our analysis into two or more geographic regions.
The Chinese success in practice, based on increasingly intensified containment and mitigation strategies, provides an example from which other countries that are experiencing epidemics would do well to learn and heed (Legido-Quigley et al., 2020).
Ethical approval
None.
Authors’ contributions
Y.X., S.T., and J.W. conceived and designed the study. B.T. analyzed the data, carried out the analysis, and performed numerical simulations. Y.X., S.T., J.W., and RAC wrote the paper. All authors have read and agreed to the published version of the manuscript.
Conflict of interest statement
None of the authors have conflict of interest (financial or personal) to report.
Acknowledgments
This research was funded by the National Natural Science Foundation of China (grant numbers: 11631012 (YX, ST), 61772017 (ST)), and by the Canada Research Chair Program (grant number: 230720 (JW)) and the Natural Sciences and Engineering Research Council of Canada (grant number: 105588-2011 (JW)). Many thanks to Fan Xia and Peiyu Liu for preparing Fig. 1.
References
- Cohen J., Normile D. New SARS-like virus in China triggers alarm. Science. 2020;367:234–235. doi: 10.1126/science.367.6475.234. [DOI] [PubMed] [Google Scholar]
- Legido-Quigley H., Asgari N., Teo Y., Leung G.M., Oshitani H., Fukuda K. Are high-performing health systems resilient against the COVID-19 epidemic? Lancet. 2020 doi: 10.1016/S0140-6736(20)30551-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li Q., Guan X., Wu P., Wang X., Zhou L., Tong Y. Early transmission dynamics in Wuhan, China, of novel coronavirus-infected pneumonia. N Engl J Med. 2020 doi: 10.1056/NEJMoa2001316. [DOI] [PMC free article] [PubMed] [Google Scholar]
- National Health Commission of the People's Republic of China. http://www.nhc.gov.cn/xcs/yqtb/202003/37c1536b6655473f8c2120ebdc475731.shtml [accessed 11.03.20] [DOI] [PMC free article] [PubMed]
- Nishiura H., Chowell G. Mathematical and statistical estimation approaches in epidemiology. Springer; Dordrecht: 2009. The effective reproduction number as a prelude to statistical estimation of time-dependent epidemic trends; pp. 103–121. [Google Scholar]
- Nishiura H., Linton N.M., Akmetzhanov A. Serial interval of novel coronavirus (COVID-19) infections. Int J Inf Dis. 2020;93:284–286. doi: 10.1016/j.ijid.2020.02.060. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tang B., Xia F., Tang S., Bragazzi N.L., Li Q., Sun X. The effectiveness of quarantine and isolation determine the trend of the COVID-19 epidemics in the final phase of the current outbreak in China. Int J Inf Dis. 2020;95:288–293. doi: 10.1016/j.ijid.2020.03.018. [DOI] [PMC free article] [PubMed] [Google Scholar]