The coronavirus disease 2019 (COVID-19) pandemic created an unprecedented disruption to routine patient care (1). Health care professionals scrambled within weeks to attend to the surge of affected individuals amid concerns of hospital capacity and scarcity of personal protective equipment (PPE). Elective procedures, including cardiovascular imaging studies, in stable patients were deferred. Indeed, use of cardiovascular imaging decreased by 50% to 90%, with a shift in the use of certain modalities to conserve much needed PPE or lessen exposure risk to health care professionals. Several professional cardiovascular societies have put forth recommendations on appropriate use of imaging and needed precautions in the early phase of the pandemic (2, 3, 4, 5, 6, 7). Currently, the COVID-19 pandemic has peaked in some parts of the world, but incident infection is still ongoing at different rates in other regions. Communities, heath care professionals, and medical professional societies are considering how to “reopen” medical practices and imaging laboratories in this challenging milieu, while safeguarding the health of both the public and health care professionals (8, 9, 10, 11). This document, initiated by the Editors of JACC: Cardiovascular Imaging and developed in collaboration with the Cardiovascular Imaging Council of the American College of Cardiology, addresses strategies and considerations on how to ramp up multimodality cardiovascular imaging laboratories to serve patients with suspected or known cardiovascular disease and their clinicians, and achieve it safely in an environment of an abating but continued pandemic. Recognizing that practice patterns and policies vary depending on institution and locale, these recommendations are not meant to be restrictive, but rather are meant to serve as a general framework during the COVID-19 pandemic and its recovery phase. Once the pandemic abates and the disease is controlled, the use and prioritization of various modalities would revert to usual and customary practice.
Balancing Safety and Patient Care
The initial response to the COVID-19 pandemic resulted in a significant reduction of nonurgent medical and imaging activity. As we move on from this phase of “lockdown,” we need to balance the risks of infection with the risk posed by inadequate management of chronic medical conditions. Where we stand with this balance depends on community prevalence of active disease. The notion of “ramping up” assumes that transmission rate is falling, or low and stable, and will vary by region and country. There will likely continue to be regional flares of COVID-19 infection and possibly times that laboratories need to revert to an emergency posture, similar to earlier phases of the pandemic.
Re-establishing a more normal clinical operation depends on integrated communication among patients, referring physicians, the imaging teams, and administrative staff. There are few aspects to the resumption of “routine” activity that encompass patient and societal health, safety of health care professionals, choice of imaging test, and considerations for scheduling. These are summarized in Table 1 .
Table 1.
Balancing Safety and Patient Care in the COVID-19 Era
Patient and societal health
|
Safety of health care professionals
|
Choice of cardiovascular testing
|
Scheduling considerations
|
COVID-19 = coronavirus disease 2019; PPE = personal protective equipment; TEE = transesophageal echocardiography.
Patient and societal health
Hospitals and medical centers are a potential source of viral transmission, and we hold a duty of care not only to our patients, but also to our staff and the wider community. Hand hygiene, sanitizing measures, masks, and social distancing will be part of our lives for the foreseeable future. This necessitates a redesign of patient experience and clinic facilities. Both clinical referral offices and imaging laboratories should ensure patients are educated with regard to COVID-19 safety protocols and screened for any COVID-19 symptoms prior to the date of examination. Some institutions might opt for COVID-19 testing prior to procedures—they should ensure that these are done expeditiously and minimize multiple trips to the health care facility. However, a negative COVID-19 test is not sufficiently foolproof and should not detract from usual precautions while performing the test. Patients with any COVID-19 symptoms or known exposure prior to their appointment should be instructed to reschedule examinations that could be safely deferred.
Upon arrival to the facility, health screening should be performed for both patients and health care professionals including checks for temperature and symptoms suggestive of COVID-19. The number of accompanying visitors should be kept to a bare minimum (0 to 1). The number of seats and a change in the seating arrangement should be instituted to accommodate physical distancing. For the safety of patients and health professionals, the number of needed personnel and contact time to perform the test should be kept at a minimum, but this should not be attained at the expense of test quality and acquiring the needed information. Equipment should be appropriately cleaned and disinfected based on patients’ COVID-19 status and local infection control policies.
Safety of heath care professionals
The SARS-CoV-2 (severe acute respiratory syndrome coronavirus 2) virus is transmitted by droplets and contact routes. In COVID-19, a significant number of patients may be asymptomatic and may transmit the virus (1). The recommended PPE for health care professionals in cardiovascular imaging laboratories are shown in Table 2 . Appropriate PPE should be mandatory, as per institutional guidelines and routine training of PPE use provided. For patients without symptoms or low risk for COVID-19, standard precautions include a surgical mask, gloves, hand sanitation, and distancing or minimizing contact. As risk increases with close face-to-face contact (echocardiography), possibly aerosolizing tests (exercise testing), or likely aerosolizing procedures (transesophageal echocardiography [TEE]), the PPE requirements increase (Table 2). Known or suspected cases of COVID-19 need particular attention to PPE; such studies, if needed and cannot be postponed, are performed ideally in negative-pressure rooms, with sufficient air exchange so as to effectively remove most room contaminants. As viral testing becomes more available, a negative COVID-19 test prior to TEE or exercise testing will substantially reduce the risk to heath care providers, provided this is obtained within 24 to 72 h and patients quarantined in the interim. However, current testing is at best only 80% to 85% sensitive for COVID-19 due to several factors (12, 13, 14), so appropriate PPE is still needed for high-risk procedures such as exercise testing and TEE. Vulnerable heath care providers are those with increasing age (>60 years), immunosuppression, presence of comorbidities, and pregnancy. These should be taken into consideration, particularly for those performing higher-risk testing. The community prevalence of active disease may modify both testing choices and PPE requirements in the future.
Table 2.
Exposure Risk and Needed PPE During Cardiovascular Imaging in the COVID-19 Era
| CV Imaging Procedure |
Exposure Type |
Personal Protective Equipment |
|
|---|---|---|---|
| No Symptoms Suggestive of COVID-19 | Confirmed/Suspected/Recovering COVID-19 | ||
| Cardiovascular CT/CMR | Droplet/contact | Surgical mask + gloves | Surgical mask + face shield + gown + gloves∗ |
| Pharmacological stress (SPECT/PET/CMR) | Droplet/contact | Surgical mask + gloves | Surgical mask + face shield + gown + gloves∗ |
| TTE/pharmacological stress echocardiography | Droplet with close contact (face-to-face) | Surgical mask + face shield + gloves |
Surgical mask + face shield + gown + gloves∗ |
| Exercise test (SPECT/echocardiography/treadmill/MVO2)∗ | Possible aerosol generating | †N95 or N99 mask + face shield + appropriate surgical gown + gloves OR Reusable PAPR + surgical gown + gloves | Alternate test recommended (or MVo2 postponed) |
| TEE∗ | Aerosol generating | †N95 or N99 mask + face shield + appropriate surgical gown + gloves OR Reusable PAPR + surgical gown + gloves | N95 or N99 mask + face shield + appropriate surgical gown + gloves OR Reusable PAPR + surgical gown + gloves |
CMR = cardiac magnetic resonance; CT = computed tomography; CV = cardiovascular; MVO2 = myocardial oxygen consumption during exercise; PAPR = powered air-purifying respirator; PET = positron emission tomography; SPECT = single-photon emission tomography; TTE = transthoracic echocardiography; other abbreviations as in Table 1.
For safety, test is best performed in a negative-pressure room with a good air exchange.
COVID-19 testing is currently at most 80% to 85% sensitive; an N95 or N99 mask or reusable PAPR is currently still advised for optimal protection.
Any staff member that develops COVID-19 symptoms or comes into contact with a known COVID-19 case without proper PPE should be immediately quarantined and only return to work after satisfying institutional criteria. Trainees should maintain physical distancing with each other and attending physicians. Minimizing exposure of trainees and nonessential staff was vital in the acute phase of the pandemic for their own safety and for conservation of PPE. However, as the community prevalence falls and more PPEs are available, these policies should be revisited in order to provide effective training. Reading rooms should also follow sanitary requirements and physical distancing. Communication with referring physicians using digital media can be performed where applicable. Last, rostering of medical and allied health staff needs to be planned so that an infection within 1 team will not necessarily compromise another.
Choice of cardiovascular test
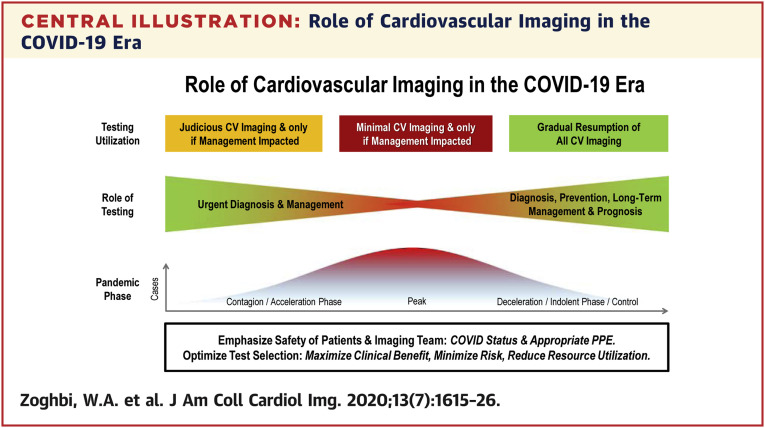
During the initial phase of the pandemic, the emphasis was on triage and performance of essential studies only. In the long term, this is of course potentially detrimental. In an environment of lower infective risk, the emphasis is changing to appropriate use (Central Illustration ). The appropriate use criteria are widely accepted (15, 16, 17, 18, 19). Although there will always be exceptions to “rarely appropriate” indications, based on the patient’s clinical setting, particular attention should be paid to routine studies in asymptomatic patients. In the post–COVID-19 era, the known financial implications of redundant testing are compounded by other safety aspects outlined above. It remains difficult to provide uniform guidelines about test selection because this is often dependent on local availability, quality, and expertise. Nonetheless, now more than ever, there is the need to develop a consensus approach to, for example, noninvasive testing for coronary artery disease (CAD) or quantification of valvular heart disease at a local level.
Central Illustration.
Role of Cardiovascular Imaging in the COVID-19 Era
Dynamic changes in the utilization and role of cardiovascular imaging during the different phases of the COVID-19 pandemic. COVID-19 = coronavirus disease 2019; CV = cardiovascular.
During the acute phase of the pandemic, there was a massive reduction in the performance of TEE. However, as TEE remains the most reliable imaging approach for the detection and assessment of bacterial endocarditis, its increased use with appropriate precautions is warranted (20). Carefully selected, elective studies may be safely performed in the coming months by the use of COVID-19 testing (if available) and needed PPE for practitioners. Appropriate emphasis has been made on reducing the encounters of any potential interaction between a patient and a person collecting images. Often, this has led to a targeted examination, particularly echocardiography. This also is unattractive in the long term, as 1 of the benefits of echocardiography is the detection of significant unsuspected findings, which are likely to be missed with focused exams. It would be preferable to put in place an examination protocol that covers the full breadth of imaging and Doppler but achieve it with the minimum possible contact with the patient (e.g., using simultaneous multiplanar acquisitions). From a research standpoint, the new era should produce a new emphasis on high-quality 3-dimensional acquisitions with off-line processing, as well as robotic image acquisitions, controlled by sonographers removed from the patient, or eventually by automated algorithms based on image recognition. Such devices are already available, but further advances in haptics will enhance safety and effectiveness.
Scheduling considerations
Laboratories are likely to face significant rush for cardiac imaging services due to pent-up demand over the last couple of months. It will be important to reopen these services thoughtfully, keeping in mind both safety and quality. The focused statements from cardiovascular societies are foundational documents that can help with planning and executing the return to normal level of clinical services in cardiac imaging.
Operations in laboratories are slower and disrupted by the pandemic and will require a redesign within institutions. Patients are concerned about contracting COVID-19 in medical institutions, partly accounting for fewer clinic visits and test deferral. Reaching out to patients, addressing their concerns, and stressing the safety measures undertaken are paramount. Allowing adequate time in between studies for sanitation of equipment, beds, and chairs will cause unavoidable time delays and may necessitate expanded hours of operations, possibly including weekends to accommodate testing requests. For those needing to use public transport, avoidance of rush-hour travel is prudent, providing another reason for labs to change opening and closing times. Owing to the acute phase of the pandemic and to slowing operations, backlogs of patients are likely present and need to be managed. In this scenario, patients will need to be prioritized through coordination between laboratory staff and referring physicians depending on the relative urgency of the clinical setting and impact of the test on patient management.
Considerations For Echocardiography
Among imaging modalities, transthoracic echocardiography (TTE) is frequently the first line imaging test in evaluating patients with suspected or known cardiovascular disease (15,17, 18, 19,21). TTE has the advantage of a bedside examination to evaluate patients in the emergency department or those hospitalized, in isolation, or in the intensive care units, which proved particularly helpful in the care of COVID-19 patients. However, compared with other modalities, TTE acquisition necessitates the closest, face-to-face contact with the patient. TTE performance thus requires at a minimum a face shield in addition to a surgical mask and gloves; this PPE increases in the setting of a positive or suspected COVID-19 patient for all modalities (Table 2). TEE, on the other hand, is a potentially aerosolizing procedure that necessitates full PPE (Table 2). The American Society of Echocardiography has provided a comprehensive statement regarding protection of patients and providers during the outbreak and more recently during the recovery phase (2,9). These statements are foundational. We will address briefly echocardiography in the COVID-19 era and during the reopening phase of laboratories.
Transthoracic echocardiography
Because TTE is the most common imaging test performed on patients with COVID-19, attention to appropriate indications and PPE use is crucial. Recent data suggest that COVID-19 infection is frequently associated with myocardial injury, myocardial dysfunction, or clinical heart failure as seen in >50% of fatalities and >10% of survivors (22). Moreover, recent data from Wuhan and New York have suggested that an assessment of cardiac function, particularly right ventricular size and function, using limited TTE during the first week of hospital stay may be extremely insightful for early risk stratification of patients (23). With the ongoing COVID-19 pandemic, point-of-care ultrasound (POCUS) or limited TTE continue to play critical roles for driving decisions for patient care, especially for COVID-19–positive patients (24). POCUS can be particularly helpful in the hands of physicians experienced with echocardiography who are actively taking care of COVID-19 patients in the hospital. The benefits of POCUS include reduced time to diagnosis, easier disinfection, reduced costs, and help in triaging appropriate patients for limited or comprehensive echocardiograms. In intensive care units or hospital areas dedicated to COVID-19 patients, it is advisable to have a dedicated scanner, if possible. Although POCUS and limited examinations can be performed, it is imperative to emphasize the importance of comprehensiveness and quality of a study to assess and act on the information that is gleaned. The appropriate use of contrast enhancing agents for evaluation of ventricular function cannot be understated (25).
As patient referral to the echocardiography laboratory increases in the inpatient and outpatient settings with gradual resumption of operations, the emphasis on safety of patients and health care professionals is still paramount. TTE examinations should provide a comprehensive evaluation of cardiac structure and function for optimal interpretation and decision making. The appropriate indications for TTE are extensive (17,18,21) and are prioritized according to the seriousness of the clinical condition, scheduling backlog, and available PPE (9). Table 3 lists the use of TTE and other modalities in selected clinical scenarios and how the pandemic has affected their use. With the measures taken for safety and scheduling, TTE activity should be able to resume to a near normal state, with the expected slowing of daily operations afforded by the added safety precautions.
Table 3.
Role of Cardiovascular Imaging Specific to the COVID-19 Era: Minimize Risk, Reduce Resource Utilization, and Maximize Clinical Benefit
| Condition | Indication | TTE | TEE | CTA | CMR | Nuclear Cardiology (SPECT/PET)∗ |
|---|---|---|---|---|---|---|
| CAD/myocardial injury | After STEMI intervention in selected COVID-19(+) | ++++ | x | x | + | x |
Stable NSTEMI/ACS
|
++++ ++++ |
x x |
++† ++++ |
+† ++++ |
+† ++++ |
|
Chest pain with
|
+++ ++ |
x x |
++++ ++ |
++++ ++++ |
++++ ++++ |
|
| Cardiomyopathy/arrhythmias | New onset heart failure/cardiomyopathy | ++++ | + | +++ | ++++ | +++ |
| Myocardial viability imaging | + | x | + | ++++ | ++++ | |
| LAA evaluation prior to restoration of sinus rhythm | x | ++† | ++++ | ++ | x | |
| Valvular/structural | Endocarditis (native or prosthetic valve) | +++ | ++++ | ++ | ++ | ++ |
| Endocarditis, invasive complications (e.g., abscess, pseudoaneurysm) | ++ | ++++ | ++++ | ++ | ++ | |
| Prosthetic valve dysfunction (pannus, thrombus, calcification) | ++++ | ++† | ++++ | + | x | |
Structural intervention planning
|
+++ ++++ |
+† ++++ |
++++ ++ |
++ ++ |
x x |
|
| Masses/other | Cardiac mass evaluation | ++++ | ++† | +++ | ++++ | + |
| Pericardial diseases | ++++ | +† | +++ | ++++ | x |
All clinical scenarios in the table assume no active or symptomatic COVID-19 disease, unless otherwise specified. 1+ to 4+ denote a measure of suitability for use during the peri–COVID-19 pandemic period and not necessarily a determination of any inherent diagnostic superiority of one modality over another or comparative efficacy. Strength of the indication and use of a test (1+ to 4+; X = rarely, if at all) and its traditional appropriateness for the clinical condition may be modified by the COVID-19 pandemic as noted. The table summarizes most common clinical indications relevant during the pandemic and cannot capture all nuances in clinical presentations which may affect appropriate test use.
(+) = positive; ACS = acute coronary syndrome; CAD = coronary artery disease; CTA = computed tomography angiography; LAA = left atrial appendage; NSTEMI = non–ST-segment elevation myocardial infarction; STEMI = ST-segment elevation myocardial infarction; TAVR = transaortic valve replacement; other abbreviations as in Tables 1 and 2.
Stress echocardiography has similar scoring to stress nuclear for the CAD and cardiomyopathy indications on this table. The stress type for all imaging modalities, where applicable, is pharmacological stress. Exercise stress has specific considerations during the active pandemic.
Reduced test use or priority compared with other tests because of COVID-19 risk exposure or need for more PPE. This reduction in use will undoubtedly lessen and be back to usual practices once the active infection rate of COVID-19 in the community is low and the pandemic is controlled.
Intensified medical therapy and conservative approach when possible in view of COVID-19 status.
Good imaging practices can make the procedure safe and efficient in the peripandemic milieu:
-
•
In COVID-19–positive or suspected patients, the clinical relevance of the indication for TTE is paramount.
-
•
POCUS or limited TTE can help assist bedside evaluation of cardiac structure and function and is particularly helpful in COVID-19–positive patients to help expedite care and further triage patients who need a comprehensive TTE.
-
•
The use of ultrasound-enhancing agents is essential in technically difficult studies to enhance assessment of regional and global function and attain a diagnostic study.
-
•
As the pandemic is abating, comprehensive TTE should be aimed for with appropriate PPE and efficiency to address the myriad of clinical questions of cardiac and valvular function, pericardial diseases, and hemodynamics.
Transesophageal echocardiography
TEE is a powerful modality for the evaluation of cardiac structure and function in cases in which TTE may be limited or technically difficult, and for planning or guidance during interventional procedures. Because of the safety concerns regarding potential for aerosol generation during the procedure and need for scarce PPE, the use of TEE during the acute phase of the pandemic significantly decreased, almost to a halt. A shift also was seen in certain traditional TEE indications toward alternative imaging modalities, which may offer similar diagnostic accuracy with less safety risk to staff and resource use. This scenario was commonly seen in patients undergoing cardioversion in which computed tomography angiography (CTA) was used to exclude left atrial thrombus. Less common clinical scenarios were those with prosthetic valve dysfunction, evaluation of cardiac masses, or pericardial effusion in critically ill patients with technically difficult TTE. Of concern is that during the acute phase of the pandemic, a significant decrease in TEE was also seen in patients with suspected endocarditis of native or prosthetic valves or complications of endocarditis such as abscess or pseudo aneurysm. Table 3 shows the current indications and strength of TEE in common clinical scenarios and where its use decreased due to the COVID-19 pandemic.
As the rate of COVID-19 infections decreases, laboratories have gradually seen an increase in TEE procedures using appropriate safety measures. As more PPE is available and most centers have access to COVID-19 testing prior to the procedure, a return to appropriate use of TEEs in the clinical scenarios in which it performs best should be aimed for (Table 3). The following are few considerations for TEE in the waning of the pandemic, aiming for maximal safety and clinical impact:
-
•
TEEs in the era of COVID-19 ideally should be performed in a negative-pressure room with good air circulation.
-
•
Testing for COVID-19 prior to TEE is strongly encouraged, if available, to get interim results between 0 and 3 days before the procedure, with quarantine instituted from the time of the test to the procedure.
-
•
A negative COVID-19 polymerase chain reaction test puts the asymptomatic patient in a low-risk category but does not exclude the disease completely. Although it may alleviate some of the apprehension around the test, maintaining appropriate PPE level is still advised, for the safety of all health care staff involved.
-
•
TEE is uniquely helpful in clinical conditions such as native or prosthetic valve endocarditis and evaluation of associated complications.
-
•
TEE is essential in planning edge-to-edge repair of mitral or tricuspid valves.
-
•
Although TEE is particularly helpful in the assessment of left atrium and appendage prior to cardioversion, occluder device, or atrial fibrillation ablation, alternative testing was used during the early phase COVID-19 for safety concerns and PPE availability.
-
•
As the disease wanes and with more PPE availability, there is a gradual increase in TEE use for its classic and appropriate indications, guided by local conditions and practices.
-
•
The PPE needed for TEE may be re-evaluated in the future by health care professionals if the prevalence of the disease and immunity in the population permit.
Considerations For Stress Testing Modalities (Single-Photon Emission Tomography/Positron Emission Tomography/Echocardiography/Cardiac Magnetic Resonance)
Stress testing is an essential approach in the evaluation and care of patients with suspected or known cardiovascular disease (15). This includes exercise or pharmacologic testing with any of the imaging modalities of nuclear imaging (single-photon emission tomography [SPECT]/positron emission tomography [PET]), echocardiography, or cardiac magnetic resonance (CMR). In the acute phase of the COVID-19 pandemic, exercise testing was avoided, mainly due to infectious risk. Medical therapy for cardiovascular disease in COVID-19 patients needs to be maximized and testing deferred whenever possible, particularly if clinically stable (Table 3). An exercise or stress test is an elective procedure. For indications of suspected CAD in this scenario, coronary CTA is preferred over exercise, but a pharmacological study may also be appropriate. If patients have typical crescendo angina despite optimal medical therapy, coronary angiography with possible percutaneous coronary intervention may be an optimal approach.
A subgroup of COVID-19 patients experience chest pain following the acute phase of infection. As the long-term cardiovascular sequelae of COVID-19 infection remain unknown, it is likely that physicians may want to consider using a diagnostic imaging procedure for assessment of CAD risk. As the pandemic is tapering, the use of stress testing is increasing gradually, with its required safety precautions. The American Society of Nuclear Cardiology, Society for Cardiovascular Magnetic Resonance, and American Society of Echocardiography have recently published guidance on re-establishment of care in laboratories (9, 10, 11). We hereby propose some considerations for the safe reinstitution of stress testing that pertain to all imaging modalities.
General safety considerations for stress testing
The following are safety considerations specific to stress testing, in addition to the general safety detailed previously.
-
•
Know laboratory air circulation patterns—consult engineering on optimized equipment or staff positioning. Given the uncertainty regarding the aerosol generating capacity of exercise stress testing, it may be prudent to use a dedicated room for exercise testing, with negative pressure if possible.
-
•
Allow time for air changes (outpatient facilities usually have a lower exchange than inpatient facilities) before cleaning surfaces and putting a new patient in the room.
-
•
Avoid manual blood pressure measurement if possible. Automated blood pressure is commonly used and reasonably accurate in stationary patients undergoing pharmacological stress testing. For patients undergoing treadmill or bicycle exercise stress testing, accuracy of blood pressure readings may depend on equipment available.
-
•
Personnel overseeing the test should maintain distance (6 feet or 2 m) to the patient whenever possible, with brief closer encounters as needed.
-
•
Personnel involved should wear appropriate PPE, including mask, face shield (particularly during stress echocardiography), and gloves. When possible, the patient should be encouraged to exercise while wearing a surgical mask. If this is not possible, consider the use of face shields.
Choosing exercise versus pharmacologic stress
The following are considerations for exercise versus pharmacological stress testing:
-
•
In settings of moderate to high prevalence of active COVID-19 in the community, pharmacological stress is preferred over exercise, when clinically appropriate, because of added safety concerns and needed PPE during exercise.
-
•
If pharmacological stress is used, careful history can provide information on functional capacity.
-
•
If exercise is thought to be necessary, consider COVID-19 testing before the exercise test.
-
•
If exercising, choose exercise protocols carefully to improve time efficiency. Match the appropriate protocol to the patient—slower protocols lengthen interaction time. A bicycle protocol is associated with lower peak ventilations per minute.
-
•
When a very low prevalence of active COVID-19 is reached in the community, exercise may reclaim first choice when indicated, driven by its provision of much additional information and higher workloads than pharmacological stress.
Considerations for treadmill testing and cardiopulmonary exercise testing
Cardiopulmonary exercise testing is an elective procedure and should be deferred during the acute pandemic phase because collection of exhaled air may enhance concentration of viral particles in the room. However, in the deceleration or indolent phase with low community prevalence of active infections, the use of exercise testing without imaging to assess exercise tolerance, assess arrhythmias during exercise, and determine myocardial oxygen consumption in evaluating patients for heart transplantation are all essential tests, the neglect of which may compromise patient care. The following are some considerations for stress testing in the COVID-19 era:
-
•
Avoid cardiopulmonary exercise testing in patients with prior COVID-19 diagnosis unless clinical recovery is confirmed along with 2 negative COVID-19 tests.
-
•
Assess whether pharmacological stress in association with imaging is an appropriate alternative test. Converting an exercise treadmill test to a pharmacological test is costlier. The precautions noted against exercise need to be weighed.
-
•
Consider available questionnaires alternatively to estimate physical work capacity (e.g., Duke Activity Status Index).
-
•
In heart failure patients being evaluated for transplantation or ventricular assist therapy, consider COVID-19 testing prior to determination of myocardial oxygen consumption during exercise. Also, consider alternatives such as a 6-min walk test that allow for safe distancing between the staff and patients.
General Considerations For Nuclear Cardiology
Nuclear imaging has a robust knowledge base of clinical experience, diagnostic value, and outcomes, and the increasing availability of PET significantly enhances its utility. It was one of the most widely used modalities in cardiac imaging before the COVID-19 pandemic and is likely to regain those usage levels as this pandemic gradually recedes. All commonly used cardiac nuclear imaging procedures are nonaerosolizing and have other advantages of relatively short contact time with the patient, largely automated and time-efficient protocols, and machines that do not need personnel to be in close proximity to the patient for operation. This can reduce spread of infection as well as conserve precious resources. Although cardiac nuclear imaging has minimal utility in managing the acute stages in COVID-19–positive patients, it becomes increasingly valuable as we reopen services to the general population.
Good imaging practices can make the procedure safe and efficient in the peripandemic milieu (3,10,26,27):
-
•
Following best practices for the COVID-19 era, as recommended by various nuclear imaging societies.
-
•
Using protocols that minimize study time without affecting test accuracy, e.g., stress only imaging where feasible and safe.
-
•
Incorporating use of PET instead of SPECT where feasible.
-
•
Avoiding protocols that can aerosolize (e.g., using pharmacological stress instead of exercise stress).
Nuclear cardiology studies are generally not needed in managing acute cardiac illness in COVID-19–positive patients. However, nuclear cardiology has an advantageous role in the peripandemic milieu in patients without known COVID-19 or its risk factors in the following (10,27, 28, 29, 30, 31):
-
•
Evaluating ischemia in patients with known CAD.
-
•
Evaluating patients with chest pain syndromes. It is particularly useful in patients that are not good candidates for anatomic noninvasive imaging (e.g., patients with stents, significant coronary calcification, dye allergy, risk of worsening renal function).
-
•
Evaluating for myocardial viability.
-
•
Screening for amyloidosis.
-
•
Identifying inflammatory stages of sarcoidosis.
-
•
Identifying infections in implanted devices.
General Considerations For Computed Tomography
Computed tomography (CT) can be used to rapidly evaluate multiple forms of cardiac disease throughout all phases of the COVID-19 pandemic, with efficiency and safety (4). The selective use of CT has been shown to be valuable in the acute phase of COVID-19 and will likely serve an important role for new symptoms of possible angina during the convalescent or chronic phase of their illness (15,16). As institutions begin to reintroduce full cardiovascular imaging services, CT will continue to allow for safe and rapid diagnosis of conditions ranging from CAD to valvular heart disease (8,15,18,19,21) (Table 3).
CT in acute coronary syndromes with known or suspected COVID-19
Patients with definitive ST-segment elevation myocardial infarction should proceed directly to expedited therapy (percutaneous coronary intervention or thrombolysis) as per local institutional protocol. In COVID-19–positive patients with elevated cardiac biomarkers, the differential diagnosis may include acute coronary syndrome, myocarditis, or myocardial injury (32). In this setting, the value of coronary CTA to help stratify risk and guide the need for and timing of intracoronary angiography is becoming increasingly established (33,34). Multiphase coronary CTA imaging can allow for an evaluation of left ventricular ejection fraction and regional wall motion abnormalities. Coronary CTA may enable the evaluation of myocarditis through a dedicated delayed iodine enhancement protocol at highly specialized centers (35). Overall, coronary CTA in this setting should only be considered if it is expected to result in a meaningful change to patient management or outcomes, as well as reduce resource use (i.e., avoid invasive angiography) (Table 3) (4).
-
•
Coronary CTA may be useful in selected patients who have elevated cardiac enzymes, inconclusive electrocardiogram, and symptoms of possible acute coronary syndrome in order to exclude obstructive CAD.
-
•
Coronary CTA may enable the evaluation of pulmonary embolism and incidental pulmonary findings such as pneumonia. If typical or atypical pulmonary findings are encountered, consultation with a radiologist with thoracic expertise is encouraged.
CT in the deceleration or indolent phase of COVID-19
Coronary CTA may have distinct advantages in the deceleration and indolent phases of the coronavirus pandemic with regard to efficiency, safety, and resource use (4,7). The ability of coronary CTA to decisively exclude CAD or high-risk anatomy may prevent the need for inpatient admissions from the emergency department, resource use, and exposure to health care workers. On the one hand, in suspected or known cases of COVID-19 disease, coronary CTA is generally preferred over stress testing modalities that increase aerosolization risk (e.g., exercise stress testing) or pharmacological stress tests with long acquisition times and exposure time to patients. In these cases, it is advisable to postpone testing till after recovery from the viral infection. On the other hand, stress testing is preferred over coronary CTA in patients with known CAD, heavy coronary calcifications, and previous stents, and in patients with contraindications to iodinated contrast agents (Table 3). Other clinical scenarios in which coronary CTA may be preferred or a reasonable alternative cardiac imaging modality in the COVID-19 era are the following (4,7,36,37) (Table 3):
-
•
Evaluation of patients with no known CAD presenting with symptoms of possible angina.
-
•
Identifying patients with CAD who can be treated conservatively (e.g., by excluding high-risk anatomy or through the use of CT–fractional flow reserve to exclude functionally significant lesions).
-
•
Cardiac CTA may be preferred in the planning of structural heart procedures such as transcatheter aortic valve replacement and left atrial appendage closure. TEE is still the preferred modality for planning mitral and tricuspid valve edge-to-edge repair.
-
•
Cardiac CTA may be preferred or a reasonable alternative to TEE in the COVID-19 era in excluding left atrial or appendage thrombus prior to cardioversion.
-
•
Cardiac CTA may be a reasonable alternative to TEE in the evaluation of prosthetic and mechanical heart valve dysfunction, perivalvular extension of endocarditis, or possible myocardial abscess.
The scenarios of preference to or alternate to TEE again depend on the status of the pandemic, continued safety concerns and availability of needed PPE.
Coronary artery calcium scoring
Coronary artery calcium (CAC) imaging is the test with the least urgent indication during the pandemic. Dedicated CAC imaging may be considered to decide on the decision to withhold, postpone, or initiate statin therapy as per current American College of Cardiology/American Heart Association guidelines for primary prevention in patients at intermediate or borderline risk. This can be performed at a later phase during the pandemic when the incidence of active infection has tapered, and institutions have determined they may fully resume routine imaging services with appropriate safety considerations. However, CAC may be detected on all noncontrast chest CTs and may be helpful in identifying patients with COVID-19 who have atherosclerotic plaque and cardiac risk.
General Considerations For CMR Imaging During COVID-19
CMR is well positioned to address the cardiac complications from COVID-19, particularly myocarditis, in addition to the myriad of other clinical indications (15,18,19,21). CMR also provides comprehensive answers, by multicomponent imaging in one setting, and thus may reduce PPE use and the need for patient transportation to multiple testing laboratories, and limits infectious exposure during the COVID-19 pandemic. CMR examination, including pharmacological stress, is not an aerosolizing procedure, and its PPE requirement is similar to that of CT. In a single imaging session, CMR can assess cardiac function, ischemia, viability, and valvular function (15,18,19,21). The advent of rapid protocols as well as real-time and single-heartbeat data acquisition ameliorates this situation and decreases the staff and room exposure time (38, 39, 40). In concert with global hospital planning to cope with local surges of COVID-19, CMR programs have deferred many nonurgent studies to reduce risk of infection spread, reduce usage of PPE, and conserve hospital resources. However, we are now positioned to advance appropriate use of CMR to meet the needs for cardiac examination in concordance with society recommendations (11). Several general recommendations on use of CMR during the pandemic can be made (Table 3):
-
•
Shortened, focused CMR protocols (maximum of ∼30 min) should be used across all clinical indications.
-
•
CMR is a preferred method in diagnosing the etiology of left ventricular dysfunction by assessing the pattern of cardiac dysfunction and myocardial tissue characteristics using myocardial perfusion, late gadolinium enhancement, and tissue mapping.
-
•
In patients with chest pain and recent/previous myocardial injury, CMR can assess the underlying etiology (ischemia vs. myocarditis) and residual ischemic burden. The test should be performed if it alters planned medical management and should be avoided or postponed during an active COVID-19 infection.
-
•
In patients with suspected ischemia, pharmacological stress CMR can be safely added to a study session to diagnose and risk-stratify CAD to guide the use of invasive angiography.
With multicomponent imaging, CMR may obviate the need to perform some TEEs during COVID-19. CMR can determine pulmonary vein anatomy and detect left atrial or appendage thrombus (41,42) and may lessen the need for TEE in patients with atrial fibrillation before urgent electrocardioversion or pulmonary vein isolation. The most common approach of CMR imaging in this setting employs a combination of cine imaging, contrast-enhanced magnetic resonance angiography, and late gadolinium enhancement with long inversion time (42). Other technical strengths of late gadolinium enhancement with long inversion time include high feasibility in presence of irregular cardiac rhythm, high tissue contrast between thrombus and surrounding structures, and a lack of need for breath-holding. CMR is limited compared with TEE in detecting small, highly mobile valvular vegetations for work-up of infectious endocarditis but is the preferred modality for defining the presence, extent, and characteristics of nonvalvular cardiac masses.
Resuming CMR service to meet clinical demands
With resumption of services, rescheduling of backlogged CMR studies should be done by categories of clinical priorities. CMR studies with a lower clinical priority acquired with a short and focused protocol can be scheduled into short available time slots. These triage guidelines should be developed with clinical partners and effectively communicated to referral organizations. Wherever possible, redundant imaging examinations should be consolidated to provide the necessary diagnostic or prognostic information for clinical decision making. This will require coordination with other cardiac imaging departments for triage efficiency. Through safe, thoughtful, and effectively communicated measures, CMR centers can provide timely access to patients with urgent indications throughout the COVID-19 pandemic period.
Conclusions
The COVID-19 pandemic has affected human life, stressed health care capacity, and delayed usual delivery of care. As we enter a deceleration or indolent phase of the disease and a return to a “new normal” for the foreseeable future, cardiovascular imaging laboratories will adjust to a different workflow and safety precautions for patients and staff alike. The focus ultimately is the ability to offer the necessary cardiovascular tests and information for the clinical team to provide the best care for patients. To be successful in this new safety-driven modus operandi, innovation, coordination, and adaptation among clinicians, staff, and patients is necessary until herd immunity or control of COVID-19 is achieved.
Footnotes
The views expressed in this paper by the American College of Cardiology's Imaging Section and Leadership Council do not necessarily reflect the views of the American College of Cardiology. Dr. Blankstein has received research support from Amgen Inc. and Astellas Inc. Dr. Jaffer has received research support from Canon and Siemens Healthineers; and has served as a speaker for Siemens Healthineers and Biotronik. Dr. Leipsic has received grant support from GE Healthcare and Edwards Lifesciences; and has served on the Speakers Bureau for GE Healthcare and Philips; and has served as a consultant for and owns stock options in Circle Cardiovascular Imaging and HeartFlow. Dr. Nagel has received research support Siemens Healthineers. Dr. Nieman has received research support from Siemens Healthineers and HeartFlow. Dr. Salerno has received research support from Siemens Healthineers. Dr. Sengupta has served as an advisor to Ultromics, HeartSciences, and Kencor Health. All other authors have reported that they have no relationships relevant to the contents of this paper to disclose.
The authors attest they are in compliance with human studies committees and animal welfare regulations of the authors’ institutions and Food and Drug Administration guidelines, including patient consent where appropriate. For more information, visit the JACC: Cardiovascular Imagingauthor instructions page.
References
- 1.Centers for Disease Control and Prevention Coronavirus (COVID-19) https://www.cdc.gov/coronavirus/2019-ncov/index.html Available at:
- 2.Kirkpatrick J.N., Mitchell C., Taub C., Kort S., Hung J., Swaminathan M. ASE statement on protection of patients and echocardiography service providers during the 2019 novel coronavirus outbreak. J Am Coll Cardiol. 2020;75:3078–3084. doi: 10.1016/j.jacc.2020.04.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Skali H., Murthy V.L., Al-Mallah M.H. Guidance and best practices for nuclear cardiology laboratories during the coronavirus disease 2019 (COVID-19) pandemic: An Information Statement from ASNC and SNMMI. J Nucl Med. 2020;61:784–791. [PMC free article] [PubMed] [Google Scholar]
- 4.Choi A.D., Abbara S., Branch K.R. Society of Cardiovascular Computed Tomography guidance for use of cardiac computed tomography amid the COVID-19 pandemic. J Cardiovasc Comput Tomogr. 2020;14:101–104. doi: 10.1016/j.jcct.2020.03.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Society for Cardiovascular Magnetic Resonance SCMR’S COVID-19 preparedness toolkit. https://scmr.org/page/COVID19 Available at:
- 6.Skulstad H., Cosyns B., Popescu B.A. COVID-19 pandemic and cardiac imaging: EACVI recommendations on precautions, indications, prioritization, and protection for patients and health care personnel. Eur Heart J Cardiovasc Imaging. 2020;21:592–598. doi: 10.1093/ehjci/jeaa072. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.European Society of Cardiology ESC guidance for the diagnosis and management of CV disease during the COVID-19 Pandemic. https://www.escardio.org/Education/COVID-19-and-Cardiology/ESC-COVID-19-Guidance Available at:
- 8.Wood D.A., Mahmud E., Thourani V.H. Safe reintroduction of cardiovascular services during the COVID-19 pandemic: guidance from North American Society Leadership. J Am Coll Cardiol. 2020 May 4 doi: 10.1016/j.jacc.2020.04.063. [E-pub ahead of print] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Hung J., Abraham T.P., Cohen M.S. ASE statement on the reintroduction of echocardiography services during the COVID-19 pandemic. J Am Soc Echocardiogr. 2020 May 20 doi: 10.1016/j.echo.2020.05.019. [E-pub ahead of print] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Skali H., Murthy V., Paez D. Guidance and best practices for reestablishment of non-emergent care in nuclear cardiology laboratories during the coronavirus disease 2019 (COVID-19) pandemic: an information statement from ASNC, IAEA, and SNMMI. J Nucl Cardiol. 2020 May 14 doi: 10.2967/jnumed.120.251355. [E-pub ahead of print] [DOI] [PubMed] [Google Scholar]
- 11.Han Y., Chen T., Bryant J. Society for Cardiovascular Magnetic Resonance (SCMR) guidance for the practice of cardiovascular magnetic resonance during the COVID-19 pandemic. J Cardiovasc Magn Reson. 2020;22:26. doi: 10.1186/s12968-020-00628-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Kucirka L.M., Lauer S.A., Laeyendecker O., Boon D., Lessler J. Variation in false-negative rate of reverse transcriptase polymerase chain reaction–based SARS-CoV-2 tests by time since exposure. Ann Intern Med. 2020 May 13 doi: 10.7326/M20-1495. [E-pub ahead of print] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Wang W., Xu Y., Gao R. Detection of SARS-CoV-2 in different types of clinical specimens. JAMA. 2020;323:1843–1844. doi: 10.1001/jama.2020.3786. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.U.S. Food & Drug Administration FAQs on testing for SARS-CoV-2. https://www.fda.gov/medical-devices/emergency-situations-medical-devices/faqs-testing-sars-cov-2?utm_campaign=2020-05-18%20CDRH%20New&utm_medium=email&utm_source=Eloqua Available at:
- 15.Wolk M.J., Bailey S.R., Doherty J.U. ACCF/AHA/ASE/ASNC/HFSA/HRS/SCAI/SCCT/SCMR/STS 2013 multimodality appropriate use criteria for the detection and risk assessment of stable ischemic heart disease: a report of the American College of Cardiology Foundation Appropriate Use Criteria Task Force, American Heart Association, American Society of Echocardiography, American Society of Nuclear Cardiology, Heart Failure Society of America, Heart Rhythm Society, Society for Cardiovascular Angiography and Interventions, Society of Cardiovascular Computed Tomography, Society for Cardiovascular Magnetic Resonance, and Society of Thoracic Surgeons. J Am Coll Cardiol. 2014;63:380–406. doi: 10.1016/j.jacc.2013.11.009. [DOI] [PubMed] [Google Scholar]
- 16.AJ T., Cerqueira M., JM H., Mark D., Min J., O’Gara P. ACCF/SCCT/ACR/AHA/ASE/ASNC/NASCI/SCAI/SCMR 2010 appropriate use criteria for cardiac computed tomography. A report of the American College of Cardiology Foundation Appropriate Use Criteria Task Force, the Society of Cardiovascular Computed Tomography, the American College of Radiology, the American Heart Association, the American Society of Echocardiography, the American Society of Nuclear Cardiology, the North American Society for Cardiovascular Imaging, the Society for Cardiovascular Angiography and Interventions, and the Society for Cardiovascular Magnetic Resonance. J Am Coll Cardiol. 2010;56:1864–1894. doi: 10.1016/j.jacc.2010.07.005. [DOI] [PubMed] [Google Scholar]
- 17.American College of Cardiology Foundation Appropriate Use Criteria Task Force, American Society of Echocardiography, American Heart Association, et al. ACCF/ASE/AHA/ASNC/HFSA/HRS/SCAI/SCCM/SCCT/SCMR 2011 Appropriate Use Criteria for Echocardiography. A report of the American College of Cardiology Foundation Appropriate Use Criteria Task Force, American Society of Echocardiography, American Heart Association, American Society of Nuclear Cardiology, Heart Failure Society of America, Heart Rhythm Society, Society for Cardiovascular Angiography and Interventions, Society of Critical Care Medicine, Society of Cardiovascular Computed Tomography, and Society for Cardiovascular Magnetic Resonance Endorsed by the American College of Chest Physicians. J Am Coll Cardiol. 2011;57:1126–1166. doi: 10.1016/j.jacc.2010.11.002. [DOI] [PubMed] [Google Scholar]
- 18.Doherty J.U., Kort S., Mehran R., Schoenhagen P., Soman P. ACC/AATS/AHA/ASE/ASNC/HRS/SCAI/SCCT/SCMR/STS 2017 appropriate use criteria for multimodality imaging in valvular heart disease: a report of the American College of Cardiology Appropriate Use Criteria Task Force, American Association for Thoracic Surgery, American Heart Association, American Society of Echocardiography, American Society of Nuclear Cardiology, Heart Rhythm Society, Society for Cardiovascular Angiography and Interventions, Society of Cardiovascular Computed Tomography, Society for Cardiovascular Magnetic Resonance, and Society of Thoracic Surgeons. J Am Coll Cardiol. 2017;70:1647–1672. doi: 10.1016/j.jacc.2017.07.732. [DOI] [PubMed] [Google Scholar]
- 19.Doherty J.U., Kort S., Mehran R. ACC/AATS/AHA/ASE/ASNC/HRS/SCAI/SCCT/SCMR/STS 2019 Appropriate Use Criteria for Multimodality Imaging in the Assessment of Cardiac Structure and Function in Nonvalvular Heart Disease: A Report of the American College of Cardiology Appropriate Use Criteria Task Force, American Association for Thoracic Surgery, American Heart Association, American Society of Echocardiography, American Society of Nuclear Cardiology, Heart Rhythm Society, Society for Cardiovascular Angiography and Interventions, Society of Cardiovascular Computed Tomography, Society for Cardiovascular Magnetic Resonance, and the Society of Thoracic Surgeons. J Am Coll Cardiol. 2019;73:488–516. doi: 10.1016/j.jacc.2018.10.038. [DOI] [PubMed] [Google Scholar]
- 20.Habib G., Lancellotti P., Antunes M.J. 2015 ESC guidelines for the management of infective endocarditis: the task force for the management of infective endocarditis of the European Society of Cardiology (ESC) endorsed by: European Association for Cardio-Thoracic Surgery (EACTS), the European Association of Nuclear Medicine (EANM) Eur Heart J. 2015;36:3075–3128. doi: 10.1093/eurheartj/ehv319. [DOI] [PubMed] [Google Scholar]
- 21.Patel M.R., White R.D., Abbara S. 2013 ACCF/ACR/ASE/ASNC/SCCT/SCMR appropriate utilization of cardiovascular imaging in heart failure: a joint report of the American College of Radiology Appropriateness Criteria Committee and the American College of Cardiology Foundation Appropriate Use Criteria Task Force. J Am Coll Cardiol. 2013;61:2207–2231. doi: 10.1016/j.jacc.2013.02.005. [DOI] [PubMed] [Google Scholar]
- 22.Zhou F., Yu T., Du R. Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: a retrospective cohort study. Lancet. 2020;395:1054–1062. doi: 10.1016/S0140-6736(20)30566-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Li Y., Li H., Zhu S. Prognostic value of right ventricular longitudinal strain in patients with COVID-19. J Am Coll Cardiol Img. 2020 Apr 28 doi: 10.1016/j.jcmg.2020.04.014. [E-pub ahead of print] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Johri A.M., Galen B., Kirkpatrick J.N., Lanspa M., Mulvagh S., Thamman R. ASE statement on point-of-care ultrasound (POCUS) during the 2019 novel coronavirus pandemic. J Am Soc Echocardiogr. 2020;33:670–673. doi: 10.1016/j.echo.2020.04.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Porter T.R., Mulvagh S.L., Abdelmoneim S.S. Clinical applications of ultrasonic enhancing agents in echocardiography: 2018 American Society of Echocardiography guidelines update. J Am Soc Echocardiogr. 2018;31:241–274. doi: 10.1016/j.echo.2017.11.013. [DOI] [PubMed] [Google Scholar]
- 26.Gewirtz H., Dilsizian V. Myocardial viability: survival mechanisms and molecular imaging targets in acute and chronic ischemia. Circ Res. 2017;120:1197–1212. doi: 10.1161/CIRCRESAHA.116.307898. [DOI] [PubMed] [Google Scholar]
- 27.Dilsizian V., Bacharach S.L., Beanlands R.S. ASNC imaging guidelines/SNMMI procedure standard for positron emission tomography (PET) nuclear cardiology procedures. J Nucl Cardiol. 2016;23:1187–1226. doi: 10.1007/s12350-016-0522-3. [DOI] [PubMed] [Google Scholar]
- 28.Mathew R.C., Bourque J.M., Salerno M., Kramer C.M. Cardiovascular imaging techniques to assess microvascular dysfunction. J Am Coll Cardiol Img. 2019 Oct 11 doi: 10.1016/j.jcmg.2019.09.006. [E-pub ahead of print] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Chareonthaitawee P., Beanlands R.S., Chen W. Joint SNMMI-ASNC Expert Consensus document on the role of (18)F-FDG PET/CT in cardiac sarcoid detection and therapy monitoring. J Nucl Med. 2017;58:1341–1353. doi: 10.2967/jnumed.117.196287. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Gillmore J.D., Maurer M.S., Falk R.H. Nonbiopsy diagnosis of cardiac transthyretin amyloidosis. Circulation. 2016;133:2404–2412. doi: 10.1161/CIRCULATIONAHA.116.021612. [DOI] [PubMed] [Google Scholar]
- 31.Kim J., Feller E.D., Chen W., Liang Y., Dilsizian V. FDG PET/CT for early detection and localization of left ventricular assist device infection: impact on patient management and outcome. J Am Coll Cardiol Img. 2019;12:722–729. doi: 10.1016/j.jcmg.2018.01.024. [DOI] [PubMed] [Google Scholar]
- 32.Shi S., Qin M., Shen B. Association of cardiac injury with mortality in hospitalized patients with COVID-19 in Wuhan, China. JAMA Cardiol. 2020 Mar 25 doi: 10.1001/jamacardio.2020.0950. [E-pub ahead of print] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Linde J.J., Kelbæk H., Hansen T.F. Coronary CT angiography in patients with non-ST-segment elevation acute coronary syndrome. J Am Coll Cardiol. 2020;75:453–463. doi: 10.1016/j.jacc.2019.12.012. [DOI] [PubMed] [Google Scholar]
- 34.Smulders M.W., Kietselaer B.L., Wildberger J.E. Initial imaging-guided strategy versus routine care in patients with non–ST-segment elevation myocardial infarction. J Am Coll Cardiol. 2019;74:2466–2477. doi: 10.1016/j.jacc.2019.09.027. [DOI] [PubMed] [Google Scholar]
- 35.Pontone G., Baggiano A., Conte E. “Quadruple rule out” with cardiac computed tomography in COVID-19 patient with equivocal acute coronary syndrome presentation. J Am Coll Cardiol Img. 2020 Apr 21 doi: 10.1016/j.jcmg.2020.04.012. [E-pub ahead of print] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Feuchtner G., Plank F., Mueller S. Cardiac CTA for evaluation of prosthetic valve dysfunction. J Am Coll Cardiol Img. 2017;10:91–93. [Google Scholar]
- 37.Kim I., Chang S., Hong G. Comparison of cardiac computed tomography with transesophageal echocardiography for identifying vegetation and intracardiac complications in patients with infective endocarditis in the era of 3-dimensional images. Circ Cardiovasc Imaging. 2018;11 doi: 10.1161/CIRCIMAGING.117.006986. [DOI] [PubMed] [Google Scholar]
- 38.Hendel R.C., Friedrich M.G., Schulz-Menger J. CMR first-pass perfusion for suspected inducible myocardial ischemia. J Am Coll Cardiol Img. 2016;9:1338–1348. doi: 10.1016/j.jcmg.2016.09.010. [DOI] [PubMed] [Google Scholar]
- 39.D’Angelo T., Grigoratos C., Mazziotti S. High-throughput gadobutrol-enhanced CMR: a time and dose optimization study. J Cardiovasc Magn Reson. 2017;19:83. doi: 10.1186/s12968-017-0400-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Foley J.R., Richmond C., Fent G.J. Rapid Cardiovascular Magnetic Resonance for Ischemic Heart Disease Investigation (RAPID-IHD) J Am Coll Cardiol Img. 2020 Apr 15 doi: 10.1016/j.jcmg.2020.01.029. [E-pub ahead of print] [DOI] [PubMed] [Google Scholar]
- 41.Chen J., Zhang H., Zhu D., Wang Y., Byanju S., Liao M. Cardiac MRI for detecting left atrial/left atrial appendage thrombus in patients with atrial fibrillation : Meta-analysis and systematic review. Herz. 2019;44:390–397. doi: 10.1007/s00059-017-4676-9. [DOI] [PubMed] [Google Scholar]
- 42.Kitkungvan D., Nabi F., Ghosn M.G. Detection of LA and LAA thrombus by CMR in patients referred for pulmonary vein isolation. J Am Coll Cardiol Img. 2016;9:809–818. doi: 10.1016/j.jcmg.2015.11.029. [DOI] [PubMed] [Google Scholar]