Abstract
Background
The novel coronavirus SARS-CoV-2 has caused a pandemic, overwhelming health care systems around the world. Hospitals around the world, including the United States, have been struggling to adapt to the influx of patients with COVID-19, the illness caused by SARS-CoV2, given limited resources and high demand for medical care.
Objectives
This article seeks to provide emergency physicians with a guide to sonographic findings in COVID-19 and an algorithm by which point-of-care lung ultrasound may assist emergency physicians caring for these patients during the SARS-CoV-2 pandemic.
Discussion
The studies currently being published have established a typical set of ultrasound findings in COVID-19. Point-of-care lung ultrasound is rapid and accessible in most emergency departments in the United States, and even in many resource-poor settings.
Conclusion
Point-of-care ultrasound provides numerous benefits to emergency providers caring for patients with COVID-19, including decreasing resource utilization, assisting in diagnosis, guiding management of the critically ill patient, and aiding in rapid triage of patients under investigations for COVID-19.
Keywords: point of care ultrasound, emergency ultrasound, lung ultrasound, thoracic ultrasound, coronavirus, COVID-19, Covid
Introduction
With the continued spread of the novel coronavirus severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2; causing the illness coronavirus disease [COVID]-19), an influx of patients under investigation (PUIs) presenting to the emergency department (ED) is an inevitability for many hospital systems. This anticipated influx in ED volume of PUIs presents unique challenges to the ED workflow. Clinical presentations of COVID-19 can vary from mild or asymptomatic to critical with acute respiratory failure. As a result, many EDs are erecting disaster tents outside of their main ED for rapid triage, segregation away from non-PUI ED patients, and disposition of well-appearing patients, in addition to expanding their ability to care for intubated patients. Although standard imaging techniques will undoubtedly be employed, point-of-care ultrasound (POCUS) offers a unique strategy for the diagnosis and risk stratification of COVID-19 without utilizing significant ED resources.
Ultrasound in COVID-19
Lung Ultrasound
The typical ultrasound pathology described using a linear and curvilinear ultrasound transducer in patients with COVID-19 are listed below, with corresponding examples from patients with COVID-19 (Figure 1, Figure 2, Figure 3, Figure 4 , also see Video 1) (1, 2, 3):
-
1.
Fused B lines or comet tail artifact are visible under the pleura and can appear discrete, multifocal, or confluent.
-
2.
The involved interstitial tissues have localized thickening and edema, and there is localized pleural effusion around the lesions.
-
3.
The pleural line is discontinuous and interrupted.
-
4.
Subpleural lesions demonstrate patchy, strip, and nodular consolidation.
-
5.
Air bronchogram sign can be seen in the consolidation.
-
6.
Color Doppler ultrasound shows insufficient blood supply in the lesions.
-
7.
Large pleural effusions are rare.
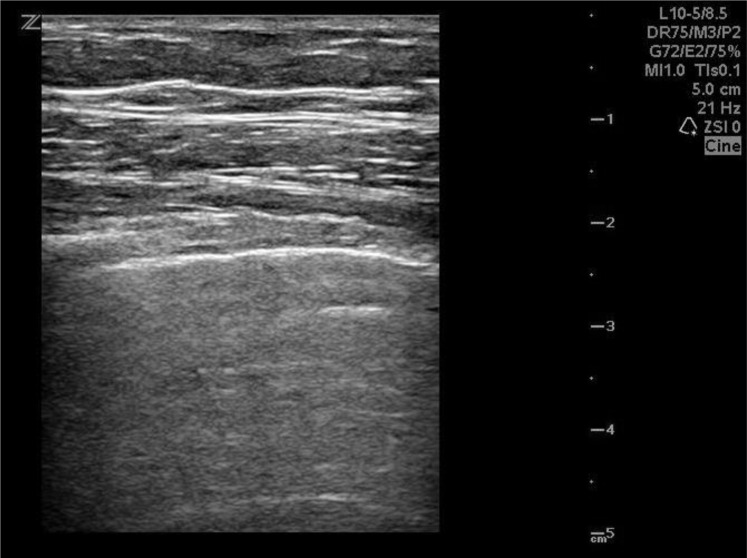
Figure 1.
Normal lung ultrasound with A-line pattern in a patient with COVID-19.
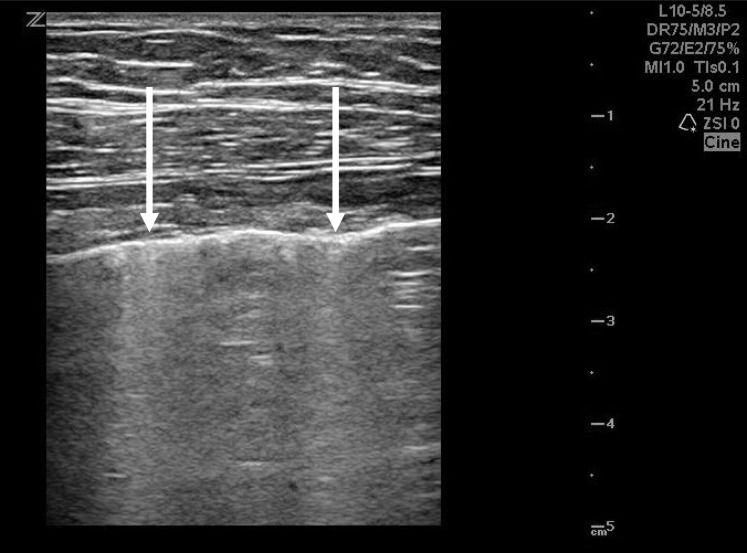
Figure 2.
Patchy Comet-tail artifact (arrows) in a patient with COVID-19.
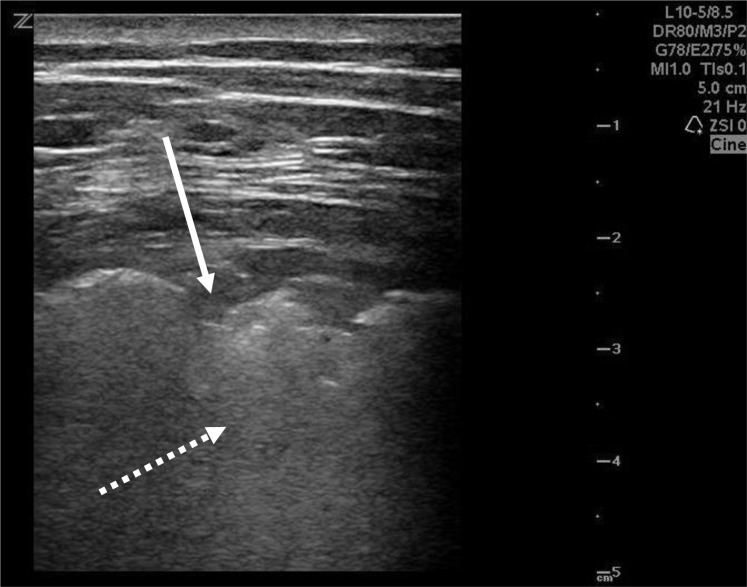
Figure 3.
Pleural line discontinuous, interrupted, and not smooth (solid arrow) with localized edema (dashed arrow) in a patient with COVID-19.
Figure 4.
Subpleural lesion with nodular consolidation (solid arrow), comet-tail artifact (dashed arrow) in a patient with COVID-19.
Currently, there is no consensus on the most appropriate method of ultrasound imaging the PUI population. Although the Volpicelli eight-view approach can be performed, one small study of patients with COVID-19 undergoing computed tomography imaging found that the right lower lobe was the most sensitive for pathology (4). In addition, the posterior lung was involved in 67% of cases (5). Another study of 20 patients with COVID-19 undergoing POCUS imaging found that most lung pathology was found primarily in the posterior lung bases (1). Therefore, scanning the posterior lungs should be prioritized in any lung ultrasound imaging protocol. To obtain the best image quality for the assessment of COVID-19 lung pathology, it is also recommended that a high-frequency linear array transducer or a curvilinear transducer be used (1,3,6).
Cardiac Ultrasound
There have also been numerous reports of COVID-19-related myocarditis and myocardial injury (7, 8, 9, 10). Although the true incidence of COVID-19 myocarditis is unknown, one study found the incidence of dysrhythmia was 16.7%, and acute cardiac injury was 7.2% (10). Another COVID-19 study found that in a series of 21 critically ill intensive care unit patients, one-third developed cardiomyopathy (11). Not all PUIs presenting with respiratory complaints are necessarily linked to COVID-19. Rather, some patients may present with acute heart failure exacerbation, myocardial infarction, valvular disease, pulmonary embolus, or pericardial tamponade. Therefore, in addition to lung ultrasound, a focused cardiac ultrasound should be considered in the PUI population, and is strongly encouraged in any critically ill PUI.
Risk Stratification
Because the volume of PUIs will likely increase during a pandemic, lung ultrasound has the potential to become a tool for risk stratification for several reasons. First, lung ultrasound has shown strong evidence that it has noninferior or superior accuracy compared with chest x-ray study (CXR) for many of the most common causes of dyspnea (12,13). Although CXR imaging is appropriate for the evaluation of lung pathology in COVID-19, up to 18% of patients have a normal initial CXR (14). In addition, a study of patients with a diagnosis of either bacterial pneumonia or H1N1 pneumonia who underwent lung ultrasound imaging found that bedside chest ultrasound provided early detection of interstitial involvement in H1N1 pneumonia even when the CXR was normal (15). It is therefore reasonable to assume that lung ultrasound may have an equivalent or higher sensitivity for detecting lung pathology compared with CXR imaging. If a PUI can avoid CXR, a decrease in radiology resources would likely provide substantial improvements in time to discharge and a decrease in exposure of staff and other patients to PUIs. Ultrasound can also theoretically be used to monitor disease progression. Although no current studies are available, the generally accepted disease progression of COVID-19 is normal lung parenchyma, to scattered B-lines, to confluent B-lines with consolidation. Thus, lung ultrasound could be used for reassessment, or even shed light onto COVID-19 disease staging.
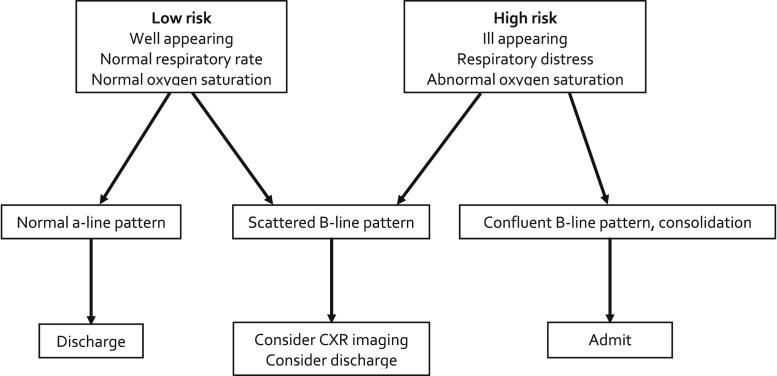
We propose an algorithm that utilizes lung ultrasound as a screening tool to risk-stratify PUIs into low- and high-risk categories (Figure 5 ). Low-risk patients (well appearing, reassuring vital signs) will most likely be discharged from the ED. Many of these low-risk patients will have some facet of respiratory symptoms that may invoke a provider to order a radiology study, specifically, CXR. Utilization of lung ultrasound in low-risk PUIs may therefore be considered to decrease the use of radiology resources. Should a low-risk PUI have lung ultrasound findings indicative of advanced disease, the PUI may need further work-up, including chest radiograph imaging or reassessment for proper disposition. In high-risk PUIs (respiratory distress or grossly abnormal vital signs), ultrasound can help determine how far a patient's disease has progressed and also assess for myocardial dysfunction. Again, the poor sensitivity of CXR imaging and the risk of nosocomial infection to other patients and hospital staff should be considered for all PUIs. If lung ultrasound is performed and advanced disease (i.e., confluent b-line pattern, consolidation) is appreciated, the PUI may be at markedly increased risk of decompensation. Given the significant amount of myocardial disease in critically ill patients with COVID-19, focused cardiac ultrasound should also be used in all high-risk patients.
Figure 5.
Algorithm for PUI screening with lung POCUS. CXR = chest x-ray.
Personal Protective Equipment and Machine Disinfection Procedures
Although ultrasound is generally associated with few risks, the PUI patient population is unique in that providers performing POCUS may have prolonged close contact with the patient. It should be stated that the current recommendation from the Centers for Disease Control and Prevention is to prioritize N95 respirators for aerosol-generating procedures (e.g., intubation, bronchoscopy) (16). Because POCUS does not qualify as an aerosol-generating procedure, surgical masks can be used as personal protective equipment. Notwithstanding, because minimizing PUI contact is always preferred, POCUS should be performed only if it may change clinical decision-making.
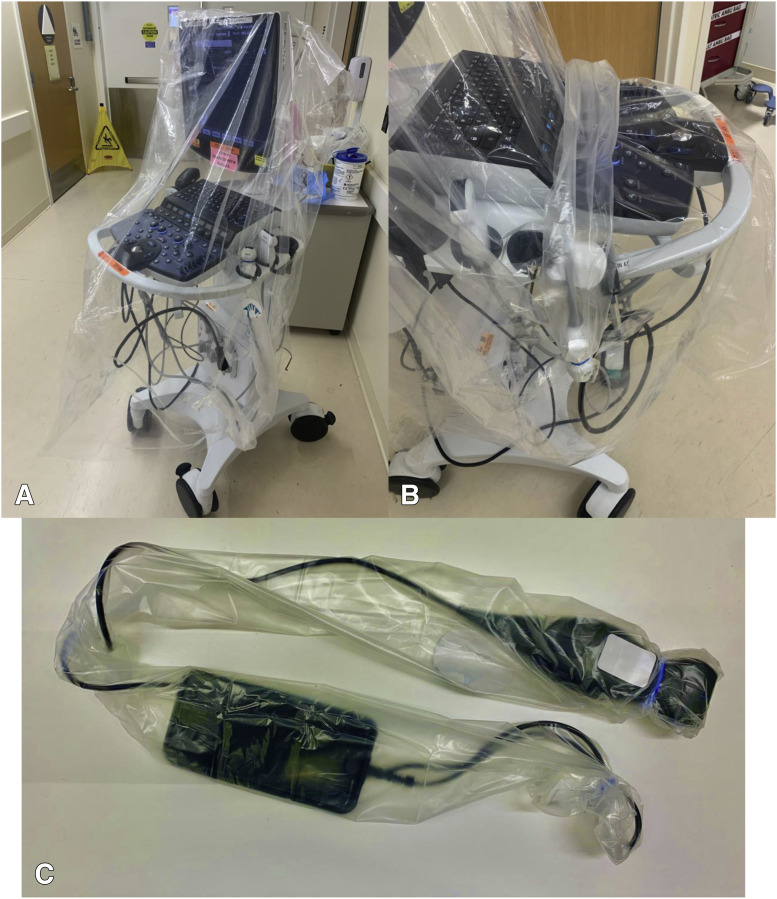
Ultrasound machines can also be exposed to respiratory droplets from PUI after prolonged contact. A recent article stated that viable SARS-CoV-2 can remain on fomites for up to 72 h (17). Strict disinfection control should be maintained. For POCUS cart-based machines, a large plastic equipment cover can be placed over the machine and exchanged between patients (Figure 6 ). In addition, using disposable ultrasound transducer covers between examinations can be used to avoid contaminating the transducer. After use, the machine and transducer should be disinfected using a product approved by the Environmental Protection Agency (EPA) for SARS-CoV2. A full list can be found at the EPA website: https://www.epa.gov/pesticide-registration/list-n-disinfectants-use-against-sars-cov-2.
Figure 6.
Large plastic equipment cover over POCUS cart-based machine (A) with disposable ultrasound probe over phased-array ultrasound probe (B). Disposable ultrasound probe cover encompassing the entirety of a hand-held portable ultrasound (C).
The disinfection of hand-held portable ultrasound machines may be less cumbersome. These machines may be able to fit entirely in a sterile transducer cover and closed off to the external environment (Figure 6). After use, the apparatus can be removed and more easily cleaned with an EPA-approved disinfectant.
Conclusion
The implementation of bedside POCUS during this novel coronavirus pandemic will likely be different across institutions. The ability to utilize POCUS will vary based on ED volume, availability of resources, and workflows specific to institutional needs. Having a basic understanding of ultrasound's ability to diagnose and risk-stratify may improve workflow, risk-stratify PUIs, and diagnose lung pathology missed by traditional radiological imaging. The proposed algorithm may assist in decreased utilization of resources and expediting care of PUIs. Further studies are needed to determine the impact of such risk-stratifying algorithms on ED throughput, costs, and radiation exposure to the patient during the SARS-CoV-2 pandemic.
Footnotes
Streaming video: A brief real-time video clip that accompanies this article is available in streaming video at www.journals.elsevierhealth.com/periodicals/jem. Click on Video Clip 1.
Supplementary Data
Linear ultrasound of thorax in a patient with COVID-19. There are multiple areas of irregular, discontinuous pleural line with concomitant subpleural consolidation, comet-tail artifact and localized edema.
References
- 1.Huang Y., Wang S., Liu Y. A preliminary study on the ultrasonic manifestations of peripulmonary lesions of non-critical novel coronavirus pneumonia (COVID-19) (February 26, 2020) https://ssrn.com/abstract=3544750 Available at: Accessed April 7, 2020.
- 2.Peng Q., Wang X., Zhang L. Chinese Critical Care Ultrasound Study Group (CCUSG). Findings of lung ultrasonography of novel corona virus pneumonia during the 2019–2020 epidemic. Intensive Care Med. 2020;46:849–850. doi: 10.1007/s00134-020-05996-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Buonsenso D., Piano A., Raffaelli F. Point-of-care lung ultrasound findings in novel coronavirus disease-19 pnemoniae: a case report and potential applications during COVID-19 outbreak. Eur Rev Med Pharmacol Sci. 2020;24:2776–2780. doi: 10.26355/eurrev_202003_20549. [DOI] [PubMed] [Google Scholar]
- 4.Gargani L., Volpicelli G. How I do it: lung ultrasound. Cardiovasc Ultrasound. 2014;12:25. doi: 10.1186/1476-7120-12-25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Yoon S.H., Lee K.H., Kim J.Y. Chest radiographic and CT findings of the 2019 novel coronavirus disease (COVID-19): analysis of nine patients treated in Korea. Korean J Radiol. 2020;21:494–500. doi: 10.3348/kjr.2020.0132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Soldati G., Smargiassi A., Inchingolo R. Is there a role for lung ultrasound during the COVID-19 pandemic? J Ultrasound Med. 2020;39:1459–1462. doi: 10.1002/jum.15284. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Zeng J.H., Liu Y., Yuan J. First case of COVID-19 infection with fulminant myocarditis: a case report and insights. Infection. 2020:1–5. doi: 10.20944/preprints202003.0180.v1. [Epub ahead of print] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.American College of Cardiology (ACC) ACC Clinical Bulletin: cardiac implications of novel coronavirus (COVID-2019) https://spc.pt/wp-content/uploads/2020/03/S20028-ACC-Clinical-Bulletin-Coronavirus.pdf Available at:
- 9.Guo T., Fan Y., Chen M. Cardiovascular implications of fatal outcomes of patients with coronavirus disease 2019 (COVID-19) JAMA Cardiol. 2020;5:811–818. doi: 10.1001/jamacardio.2020.1017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Inciardi R.M., Lupi L., Zaccone G. Cardiac involvement in a patient with coronavirus disease 2019 (COVID-19) JAMA Cardiol. 2020 doi: 10.1001/jamacardio.2020.1096. [Epub ahead of print] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Arentz M., Yim E., Klaff L. Characteristics and outcomes of 21 critically ill patients with COVID-19 in Washington State. JAMA. 2020;323:1612–1614. doi: 10.1001/jama.2020.4326. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Chavez M.A., Shams N., Ellington L.E. Lung ultrasound for the diagnosis of pneumonia in adults: a systematic review and meta-analysis. Respir Res. 2014;15:50. doi: 10.1186/1465-9921-15-50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Yousefifard M., Baikpour M., Ghelichkhani P. Screening performance characteristic of ultrasonography and radiography in detection of pleural effusion; a meta-analysis. Emerg (Tehran) 2016;4:1–10. [PMC free article] [PubMed] [Google Scholar]
- 14.Guan W.J., Ni Z.Y., Hu Y. Clinical characteristics of coronavirus disease 2019 in China. N Engl J Med. 2020;382:1708–1720. doi: 10.1056/NEJMoa2002032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Testa A., Soldati G., Copetti R., Giannuzzi R., Portale G., Gentiloni-Silveri N. Early recognition of the 2009 pandemic influenza A (H1N1) pneumonia by chest ultrasound. Crit Care. 2012;16:R30. doi: 10.1186/cc11201. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Centers for Disease Control and Prevention (CDC) Interim infection prevention and control recommendations for patients with suspected or confirmed coronavirus disease 2019 (COVID-19) in healthcare settings. tools.cdc.gov/medialibrary/index.aspx#/media/id/404359 Available at:
- 17.van Doremalen N., Bushmaker T., Morris D.H. Aerosol and surface stability of SARS-CoV-2 as compared with SARS-CoV-1. N Engl J Med. 2020;382:1564–1567. doi: 10.1056/NEJMc2004973. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Linear ultrasound of thorax in a patient with COVID-19. There are multiple areas of irregular, discontinuous pleural line with concomitant subpleural consolidation, comet-tail artifact and localized edema.