Abstract
If the presence of a goiter causes airway deformities in the supraglottic and infraglottic areas, difficult airway should be considered and airway evaluation including physical examination, radiologic studies, and indirect laryngoscopy should be preoperatively performed to determine the airway management plan. Various methods such as direct laryngoscopy, videolaryngoscopy, awake fiberoptic intubation, tracheostomy, and extracorporeal membrane oxygenation support have been reported to secure the airway. In most previously reported goiter cases, the upper airway patency was well maintained and the endotracheal tube was easily passed even when there was severe tracheal narrowing and deviation. We describe a case of successful combined use of videolaryngoscopy and fiberoptic bronchoscopy for advancement of an endotracheal tube through a narrow trachea due to the presence of a huge goiter.
Keywords: Bronchoscopes, goiter, intubation, thyroid, tracheostomy
Introduction
A goiter is defined as an enlarged thyroid gland. If it is sufficiently large to be accompanied by distorted upper airway or tracheal compression with deviation, cautious airway management should be planned.1,2 Various methods are selectively used depending on operator skill, patient condition, and equipment availability such as direct laryngoscopy, videolaryngoscopy, and awake fiberoptic intubation.3–5 The effects of tracheal deviation and compression on tube advancement remain controversial.4 Here, we experienced a case where tracheal compression and deviation caused by a goiter interfered with tube advancement. The patient was successfully treated with videolaryngoscopy and fiberoptic bronchoscopy.
Case
A 59-year-old, 43 kg, 146 cm, female patient was admitted to the Department of Otolaryngology–Head and Neck Surgery for the treatment of a 5 × 5.5 × 6 cm3 multinodular goiter suspected of tracheoesophageal and internal jugular vein invasion. Biopsies of the esophagus and thyroid lesion were preoperatively performed, and a rare pathologic diagnosis of Hurthle cell cancer was suspected. After deciding that surgical treatment was required, major surgery involving otorhinolaryngology, cardiothoracic, and cardiovascular surgeons was planned.
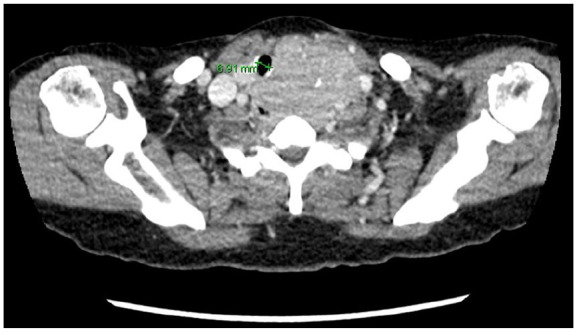
Preoperatively, the thyromental distance was greater than three finger breadths,6 the Mallampati score was 2,7 and there was no head and neck motion limitation.6 Furthermore, it was confirmed that the airway was intact up to the glottis level. However, chest radiography and neck computed tomography showed marked narrowing of the trachea, along with deviation to the right (Figures 1 and 2). It was apparent that careful anesthetic planning was crucial to minimize unexpected difficulties during intubation.
Figure 1.

Neck CT showing tracheal deviation.
Figure 2.
Neck CT showing tracheal narrowing.
In the operating room, standard monitoring revealed an initial arterial pressure of 196/92 mmHg, heart rate of 78 beats/min, and peripheral oxygen saturation (SpO2) of 97% while breathing room air. General anesthesia was induced using 150 mg propofol and 0.05–0.1 μg/kg/min remifentanil. After confirming loss of consciousness and adequate mask ventilation, 50 mg rocuronium was injected. To protect the recurrent laryngeal nerve, the surgeon requested that an electromyographic endotracheal tube be used for intubation. The duty anesthesiologist anticipated intubation difficulty and performed the first attempt using a videolaryngoscope (Glidescope®; GVL Verathon Inc., WA). The glottis was easily located, and an electromyographic endotracheal tube (ID 7.0) (Medtronic Inc., Jacksonville, FL) was inserted through the vocal cords. However, the endotracheal tube could not be advanced into the trachea even with the rotation tube maneuver, and the tip was stuck just under the vocal cords. Mask ventilation was restarted, and the duty anesthesiologist enlisted the help of an airway expert. The ID 7.0 electromyographic endotracheal tube was suspected to be too large for the narrowed trachea, and use of the smaller-sized ID 6.0 was attempted. The tube was inserted through the glottis using the videolaryngoscope; however, the tube became stuck with severe resistance and could not advance over 18 cm depth. The endotracheal-tube advancement was stopped, and mechanical ventilation started after ballooning the cuff. A flexible fiberoptic bronchoscope (LF-GP; Olympus, Tokyo, Japan) with an outer diameter of 3.8 mm was inserted into the lumen of the endotracheal tube, and compression of the tracheal lumen in crescent shape was seen at the tip of the tube. The bronchoscope was advanced gently through the narrowed trachea and placed near the carina, and the endotracheal tube was successfully advanced, guided by the bronchoscope, and fixed at 22 cm depth. Mechanical ventilation was initiated after confirming the appropriate position of the tube with the bronchoscope.
The otorhinolaryngology surgeon performed total thyroidectomy, lymph-node dissection, total laryngectomy with mediastinal tracheostomy, and reconstruction with pectoralis major myocutaneous flap. The cardiothoracic surgeon performed partial esophagectomy, partial sternum resection, and reconstruction. The total anesthetic time was 745 min, and the operation duration, 530 min. The patient was transferred to the intensive care unit with tracheostomy and remained sedated for 1 day. She was moved to the general ward 6 days postoperatively and discharged 36 days postoperatively.
Discussion
Previous studies have reported intubation attempts with various methods in patients with goiter, one of them being awake fiberoptic intubation. However, previous reports have shown that attempts using awake fiberoptic intubation alone fail in 12%–16% of patients with goiter,3,4 and such patients could be successfully intubated using direct laryngoscopy or videolaryngoscopy after intravenous induction4 because awake fiberoptic intubation requires patient cooperation, and topicalization may intensify respiratory depression. Total obstruction of the airway by fiberoptic bronchoscopy in patients with stridor due to partial airway obstruction may cause desaturation, which may further distress the patient.3 Moreover, a clear laryngeal view can be easily attained by direct laryngoscopy or videolaryngoscopy because goiters usually do not affect the upper airway patency from the mouth to the vocal cords.4 In other words, if the airway difficulty caused by the goiter is limited to the infraglottic area, a technique requiring complex skills such as awake fiberoptic intubation can interfere with securing the airway by complicating access to the supraglottic area, and additional experienced personnel may be required who can apply airway-clearing maneuvers such as jaw thrust and lingual traction.8
Therefore, when preparing an airway-management plan for a patient with a goiter, it is recommended to consider the location (supraglottic, infraglottic, or both) of airway difficulties that will be encountered. Here, the airway difficulty was only expected to be infraglottic. Therefore, direct laryngoscopy may appear a reasonable choice, similar to videolaryngoscopy, regarding approaching the glottis.9 However, in our case, the videolaryngoscope was used in the first intubation attempt because it has a camera at the end of the blade, allowing better vocal-cord viewing, particularly in difficult airways, and not all laryngoscopy-related complications can be anticipated even if the preoperative airway assessment is normal.10 Furthermore, videolaryngoscopy may provide prompt assistance to the operator when performing external laryngeal manipulation or changing the stylet angle because the assistant can view the screen.11 In addition, an electromyographic tube can be closely aligned to the vocal cords with a videolaryngoscope, enabling optimal monitoring of the nerve.3,12
Recently, videolaryngoscopy and fiberoptic bronchoscopy have been used simultaneously to improve the success rate of difficult tracheal intubation.13–16 In this combined videolaryngoscopy with fiberoptic bronchoscopy approach, videolaryngoscopy is used to displace the soft palate and tongue from the posterior pharyngeal wall, clearing the upper airway and facilitating tube passage over the fiberoptic bronchoscope.17,18 Here, intubation was successfully performed using this combined videolaryngoscopy with fiberoptic bronchoscope technique after induction. However, the approach was different in terms of the location of the lesion to be overcome. In our case, there was no complication of supra/infraglottic pathology that would obstruct the access of the fiberoptic bronchoscope to the vocal cords, and the videolaryngoscope had an accessory role; the fiberoptic bronchoscope was locally used to resolve the infraglottic tracheal deviation after easily accessing the glottis with the videolaryngoscope. In this case, an acute angle-blade videolaryngoscope was used to locate the vocal cords, mount the endotracheal tube on the glottis, and use a fiberoptic bronchoscope to advance the tube. We encountered difficulty passing the endotracheal tube due to tracheal deviation, contrary to previous reports showing that there was no difficulty in passing the tube through a compressed or narrowed trachea.2 This inconsistency may be because of the shorter tracheal length in Asian women, more acutely angled tracheal deviation, and the larger outer diameter of the electromyographic tube.12 A fiberoptic bronchoscope can be advantageously used as a central axis for tube advancement. The advantages of the fiberoptic bronchoscope are: sufficient rigidity to pass beyond the tracheal deviation or narrowing site caused by the movable adjacent organ, sufficient flexibility to avoid causing major trauma to the trachea, and visibility of the distal lens to ensure that the tube tip is properly advanced along the trachea and positioned above the carina after completing tube advancement. The role of the fiberoptic bronchoscope in our case may seem similar with the frova introducer, commonly used as a guide to overcome the acute angle axis of anterior airway when using videolaryngoscopy,19 although this frova technique is blind and focused on resolving supraglottic airway deformity. Here, we used an LF-GP bronchoscope with outer diameter 3.8 mm, rather than a smaller fiberoptic bronchoscope, because as the size difference between the endotracheal tube increases, there is a risk of impingement and damage to the surrounding tissue such as the tracheal wall.18
If there are findings suggesting difficult intubation involving the supraglottic area, such as limited mouth opening or neck extension, and Mallampati score 4 in preoperative airway examinations, awake fiberoptic intubation should be considered.20 Invasive intubation methods such as awake tracheostomy can be selected if the oral approach is estimated to be very risky because the larynx is swollen and displaced or if there is tumor invasion to the trachea.21 However, tracheostomy may be very difficult due to an enlarged thyroid mass, distorted anatomy of the trachea, and bleeding tendency. In our case, normal upper airway was estimated based on the preoperative airway assessment, and awake fiberoptic intubation or awake tracheostomy was not considered in the intubation plan. Extracorporeal membrane oxygenation (ECMO) can be placed before anesthesia induction if critical airway narrowing due to tracheal invasion exists.22,23 A case of veno-arterial ECMO in a patient with goiter and severe rheumatoid arthritis, with failure to move the cervical spine and limited mouth opening was reported.24 Therefore, careful preoperative assessment and planning are essential to selecting safe airway management methods for patients with goiter. Here, unexpected difficulty of tube advancement in an infraglottic lesion was encountered, although the preoperative assessment results suggested normal upper airway, and it was not anticipated that tube advancement would be difficult based on the previous literature showing a lack of association between tracheal compression/deviation and intubation difficulty.4 Meanwhile, a recent report suggested that human error such as judgment deficiency and inadequate planning remained the main cause of intubation failure.25 Therefore, when we anesthetize patients with goiter, a multidisciplinary team approach including airway experts and ENT physicians with clear communication and backup planning should be recommended.26
Conclusion
In our patient with thyroid goiter, the use of videolaryngoscopy combined with flexible fiberoptic bronchoscopy successfully secured the airway by visualizing the glottis and facilitating passage of the tube. Preoperative airway assessment is needed for clinical planning. Assessments including physical examination, symptom assessment, radiologic imaging, and laryngoscopy can be considered to guarantee more stable and safe airway management.
Footnotes
Declaration of conflicting interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Ethical approval: Ethical approval to report this case was obtained from the institutional review board (IRB) of Severance Hospital and Yonsei University Health System (IRB no. 4-2019-0474).
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
Informed consent: Written informed consent was obtained from the patient for their anonymized information to be published in this article.
ORCID iD: Hyun Joo Kim  https://orcid.org/0000-0003-1963-8955
https://orcid.org/0000-0003-1963-8955
References
- 1. Amathieu R, Smail N, Catineau J, et al. Difficult intubation in thyroid surgery: myth or reality? Anesth Analg 2006; 103: 965–968. [DOI] [PubMed] [Google Scholar]
- 2. Bouaggad A, Nejmi SE, Bouderka MA, et al. Prediction of difficult tracheal intubation in thyroid surgery. Anesth Analg 2004; 99(2): 603–606. [DOI] [PubMed] [Google Scholar]
- 3. Gilfillan N, Ball CM, Myles PS, et al. A cohort and database study of airway management in patients undergoing thyroidectomy for retrosternal goitre. Anaesth Intensive Care 2014; 42(6): 700–708. [DOI] [PubMed] [Google Scholar]
- 4. Loftus PA, Ow TJ, Siegel B, et al. Risk factors for perioperative airway difficulty and evaluation of intubation approaches among patients with benign goiter. Ann Otol Rhinol Laryngol 2014; 123(4): 279–285. [DOI] [PubMed] [Google Scholar]
- 5. Cook TM, Morgan PJ, Hersch PE. Equal and opposite expert opinion. Anaesthesia 2011; 66(9): 828–836. [DOI] [PubMed] [Google Scholar]
- 6. Crawley SM, Dalton AJ. Predicting the difficult airway. BJA Education 2015; 15: 253–257. [Google Scholar]
- 7. Samsoon GL, Young JR. Difficult tracheal intubation: a retrospective study. Anaesthesia 1987; 42(5): 487–490. [DOI] [PubMed] [Google Scholar]
- 8. Durga VK, Millns JP, Smith JE. Manoeuvres used to clear the airway during fibreoptic intubation. Br J Anaesth 2001; 87(2): 207–211. [DOI] [PubMed] [Google Scholar]
- 9. Lewis SR, Butler AR, Parker J, et al. Videolaryngoscopy versus direct laryngoscopy for adult patients requiring tracheal intubation. Cochrane Database Syst Rev 2016; 11: CD011136. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Roth D, Pace NL, Lee A, et al. Bedside tests for predicting difficult airways: an abridged Cochrane diagnostic test accuracy systematic review. Anaesthesia 2019; 74(7): 915–928. [DOI] [PubMed] [Google Scholar]
- 11. Watt S, Kalpan J, Kolli V. Case report of the use of videolaryngoscopy in thyroid goiter masses: an airway challenge. Int J Surg Case Rep 2016; 27: 119–121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Berkow L, Dackiw AP, Tufano RP. Use of the GlideScope for placement of a recurrent laryngeal nerve monitoring endotracheal tube. J Clin Anesth 2011; 23(1): 81–83. [DOI] [PubMed] [Google Scholar]
- 13. Sharma D, Kim LJ, Ghodke B. Successful airway management with combined use of Glidescope videolaryngoscope and fiberoptic bronchoscope in a patient with Cowden syndrome. Anesthesiology 2010; 113(1): 253–255. [DOI] [PubMed] [Google Scholar]
- 14. Gómez-Ríos MA, Nieto Serradilla L. Combined use of an Airtraq® optical laryngoscope, Airtraq video camera, Airtraq wireless monitor, and a fibreoptic bronchoscope after failed tracheal intubation. Can J Anaesth 2011; 58: 411–412. [DOI] [PubMed] [Google Scholar]
- 15. Greib N, Stojeba N, Dow WA, et al. A combined rigid videolaryngoscopy-flexible fibrescopy intubation technique under general anesthesia. Can J Anaesth 2007; 54(6): 492–493. [DOI] [PubMed] [Google Scholar]
- 16. Lenhardt R, Burkhart MT, Brock NG, et al. Is video laryngoscope-assisted flexible tracheoscope intubation feasible for patients with predicted difficult airway? A prospective, randomized clinical trial. Anesth Analg 2014; 118(6): 1259–1265. [DOI] [PubMed] [Google Scholar]
- 17. Stacey MR, Rassam S, Sivasankar R, et al. A comparison of direct laryngoscopy and jaw thrust to aid fibreoptic intubation. Anaesthesia 2005; 60(5): 445–448. [DOI] [PubMed] [Google Scholar]
- 18. Asai T, Shingu K. Difficulty in advancing a tracheal tube over a fibreoptic bronchoscope: incidence, causes and solutions. Br J Anaesth 2004; 92: 870–881. [DOI] [PubMed] [Google Scholar]
- 19. Ciccozzi A, Angeletti C, Guetti C, et al. GlideScope and Frova introducer for difficult airway management. Case Rep Anesthesiol. Epub ahead of print 7 August 2013. DOI: 10.1155/2013/717928. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Kaur H, Kataria AP, Muthuramalingapandian M, et al. Airway considerations in case of a large multinodular goiter. Anesth Essays Res 2017; 11(4): 1097–1100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Hohn A, Kauliņš T, Hinkelbein J, et al. Awake tracheostomy in a patient with stridor and dyspnea caused by a sizeable malignant thyroid tumor. Clin Case Rep 2017; 5: 1891–1895. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Liou JY, Chow LH, Chan KH, et al. Successful anesthetic management of a patient with thyroid carcinoma invading the trachea with tracheal obstruction. J Chin Med Assoc 2014; 77(9): 496–499. [DOI] [PubMed] [Google Scholar]
- 23. De Piero ME, Fontana D, Quaglino F, et al. Extracorporeal membrane oxygenation (ECMO)-assisted surgery for mediastinal goiter removal. J Cardiothorac Vasc Anesth 2018; 32(1): 448–451. [DOI] [PubMed] [Google Scholar]
- 24. Shao Y, Shen M, Ding Z, et al. Extracorporeal membrane oxygenation-assisted resection of goiter causing severe extrinsic airway compression. Ann Thorac Surg 2009; 88(2): 659–661. [DOI] [PubMed] [Google Scholar]
- 25. Joffe AM, Aziz MF, Posner KL, et al. Management of difficult tracheal intubation: a closed claims analysis. Anesthesiology 2019; 131(4): 818–829. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Frerk C, Mitchell VS, McNarry AF, et al. ; Difficult Airway Society intubation guidelines working group. Difficult Airway Society 2015 guidelines for management of unanticipated difficult intubation in adults. Br J Anaesth 2015; 115: 827–848. [DOI] [PMC free article] [PubMed] [Google Scholar]


