Abstract
Background: Incidental findings are a well-known complication of imaging studies done for both diagnostic and research purposes. Little is known about the rates and types of incidental findings found on brain MRI in patients with HIV infection, who may be at risk for HIV-Associated Neurocognitive Disorders (HAND). Methods: The parent study included 108 adults with HIV infection and 125 demographically-matched uninfected controls who completed MRI and neuropsychological testing. Incidental findings were classified by the study team as vascular, neoplastic, congenital, other neurologic, or non-neurologic. Categorical measures were compared using Pearson chi-square tests; continuous measures were compared using t-tests. Results: Among participants with HIV infection, 36/108 (33%) had incidental findings compared to 33/125 (26%) controls (p = 0.248). Rates of incidental findings were significantly correlated with increasing age in both participants with HIV infection (p = 0.013) and controls (p = 0.022). We found no correlation between presence of incidental findings and sex or race/ethnicity among either cohort, and no correlation with CD4 count or HAND status for the HIV-infected cohort. Conclusions: Incidental findings were common in both participants with HIV infection and controls, at higher rates than previously reported in healthy populations. There was no significant difference in prevalence between the groups.
Subject terms: HIV infections, Diseases of the nervous system, Magnetic resonance imaging
Introduction
MRI of the brain is increasingly used both for scientific research and as a diagnostic tool to guide clinical medicine. In recent years, new generations of MRI machines have become available to investigators and clinicians providing the ability to achieve higher resolution and greater imaging power. Because of this increase in imaging ability, investigators are better able to detect changes in neuroanatomy and function. With this tendency towards higher processing power, however, has come increasing incidence of incidental findings, both in imaging studies performed for research purposes and for clinical care1–3. Incidental findings are defined as “a finding concerning an individual research participant that has potential health or reproductive importance and is discovered during conducting research but is beyond the aims of the study”2. Recent studies have found that incidental findings are found on up to 48% of structural MRI studies3,4. These incidental findings pose an ethical dilemma, as they often require further workup and diagnostic evaluation, resulting in increased patient anxiety, and increased cost to healthcare systems. Furthermore, many of the subjects in these studies are volunteers and the images obtained in these studies may not be reviewed by a suitably qualified Diagnostic Radiologist; therefore, incidental findings may go unrecognized or the subjects are lost to follow-up5. Risks of false-positive findings and the burden of medical follow-up are an ongoing source of discussion in effort to find the best practice for managing such findings6.
Previous studies have investigated and characterized incidental findings in the general population, but few studies have applied these methods to specialized patient populations such as those with HIV infection3,7–9. HIV is known to cause a wide array of functional neurocognitive changes over time, collectively referred to as HIV-Associated Neurocognitive Disorders (HAND). Although severe neurocognitive impairment has become rare over the last decade, HAND remains a prominent area of research as scientists and clinicians attempt to understand the effects of chronic HIV infection on the brain10. To date, there has been only one study that has reported rates of incidental findings on brain MRI in PWH or characterization of those findings3.
An ongoing NIH-funded study (MH103220) of magnetoencephalography (MEG) and MRI Markers of HIV-Associated Neurocognitive Disorders Across the Lifespan was designed to examine the brain basis of HAND and identify markers of disease progression11,12. In this study, we focus on 108 PWH and 125 matched controls who completed neuropsychological testing, MEG, and brain MRI. The investigative team noted a large number of incidental findings during the conduct of the study and conducted the post-hoc analyses reported here. We hypothesized that PWH have higher prevalence of incidental findings on brain MRI, and that this higher prevalence will be correlated inversely with CD4 T-cell counts.
Methods
Study design and participants
The study included 108 adults with HIV-infection and 125 demographically-matched, uninfected controls without cognitive impairment. The controls were matched on age, sex, ethnicity, and handedness. Exclusion criteria for both groups included any active, severe psychiatric illness, drug or alcohol abuse, major neurologic disease or history of significant head trauma. Demographic and medical history data were collected through participant interview and from the medical records. All participants completed neuropsychological tests to assess multiple domains most affected by HIV disease, including: (1) Wide Range Achievement Test (WRAT-4 Reading), (2) Hopkins Verbal Learning Test-Revised, (3) Trailmaking A and B, (4) Grooved Pegboard – dominant and non-dominant, (5) Wechsler Adult Intelligence Scale (WAIS-III) Digit Symbol, (6) WAIS-III Symbol Search, (7) Stroop Interference Task, and (8) Verbal Fluency (letter and category). All participants also completed the self-reported assessment of Activities of Daily Living Scale (ADLS). Composite scores for each domain were computed by calculating demographically-normalized z-scores and taking an average of the z-scores for all tests within that domain. Together with the assessment of activities of daily living, these scores were used to diagnose HAND according to the Frascati guidelines13.
Participants with HIV infection underwent CD4 count and viral load testing, and control participants underwent HIV testing to exclude HIV infection. Urine pregnancy testing was performed, if indicated. All participants then underwent MEG using a 306-sensor Elekta MEG system and MRI on a Philips 3-Tesla MRI scanner. The MRI protocol included a structural MRI T1 scan designed to highlight the gray/white matter boundary, a T2-weighted FLAIR (fluid-attenuated inversion recovery) sequence, followed by a diffusion-weighted sequence, and a resting-state fMRI scan. The protocol did not involve contrast agents or sedation of any kind and earplugs were provided to minimize the loud noise from the scanner. In this study, we focus on the T1-weighted structural images. Briefly, participants underwent high-resolution T1-weighted MRI on a Philips Achieva 3 T X-series scanner using an eight-channel head coil and a 3D fast-field echo sequence (TR: 8.09 ms; TE: 3.7 ms; field of view: 240 mm; slice thickness: 1.0 mm with no gap; in‐plane resolution: 1.0 × 1.0 mm).
Each MRI study was read by the same expert neuroradiologist, who was blind to the participant’s HIV status. Incidental findings were classified by the study team as vascular, neoplastic, congenital, other neurologic, or non-neurologic. The diagnoses were made based on the characteristics of the MRI findings.
Standard protocol approvals, registrations, and patient consents
The Institutional Review Board of the University of Nebraska Medical Center approved this study. Each participant provided written informed consent following a detailed explanation of the study. All participants completed the same protocol.
Statistical analysis
Categorical measures were compared using Pearson chi-square tests or Fisher’s exact tests while continuous measures were compared using t-tests. All analyses were conducted using STATA v14.2 (The StataCorp, LLC, College Station, TX). P values of less than 0.05 were considered significant.
Results
Participants
Participant characteristics are shown in Table 1. The age range was 26–72 years. On average, for the whole cohort, 43% were female and 60% white. There were no significant differences between the groups.
Table 1.
Participant Characteristics.
| Participants with HIV (%). | Participants without HIV (%) | |
|---|---|---|
| Age in years (range) | 26–72 | 23–72 |
| Sex | ||
| Male | 63 (58) | 69 (55) |
| Female | 45 (42) | 56 (45) |
| Race: | ||
| White | 63 (58) | 76 (61) |
| Black | 31 (29) | 34 (27) |
| Other | 14 (13) | 15 (12) |
| Ethnicity | ||
| Non-Hispanic | 99 (92) | 117 (94) |
| Hispanic | 9 (8) | 8 (6) |
Prevalence and types of incidental findings
36/108 (33%) PWH and 33/125 (26%) of control participants exhibited an incidental finding on brain MRI. However, this difference was not statistically significant (p = 0.248). Table 2 describes the 43 incidental findings reported in the PWH cohort and the 43 findings reported among the control arm. Of these, neurologic incidental findings comprised 63% of the findings in the cohort with HIV infection and 44% in the control cohort Vascular findings comprised 10% in the cohort with HIV infection, and 28% in the controls. Neoplastic findings comprised 5% of the findings in both cohorts.. None of these differences were statistically significant between the groups.
Table 2.
Incidental Findings in Participants with HIV and Controls.
| Finding | Participants with HIV Infection (%) | Control Participants (%) |
|---|---|---|
| Number with Incidental Findings (%) | 36/108 (33%) | 33/125 (26%) |
| Neurologic | 27 (62.8) | 19 (44.2) |
| White Matter Loss | 20 (46.5) | 9 (20.9) |
| Empty Sella/Pseudotumor Cerebri | 6 (14) | 8 (18.6) |
| Basal Ganglia Disease | 1 (2.3) | 0 |
| Normal Pressure Hydrocephalus | 0 | 1 (2.3) |
| Chiari Malformation | 0 | 1 (2.3) |
| Vascular | 6 (14) | 12 (27.9) |
| Chronic Small Vessel Ischemic Disease | 5 (11.6) | 10 (23.3) |
| Lacunar Lesion | 1 (2.3) | 1 (2.3) |
| Brainstem Lesion | 0 | 1 (2.3) |
| Neoplastic | 2 (4.6) | 2 (4.6) |
| Meningioma | 1 (2.3) | 0 |
| Colloid Cyst | 1 (2.3) | 0 |
| Pituitary Adenoma | 0 | 1 (2.3) |
| Interventricular Nodule | 0 | 1 (2.3) |
| Non-Neurologic | 8 (18.6) | 10 (23.3) |
| Maxillary Sinus Disease | 6 (14) | 7 (16.3) |
| Ethmoid Sinus Disease | 1 (2.3) | 1 (2.3) |
| C3–4 Disc Protrusion with Mild Cord Compression | 1 (2.3) | 0 |
| Expanded Spinal Cord Canal | 0 | 1 (2.3) |
| Congenitally Short Pedicles in Upper Cervical Spine | 0 | 1 (2.3) |
Note: some participants had more than one finding.
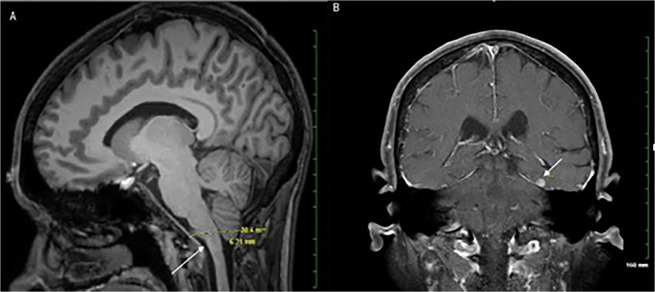
Non-neurologic findings comprised 19% of the findings in the cohort with HIV infection and 23% in the controls. Among PWH, the most common incidental findings were white matter loss (47%), empty sella/pseudotumor cerebri (14%), and maxillary sinus disease (14%). Findings of particular clinical significance were a Type I Chiari Malformation found in one of the control patients and a meningioma found in one of the PWH, as shown in Fig. 1.
Figure 1.
Representative Incidental Findings on Brain MRI. Arrows indicate the abnormalities in each image. Panel (A) shows low lying cerebellar tonsils (type I Chiari malformation) more than 5 mm below the level of the foramen magnum on a T1-weighted sagittal image obtained for diagnostic purposes after the original research image. A meningioma is shown on the T1-weighted coronal image in Panel (B).
Associations between clinical variables and incidental findings in participants with HIV-Infection
Tables 2 and 3 describe how rates of incidental findings were significantly correlated with increased age in both PWH (p = 0.013) and control participants (p = 0.022). The average age of participants with incidental findings was 51.3 years and 49.1 years, versus 45.1 and 42.0 years without incidental findings in the PWH and control cohorts, respectively. There were no significant correlations with sex, or race/ethnicity (Table 4). The average CD4+ count in PWH with incidental findings was 714 cells/cumm, and for those without incidental findings 784 cells/cumm (p = 0.435). We found no correlation among presence or absence of incidental findings and HAND status for the cohort with HIV infection.
Table 3.
Distribution of Findings in Participants with HIV by Age, Sex, Race/Ethnicity, CD4+ Level, and HAND status.
| No Incidental Findings Mean (SD) or n (%) | Incidental Findings Mean (SD) or n (%) | p-value | ||
|---|---|---|---|---|
| Age (in years) | 45.1 (12.4) | 51.3 (11.3) | 0.013 | |
| Sex | ||||
| Male | 43 (60) | 20 (56) | 0.679 | |
| Female | 29 (40) | 16 (44) | ||
| Race and Ethnicity | ||||
| NH White Only | 43 (60) | 20 (56) | 0.734 | |
| NH Black Only | 19 (26) | 12 (33) | ||
| Other | 10 (14) | 4 (11) | ||
| CD4+ (cells/μL) | 784 (429) | 714 (446) | 0.435 | |
| Neurocognitive Disorder* | ||||
| Normal | 48 (67) | 20 (56) | 0.429 | |
| ANI | 12 (17) | 11 (31) | ||
| MND | 7 (10) | 3 (8) | ||
| HAD | 5 (7) | 2 (6) | ||
*ANI = Asymptomatic Neurocognitive Impairment, MND = Mild neurocognitive disorder, HAD = HIV-associated Dementia
Table 4.
Distribution of Findings in Control Participants by Age, Sex, and Race/Ethnicity.
| No Incidental Findings Mean (SD) or n (%) | Incidental Findings Mean (SD) or n (%) | p-value | |
|---|---|---|---|
| Age (in years) | 42.0 (14.2) | 49.1 (16.8) | 0.022 |
| Sex | |||
| Male | 48 (52) | 21 (64) | 0.256 |
| Female | 44 (48) | 12 (36) | |
| Race and Ethnicity | |||
| NH White Only | 60 (65) | 16 (48) | 0.205 |
| NH Black Only | 23 (25) | 11 (33) | |
| Other | 9 (10) | 6 (18) | |
Discussion
We found high prevalence of incidental findings, but surprisingly, no significant difference in rates between the two groups with and without HIV infection. Increasing age was the only factor correlated with more frequent incidental findings. A smaller study comparing patients with HIV infection and demographically matched controls had similar findings, although in this study, the neuroradiologist was not blinded to the participant serostatus which may have led to some bias in reporting3.
In 1999, Katzman et al.8 retrospectively studied the prevalence of incidental imaging findings in a healthy asymptomatic population. This group reported an incidence of 18% incidental findings in their cohort of 1000 research subjects. At the other extreme, more recent studies show that incidental findings appear in 84% of populations with exposures to known neurotoxins14. In this study, we found a rate of 33.3% in the HIV cohort, 27% in the controls. Such a wide range of prevalence has been hypothesized to be due to varying methods, populations, and sample sizes9,15,16. Furthermore, there is evidence that the prevalence of incidental finding detection is more likely using high-resolution MRI sequences17. Certainly, as MRI technology continues to advance and achieve higher sensitivities and images achieve higher resolutions, we will likely continue to see increasing prevalence of incidental findings. For scientists conducting research using neuroimaging, the decision on how to manage disclosure of these findings will continue to pose a complex ethical dilemma18. Despite concerns raised by both clinical and non-clinical researchers, a consensus protocol for the management of incidental findings has not been reached1,19.
Chief among the ethical concerns posed by these findings is the necessity, timing, and context of disclosure to both patients and research participants. Generally, scientific research has followed the fundamental principle of primum non nocere (first, do no harm), as well as general duty to help and rescue16. The prevalence of clinically significant incidental findings among healthy participants is estimated around 2.7% in brain MRI, with a number needed to scan of around 37 for one finding deemed of clinical significance15. This study identified a spectrum of incidental findings ranging from benign sinus disease to brain neoplasms (Table 2), all of which have clinical significance to varying degrees. This further complicates the ethical debate surrounding disclosure, because the definitions of clinical significance are broad, the extent of potential harm by non-disclosure is often unknown, and general duty to help and rescue is often ill-defined and not-standardized. Risks of false-positive findings and the cost burden of further testing and imaging are important considerations.
Potential limitations of this study include the fact that matching did not include other potentially relevant factors such as cardiovascular disease risk factors, medication exposure, socioeconomic status, access to healthcare or lifestyle. Additionally, to maintain coherence with previous literature on incidental findings, abnormalities were classified according to a four-category scheme used in prior studies4,5,14. Thus, our system for classifying incidental findings was limited by the broad scope of the various categories which contained a spectrum of diagnoses that was broad in potential severity. Finally, as this is a post-hoc analysis, we did not plan to collect clinical outcomes of the incidental findings observed.
Although we found high levels of incidental findings in both arms, there was no statistically significant difference between the two groups. Age was the only factor correlated with rates of incidental findings in either PWH or controls. This is consistent with findings that have been previously reported in the general population and in patients with HIV infection4,17. Furthermore, in the cohort with HIV infection, there was no observable difference in the rates of incidental findings based on the presence or absence of HAND or degree of immunosuppression.
This work highlights and reinforces the need for consistent protocols for the handling of incidental findings on MRI scans in functional and structural brain research. The findings of this study will be relevant to future studies reliant upon brain imaging in PWH. Awareness of the high likelihood of incidental findings and knowledge that this risk increases with age can help researchers prepare for unexpected results and ultimately their clinical management during the consent process. Furthermore, research subjects will be more informed and can better prepare themselves for findings that do come up. Clinically, improved awareness of expected frequency and character of these potential findings can help clinicians better inform patients on the risks and benefits of undergoing a brain imaging study, both for research purposes and for clinical care.
Acknowledgements
We thank the participants and all the study staff. This research was supported by grants R01-MH103220, R01-MH116782, R01-MH118013, and P30-MH062261 from the National Institutes of Health. The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
Author contributions
J.O., M.W., T.W. and S.S. contributed to acquisition of data, K.F.H., H.R.S. and S.S. wrote the main manuscript text, K.F.H. prepared the figures. K.F.H., H.R.S., J.O., M.W., T.W. and S.S. reviewed and approved the manuscript.
Data availability
The authors will make data and associated protocols available to readers without undue qualifications in material transfer agreements.
Competing interests
The authors declare no competing interests.
Footnotes
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Illes J, et al. Practical approaches to incidental findings in brain imaging research. Neurology. 2008;70:384–390. doi: 10.1212/01.wnl.0000280469.17461.94. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Gibson LM, et al. Factors associated with potentially serious incidental findings and with serious final diagnoses on multi-modal imaging in the UK Biobank Imaging Study: A prospective cohort study. Plos One. 2019;14:e0218267. doi: 10.1371/journal.pone.0218267. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Chhabra S, et al. Co BRAc: Clinical research cerebral MRI findings in HIV-positive subjects and appropriate controls. AIDS. 2018;32:2077–2081. doi: 10.1097/QAD.0000000000001910. [DOI] [PubMed] [Google Scholar]
- 4.Li S, et al. Incidental findings on brain MRI among Chinese at the age of 55-65 years: the Taizhou Imaging Study. Sci Rep. 2019;9:464. doi: 10.1038/s41598-018-36893-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Kim BS, Illes J, Kaplan RT, Reiss A, Atlas SW. Incidental findings on pediatric MR images of the brain. AJNR Am J Neuroradiol. 2002;23:1674–1677. [PMC free article] [PubMed] [Google Scholar]
- 6.Illes J, et al. Ethics. Incidental findings in brain imaging research. Science. 2006;311:783–784. doi: 10.1126/science.1124665. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.O’Sullivan JW, Muntinga T, Grigg S, Ioannidis JPA. Prevalence and outcomes of incidental imaging findings: umbrella review. BMJ. 2018;361:k2387. doi: 10.1136/bmj.k2387. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Katzman GL, Dagher AP, Patronas NJ. Incidental findings on brain magnetic resonance imaging from 1000 asymptomatic volunteers. JAMA. 1999;282:36–39. doi: 10.1001/jama.282.1.36. [DOI] [PubMed] [Google Scholar]
- 9.Takashima K, et al. Discovery and informing research participants of incidental findings detected in brain magnetic resonance imaging studies: Review and multi-institutional study. Brain Behav. 2017;7:e00676. doi: 10.1002/brb3.676. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Clifford DB, Ances BM. HIV-associated neurocognitive disorder. Lancet Infect Dis. 2013;13:976–986. doi: 10.1016/S1473-3099(13)70269-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Wiesman AI, et al. Aberrant occipital dynamics differentiate HIV-infected patients with and without cognitive impairment. Brain. 2018;141:1678–1690. doi: 10.1093/brain/awy097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Lew BJ, et al. Neural dynamics of selective attention deficits in HIV-associated neurocognitive disorder. Neurology. 2018;91:e1860–e1869. doi: 10.1212/WNL.0000000000006504. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Antinori A, et al. Updated research nosology for HIV-associated neurocognitive disorders. Neurology. 2007;69:1789–1799. doi: 10.1212/01.WNL.0000287431.88658.8b. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Alphs HH, Schwartz BS, Stewart WF, Yousem DM. Findings on brain MRI from research studies of occupational exposure to known neurotoxicants. AJR Am J Roentgenol. 2006;187:1043–1047. doi: 10.2214/AJR.05.0421. [DOI] [PubMed] [Google Scholar]
- 15.Ozdemir M, Kavak RP. Season, Age and Sex-Related Differences in Incidental Magnetic Resonance Imaging Findings of Paranasal Sinuses in Adults. Turk Arch Otorhinolaryngol. 2019;57:61–67. doi: 10.5152/tao.2019.4142. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Keuss SE, et al. Incidental findings on brain imaging and blood tests: results from the first phase of Insight 46, a prospective observational substudy of the 1946 British birth cohort. BMJ Open. 2019;9:e029502. doi: 10.1136/bmjopen-2019-029502. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Morris Z, et al. Incidental findings on brain magnetic resonance imaging: systematic review and meta-analysis. BMJ. 2009;339:b3016. doi: 10.1136/bmj.b3016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Leung L. Incidental Findings in Neuroimaging: Ethical and Medicolegal Considerations. Neurosci J. 2013;2013:439145. doi: 10.1155/2013/439145. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.King ML. A Social Constructivism Decision-Making Approach to Managing Incidental Findings in Neuroimaging Research. Ethics Behav. 2018;28:393–410. doi: 10.1080/10508422.2017.1306445. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The authors will make data and associated protocols available to readers without undue qualifications in material transfer agreements.