Abstract
Background
The coronavirus disease (COVID)-19 pandemic quickly challenged New York City health care systems. Telemedicine has been suggested to manage acute complaints and divert patients from in-person care.
Objectives
The objective of this study was to describe and assess the impact of a rapidly scaled virtual urgent care platform during the COVID-19 pandemic.
Methods
This was a retrospective cohort study of all patients who presented to a virtual urgent care platform over 1 month during the COVID-19 pandemic surge. We described scaling our telemedicine urgent care capacity, described patient clinical characteristics, assessed for emergency department (ED) referrals, and analyzed postvisit surveys.
Results
During the study period, a total of 17,730 patients were seen via virtual urgent care; 454 (2.56%) were referred to an ED. The most frequent diagnoses were COVID-19 related or upper respiratory symptoms. Geospatial analysis indicated a wide catchment area. There were 251 providers onboarded to the platform; at peak, 62 providers supplied 364 h of coverage in 1 day. The average patient satisfaction score was 4.4/5. There were 2668 patients (15.05%) who responded to the postvisit survey; 1236 (49.35%) would have sought care in an ED (11.86%) or in-person urgent care (37.49%).
Conclusions
A virtual urgent care platform was scaled to manage a volume of more than 800 patients a day across a large catchment area during the pandemic surge. About half of the patients would otherwise have presented to an ED or urgent care in person. Virtual urgent care is an option for appropriate patients while minimizing in-person visits during the COVID-19 pandemic.
Keywords: telemedicine, telehealth, urgent care, COVID-19, New York City
Introduction
In late 2019, a novel coronavirus disease (COVID-19), caused by the severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) virus, first emerged in Wuhan, China (1). The COVID-19 pandemic has since rapidly and aggressively spread across the world, and New York City has emerged as a major global epicenter (2). The spread of the virus has challenged health care delivery and hospital-based care (3,4). National shortages in personal protective equipment further strained patient care delivery in emergency departments (EDs) and hospitals (5). EDs in pandemic hotspots experienced high-acuity patient loads and severe boarding as hospitals struggled to manage patient placement and flow (6). Primary care offices also declined to see patients with upper respiratory symptoms in their office spaces for fear of infecting other patients, contributing to unmet patient needs.
To combat virus transmission and slow spread, many states have extensively implemented social distancing and stay-at-home orders. Telehealth and virtual care were promoted as solutions to deliver medical care while allowing for social distancing, and to help decrease patient load on EDs (7, 8, 9). Virtual and telehealth visits have been previously studied and found to be effective for a wide application of medical scenarios, including dermatology visits, wound care, psychiatric care or consultation, and infectious disease practice (10, 11, 12, 13, 14). Telehealth care for urgent and acute visits has also been well described (15, 16, 17, 18).
Our institution has operated a virtual urgent care (VUC) platform since 2017, staffed by emergency physicians to treat nonemergent acute complaints, such as urinary tract infections, dermatologic complaints, or upper respiratory infections. During the COVID-19 pandemic surge in New York City, to provide care to patients seeking urgent care and to avoid in-person visits to busy EDs, the program was rapidly scaled to deliver urgent care services to hundreds of patients daily via a telehealth platform. Patients register for an available time slot on the VUC website, and interact with a provider via an audio-video interface integrated into a patient-facing electronic health record (EHR) application. This study seeks to describe patient presentations to VUC in the setting of the COVID-19 pandemic in New York City; analyze patient demographics, including geography; and consider the effect of a VUC option to decrease ED and in-person care presentations.
Materials and Methods
Study Design
This was a retrospective cohort study of all patients who presented to our VUC over a 1-month period from March 8 to April 7, 2020. For volume trends, we also collected the number of patients seen daily in the 2 weeks prior to the study period. We performed a review of collected survey data on all patients seen by VUC in the study period, and retrospectively reviewed patient records for additional data of interest defined at the study onset.
The study was approved by the Institutional Review Board of the New York University School of Medicine, Office of Science and Research. A waiver of consent and authorization was granted for this study.
Study Setting and Population
New York University Langone Health is a large urban academic health network in the New York City area, with an urban academic tertiary care medical center, an urban community Level I trauma center, a suburban Level I trauma center, and an urban free-standing ED, along with a network of outpatient clinics and urgent care centers. The network typically sees 300,000 annual ED visits and approximately 20,000 annual urgent care visits across these sites. The network's VUC typically sees about 6000 annual visits (on average, 15–20 daily visits) via an online video telehealth platform. The health system uses Epic software (Epic Systems, Verona WI) for EHRs. All child and adult patients presenting to VUC from March 8 to April 7, 2020 were included in the study.
The VUC platform is fully integrated into the Epic EHR platform and is available as a custom augmented Epic MyChart application on mobile devices and computers; the platform permits patients to sign up for a time slot up to 48 h in advance (up to 30 min prior to an open time slot). Patients can be seen from their homes (or anywhere else they might be, so long as they have a mobile device or a computer and internet access). The application instructs the patient to complete a previsit screen for medical history, medications, allergies, pharmacy, and the purpose of the visit. The patient then logs into the application and is “roomed” in the video visit at the appointed time to meet with a provider. Providers use Epic on their computer for health record review and documentation, and conduct the video visit via the Epic mobile applications Canto (iPad; Apple, Cupertino, CA) or Haiku (smartphone; Haiku Inc., New York, NY). Providers can function from a department's on-site office or from a virtual 'remote office'.
Data Collection and Outcomes
EHR data were queried from the Epic Systems Clarity database with the use of Oracle SQL Developer (Oracle Corporation, Redwood City, CA) and exported for data analysis. Retrospectively, we extracted the following variables from the cohort records: patient age, gender, visit time and date, visit diagnosis, ethnicity, address data, insurance status, return visit to VUC within 1 week, International Classification of Diseases, Tenth Revision diagnosis code, and referral to an ED. We also extracted time stamps for when patients entered the video visit, when providers entered the video visit, and when providers left the video visit. In addition, the total number of patients seen each day was collected, and we further captured daily volume for a period of 2 weeks prior to the defined study period for comparison. We also collected from our administrative data the number of active providers seeing patients via VUC during the study period, and the number of new providers onboarded.
A voluntary survey was administered to each patient at the conclusion of their VUC visit. The survey asked a series of questions, including: “Would you have gone to an ED or urgent care center in person today if VUC was not available?” followed by discrete answer choices (ED, urgent care, primary care physician, or nowhere). Patients were also asked, “How satisfied were you with the virtual urgent care medical care?,” “Did your VUC visit meet your needs today?,” “Are you likely to use VUC again?,” and “Are you likely to recommend VUC to others?,” with answers on a 1–5 scale for each question.
Data Analysis
We performed a descriptive analysis of the age, gender, race/ethnicity, and insurance type of patients presenting to the VUC during the study period. We also reported the top 20 diagnoses for these patients and reported results of the patient surveys. We plotted the daily visit volume over the study period, in addition to the 2 weeks prior to the study period for comparison. We also performed geographic analysis of the distribution of the VUC visits by ZIP code. Survey results were collated and the results were analyzed to determine the rate at which patients would have used in-person care options as defined above, and their average satisfaction scores.
We analyzed time stamp data to assess wait times and visit durations. Wait time was defined as the time between scheduled appointment time and the time the provider entered the video visit. Visit duration time was defined as the time elapsed from provider entering the video visit, to when the provider left the video visit. To exclude inaccurate time stamp data caused by occasional technical issues and increase accuracy, duration times > 2 h were excluded from the analysis.
Descriptive statistics and data analysis were performed using Stata V14.2 (StataCorp, College Station, TX). Geographic analysis was performed using ArcGIS Desktop V10.5.1 (ESRI, Redlands, CA).
Results
During the 1-month period included in the study, a total of 17,730 patients were seen via VUC. Patient demographics and characteristics are presented in Table 1 . The most frequent diagnosis during the study period was “advice given regarding COVID-19 virus infection”—5162 visits (29.76%)—followed by cough, upper respiratory infection, “suspected COVID-19 infection,” fever, and viral illness. The 20 most frequent visit diagnoses are provided in Table 2 . Of all patients, 454 (2.56%) were referred for an in-person ED evaluation.
Table 1.
Patient Demographics and Characteristics in Virtual Urgent Care During the Study Period
| Number of Patients | % | |
|---|---|---|
| Gender | ||
| Male | 6774 | 38.2 |
| Female | 10,952 | 61.8 |
| Other/unspecified | 4 | 0.02 |
| Age, years | ||
| ≤ 19 | 301 | 1.7 |
| 20–29 | 2661 | 15.0 |
| 30–39 | 5350 | 30.2 |
| 40–49 | 3952 | 22.3 |
| 50–59 | 2969 | 16.8 |
| 60–69 | 1776 | 10.0 |
| 70–79 | 553 | 3.1 |
| ≥ 80 | 168 | 0.9 |
| Race/ethnicity | ||
| Asian | 1312 | 7.4 |
| Black | 2056 | 11.6 |
| Hispanic/Other | 5664 | 31.9 |
| White | 8698 | 49.0 |
| Insurance/payor | ||
| Private | 11,879 | 67.0 |
| Medicaid/Medicare/Managed Care | 4610 | 26.0 |
| Self-pay | 1241 | 6.9 |
Table 2.
The Twenty Most Common Diagnoses Amongst Patients Seen in Virtual Urgent Care During the Study Period
| Diagnosis | Number of Patients (%) |
|---|---|
| Advice give regarding COVID-19 infection | 5162 (29.76) |
| Cough | 1753 (10.11) |
| Upper respiratory infection | 1582 (9.12) |
| Suspected COVID-19 infection | 1347 (7.77) |
| Fever | 1080 (6.23) |
| Viral illness | 641 (3.7) |
| Sore throat/pharyngitis | 636 (3.67) |
| Sinusitis | 393 (2.27) |
| Exposure to COVID-19 | 378 (2.18) |
| Dyspnea | 190 (1.1) |
| Chest pain | 189 (1.09) |
| Asthma | 168 (0.97) |
| Diarrhea | 165 (0.95) |
| COVID-19 viral infection | 161 (0.93) |
| Abdominal pain | 156 (0.9) |
| Low back pain | 137 (0.79) |
| Urinary tract infection | 136 (0.78) |
| Rash | 132 (0.76) |
| Anxiety | 110 (0.63) |
| Headache | 104 (0.6) |
COVID-19 = coronavirus disease-19.
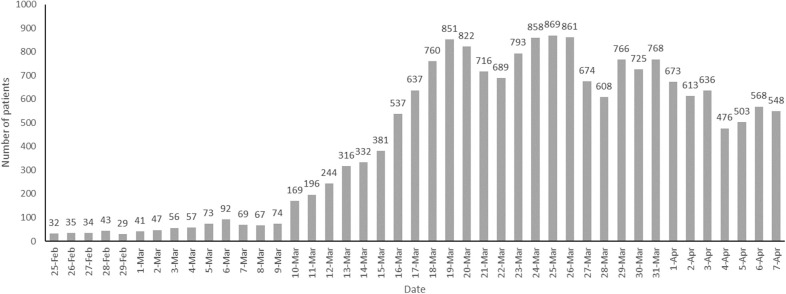
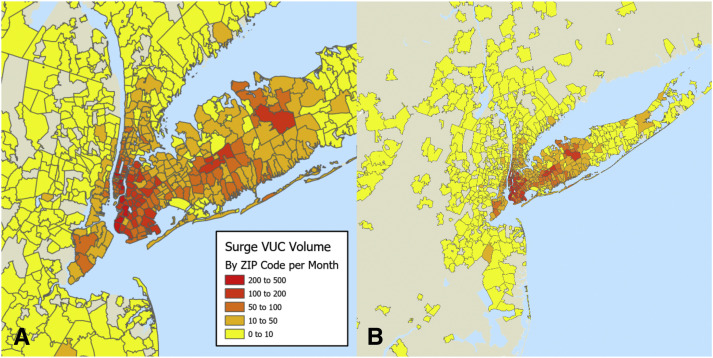
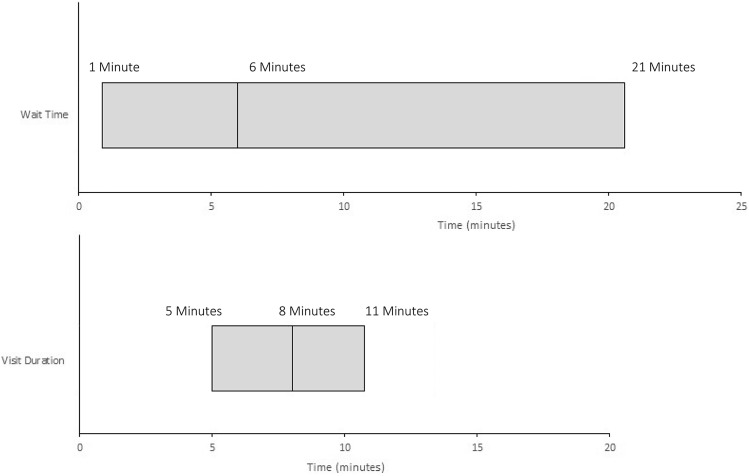
Daily volumes in VUC rapidly increased during the early portion of the study period, and peaked at 869 completed daily visits by mid-March (Figure 1 ). Geospatial analysis demonstrated a wide catchment area of patients for VUC, in both the New York City metropolitan area (Figure 2 A) and the wider tri-state area (Figure 2B). The median wait time to be seen during the study period was 6 min (interquartile range 0–21 min). Median visit duration during the study period was 8 min (interquartile range 5–11 min) (Figure 3 ).
Figure 1.
Daily patient volumes in virtual urgent care during the study period. The twelve days preceding the study period are also included for comparison.
Figure 2.
Geocoded map of virtual urgent care patient volume by zip code in the (A) larger tristate area and (B) in the New York City area.
Figure 3.
Box plot of median wait time and median visit duration, with interquartile ranges, for virtual urgent care visits during the one-month study period.
Previously, during “normal” operations, the VUC was staffed by a single emergency physician at a time; two physicians were scheduled for sequential 8-h shifts per calendar weekday (or a single 12-h shift per weekend day). In response to rapidly escalating daily volumes, available emergency medicine attendings across the United States were recruited and asked to staff VUC whenever their schedule permitted. Recruiting was primarily done from the existing or previous emergency medicine faculty, or residency alumni of the institution. We expanded the VUC regular operating hours of 7 am–11 pm on weekdays and 7 am–7 pm on weekends to a 24-h model; physician assistants were also added to the platform. Providers were on-boarded, trained via teleconference with a focused Epic training, and then staffed VUC in an “on-demand” fashion. Liability coverage was provided by the group's existing medical malpractice coverage; New York State provided additional liability protections during the state of emergency (19). A total of 251 physicians and physician assistants were ultimately onboarded and trained for VUC in late February and early March. As in-person urgent care centers within the network closed in early March, those providers were redeployed online to provide additional VUC coverage during the study period. At the peak of the study period, a total of 62 providers were available to see at least some patients daily via the VUC platform, for a total of 364 provider-hours in that 24-h period (March 25).
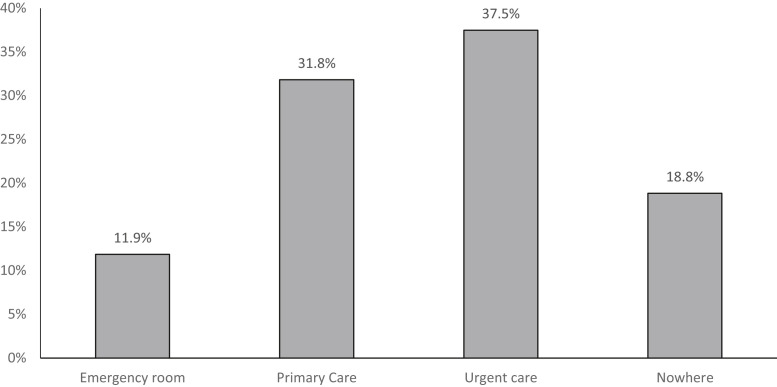
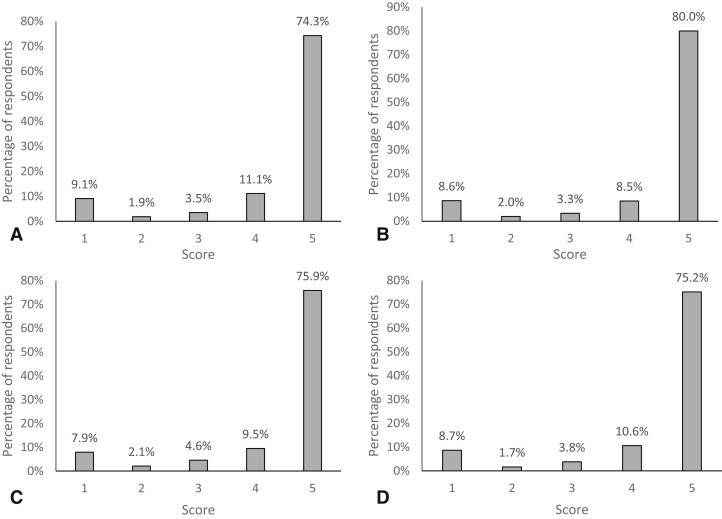
Of the 17,730 patients seen in the study period, 2668 (15.05%) responded to the online survey at the time of visit completion. A total of 2165 (81.16%) reported that they would have sought care in person had the VUC option been unavailable—either in an ED (11.86%), urgent care center (37.49%), or via their primary care provider (31.82%); 18.84% of survey respondents reported that they would not have sought care elsewhere (Figure 4 ). Survey results for satisfaction and likelihood to recommend VUC are presented in Figure 5 .
Figure 4.
Survey responses to “Where would you have sought care today had virtual urgent care not been available?”.
Figure 5.
Patient survey response scores, on a 1 to 5 scale, for satisfaction (A), likelihood to recommend (B), likelihood to use again (C), and overall needs met rating (D).
Discussion
COVID-19, clinically, may range in severity from asymptomatic cases, to mild upper respiratory symptoms, to more severe lower pulmonary disease. The most frequent complaints are nonspecific—fever, myalgias, fatigue, cough, and dyspnea; less common gastrointestinal symptoms, congestion or sore throat, or loss of smell or taste may occur (20,21). The Centers for Disease Control and Prevention reported a hospitalization rate of about 12% during the month of March amongst confirmed COVID-19 cases in the United States, suggesting that many patients with suspected or confirmed, but relatively mild, disease can be managed at home with supportive care and do not require hospitalization (22,23). No specific therapy or antiviral currently exists for outpatient management of COVID-19, but isolation and self-quarantine remain a mainstay of public health management to prevent viral transmission (24). Our results indicate that the majority of patients seen during this period would have traveled to seek care in an ED, urgent care center, or primary care office, had VUC video visit been unavailable to them. These results are similar to previously published rates of alternative care destinations for virtual acute care, in which 12% of patients indicated they would have presented to an ED and 33% would have presented to an urgent care center (25). The overwhelming majority of patients had symptoms concerning for potential COVID-19 infection (Table 2); a VUC video visit allows for access to care while observing social distancing and quarantine provisions.
A number of studies have compared telemedicine-based urgent care to in-person care. A claims-based analysis of acute care telemedicine suggested that patients managed virtually had a similar follow-up rate and lower rates of laboratory testing and imaging, with associated cost savings (15,26). During the current COVID-19 pandemic, with shelter-in-place ordinances access the nation, virtual on-demand care provides access to care but allows patients to remain in the safety of their homes (9,11). Urgent care telemedicine visits have been estimated to result in short-term cost savings due to diversion of patients away from more expensive care settings (16,25). Overall, patient satisfaction results in our study indicated that the majority of patients were both satisfied and would use VUC again (Figure 5). Patients from other centers asked to assess their experience with virtual evaluations in prior studies have similarly reported high rates of satisfaction outside a pandemic situation (27, 28, 29, 30).
Our results also demonstrate that VUC was utilized by patients in a large geographic catchment area both within and outside the New York City area. Previous studies of the geographic reach of telecare have similarly demonstrated wide geographic patient intake compared with in-person care (31). These data—both geographic and total patient volume—suggest that the patient interest in a telemedicine urgent care service is widespread in the setting of the COVID-19 pandemic. Physicians and physician assistants can be rapidly introduced to a telemedicine urgent care model under emergency circumstances. In summary, our findings suggest that during a pandemic, telehealth video visits can treat large numbers of patients, lessen unnecessary in-person visits, provide a high degree of patient satisfaction, and help achieve public health social distancing/self-quarantine goals.
Limitations
This study was subject to a number of limitations. First, we did not assess overall quality of care delivered via telemedicine. Although the survey respondents were generally satisfied with their care, it is difficult to compare telemedicine care to traditional in-person urgent or ED care with respect to classically applied quality measures. In addition, surveys were collected after the VUC visit was completed. This might bias the data in a number of subtle ways. For example, a patient who was reassured about their symptoms or managed expectantly might report that they would not have sought in-person care after the fact if they felt, in hindsight, that it would not have been helpful. Similarly, patients who felt their complaint was minor but then needed an intervention or were prescribed a medication might respond differently after visit completion.
This study was specifically performed during a pandemic situation in New York City, and the results may not be generalizable to telemedicine or virtual care experience outside those conditions; patients may prioritize care from a distance during the study period given the circumstances. Satisfaction data may be influenced by the optional nature of the study; patients who were frustrated might have been more likely than satisfied patients to complete the survey, for example, which may bias the survey data. Finally, although the survey data suggest that VUC was able to divert patients from busy EDs or urgent care centers, limited survey responses and other confounding variables limit our ability to conclusively demonstrate this effect. We did not specifically examine any specified 24-h outcomes or returns to VUC or ED in this work. Future research should examine quality measures for urgent care delivered via telemedicine platforms and consider systemic effects in a more rigorous study.
Conclusions
A VUC was scaled to manage a daily visit volume of more than 800 diverse patients a day, with a variety of complaints, across a large geographic catchment area, during an emergency situation such as a viral pandemic. Physicians were rapidly onboarded, trained, and deployed to see patients on the platform. A large percentage of patients seen via VUC during the study period had viral upper respiratory infection symptoms and possible or probable COVID-19; the opportunity to counsel and quarantine patients who do not require hospital admission at home has obvious public health implications to mitigate disease spread and minimize hospital and ED crowding. Overall reported satisfaction was high. About 50% of patients indicated they would have presented to a local ED or urgent care in person if not for VUC availability, suggesting successful diversion of thousands of patients from crowded hospitals and urgent care centers.
Article Summary
1. Why is this topic important?
The coronavirus disease (COVID)-19 pandemic surge in New York City led to highly crowded emergency departments (EDs) and urgent care centers. Access to health care was further complicated by social distancing policies and patient and provider fears. Telemedicine and virtual care have been proposed as a possible solution to some of these challenges.
2. What does this study attempt to show?
This study describes the rapid scaling of a telemedicine virtual urgent care to treat and evaluate a large number of patient presentations in the setting of the COVID-19 pandemic in New York City.
3. What are the key findings?
Tens of thousands of patients were evaluated and treated over the course of the study period via a virtual urgent care platform; a variety of diagnoses from a wide geographic catchment area were included. Survey data indicate that many of these patients would have otherwise presented to overcrowded in-person care settings.
4. How is patient care impacted?
In the setting of social-distancing orders and pandemic conditions, telemedicine virtual urgent care may be rapidly scaled to provide access to care for a variety of clinical presentations, across large geographic areas, and may help divert appropriate patients from busy EDs or urgent care centers.
References
- 1.Wu Z., McGoogan J.M. Characteristics of and important lessons from the coronavirus disease 2019 (COVID-19) outbreak in China: summary of a report of 72,314 cases from the Chinese Center for Disease Control and Prevention. JAMA. 2020;323:1239–1242. doi: 10.1001/jama.2020.2648. [DOI] [PubMed] [Google Scholar]
- 2.Centers for Disease Control and Prevention (CDC) Cases in the U.S. https://www.cdc.gov/coronavirus/2019-ncov/cases-updates/cases-in-us.html#reporting-cases Available at:
- 3.Smith N., Fraser M. Straining the system: novel coronavirus (COVID-19) and preparedness for concomitant disasters. Am J Public Health. 2020;110:648–649. doi: 10.2105/AJPH.2020.305618. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Cao Y., Li Q., Chen J. Hospital emergency management plan during the COVID-19 epidemic. Acad Emerg Med. 2020;27:309–311. doi: 10.1111/acem.13951. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Iacobucci G. Covid-19: doctors still at “considerable risk” from lack of PPE, BMA warns. BMJ. 2020:m1316. doi: 10.1136/bmj.m1316. [DOI] [PubMed] [Google Scholar]
- 6.CDC COVID-19 Response Team Severe outcomes among patients with coronavirus disease 2019 (COVID-19) - United States, February 12–March 16, 2020. MMWR Morb Mortal Wkly Rep. 2020;69:343–346. doi: 10.15585/mmwr.mm6912e2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Humphreys J., Schoenherr L., Elia G. Rapid implementation of inpatient telepalliative medicine consultations during COVID-19 pandemic. J Pain Symptom Manage. 2020;60:e54–e59. doi: 10.1016/j.jpainsymman.2020.04.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Berg E.A., Picoraro J.A., Miller S.D. COVID-19 – a guide to rapid implementation of telehealth services. J Pediatr Gastroenterol Nutr. 2020;70:734–740. doi: 10.1097/MPG.0000000000002749. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Khairat S., Meng C., Xu Y., Edson B., Gianforcaro R. Interpreting COVID-19 and virtual care trends: cohort study. JMIR Public Health Surveill. 2020;6:e18811. doi: 10.2196/18811. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Duffy S., Lee T.H. In-person health care as option B. N Engl J Med. 2018;378:104–106. doi: 10.1056/NEJMp1710735. [DOI] [PubMed] [Google Scholar]
- 11.Coombes C.E., Gregory M.E. The current and future use of telemedicine in infectious diseases practice. Curr Infect Dis Rep. 2019;21:41. doi: 10.1007/s11908-019-0697-2. [DOI] [PubMed] [Google Scholar]
- 12.Healy P., McCrone L., Tully R. Virtual outpatient clinic as an alternative to an actual clinic visit after surgical discharge: a randomised controlled trial. BMJ Qual Saf. 2019;28:24–31. doi: 10.1136/bmjqs-2018-008171. [DOI] [PubMed] [Google Scholar]
- 13.Tolins M.L., Hippe D.S., Morse S.C., Evans H.L., Lober W.B., Vrablik M.C. Wound care follow-up from the emergency department using a mobile application: a pilot study. J Emerg Med. 2019;57:629–636. doi: 10.1016/j.jemermed.2019.07.017. [DOI] [PubMed] [Google Scholar]
- 14.Koziatek C., Klein N., Mohan S. Use of a telehealth follow-up system to facilitate treatment and discharge of emergency department patients with severe cellulitis. Am J Emerg Med. 2020 doi: 10.1016/j.ajem.2020.01.061. [Epub ahead of print] [DOI] [PubMed] [Google Scholar]
- 15.Tan L.F., Mason N., Gonzaga W.J. Virtual visits for upper respiratory tract infections in adults associated with positive outcome in a Cox model. Telemed J E Health. 2017;23:200–204. doi: 10.1089/tmj.2016.0018. [DOI] [PubMed] [Google Scholar]
- 16.Wilson L. Urgent care embraces telehealth more centers see advantages of virtual services. Health Data Manag. 2017;25:38–40. [PubMed] [Google Scholar]
- 17.Gough F., Budhrani S., Cohn E. ATA practice guidelines for live, on-demand primary and urgent care. Telemed J E Health. 2015;21:233–241. doi: 10.1089/tmj.2015.0008. [DOI] [PubMed] [Google Scholar]
- 18.McConnochie K.M., Conners G.P., Brayer A.F. Effectiveness of telemedicine in replacing in-person evaluation for acute childhood illness in office settings. Telemed J E Health. 2006;12:308–316. doi: 10.1089/tmj.2006.12.308. [DOI] [PubMed] [Google Scholar]
- 19.New York State No. 202.10: Continuing temporary suspension and modification of laws relating to the disaster emergency. https://www.governor.ny.gov/news/no-20210-continuing-temporary-suspension-and-modification-laws-relating-disaster-emergency Available at:
- 20.Guan W.-J., Ni Z.-Y., Hu Y. Clinical characteristics of coronavirus disease 2019 in China. N Engl J Med. 2020;382:1708–1720. doi: 10.1056/NEJMoa2002032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Huang C., Wang Y., Li X. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet. 2020;395:497–506. doi: 10.1016/S0140-6736(20)30183-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Centers for Disease Control and Prevention (CDC) COVIDView: a weekly surveillance summary of U.S. COVID-19 activity. https://www.cdc.gov/coronavirus/2019-ncov/covid-data/covidview/index.html#hospitalizations Available at:
- 23.Giwa A.L., Desai A., Duca A. Novel 2019 coronavirus SARS-CoV-2 (COVID-19): an updated overview for emergency clinicians. Emerg Med Pract. 2020;22:1–28. [PubMed] [Google Scholar]
- 24.Bhimraj A., Morgan R.L., Shumaker A.H. Infectious Diseases Society of America guidelines on the treatment and management of patients with COVID-19. Infect Dis Soc Am. 2020 doi: 10.1093/cid/ciaa478. [Epub ahead of print] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Nord G., Rising K.L., Band R.A., Carr B.G., Hollander J.E. On-demand synchronous audio video telemedicine visits are cost effective. Am J Emerg Med. 2019;37:890–894. doi: 10.1016/j.ajem.2018.08.017. [DOI] [PubMed] [Google Scholar]
- 26.Gordon A.S., Adamson W.C., DeVries A.R. Virtual visits for acute, nonurgent care: a claims analysis of episode-level utilization. J Med Internet Res. 2017;19:e35. doi: 10.2196/jmir.6783. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Powell R.E., Stone D., Hollander J.E. Patient and health system experience with implementation of an enterprise-wide telehealth scheduled video visit program: mixed-methods study. JMIR Med Inform. 2018;20:e10. doi: 10.2196/medinform.8479. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Polinski J.M., Barker T., Gagliano N., Sussman A., Brennan T.A., Shrank W.H. Patients’ satisfaction with and preference for telehealth visits. J Gen Intern Med. 2016;31:269–275. doi: 10.1007/s11606-015-3489-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Martinez K.A., Rood M., Jhangiani N. Patterns of use and correlates of patient satisfaction with a large nationwide direct to consumer telemedicine service. J Gen Intern Med. 2018;33:1768–1773. doi: 10.1007/s11606-018-4621-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Foster C.B., Martinez K.A., Sabella C., Weaver G.P., Rothberg M.B. Patient satisfaction and antibiotic prescribing for respiratory infections by telemedicine. Pediatrics. 2019;144:e20190844. doi: 10.1542/peds.2019-0844. [DOI] [PubMed] [Google Scholar]
- 31.Kaufman T., Geraghty E.M., Dullet N., King J., Kissee J., Marcin J.P. Geospatial information system analysis of healthcare need and telemedicine delivery in California. Telemed J E Health. 2017;23:430–434. doi: 10.1089/tmj.2016.0144. [DOI] [PubMed] [Google Scholar]