Abstract
Objective
To assess the reasons for discharge delays for children with long-term mechanical ventilation.
Study design
Charts of children (0–18 years of age) with a new tracheostomy in the Pulmonary Habilitation Program at the Ann and Robert H. Lurie Children’s Hospital of Chicago were retrospectively reviewed for demographic information, medical diagnoses, medical stability, discharge to home, reasons for discharge delay, and hours of staffed home nursing. All patients were discharged on mechanical ventilation. Discharge delay was defined as >10 days after medical stability. Hospital charges were analyzed and excess charges quantified beginning with the date of delay. Descriptive statistics and Pearson χ2 tests were used to compare nursing hours and demographics.
Results
Of 72 patients, 55% were male with mean age 1.8 years (SD 3.8) at tracheostomy placement. The most common long-term mechanical ventilation indication was chronic lung disease (n = 47, 65%); 54% had discharge delays, the majority were primarily due to lack of home nursing (62%), followed by delay of caregiver training (18%), caregiver health and social issues (8%), and delay in a transitional care facility bed (8%). Of the 39 delayed patients, 10% ($13 217 889) of hospital charges occurred during excess days with a median of $186 061 (IQR $117 661–$386 905) per patient.
Conclusions
Over one-half of children discharged to the community from a large inpatient pediatric long-term mechanical ventilation program had a nonmedical delay of discharge home, most commonly because of home nurse staffing. This case series provides further evidence that limited availability of home nursing impedes efficient discharge and prolongs hospitalizations. (J Pediatr 2019;212:166–71).
Children who require invasive long-term mechanical ventilation through a tracheostomy are increasing in number and expend 1.5 billion inpatient dollars annually.1 Because of the need for an awake and trained caregiver to support a child with long-term mechanical ventilation at all times, current guidelines support professional in-home caregivers, often in the form of private duty nursing, to provide suctioning, monitoring, and other direct healthcare tasks.2 Home care is complicated because children with long-term mechanical ventilation have high levels of comorbidities and medication use.2–4 Home care for children requiring long-term mechanical ventilation care is far less expensive than hospital-based care,5,6 with a difference as high as $14 000 per month.5,7 However, hospital length of stay can be prolonged due to obstacles related to home care, such as approval of public funding, assignment of nursing, and arranging medical foster care.8,9
Because home care is more cost effective, expeditious discharge has potentially significant economic benefit. Discharge for this population involves many factors including arranging for durable medical equipment to be sent to the home, training caregivers, home modifications, and home care nursing.10,11 However, perhaps more important than financial savings, home care has significant psychological and developmental benefit to the child and family. Long inpatient hospitalizations disrupt the family unit and have a negative impact on the development of the child.12 In addition, longer hospitalizations have been associated with negative parental outcomes such as stress, post-traumatic stress disorder, depression, and anxiety.13–16 Hospitalization also disrupts parent-child bonding.17
For all of these reasons, finding opportunities to expedite discharge is essential for quality care of this vulnerable population. Standardizing discharge processes has been shown to decrease overall length of stay without jeopardizing patient safety,18 however, it is not completely known to what extent external factors impede timely discharge. Although delays in discharges have been described generally, quantifying the impact of these delays, both in delayed hospital discharge days and increased inpatient costs, is yet unknown for the long-term mechanical ventilation population.10,19–21 Therefore, our study objective was to identify the primary cause of delay in discharge of hospitalized children with long-term mechanical ventilation, and secondarily to quantify the excess days and cost attributable to delays.
Methods
We completed a retrospective chart review of hospitalized children with long-term invasive mechanical ventilation at Ann and Robert H. Lurie Children’s Hospital of Chicago (“Lurie Children’s Hospital”) from January 2015-September 2017. Data were extracted from the medical chart, including a previously described hospital flowsheet for preparing to discharge patients with long-term mechanical ventilation.10 None of the patients in the current study overlap with those reported in our prior study. The institutional review board at Lurie Children’s Hospital approved study procedures.
Study Setting
Pediatric patients with invasive mechanical ventilation, as well as other children with medical complexity, receive coordination and resource allocation approval through the University of Illinois at Chicago Division of Specialized Care for Children (DSCC), a Title V program. The DSCC home care program focuses specifically on helping children with medical complexity successfully live in the community, including facilitating approval for in-home nursing support and durable medical equipment. Home health nurses can be registered nurses or licensed practical nurses who are trained to care for patients with tracheostomies and ventilators, in addition to their other medical needs. In Illinois, children with 24-hour ventilator needs typically are approved to receive 16–18 hours per day of home nursing, however, home nursing shortages exist throughout the state typically resulting in incomplete nurse staffing. Illinois also has 3 transitional care facilities with a total of 48 transitional care beds equipped to care for this population.
The Pulmonary Habilitation Program began at what is now Lurie Children’s Hospital in 1976. Lurie Children’s Hospital serves as the primary referral center for subspecialty pediatric care in the Chicagoland area. This program provides comprehensive services across multiple inpatient units and outpatient pulmonary clinics for children with invasive home mechanical ventilation and includes physicians, advanced practice nurses, a social worker, case management, respiratory therapist, and child life specialists. The program currently serves approximately 160 children, and its goal is to prepare families to care for their child who requires long-term invasive mechanical ventilation support in the family home or other least restrictive environment. In current practice, a best-case scenario for a child in the program requiring 24/7 invasive home mechanical ventilation is 16 hours/day of private duty nursing 7 days per week. This staffing level is almost never available. In general, the program requires a minimum of 40 hours/week to be staffed over 5 days. This requirement is modified depending on how many family caregivers are available and other social issues, such as caregiver health. In some cases, nursing agencies are unable to staff a case. For purposes of this report, “lack of home nursing” means that insufficient private duty nurse staffing is available to support a safe discharge, as determined in collaborative discussions between the DSCC care coordinator, hospital staff, and family. Children ventilated nonin-vasively are not included in this program.
Patient Identification and Demographic Characteristics
Patients of any age were eligible for the study if they were part of the program while hospitalized and had not been previously living at home with a ventilator. Patients were excluded if they were in foster care. Demographic characteristics race/ethnicity, age, and sex were collected from the medical record. In addition, the study team characterized primary diagnosis grouped into 5 categories: chronic lung disease because of prematurity, hypoxic ischemic encephalopathy/central nervous system disorders, primary neuromuscular disorders, genetic/metabolic disorders, and trauma. Number of home nursing hours, if home nursing was fully staffed, date of medical readiness to discharge, days from medical readiness to discharge, discharge location, transitional care location, and type of primary insurance also were collected and analyzed.
Delay of Discharge
For each patient, the date of medical stability for discharge was determined upon retrospective review of the medical chart by 2 reviewers who evaluated each chart independently then met and discussed each date until complete consensus was reached. For the purposes of this study, medical stability was defined as at least 1 week without any change in ventilator settings on a portable (home) ventilator, no acute illness, no active medical management, and feedings at goal for discharge. Patients preparing for discharge to home or to a transitional care facility were included. Discharge delay was defined as a discharge date greater than 10 days after a child achieved medical stability to account for the complexity of arranging for transition to home care. We used 10 days to conservatively capture excess delay of discharge and because there is no accepted standard discharge timeline. Team members completing chart review categorized reasons for delay of discharge as due to nursing (eg, inability for an agency to find available skilled nurses to fill needed shifts), caregiver health and social issues (eg, inadequate housing, health of primary caregiver, difficulty identifying a backup caregiver), lack of an available bed at a transitional care facility if this was to be the desired destination, or delay in caregiver training (eg, caregiver delayed in completing 24 hour stay in the hospital or demonstrating ability to change the tracheostomy, etc). In the case of multiple causes for delay, a primary reason was selected after chart review by multiple clinical team members who came to consensus agreement.
Nursing Hours Staffed
Medical charts were reviewed for information regarding the number of staffed nursing hours/week. We used the lower end of typical hours approved (16 hours/day) to set a conservative threshold relative in Illinois for “fully staffed nursing,” or at least 112 hours/week.
Hospital Charges
Hospital charges for each patient admission were extracted from the hospital financial department. Total and median hospitalization charges for the patients were calculated. By extracting data from the hospital financial department it was possible to assign individual charges to the day that they were billed, therefore, the total and median “excess” hospital charges were defined as the hospital charges that occurred from day 11 onward after the date of the medical stability until the date of discharge.
Statistical Analyses
Descriptive statistics were used for demographic and medical characteristics of the population. Pearson χ2 tests were used for comparisons between nursing staffing status and demographic characteristics. Hospital charges were reported as medians with IQR ranges because of non-normal distributions. Statistical analyses were completed using Stata/SE 14 and STATA 15.1 (Stata Corp, College Station, Texas).
Results
Patient Demographic Characteristics
Of the 72 children eligible for study inclusion, 55% percent were male (Table I). The mean age was 1.8 years (SD 3.8, range 0.4–18.8) at tracheostomy placement, and the majority were <1 year of age (n = 54, 75%); 33% were non-Hispanic black and 89% from English-speaking families. The most common diagnostic category was chronic lung disease because of prematurity (n = 47, 65%) with the other diagnoses as listed. This is a medically complex population of patients invasively ventilated through a tracheostomy. All patients also had an enteral feeding tube. Only 5 (7%) required less than 24/7 ventilation.
Table I.
Demographic characteristics of children enrolled in the Pulmonary Habilitation Program (N = 72)
| Demographic characteristics | n (%) |
|---|---|
| Male sex | 40 (55) |
| Age | |
| <1 y | 54 (75) |
| 1–2 y | 11 (15) |
| 3–5 y | 1 (1) |
| 6–10 y | 2 (3) |
| 11–18 y | 4 (6) |
| Race/ethnicity | |
| Non-Hispanic white | 22 (31) |
| Non-Hispanic black | 24 (33) |
| Hispanic | 20 (28) |
| Other | 6 (8) |
| Primary language | |
| English | 64 (89) |
| Spanish | 7 (10) |
| Other | 1 (1) |
| Diagnostic categories | |
| Bronchopulmonary dysplasia/chronic lung disease | 47 (65) |
| Hypoxic ischemic encephalopathy/central nervous system | 14 (19) |
| Neuromuscular disorder | 6 (8) |
| Genetic/metabolic disorder | 4 (6) |
| Trauma | 1 (1) |
Reasons for and Days of Delays in Discharge
Of the total 72 patients discharged home for the first time with a ventilator, 39 were discharged beyond 10 days after medical stability (54%). Of these 39, 24 (62%) were primarily due to lack of home nursing, 7 (18%) were due to a delay of caregiver training, 3 (8%) were due to social issues, and 3 (8%) were due to a delay in a transitional care facility bed. Two patients (5%) experienced a delay in discharge due to issues with commercial insurance approval for home nursing. The extent of delays beyond 10 days were a median (range) of 28 days (11–268) for home health nursing, 41 days (17–53) for caregiver training, 36 days (33–58) for social reasons, and 19 days (13–21) for lack of transitional care bed as the primary cause (Figure 1). The 2 cases of discharge delay attributable to insurance lead to an average of 23.5 days of excess hospitalization.
Figure 1.
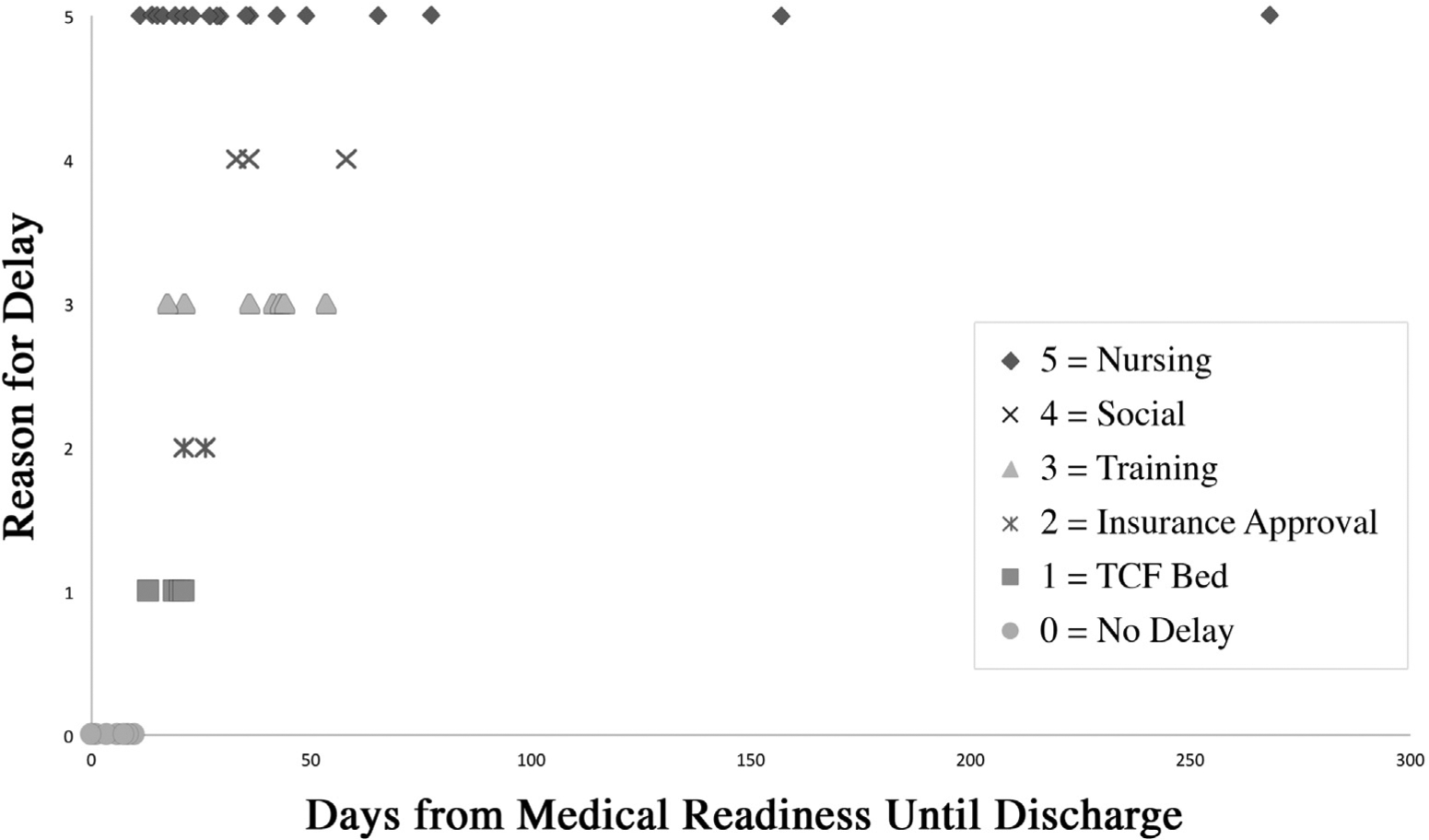
Days from medical stability to discharge by primary cause of delay.
Total hospital charges from admission date to discharge date for all patients (n = 72) were $210 637 024 with a median per patient hospitalization charge of $2 307 594 (IQR $1 272 711-$3 775 933).
Charge data for patients who experienced a delay beyond 10 days are shown in Table II. Of those 39 patients with delays in discharge, 10% ($13 217 889) of hospital charges were attributed to delay with a median excess of $186 061 (IQR $117 661–$386 905) per patient. Of the 24 patients with primary delays because of nursing, 12% ($9 330 777) of hospital charges were attributed to the delay with a median excess of $180 410 (IQR $89 079 –$362,660) per patient.
Table II.
Inpatient hospital charges for patients with long-term mechanical ventilation with delays in discharge
| Study populations | Total $ | Median $ (IQR) |
|---|---|---|
| Full cohort (N = 72) | ||
| Total hospital stay charges | $210 637 024 | $2 307 594 ($1 272 711–$3 775 933)] |
| Patients with delays (n = 39) | ||
| Total hospital stay charges | $125 936 456 | $2 699 643 ($1 694 440–$4 003 849) |
| Excess charges | $13 217 889 | $186 061 ($117 661–$386 905) |
| Patients with primary nursing delays (n = 24) | ||
| Total hospital stay charges | $79 151 780 | $3 030 423 ($1 734 007–$4 240 832) |
| Excess charges | $9 330 777 | $180 410 ($89 079–$362 660) |
Attributable Delay of Discharge for Children with Long-Term Mechanical Ventilation
Of those patients for whom hours of staffed home nursing were able to be extracted from the medical chart (n = 34), 26% had fully staffed cases and the remainder had incomplete staffing. In addition, 29% received less than one-half of the number of approved nursing hours staffed (Figure 2). Nursing staffing status (fully staffed vs not) was not associated with type of primary insurance (P = .5).
Figure 2.
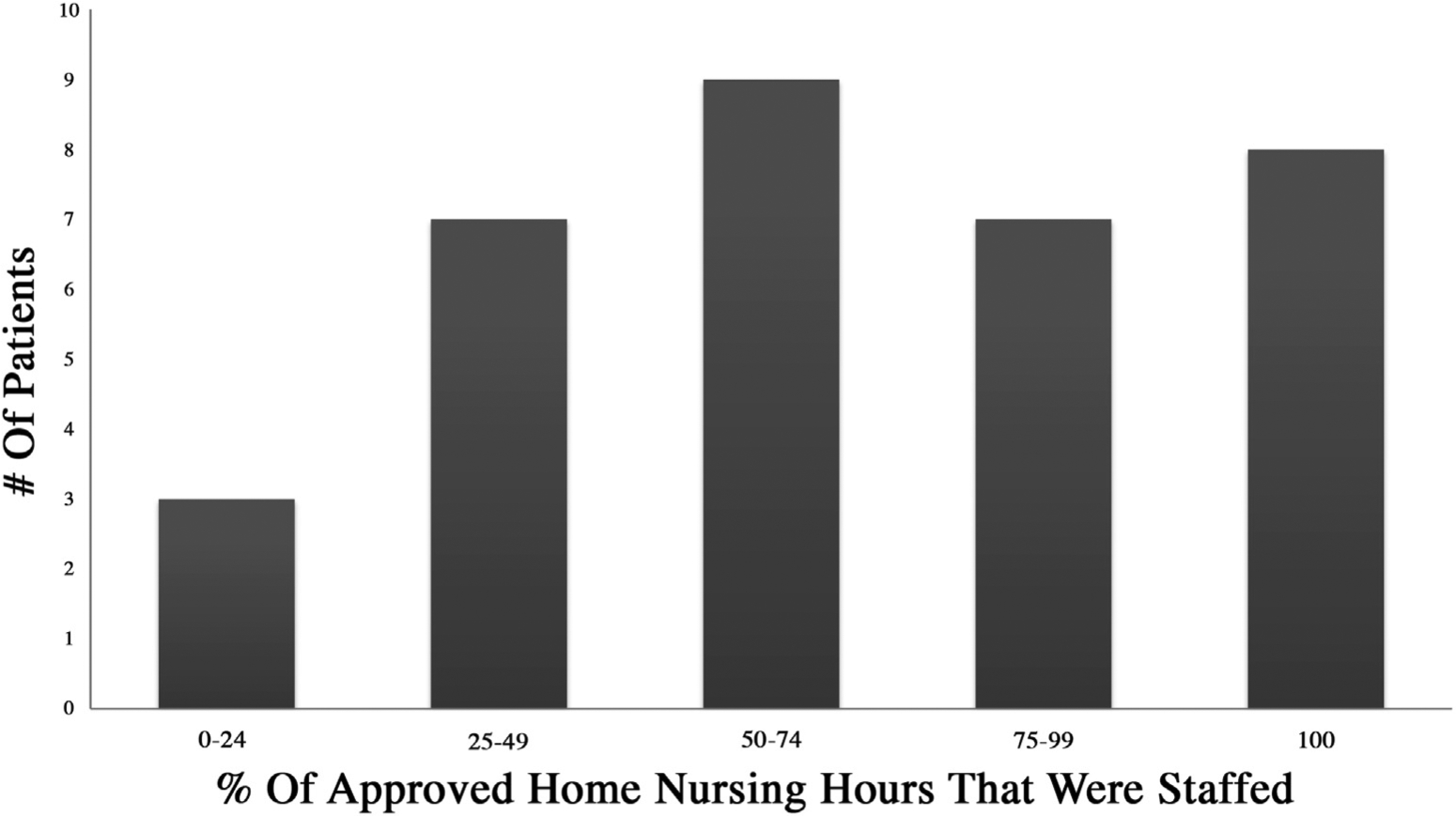
Distribution of percentage of staffed nursing hours* (n = 34). *Fully staffed nursing defined as 112 hours/week.
Discussion
In this study of children discharged for the first time to home with a ventilator from a single program in a tertiary care center, we found that over one-half of children had a nonmedical delay of discharge. Of these, 60% were due to home nursing delays. Even at the time of discharge, only 25% of children were expected to receive their full home nursing allocation to support the care of the child with long-term mechanical ventilation living at home. Notably, the 2016 American Thoracic Society guidelines described the need for an awake and trained caregiver in the home at all times. The guidelines authors describe that these recommendations were made with a very low quality of evidence.2 Furthermore, these may not be realistic goals for many locations given the home healthcare work force. Our study describes real-world practices, and we acknowledge that if the medical teams had awaited full nurse staffing for all cases before discharge, the delay of discharge would have presumably been much greater. Nevertheless, these delays contributed to increased and arguably unnecessary in-patient spending that could be potentially allocated elsewhere.
Solving the dilemma of unmet home nursing needs is not a simple challenge; home nursing shortages stem from various causes, and often persist past discharge.22 This may be due in part to the frequent shortages in the homecare workforce. Homecare nurses report job flexibility and independence as attractive factors and the amount of paperwork, overtime, and salary as issues causing dissatisfaction.23,24 In addition, as with other clinicians, compassion fatigue is experienced frequently among nurses caring for children with chronic conditions and may contribute to workforce burnout.25 However, inadequate payment for services is thought to be the primary driver of shortages in the pediatric home health workforce. In a recent Policy Statement of the American Academy of Pediatrics, The Section on Home Care, Committee on Child Health Financing propose that inadequate Medicaid payments to nursing providers, sometimes less even than the cost of providing services, are linked to prolonged hospitalizations.26 Although we did not find a relationship between insurance status and delay of discharge in our patients, we believe this may likely be because the impact of inadequate Medicaid payments to nursing providers is farther upstream, impacting the size of the homecare work force overall and therefore causing discharge delays for the full population. Also, our small study population was a majority Medicaid-insured, therefore, we may have been under powered to see differences by insurance status.
The second most common reason for delay of discharge was delay due to parent/caregiver training. Extensive parent training is essential to care for children with such complex medical needs. As a result of the enormous breadth of material that needs to be covered, it is important to begin the training as soon as possible during a child’s hospital stay.2,10 However, despite even best efforts by all parties, parent training is challenged by coordinating with busy parents who are balancing the care of a hospitalized child with employment and sibling caretaking. As programs work to prioritize family-centered care, they will need to consider how best to support parents with these competing priorities.
A medical charges analysis of children with medical complexity demonstrated that even a small decrease in the number of inpatient days may provide the savings needed to fund possibly more effective and less expensive care coordination programs.27 Although inpatient and home healthcare systems are infrequently integrated, perhaps small changes to improve hospital-to-home transition efficiency and support to the home healthcare work force would be cost effective to the healthcare system as a whole.
Our study has several limitations. First, our study may lack generalizability to a national population because it was conducted at a single institution within a single state. Practice standards likely differ between institutions, and there is great variability in home health receipt among states and regions of the US.28 Of note, the state of Illinois allows licensed practical nurses to care for children with long-term mechanical ventilation at home. Our sample also accessed the state DSCC program. However, core features of discharge challenges may likely be shared nationally; a survey of providers for children with long-term mechanical ventilation suggests that home nursing delays exist across the US.29 Second, medical stability for discharge and reasons for delay of discharge were determined retrospectively from chart review. We addressed this limitation by using a conservative definition of delay of discharge (>10 days after medical stability) and utilizing consensus chart review, however, future studies may estimate these delays more accurately by using prospective strategies. Notably, using a conservative 10 days after medical stability likely underestimates inpatient excess and the potential for improved efficiency. Also, we realize that there are interrelated factors which impact a family’s readiness for discharge. For simplicity, and in some cases to preserve anonymity of unique patient situations, we collapsed reasons for delay into larger categories such as “social” or “training.”
We were unable to access reliable financial data to evaluate direct and indirect costs, and instead analyzed charge data for this study, which likely inflates the true financial impact. Thus, although cost data is preferable, this charge data provided an opportunity to estimate the financial impact and unnecessary excess payment that occurred due to delays, especially in proportion to the overall hospital charges. Because of our overall small sample, we are cautious to over-interpret the broader application of our quantitative findings.
We would also like to acknowledge that the majority of our patients were discharged before a full cadre of nurses were obtained to staff the case. We recognize that some programs may have different discharge practices, which are highly influenced by the local ability to secure home care nursing. Although we believe that home healthcare availability likely substantially impacts child health and family well-being, assessing the adequacy of home care was not the focus of this study.
Hospitalization restricts independent functioning, school participation, and peer interaction, thus, decreasing opportunities to learn and develop. Furthermore, the exposure to stressors, and the disruption of parent-child interaction and sleep impact negatively on learning and developing.12 Certainly, it is in the best interest of the child, family, and healthcare system overall to decrease inpatient hospitalization days and promote supported days at home where a child can access community and home-based programs that promote development. The issues of nursing shortages and skilled training of lay caregivers are as complex as the children they impact. Future studies should focus on quality interventions, which effectively expedite these hospital-to-home transitions without jeopardizing patient safety or family resiliency.
Acknowledgments
S.A.S. received support from The University of Chicago Patient Centered Outcomes Research K12 Training Program (5K12HS023007) and the T73 Leadership Education in Neurodevelopmental and Related Disorders Training Program (LEND). D.G. serves as an Associate Editor for The Journal of Pediatrics. The other authors declare no conflicts of interest.
References
- 1.Benneyworth BD, Gebremariam A, Clark SJ, Shanley TP, Davis MM. Inpatient health care utilization for children dependent on long-term mechanical ventilation. Pediatrics 2011;127:e1533–41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Sterni LM, Collaco JM, Baker CD, Carroll JL, Sharma GD, Brozek JL, et al. An Official American Thoracic Society Clinical Practice Guideline: Pediatric Chronic Home Invasive Ventilation. Am J Respir Crit Care Med 2016;193:e16–35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Overman AE, Liu M, Kurachek SC, Shreve MR, Maynard RC, Mammel MC, et al. Tracheostomy for infants requiring prolonged mechanical ventilation: 10 years’ experience. Pediatrics 2013;131:e1491–6. [DOI] [PubMed] [Google Scholar]
- 4.Elias ER, Murphy NA , Council on Children with D. Home care of children and youth with complex health care needs and technology dependencies. Pediatrics 2012;129:996–1005. [DOI] [PubMed] [Google Scholar]
- 5.Fields AI, Rosenblatt A, Pollack MM, Kaufman J. Home care cost-effectiveness for respiratory technology-dependent children. Am J Dis Child 1991;145:729–33. [PubMed] [Google Scholar]
- 6.Committee on Child Health Financing SoHCAAoP. Financing of pediatric home health care. Committee on Child Health Financing, Section on Home Care, American Academy of Pediatrics. Pediatrics 2006;118:834–8. [DOI] [PubMed] [Google Scholar]
- 7.King AC. Long-term home mechanical ventilation in the United States. Respir Care 2012;57:921–30. discussion 30–2. [DOI] [PubMed] [Google Scholar]
- 8.Sobotka SA, Gaur DS, Goodman DM, Agrawal RK, Berry JG, Graham RJ. Pediatric patients with home mechanical ventilation: The health services landscape. Pediatr Pulmonol 2019;54:40–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.DeWitt PK, Jansen MT, Ward SL, Keens TG. Obstacles to discharge of ventilator-assisted children from the hospital to home. Chest 1993;103:1560–5. [DOI] [PubMed] [Google Scholar]
- 10.Sobotka SA, Hird-McCorry LP, Goodman DM. Identification of fail points for discharging pediatric patients with new tracheostomy and ventilator. Hosp Pediatr 2016;6:552–7. [DOI] [PubMed] [Google Scholar]
- 11.Maynard R, Christensen E, Cady R, Jacob A, Ouellette Y, Podgorski H, et al. Home health care availability and discharge delays in children with medical complexity. Pediatrics 2018;143:e20181951. [DOI] [PubMed] [Google Scholar]
- 12.Sobotka S, Agrawal RK, Msall ME. Prolonged hospital discharge for complex children with technology dependency: a source of healthcare disparities. Pediatr Ann 2017;46:e365–70. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Diaz-Caneja A, Gledhill J, Weaver T, Nadel S, Garralda E. A child’s admission to hospital: a qualitative study examining the experiences of parents. Intensive Care Med 2005;31:1248–54. [DOI] [PubMed] [Google Scholar]
- 14.Knoester H, Grootenhuis MA, Bos AP. Outcome of paediatric intensive care survivors. Eur J Pediatr 2007;166:1119–28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Samuel VM, Colville GA, Goodwin S, Ryninks K, Dean S. The value of screening parents for their risk of developing psychological symptoms after PICU: a feasibility study evaluating a pediatric intensive care follow-up clinic. Pediatr Crit Care Med 2015;16:808–13. [DOI] [PubMed] [Google Scholar]
- 16.Fauman KR, Pituch KJ, Han YY, Niedner MF, Reske J, LeVine AM. Predictors of depressive symptoms in parents of chronically ill children admitted to the pediatric intensive care unit. Am J Hosp Palliat Care 2011;28:556–63. [DOI] [PubMed] [Google Scholar]
- 17.Noyes J ‘Ventilator-dependent’ children who spend prolonged periods of time in intensive care units when they no longer have a medical need or want to be there. J Clin Nurs 2000;9:774–83. [Google Scholar]
- 18.Baker CD, Martin S, Thrasher J, Moore HM, Baker J, Abman SH, et al. A standardized discharge process decreases length of stay for ventilator-dependent children. Pediatrics 2016;137:1–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Edwards EA, O’Toole M, Wallis C. Sending children home on tracheostomy dependent ventilation: pitfalls and outcomes. Arch Dis Child 2004;89:251–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Graf JM, Montagnino BA, Hueckel R, McPherson ML. Children with new tracheostomies: planning for family education and common impediments to discharge. Pediatr Pulmonol 2008;43:788–94. [DOI] [PubMed] [Google Scholar]
- 21.Cross D, Leonard BJ, Skay CL, Rheinberger MM. Extended hospitalization of medically stable children dependent on technology: a focus on mutable family factors. Issues Compr Pediatr Nurs 1998;21:63–84. [DOI] [PubMed] [Google Scholar]
- 22.Hefner JL, Tsai WC. Ventilator-dependent children and the health services system. Unmet needs and coordination of care. Ann Am Thorac Soc 2013;10:482–9. [DOI] [PubMed] [Google Scholar]
- 23.Anthony A, Milone-Nuzzo P. Factors attracting and keeping nurses in home care. Home Healthcare Nurse 2005;23:372–7. [DOI] [PubMed] [Google Scholar]
- 24.Ellenbecker CH. A theoretical model of job retention for home health care nurses. J Adv Nurs 2004;47:303–10. [DOI] [PubMed] [Google Scholar]
- 25.Maytum JC, Heiman MB, Garwick AW. Compassion fatigue and burnout in nurses who work with children with chronic conditions and their families. J Pediatr Health Care 2004;18:171–9. [DOI] [PubMed] [Google Scholar]
- 26.Simpser E, Hudak ML , Section On Home Care COCHF. Financing of pediatric home health care. Pediatrics 2017;139:834–8. [DOI] [PubMed] [Google Scholar]
- 27.Berry JG, Hall M, Neff J, Goodman D, Cohen E, Agrawal R, et al. Children with medical complexity and Medicaid: spending and cost savings. Health Aff (Millwood) 2014;33:2199–206. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Berry JG, Hall M, Dumas H, Simpser E, Whitford K, Wilson KM, et al. Pediatric hospital discharges to home health and postacute facility care: A national study. JAMA Pediatr 2016;170:326–33. [DOI] [PubMed] [Google Scholar]
- 29.Sobotka SA, Gaur DS, Goodman DM, Agrawal RK, Berry JG, Graham RJ. Pediatric patients with home mechanical ventilation: the health services landscape. Pediatr Pulmonol 2019;54:40–6. [DOI] [PMC free article] [PubMed] [Google Scholar]


