Abstract
Family members are the primary source of support for older adults with chronic illness and disability. Thousands of published empirical studies and dozens of reviews have documented the psychological and physical health effects of caregiving, identified caregivers at risk for adverse outcomes, and evaluated a wide range of intervention strategies to support caregivers. Caregiving as chronic stress exposure is the conceptual driver for much of this research. We review and synthesize the literature on the impact of caregiving and intervention strategies for supporting caregivers. The impact of caregiving is highly variable, driven largely by the intensity of care provided and the suffering of the care recipient. The intervention literature is littered with many failures and some successes. Successful interventions address both the pragmatics of care and the emotional toll of caregiving. We conclude with both research and policy recommendations that address a national agenda for caregiving.
Keywords: caregiving, risk factors, health effects, interventions, roles, prevalence
1. INTRODUCTION
Family caregivers are relatives, friends, partners, or neighbors who provide assistance, typically unpaid, to someone who has limitations in their physical, mental, or cognitive functioning. Caregivers represent a broad and diverse group of individuals. They span all ages and are heterogeneous across multiple dimensions, including their relationship and geographical proximity to the person for whom they provide care and the nature, duration, and intensity of assistance that they provide. Caregivers also vary in their level of competence, skill, and motivation to provide assistance.
Caregiving is not a new role for family members. People have always provided emotional, physical, and financial support to family members and others that they feel close to; what has changed in the past three decades is the number of individuals who take on this role, the duration and intensity of care provided, and the complexity of the care delivered. The aging of the population, increased longevity of older adults with significant chronic disease and disability, and an underfunded and fragmented health and social support system have all contributed to placing the major burden of care on family members. Caregivers provide a valued service to family members and society, but sometimes at great cost to themselves.
2. WHY PSYCHOLOGISTS ARE INTERESTED IN CAREGIVING
Although caregiving has become a major public health issue of interest to researchers in many different disciplines, for psychologists, interest in this topic was initially motivated by its potential as a research platform for investigating diverse social psychological phenomena. First, caregiving can be viewed as a chronic stress exposure paradigm. For many individuals, being exposed to and supporting a family member with disabling chronic illness is a major stressor. It is persistent, extending over months and often years. It is typically unpredictable and often uncontrollable and in some cases requires high levels of vigilance. It generates physical and psychological strain with little opportunity for adaption, and it has the capacity to generate secondary stressors in multiple life domains. Second, caregiving incorporates numerous life transitions of interest to psychologists, including the onset and progression of illness and disability, bereavement, and institutionalization. Third, caregiving provides a context for the application of multiple theoretical perspectives, such as stress-coping theory, helping behavior, altruism, emotion regulation, and various therapeutic treatment models such as cognitive behavioral therapy (CBT). Fourth, caregiving lends itself to many different levels of analysis and methodological approaches. At the macro level, one can study the effects of health and social system changes and their impact on caregiver and care recipient outcomes; one can also do population-based longitudinal studies to assess the impact of increasing and decreasing levels of caregiving stress exposure, identify risk factors for adverse outcomes, and assess the effects of institutionalization and bereavement. Finally, this topic also lends itself to the investigation of psychobiological processes associated with stress exposure and the application of therapeutic intervention methods to mitigate negative stress effects. All of these perspectives and methods are represented in the thousands of studies that have been published on caregiving over the past four decades.
3. PREVALENCE OF ELDER CAREGIVING
There are three distinct groups receiving informal care, roughly defined by the age of the care recipients: children with chronic illness and disability who are typically cared for by young adult parents; adult children suffering from conditions such as mental illness who are cared for by middle-aged parents; and older individuals who are cared for by their spouses or their middle-aged children. Each of these populations poses unique challenges to caregivers given the variability in health conditions, symptomatology, health and social service support systems, and the life course stage of the care recipient and caregiver. Our focus in this review is on caregivers of older adults, who are by far the most common recipients of health-related caregiving.
There are no exact estimates of the number of informal caregivers in the United States. Prevalence estimates vary widely depending on definitions used and populations sampled. At one extreme are estimates that 18.2% of the US adult population, or 43.5 million Americans, provided unpaid care to an adult relative in 2015, with the majority (34.2 million) of this care being delivered to people age 50 or older (Natl. Alliance Caregiv. & AARP Public Policy Inst. 2015). At the other extreme, data from the National Long-Term Care Survey suggest that as few as 2.7 million informal caregivers provided instrumental activities of daily living (IADL) or activities of daily living (ADL) assistance to people age 65 or older. Intermediate estimates of 17.7 million caregivers of persons age 65 or older are reported by the National Health and Aging Trends Study (NHATS) and the National Survey of Caregivers (NSOC) (Freedman et al. 2011). A review of eight nationally representative surveys found published estimates ranging in magnitude from 2.7 to 36.1 million informal caregivers providing care to older disabled adults (Giovannetti & Wolff 2010).
These differences are in part attributable to when the data were collected, the age range of the population sampled, the reference period used (1 month versus 12 months), and care recipient populations targeted, but most importantly to the definition of caregiving. Thus, the high-end estimates are generated when broad and inclusive definitions of caregiving are used [e.g., unpaid care provided during the past 12 months may include helping with personal needs or household chores, managing a person’s finances, arranging for outside services, or visiting regularly to see how they are doing (Natl. Alliance Caregiv. & AARP Public Policy Inst. 2015)]. Low-end estimates are generated when definitions require the provision of specific ADL or IADL assistance (e.g., Wolff & Kasper 2006). Intermediate estimates are generated when coordination of medical care and nursing or medical tasks are included in addition to specific ADL or IADL assistance. In the NHATS and NSOC surveys, for example, persons age 65 and older are first asked about their need for help with self-care (ADL), mobility, and household tasks (IADL) and are then asked who provides that help. The helpers (i.e., caregivers) are then asked about additional help provided with transportation, medical care activities, and interactions with the health care system and providers on behalf of the care recipient. A related issue is that definitions of caregiving do not clearly distinguish caregiving for chronic disability from caregiving for acute care episodes that might follow a hospitalization event. However, most definitions emphasize chronic disability; intermittent episodes of caregiving are not well represented in the existing data or published literature. Why is getting the right prevalence estimates important? Assuming that policies that call for increased support and recognition of family caregivers have costs associated with them, the prevalence number is one of the major drivers of the financial impact of caregiver policy at national and state levels.
Women have always made up the majority of the nation’s caregivers (Natl. Alliance Caregiv. & AARP Public Policy Inst. 1997, 2004, 2009, 2015; Penrod et al. 1995; Pinquart & Sörensen 2006; Yee & Schulz 2000), although some evidence shows that men are assuming increasing roles in caregiving (Natl. Alliance Caregiv. & AARP Public Policy Inst. 2015, Spillman & Pezzin 2000), especially in the lesbian, gay, bisexual, and transgender community (Grossman et al. 2007, Hughes & Kentlyn 2011). In 2011, roughly 62% of NSOC caregivers were women.
Same-generation caregivers (usually an older adult’s spouse) have different physical and cognitive capabilities and commitment to caregiving than next-generation caregivers (usually an older adult’s children). Because same-generation caregivers of older adults are older than next-generation caregivers, they are at a higher risk of age-related physical and cognitive declines, including chronic illness and some level of disability. Same-generation caregivers are also more likely to feel that caregiving is an obligation. A recent study found that 60% of spousal caregivers reported having no choice in taking on the caregiving role, while 51% of adult children reported having no choice (Schulz et al. 2012).
4. CAREGIVING ROLES
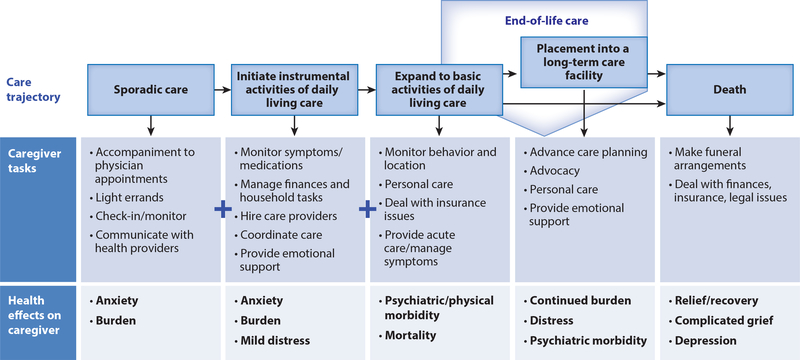
Although the caregiving role varies widely in terms of its inception and progression depending on the type and precipitating cause of disability (e.g., dementia, stroke, cancer), a prototypical longitudinal trajectory for older adult caregivers is illustrated in Figure 1. The trajectory begins with emerging awareness on the part of the caregiver that there is a problem, necessitating sporadic assistance including taking the care recipient to medical appointments, communicating with health care providers, and monitoring care recipient functioning. Over time this evolves into increasing care needs, which require assistance with household tasks (e.g., monitoring symptoms and medications, hiring care providers, coordinating care, providing emotional support) and then self-care tasks (e.g., helping with dressing, ambulating in the home, dealing with insurance, managing symptoms). End-of-life care may involve placement into a long-term care facility or enrollment in a hospice program. Note that the progression of tasks for the caregiver is cumulative. With increasing care recipient disability and need for care, the caregiver’s role becomes more labor and time intensive, more complex, and increasingly stressful. For stroke caregivers, the trajectory may begin with sudden intensity, followed by some recovery and long periods of stability, while for cancer caregivers, transitions may occur in rapid succession, each having its own learning curve as the patient moves from one treatment modality to another.
Figure 1:
Chronic disease care trajectory: caregiver tasks and health effects. Note that caregiver tasks are additive over time from the early to the late stages of a caregiving career. Figure adapted with permission from Schulz & Tompkins (2010).
Despite the unique nature of any given caregiver’s role over time, broad domains of activity characterize family caregiving. Caregiving ranges from assistance with daily activities and providing direct care to the care recipient to navigating complex health care and social service systems. The domains of the caregiving role include: assistance with household tasks, self-care tasks, and mobility; provision of emotional support; maintaining social connections; health and medical care; advocacy and care coordination; and surrogacy. Each domain has multiple tasks and activities. Cutting across these domains are ongoing cognitive and interpersonal processes in which caregivers engage, including, for example, continual problem solving, decision making, communicating with others (family members and health and human services professionals), and vigilance over the care recipient’s well-being. How caregivers manage these tasks depends on their own health status, values, preferences, knowledge, skills, and quality of relationship with the care recipient, as well as the accessibility, affordability, and adequacy of health care, long-term services and supports, and other resources (Schulz & Eden 2016).
Family involvement in health and medical tasks at home is not new, but it has become more common and is often far more complex than in the past. Older adults’ homes have become de facto clinical care settings where caregivers are performing an array of nursing or medical tasks once provided only by licensed or certified professionals in hospitals and nursing homes (Reinhard & Feinberg 2015, Reinhard et al. 2012). This also often involves interaction with complex medical technologies. This shift in the caregiver roles is, in part, the result of ongoing efforts to shorten lengths of hospitalizations and reduce nursing home placements, coupled with increasingly complex options for the medical treatment of chronic and acute conditions in noninstitutional settings.
5. IMPACT OF CAREGIVING
The effects of caregiving are both wide ranging and highly individualized. Caregivers are potentially at increased risk for adverse effects on their well-being in virtually every aspect of their lives, ranging from their health and quality of life to their relationships and economic security. Caregivers also find benefit in caregiving. Helping care recipients often instills confidence in caregivers, teaches them how to deal with difficult situations, makes them feel closer to the care recipient, and assures them that the care recipient is receiving quality care. However, the actual consequences for individual caregivers are variable, depending on a host of individual and contextual characteristics.
Overall, the body of evidence on negative effects is far larger than that on positive effects, as researchers have sought to assess the public health implications of caregiving and identify vulnerable at-risk caregivers (Schulz & Eden 2016). Documenting the adverse effects of family caregiving on both caregivers and care recipients is a requisite first step in developing interventions and public policy to address the needs of caregivers.
5.1. Psychological Distress
A large and robust literature documents higher rates of psychological distress (e.g., anxiety or depressive symptoms) among caregivers compared with noncaregiver comparison groups. Evidence has been steadily accumulating during the 20 years that have elapsed since one of the earliest reviews by Schulz and associates (1995) and now includes a vast number of individual clinical studies, multiple systematic reviews (e.g., Cuijpers 2005, Pinquart & Sörensen 2003), and an increasing number of population-based epidemiological studies (Capistrant 2016, Wolff et al. 2016). Much of this literature is based on cross-sectional studies in which caregivers are compared to comparable noncaregivers. Since matching is always imperfect, these studies raise questions about the net effect of caregiving as opposed to selection biases that may be associated with caregiver outcomes. For example, shared lifestyle factors in married couples would predict that disability and psychological distress in one partner is associated with similar characteristics in the other. Thus, an outcome attributed to caregiving such as depression may be a reflection of underlying vulnerabilities shared by both partners (Roth et al. 2015). A more compelling case for the causal relationship between caregiving and psychological distress can be made from longitudinal studies in which individuals are followed into, throughout, and out of the caregiving role. These studies demonstrate significant declines in well-being as the person enters the caregiving role, further deterioration in well-being as care demands increase, and recovery after the care recipient dies (Beach et al. 2000, Dunkle et al. 2014, Hirst 2005, Kurtz et al. 1995, Schulz et al. 2003). Intervention studies showing improvement in caregiver health and well-being when caregiving needs are addressed also support causal connections between caregiving and well-being outcomes.
5.2. Physical Health
A variety of indicators have been used to assess the physical health of caregivers, including global health status indicators, physiological measures, and health behaviors. Global health status indicators include standardized self-assessment tools such as health-related quality of life; chronic conditions; physical symptoms (e.g., Cornell Medical Index); mortality; and health service use, including clinic visits, physician or nurse practitioner visits, and days in the hospital (Schulz & Sherwood 2008).
The diversity of methods and instruments used to measure caregiver health makes cross-study comparisons and meta-analyses difficult (Grady & Rosenbaum 2015). The methodological rigor of studies that assess impacts on the physical health of caregivers is often limited by small study sample sizes, inadequate comparison or control groups, and insufficient timelines for longitudinal assessments, as well as weak statistical methods (Cameron & Elliott 2015, Grady & Rosenbaum 2015). Thus, caution is advised to avoid overattributing negative health outcomes to the effects of caregiving. The physical health status and outcomes for caregivers may be relatively independent of the caregiving role or related to individual characteristics that existed prior to assuming the caregiving role, such as socioeconomic status, health habits, and prior illness (Brown & Brown 2014, Robison et al. 2009, Roth et al. 2015, Schulz & Sherwood 2008). Nevertheless, the data support the conclusion that at least some caregivers are at risk for adverse health outcomes (Capistrant 2016).
5.3. Biomarkers
Biological indicators include a broad array of measures aimed at assessing physiological markers that are thought to be responsive to chronic stress exposure and affect subsequent illness and disease. These markers include measures of stress hormones and neurotransmitters such as cortisol, epinephrine, and norepinephrine; measures of immunologic function such as natural killer cell activity and healing response to a standardized skin puncture wound (wound healing); antibody markers such as vaccination response; cardiovascular markers such as blood pressure and heart rate; and metabolic markers such as insulin, transferrin, and plasma lipids (Allen et al. 2017, Vitaliano et al. 2003). These markers have been studied primarily in case control studies comparing stressed dementia caregivers with demographically similar noncaregiving controls. In a meta-analysis of the literature in this area, Vitaliano and associates (2003) found moderately sized statistically significant differences between dementia caregivers and controls, indicating more adverse effects among dementia caregivers. Subsequent studies have shown an increased risk of cardiometabolic changes and increased Framingham Coronary Heart Disease Risk Scores in dementia caregivers, as well as proinflammatory changes and accelerated aging of the immune system (i.e., telomere erosion) (Allen et al. 2017, Damjanovic et al. 2007, Haley et al. 2010, Kiecolt-Glaser et al. 2003, Mausbach et al. 2007, von Känel et al. 2008).
While the preponderance of evidence suggests an association between caregiving and physiological function, it is important to keep in mind that the caregivers selected for these studies are typically moderately to highly stressed dementia caregivers and, therefore, the generalizability of findings may be limited. In addition, some researchers have questioned the choice of control subjects in these case control studies, which may not adequately control for preexisting differences between caregivers and noncaregivers (O’Reilly et al. 2015). Intervention studies that use random assignment should result in equivalent populations in treatment and control groups, but the evidence regarding the negative effects of caregiving on biomarkers such as cortisol and immune system factors in these studies is mixed (Allen et al. 2017).
5.4. Social Relationships
Family relationships and quality of life may be impacted by caregiving demands, although this topic has received relatively little attention in the caregiving literature. In a large panel study of Health and Retirement Study participants, Amirkhanyan & Wolf (2006) found that adverse psychological effects of caregiving are dispersed throughout the family and not just among active caregivers. Bookwala (2009) found, in a sample of adult caregiving daughters and sons, that longer-term caregivers were significantly less happy in their marriages than those who had recently assumed the caregiving role, suggesting that it takes time for negative impacts to manifest themselves. Caregiving demands can also negatively affect the quality of the relationship between the caregiver and recipient. A substantial literature shows that, for spousal caregivers of persons with dementia, behavioral symptoms such as negative emotion expression create difficulties for caregivers that deteriorate relationship satisfaction and decrease emotional and physical intimacy (Ascher et al. 2010, de Vugt et al. 2003, Simonelli et al. 2008). Monin and associates (2019) have also shown that, among spousal caregivers of older adults with multiple chronic conditions, for both caregivers and care recipients, depressive symptoms and lower self-reported health are associated with lower relationship satisfaction, and caregivers have especially low relationship satisfaction when they are disabled themselves and their partner is more depressed.
Sources of family conflict include differing views about the appropriate boundaries for caregiving, disapproval of specific family members’ actions or attitudes, disagreements about the nature and seriousness of the care recipient’s condition, perceived failure to appreciate the demands on the primary caregiver and to provide adequate help or support, differing views regarding the quality of care provided, and disagreements over placement of the care recipient and financial matters pertaining to the care recipient (Aneshensel et al. 1995, Gwyther & Matchar 2015, Schulz & Eden 2016, Strawbridge & Wallhagen 1991).
Because of care demands and lack of other support, many caregivers also confront problems with social isolation and withdrawal from social activities and relationships. Mausbach and associates (2011) found that caregivers of patients with Alzheimer’s disease who rated their participation in pleasant events as low and their activity restrictions as high reported more depressive symptoms, negative affect, and overload compared to other caregivers.
5.5. Work
Middle-aged women at the peak of their earning power, many of whom are employed, provide the majority of care to older disabled relatives. The increasing labor force participation of women, along with the increasing demand for care, raises important questions about how effectively and at what cost the roles of caregiver and worker can be combined.
The effects of caregiving on entering and leaving the workforce, opportunities for advancement, number of hours worked, and wages are mixed. This variability in outcomes can in part be explained by the study methodology (e.g., cross-sectional versus longitudinal panel studies, sampling strategies, and analytic methods used), where data were collected, gender of the caregiver, residency status of the caregiver vis-à-vis the care recipient, and intensity (i.e., hours of care provided, type of care provided) of caregiving. Cross-sectional studies using targeted sampling strategies with univariate analyses tend to report large negative effects of caregiving on work across the board. Representative sample multivariate panel studies, which are better equipped to identify causal relations between caregiving and work-related outcomes, show small effects and sometimes no effects. That said, when subgroups of caregivers are examined, we do find consistent small to moderate negative effects on work across most studies for female caregivers who live with the care recipient and provide high-intensity personal or medical and nursing care. These negative effects also vary by national policies regarding caregiver support, such that countries with more extensive health and long-term care support systems (e.g., northern Europe) report fewer negative impacts than countries with lower levels of support (e.g., southern Europe) (Schulz 2019).
Caregiving can also interfere with work performance, leading to the caregiver receiving fewer promotions, taking on a less-demanding job, or turning down promotions. All of these scenarios would result in reduced wages. Empirical evidence on direct wage effects in large population-based studies are inconclusive, with some studies finding that caregivers earn lower wages (Bittman et al. 2007, Heitmueller & Inglis 2007) and others finding no or very small differences (Lilly et al. 2010, Van Houtven et al. 2013). Carmichael & Charles (2003) find that wages for caregivers are 18% lower for male caregivers and 9% lower for female caregivers, but only for those who provide more than 10 hours of care per week. Heitmueller & Inglis (2007) report wage reductions of 3% attributable to caregiving status in a UK sample. In a large European survey of 120,000 individuals over the age of 50—the Survey of Health, Ageing and Retirement in Europe—no evidence was found for reduced wages (Bolin et al. 2008). Lilly and associates (2007) report a similar result for their Canadian sample.
Evidence linking caregiving to reduced work hours is more consistent, showing small but reliable negative effects. For example, in the NSOC, 12% of caregivers reported missing work to help the care recipient. Kotsadam (2011) finds that caregivers have 2–3% lower numbers of working hours compared to noncaregivers. Van Houtven et al. (2013) found that caregivers providing at least 100 hours of care over the previous two years work three hours less per week than noncaregivers. Using data from the German Socio-Economic Panel Study, Meng (2013) also reports small effects. Men providing in-home care reduced work hours by 48 minutes per week and women by 35 minutes per week. Lilly and associates (2010) find no overall effects on working hours; however, when they assess the effects of high-intensity caregiving (15–20 hours per week), a negative effect emerges.
5.6. Elder Mistreatment
A potential effect of caregiving stress is elder mistreatment and neglect. Mistreatment of older adults can take many forms, including physical, emotional, and sexual abuse, as well as financial exploitation, neglect, and abandonment (https://ncea.acl.gov). To qualify as mistreatment, a behavior has to intentionally cause harm or create a serious risk of harm to a vulnerable older adult. The term domestic elder abuse is used to refer to mistreatment committed by someone with whom the older adult has a special relationship, such as a spouse, sibling, child, friend, or caregiver. Caregiver neglect is a specific type of mistreatment in which the caregiver intentionally fails to address the physical, social, or emotional needs of the older person. This neglect can include actively withholding food, water, clothing, medications, or assistance with ADL such as help with personal hygiene. Prevalence estimates of abuse have generally ranged from 7% to 10% of older adults annually, although prevalence of physical abuse (less than 2%) and sexual abuse (less than 1%) are much lower (Acierno et al. 2010, Lachs & Berman 2011, Laumann et al. 2008). Research suggests that family members commit most abuse, but it is not known if this abuse occurs primarily within a caregiving context. Rates of abuse are generally higher for older adults with dementia and/or adults who need physical assistance, suggesting that family caregivers are likely perpetrators of abuse (Beach et al. 2005). Although the data suggest that family caregivers may play a significant role in committing elder mistreatment when it does occur, there is a lack of adequate data to address this issue.
Studies of potentially harmful behaviors, defined as behaviors that are detrimental to the elder’s physical and psychological well-being, show prevalence rates of nearly 25% among caregivers. By far the most prevalent potentially harmful caregiver behavior involved negative verbal interactions like screaming or yelling (22.2%) or using a harsh tone of voice, insulting the care recipient, calling the recipient names, or swearing (11.7%). Physical forms of abuse like hitting or slapping, shaking, and handling roughly in other ways were much less prevalent, reported by only approximately 1% of the care recipients (Beach et al. 2005). The level of care recipient physical functioning was a strong predictor of potentially harmful behavior. In addition, Beach et al. (2005) found that higher levels of caregiver cognitive impairment, physical symptoms, and depression were strong predictors of care recipient-reported potentially harmful behaviors. This suggests that caregivers who are themselves in poor health are at higher risk for potentially harmful behaviors. Similar results with even higher prevalence rates were reported by Lafferty and associates (2016) in their survey of more than 2,000 caregivers in Ireland.
Other recent work examining care recipient reports of unmet needs for ADL or IADL assistance is potentially relevant to more passive forms of caregiver neglect. Beach and associates (2019) have recently shown that high-need or high-cost recipients with multiple chronic conditions, with probable dementia, and/or at end of life were more likely to report unmet needs than lower-need recipients. This suggests that caregivers are unable to keep up with high demands for care, which might ultimately result in neglect. Two other recent studies (Beach & Schulz 2017, Vazeou-Nieuwenhuis et al. 2018) have found that caregivers reporting higher burden were more likely to have care recipients who reported unmet needs for care, further supporting potential links between stressed caregivers and increased unmet needs of the care recipient.
More research is needed on the prevalence of elder mistreatment among caregivers, the type of mistreatment that they commit, the circumstances under which it occurs, and the factors that mitigate mistreatment or neglect. Of particular importance is gaining a better understanding of how and when a supportive caregiving relationship evolves into an abusive one. Finally, the extent to which family caregivers experience abuse by the older adults for whom they care is not known. Relatedly, an important line of research suggests that individuals who are abused or neglected by their parents during childhood experience more depression as caregivers to those parents (Kong & Moorman 2015).
6. RISK FACTORS FOR ADVERSE OUTCOMES
Seven classes of risk factors have been identified: (a) sociodemographic factors including lower income, lower education, being older, being female, being the spouse of the care recipient, and living with the care recipient; (b) high-intensity caregiving (more than 100 hours per month), dementia care, and having to do medical procedures (shots or injections, wound care); (c) lack of perceived choice in taking on the caregiving role; (d) high levels of perceived care recipient suffering; (e) poor health and physical functioning of the caregiver; (f) limited social and professional support; and (g) a challenging home physical environment (stairs, clutter) lacking appropriate home modifications.
Although the association between these predictors and adverse caregiver outcomes is mixed, accumulating evidence suggests that caregiving intensity (i.e., hours of caregiving per week or month), female gender, relationship to the care recipient (wives are more affected than adult daughters or others), living with the care recipient, and challenging behavioral symptoms in the care recipient are relatively robust predictors of negative psychological effects. The risk for onset of distress increases progressively with the amount of time spent in caregiving each week. A longitudinal analysis of the British Household Panel Survey found that caregivers who provided long hours of care for extended periods of time had increased levels of psychological distress, and that this association was stronger for women than for men (Hirst 2005). Caregivers who provide high-intensity care are also more likely to make treatment decisions for the care recipient, which may be a unique risk factor for adverse outcomes. In a meta-analysis of 2,854 surrogate decision makers, at least one-third experienced emotional burden as the result of making treatment decisions. Negative effects were often substantial and typically lasted months or, in some cases, years. The most common negative effects were stress, guilt over the decisions that they made, and doubt regarding whether they had made the right decisions (Wendler & Rid 2011). Female caregivers have been found to experience more psychological distress than males in a meta-analysis (Pinquart & Sörensen 2006), in an early literature review (Yee & Schulz 2000), and in a recent systematic review (Schoenmakers et al. 2010). Gender differences in depression were partially explained by differences in caregiver stressors, such as more hours of care provided per week and a greater number of caregiving tasks performed by women. Caregivers who live with the care recipient are at increased risk of adverse outcomes.
Schulz and associates (Monin & Schulz 2009; Schulz et al. 2007, 2009) have shown that these effects are in part explained by the exposure to suffering of the care recipient. Living with an older adult who is physically or psychologically suffering takes its toll on the caregiver, above and beyond the pragmatic challenges of providing assistance. Whether an individual has a choice in taking on the caregiving role may also make a difference. Nearly half of all caregivers report that they had no choice in taking on the caregiving role, and lack of perceived choice is associated with increased levels of burden and depression (Reinhard et al. 2012, Schulz et al. 2012). Care recipients’ behavioral symptoms (e.g., agitation, irritability, combativeness) are also associated with negative effects for caregivers (Ballard et al. 2000, Gitlin et al. 2012, Pinquart & Sörensen 2003, Schoenmakers et al. 2010, Schulz et al. 1995, Torti et al. 2004, van der Lee et al. 2014). In their examination of multivariate models predicting dementia caregiver burden, depression, and mental health, van der Lee and associates (2014) concluded that care recipient behavioral symptoms (e.g., waking up at night, rejecting needed care, agitation, and verbal and physical aggressiveness) were stronger predictors of caregiver burden and depression than the cognitive or functional status of the care recipient. Pinquart & Sörensen (2003) also found that care recipients’ behavior problems had a greater impact on caregivers’ burden and depression than did care recipients’ physical and cognitive impairments. Torti and associates (2004) reported that behavioral problems are associated with caregiver burden across geographic regions and cultures.
Definitive conclusions about the relative importance of different risk factors should be viewed cautiously, however, because many of these risk factors are correlated with each other, and no studies have examined all of these risk factors simultaneously in a single large population-based study. Nevertheless, existing findings on risk factors can help inform efforts to target caregivers in need of support and shape the type of support provided (Beach et al. 2005).
7. INTERVENTION RESEARCH
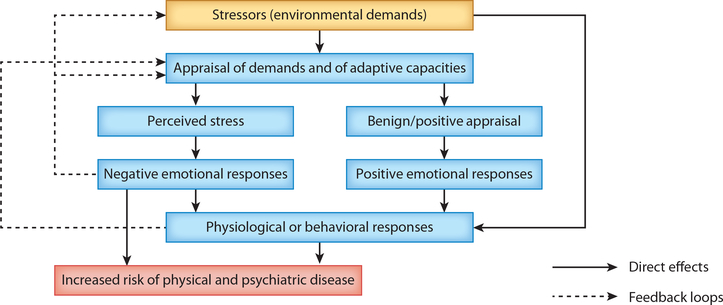
The dominant theoretical framework driving caregiver intervention research is the stress process model (see Cohen et al. 1995, Pearlin et al. 1990). An adaptation of this model applied to caregiving is presented in Figure 2 (Schulz 2000). The primary stressors or environmental demands include the functional limitations and problem behaviors of the care recipient and related social and environmental stressors. When confronted with these stressors, caregivers evaluate whether the demands pose a potential threat and whether sufficient adaptive capacities are available to cope with them. If they perceive the demands as threatening and at the same time view their coping resources as inadequate, then they perceive themselves as under stress. The appraisal of stress is presumed to result in negative affect, which under extreme conditions may directly contribute to the onset of affective psychiatric disorders. Negative emotional responses may also trigger behavioral or physiological responses that place the individual at increased risk of psychiatric or physical illness.
Figure 2:
A unified model of the stress–health process applied to caregiving. Solid lines represent direct effects and dashed lines represent feedback loops. Figure adapted with permission from Cohen et al. (1995).
More recently, this model has been elaborated on to include important reciprocal relations between care recipient and caregiver in terms of the perception of and the emotional and behavioral response to stress, as well as reciprocal effects of illness (Schulz 2000, Schulz et al. 2009).
The caregiver intervention literature is vast. At least 50 systematic reviews, many of which include meta-analyses, have been published since 2000. Indeed, since 2014, five systematic reviews of systematic reviews have been published (Clarkson et al. 2017, Corry et al. 2015, Dickinson et al. 2017, Gaugler et al. 2017, Gilhooly et al. 2016, Lopez-Hartmann et al. 2012). Rather than take the formal review process to yet another level and carry out a systematic review of systematic reviews of systematic reviews, our goal in this section is to broadly synthesize the intervention literature with the aim of describing key findings along with methodological and conceptual strengths and weaknesses.
The most common convention for classifying caregiver interventions is based on treatment content. The most common categories used are psychosocial or multicomponent interventions, which might include education about the disease and its course, information about resources, skills training, relaxation strategies, home modification, counseling, and social support. Other, more focused content areas such as physical activity and psychotherapeutic methods such as CBT or mindfulness meditation-based stress therapy have also been used to classify intervention studies. Finally, the literature also includes studies focused on professional services such as respite care and case management. While it might seem straightforward to classify a given study, Gaugler and associates (2017) show that this is not always the case. In their systematic review of systematic reviews, they identify multiple inconsistencies in how individual studies are classified.
Another method for parsing intervention studies is based on the underlying disease of the patient population. The large majority of studies focus on caregivers of persons with dementia, followed by cancer and stroke. Less frequently used categorization systems in reviews include delivery mode (i.e., technology-based versus human, individually or in groups) and target (i.e., caregiver, care recipient, or both; family; home physical environment; workplace) (Schulz et al. 2010). One can think of these variables as cross-cutting the content areas listed above. Thus, psychosocial interventions can be delivered via phone or Internet or in person via one-on-one interactions or in groups, and they may target the caregiver and/or the care recipient. One of the emerging trends in the caregiving intervention literature is the movement toward dyadic approaches to treatment. This strategy is based on the assumption that important synergies can be achieved by simultaneously treating the caregiver and care recipient (Martire & Schulz 2007, Schulz et al. 2009).
7.1. Psychosocial Interventions
The majority of caregiver interventions are best described as multicomponent psychosocial interventions. These studies are based on stress-coping theoretical models and emphasize principles of psycho-education and self-management to support caregivers by (a) addressing their main information needs, (b) equipping them with the adaptive strategies and behaviors that they need to mitigate the impact of the care recipient illness and disability on their daily lives (e.g., stress management), (c) enhancing communication skills between caregiver and care recipient and/or health care provider, (d) connecting them to other resources or services, and/or (e) providing them with social support. Outcome measures typically include indicators of psychological morbidity, burden, and stress, and depending on the specific focus of the intervention, researchers may also examine coping skills, social support, and patient outcomes such as problem behaviors (in dementia patients) and institutional placement. Although no one study is likely to include all of these components, virtually all of them include informational or educational components designed to educate the caregiver about disease symptomatology, disease progression, and sources of support.
The impact of these strategies is mixed (Dickinson et al. 2017, Gilhooly et al. 2016). Brodaty and associates (2003) reviewed 30 studies that included self-help groups, support groups, training, and counseling and found significant benefits in reducing caregiver distress but no significant differences in burden. Pusey & Richards (2001) concluded that the evidence of the effectiveness of both group-based interventions and individually based treatments was fairly weak due to inherent methodological weaknesses of the studies. In a recent meta-analysis of seven randomized controlled trial (RCT) psychoeducational interventions, Marim and associates (2013) found no significant differences in caregiver burden. In contrast, an earlier review by Pinquart & Sörensen (2006) found evidence that psychoeducational interventions reduced burden and depression, and Chien and associates (2011) found significant positive effects on depression and burden for caregiver support interventions.
Despite an increasing volume of both primary research and systematic reviews, it is difficult to conclude which combination of psychosocial treatments provides robust evidence of effectiveness. A recurrent theme in much of the intervention research is the relatively low quality of the research. Even RCTs typically do not score well on bias criteria (Savovic et al. 2018).
7.2. Meditative Interventions
Meditative interventions include a broad array of techniques, such as mindfulness meditation–based stress reduction, mindfulness-based cognitive therapy, mantra meditation, acceptance and commitment therapy, compassion-focused therapy, and dialectical behavior therapy (Collins & Kishita 2019, Collins et al. 2018, Dharmawardene et al. 2016). Core features of all of these strategies are the emphasis on and practice of meditation; being able to recognize and accept that unpleasant cognitions, emotions, and sensations are a part of life; the need to synthesize change and acceptance; and changes in the way that people relate to experiences and facilitate positive action in the face of life stressors (Collins & Kishita 2019). A robust literature on noncaregiver populations indicates that these strategies are effective in alleviating depression, anxiety, and stress in a wide range of clinical and nonclinical populations. Since stress and burden are central features of most caregiving experiences, meditative strategies should be beneficial to this population as well.
Multiple recent systematic reviews (Collins & Kishita 2019, Dharmawardene et al. 2016, Jaffray et al. 2016) report that meditative interventions were both feasible and acceptable for caregivers, with relatively low participant dropout rates. Statistically significant effect sizes were found for depression, burden, and stress. The most consistent and largest positive effects were found for depression, although these effects were not as robust as they are in the wider literature on mindfulness interventions (Jaffray et al. 2016). The research findings for meditative interventions are promising, but to date, these studies are based on small samples of predominantly caregivers of persons with dementia, include an assortment of methods (e.g., prepost, post only, and RCTs), and have high levels of heterogeneity indicating that results are not consistent across studies, and overall, study methodologies vary from very poor to moderately good (Collins & Kishita 2019). Clearly, additional high-quality research with large and diverse samples is needed to improve the robustness of the evidence for these strategies.
7.3. Physical Activity
The health benefits of physical activity for the general population as well as for individuals with chronic disease are well established (Reiner et al. 2013, Warburton et al. 2006). The benefits include enhanced physical functioning, reduced risk of cardiovascular disease and some forms of cancer, reduced stress and depression, improved mental and cognitive health, and improved general well-being and sleep. Given the physical and emotional challenges of caregiving and the fact that caregivers often report more negative health behaviors than do noncaregivers, caregivers may particularly benefit from the health-promoting effects of physical activity.
The literature includes more than a dozen intervention studies designed to enhance caregiver physical activity by having them engage in activities such as brisk walking, stair climbing, dancing, gardening, stretching, strength training, yoga, and tai chi (Cuthbert et al. 2017, Lambert et al. 2016). Outcome measures include indicators of psychological well-being such as depression and burden, physical activity levels, physical health indicators including functional capacity and fitness indicators (e.g., body strength, endurance, balance), vital signs, physical symptoms, body mass index, energy expenditure, sleep quality, and social functioning. Several recent reviews of this literature (Cuthbert et al. 2017, Lambert et al. 2016, Loi et al. 2014) claim psychological benefits (reduced stress, depression, and burden) attributable to physical activity interventions such as brisk walking. Orgeta & Miranda-Castillo (2014) report that physical activity reduced subjective burden in two of four randomized trials. Lambert and associates (2016) also conclude that there is some evidence for reductions in burden in the 14 intervention studies that they reviewed. However, none of the studies reviewed meet criteria for high-quality intervention studies (Lambert et al. 2016). For randomized trials, the litany of methodological limitations includes lack of clear specification of randomization procedures; lack of blinding among study personnel, particularly assessors of outcomes; incomplete outcome data; and selective outcome reporting. Nonrandomized trials studies suffered from the additional problem of not controlling for relevant confounding variables.
Given the strength of evidence demonstrating the beneficial effects of physical activity, should we be skeptical about the impact of physical activity on caregivers? We probably should not; however, the evidence to date does not inspire confidence in that conclusion given the many limitations characteristic of this research. In our view, research in this area should be focused on identifying optimal and feasible exercise regimens for this population and the best ways to deliver and integrate a physical activity intervention with other necessary components of caregiver interventions.
7.4. Cognitive Behavioral Therapy
CBT involves training individuals to develop cognitive and behavioral skills that will help them to cope with stressful and difficult situations. The cognitive skills developed through CBT are aimed at improving dysfunctional thoughts, while the behavioral skills increase pleasure when performing activities.
In their recent review of 12 RCTs, Kwon and associates (2017) concluded that CBT improved caregiver depression, anxiety, stress, and dysfunctional thoughts and also promoted factors that are needed to improve the quality of care, such as satisfaction with life, perceived self-efficacy, behavioral activation, and appraisal of problem behaviors. In addition, CBT positively influenced caregiving skills such as handling disruptive behaviors. However, meta-analysis was limited to depression, where a positive effect was found. In contrast to these conclusions, O’Toole and associates (2017) found only a negligible positive effect in a meta-analysis of 36 studies of cancer caregivers. Technology-based CBT interventions similarly revealed only small significant postintervention effects, with no evidence for long-term efficacy.
7.5. Respite and Care Coordination
Respite services provide the caregiver with a temporary break from caregiving duties to improve the well-being of the caregiver. They may include home care, day care, or institutional care services. One recent systematic review of 104 studies (Shaw et al. 2009) shows that burden was reduced at 2–6 months follow-up in single-sample studies but not in RCTs and quasi-experimental studies. Depression was reduced in RCTs in the short term when home care was provided, but not when day care was. However, these effects were not significant in random-effects models. Singlegroup studies suggested that quality of life was worse after respite use. Overall, there was some evidence to support respite having a positive effect on caregivers, but the evidence was limited and weak.
Another systematic review (Mason et al. 2007) summarized data from 22 studies in which caregivers were provided either day care, host family, in-home, institutional, or video respite. The impact of respite on caregivers was generally small, with better-controlled studies finding modest benefits. A more recent systematic review of day care respite studies paints a more positive picture regarding caregiver benefits (Vandepitte et al. 2016). Day care services were effective in decreasing caregiver burden and behavioral problems in persons with dementia, but they also accelerated time to nursing home admission. Because of challenges associated with implementing RCTs in community settings, Zarit and associates (2017) recommend using quasi-experimental and interrupted time series designs to assess the effects of respite care interventions.
Although there is no single accepted definition of care coordination as an intervention strategy, one common approach within this broad category involves the assignment of a case manager, usually a nurse, to the caregiver and care recipient dyad. This individual provides guidance and assistance in accessing relevant information and support services for the caregiver and patient. A unique feature of research in this area is the inclusion of both caregiver and care recipient outcomes. In a recent review of 14 coordination studies, meta-analysis showed significant improvement in both patient behavior and caregiver burden but only weak evidence of effects on caregiver mood, quality of life, and social support. Little evidence was found for patient hospitalization, mortality, quality of life, cognition, depression, or functioning (Backhouse et al. 2017). An important message emerging from this review is the importance for future trials to be rigorous in their design and implementation and focus on high-quality reporting not only of research methods, but also of the intervention details.
7.6. Technology-Based Interventions
Technology-based interventions have the potential to provide convenient and cost-effective methods of delivering a broad range of caregiver interventions. They can be used to deliver knowledge and information about the target disease, caregiver roles, and available support services. They can also be used to provide social support, deliver formal therapeutic strategies such as CBT, and monitor patient and caregiver behavior. Technology is also flexible and dynamic and offers the potential to provide information in a wide variety of formats to suit the needs of the individual caregiver. To date, the technology used has included Internet-based applications delivered via computer, tablets, or cell phones and handheld devices.
Caregivers are satisfied with and report benefiting from these interventions, but their usage is sporadic and declines over time (Wasilewski et al. 2017). Caregiver depression and burden are the primary outcome measures included in these studies, and findings are mixed, with a few studies reporting improvements on both outcomes (Egan et al. 2018, Goodwin et al. 2013, Scott et al. 2016, Wasilewski et al. 2017). In four studies assessing the effectiveness of technology-based CBT interventions, Scott and associates (2016) found small significant postintervention effects for depression but no evidence of long-term efficacy. Czaja and associates (2013) found that caregivers who received a multicomponent psychosocial intervention via videophone technology reported a decrease in burden, an increase in social support, and an increase in positive perceptions of the caregiving experience.
Overall, the literature suggests that technology-based interventions are feasible and acceptable to caregivers, and that these types of interventions can be efficacious. However, there are many remaining issues that need to be addressed, such as the cost-effectiveness of these interventions, system design characteristics, accessibility, and how to best integrate these interventions with other standard care practices.
7.7. Recommendations
There is reasonable agreement among researchers that caregivers are likely to benefit from enhanced knowledge about the disease, the caregiving role, and resources available to them. Once the informational needs have been met, caregivers might additionally benefit from training in general problem-solving skills, as well as from interventions that target managing care recipient behaviors or caregivers’ own emotional response to caregiving. Some studies have taught the caregiver rudimentary behavior management skills, including behavioral assessment techniques and methods for changing antecedents and consequences of disruptive behaviors. The efficacy of all of these components is likely to be enhanced when tailored to the specific needs of the individual. Recent intervention studies have also suggested that there may be important synergies achieved by simultaneously treating care recipients (e.g., giving medications or memory retraining) and caregivers and by altering the social and physical environments via multicomponent interventions.
Our ability to gauge the efficacy of these strategies could be substantially enhanced with the development and application of a standardized taxonomy for characterizing and measuring multicomponent psychosocial interventions (Czaja et al. 2003, Gaugler et al. 2017, Schulz et al. 2010). The application of a clearly articulated taxonomy would enable us to better describe and compare interventions across studies, as well as to link intervention components to specific outcomes. Closer attention should also be paid to the assumed links between an intervention and the proposed outcomes. For example, we should not expect that interventions aimed at reducing caregiver anger or hostility will also delay institutionalization for the care recipient. We also need to be more careful in our choice of study participants. If we target caregivers who are at or near the normal range of depressive symptomatology, then we are unlikely to achieve meaningful improvements with an intervention designed to decrease depression. In other words, we should be sure that the study participants display the problems targeted by the intervention.
Although the literature on interventions is useful in pointing toward some general rules of thumb, it suffers from numerous methodological problems. Putting aside for the moment the many methodological limitations of non-RCTs, the potential risk of bias in published RCTs is moderate to high. Most studies do not adequately describe sequence generation or allocation concealment. Although masking of participants and interventionists is not always possible, many studies fail to mask outcome assessors. Indeed, in some studies, interventionists assess outcomes for the same individuals that they treat. Outcome data are often incomplete, and methods for dealing with missing data are frequently not reported. Perhaps most egregious is the problem of selective outcome reporting, with a focus on those outcomes that yield statistically significant effects. Other limitations include small sample sizes, poor quality control in data collection and intervention implementation, and limited follow-up periods.
Many of these biases should work in favor of finding and reporting significant effects, yet the literature overall suggests small to moderate effects, at best, for some outcomes. Moreover, one could argue that our focus should be on the clinical significance of a caregiver intervention, as opposed to statistical significance in domains such as quality of life, burden, and depressive symptoms. Clinical significance generally refers to the practical value of the effects of an intervention, or the extent to which an intervention makes a real difference in the everyday lives of individuals (Kazdin 1999).
Caregiver interventions are often designed to address multiple problems, thereby affording the opportunity to achieve outcomes in multiple domains, some of which may be judged more clinically meaningful than others. We would advocate for an outcomes agenda that includes the following criteria: (a) symptomatology, i.e., the extent to which individuals return to normal functioning or experience a meaningful improvement in symptoms; (b) quality of life, i.e., the extent to which interventions broadly improve an individual’s quality of life; (c) social significance, i.e., the extent to which outcomes are important to society (e.g., the impact of the intervention on service utilization of both caregiver and care recipient); and (d) social validity, i.e., the extent to which treatment goals, procedures, and outcomes are acceptable as assessed by the client. This still leaves us with the challenge of defining what is meant by meaningful change or improved quality of life. For caregivers, this might include movement out of a clinically defined state such as major depression; changes in symptomatology equal to one standard deviation or more on a symptom scale; and consistent improvement in multiple indicators such as health, happiness, and social connectedness and engagement, reflecting one’s ability to enjoy a normal life.
To date, most studies meet criteria for social validity; study participants consistently rate the interventions as beneficial, helpful, or valuable. Some interventions show promise in achieving clinically significant outcomes in improving depressive symptoms. However, our ability to date to improve overall quality of life for caregivers appears to be limited; there is evidence that some components of quality of life, such as caregiver burden, mood, and perceived stress, are responsive to interventions, but the effects are typically small. Finally, we have few examples of societally meaningful outcomes, such as health care utilization of the caregiver and/or care recipient, delayed institutionalization of the care recipient, and reduced rehospitalizations.
The broad range of outcomes reported in this review is indicative of both strengths and weaknesses in the caregiver intervention literature. On the one hand, these outcomes point to the multifaceted impact of caregiving and the diversity of intervention effects that might be achieved. On the other hand, this diversity of outcomes, along with the diversity of interventions, makes it difficult to reach strong conclusions about what has been achieved in this literature. We recommend that a core set of outcomes be included in all intervention studies, and that they represent each of the four categories of clinical significance identified above, with much greater emphasis on the societal significance of an intervention than has been the case to date (e.g., How does it affect cost and health care utilization of caregivers and care recipients?). In making this recommendation, we are not advocating that all studies need to be designed to achieve clinical significance in all domains, but rather that at least some aspects of all domains be measured. Furthermore, it would be useful to develop consensus-based recommendations regarding specific measures to be used within each category of clinical significance. Once specific measures have been identified, the next step would be to reach consensus on what constitutes a clinically meaningful effect size for a given measure, along with recommended statistical procedures for demonstrating those effects (Kendall et al. 1999).
8. CONCLUSION AND FUTURE DIRECTIONS
The study of caregiving as a scientific enterprise is here to stay. As a platform for chronic stress research, family caregiving will continue to provide opportunities for studying the relationship among psychology, biology, and health. Social, clinical, and health psychologists will continue to advance the basic and applied science agenda in each of these areas. Inasmuch as policy and research are inextricably intertwined in the world of caregiving, their work may also have the added benefit of helping to address basic policy issues facing the nation. Moving the field forward will require an ambitious research agenda that addresses the key big picture issues detailed below.
Researchers should assess the prevalence and impact of caregiving by adopting a standardized operational definition of what it means to be an informal caregiver and use it consistently in surveys of the US population to accurately assess the prevalence of caregiving and the potential public health burden associated with caregiving. Having such data is an important requisite to developing policy on overall support programs for caregivers. We need to have accurate and consistent data on who is providing care, what types of care are provided, for how long, at what costs to the caregiver and other family members, and at what current and downstream costs and benefits to society. Inasmuch as the experience and impact of caregiving are both context and disease specific, it will also be important to develop additional measurement strategies that capture the needs of caregivers and care recipients at specific locations in a disease and treatment trajectory.
Not all caregivers need help. Research and policy should focus on those caregivers who are at risk for adverse outcomes, for example, persons caring for seriously ill high-need and high-cost patients for whom the intensity, duration, and adverse impact of caregiving reach extreme levels. Among older adults, high-need and high-cost patients include (a) patients who have three or more chronic diseases and a functional limitation in their ability to care for themselves or perform routine daily tasks, (b) patients with a diagnosis of probable dementia, and (c) patients at the end of life (Schulz et al. 2018). As noted above, recent research shows that high-need and high-cost patients are more likely to report more unmet needs for informal care (Beach et al. 2019). Identifying, assessing, and supporting caregivers caring for high-need and high-cost patients will be essential to a health care system that depends on them to provide the lion’s share of the care for these patients. Accomplishing these goals will require assessment tools tailored to these populations, support options that address the unique challenges faced by these caregivers, and new training programs that prepare providers to effectively engage caregivers of these populations.
Researchers should understand the drivers of caregiver distress. There remain important unanswered questions about caregiving that have far-reaching policy implications. For example, we need a deeper understanding of what causes distress in the caregiving experience and how best to help the caregiver. Although numerous studies point to the importance of various functional disabilities and associated care demands as causes of caregiver burden, we may be underestimating the role that factors such as care recipient suffering play in the life of a caregiver. Making these distinctions is important because it may lead to different policy responses (e.g., providing respite to ease the burdens of care provision, as well as treatments to decrease the suffering of the care recipient or to help the caregiver come to terms with the uncontrollable suffering of their loved one). The relative success of meditative intervention strategies may in part be due to the fact that they encourage reflection on what is and is not achievable in helping a loved one.
Researchers should explore how best to integrate caregivers into existing health care and support service programs. A major theme of the recent National Academies of Sciences, Engineering, and Medicine report on caregiving for older adults (Schulz & Eden 2016) is that family caregivers need to be formally integrated with existing formal health and support service programs. This will require a clear understanding of the task demands of the care assigned to them and assessment of caregiver capabilities, including their motivation to provide care; their physical, sensory, motor, and cognitive ability to perform required tasks; their levels of distress and depression; and the quantity and quality of other support available to them. Assessments of the caregiver should be a routine feature during care recipient and health care provider encounters, and these data should inform decisions about whether a caregiver is capable of taking on the caregiver role, the types of training needed, and the intensity of monitoring and external support required to assure adequate care that does not unduly compromise the caregiver’s own functioning (Schulz et al. 2018). A related need concerns the development of monitoring strategies and stopping rules for ceasing care when caregivers are no longer able to provide it. Implementing these strategies will require that we expand the training of health care and social service providers to give them the skills and tools to carry out these types of assessments, as well new mechanisms for addressing caregiver training and support needs.
Researchers should shift from efficacy to implementation research. Given the mixed success and impact of efficacy intervention trials carried out to date, we advocate a major shift in the intervention research agenda toward testing models for integrating caregiver support into existing health and long-term support service systems. Studies focused specifically on caregiving and system integration should be pursued. These studies may include the development and testing of new intervention strategies specifically focused on system integration or the widespread implementation of existing successful evidence-based treatment strategies. One example of the latter approach is the REACH intervention (Belle et al. 2006), modified versions of which have been implemented in the Department of Veterans Affairs (Nichols et al. 2016) and community and clinical settings (Burgio et al. 2009, Czaja et al. 2018).
Researchers should embrace technology to support caregivers. Technology has the potential to increase the efficiency and effectiveness of formal and informal care providers, enhance the functioning and autonomy of individuals with disability, prevent premature decline, and generally enhance the quality of life of elders. Implementing technology-based solutions will require that we develop user-friendly and highly reliable systems that are able to both identify needs and respond to them. We also need to ensure that caregivers have meaningful access to these technologies. We have made considerable progress in recent years in developing and deploying sensing and monitoring technologies that are useful in identifying individuals experiencing or at risk for adverse health outcomes. Computer, sensing, and communication technologies have also been effectively used for caregiver training and performance monitoring. Research on enabling technologies that extend the functional capability of humans, and the accessibility of these technologies, is still in the early stages of development and should receive high priority (Schulz et al. 2015).
Researchers should educate and prepare all adults for caregiving. Because caregiving is so prevalent in our society and integral to the health and well-being of the population, all adults need to be educated about the likelihood of becoming a caregiver and a care recipient, the roles and responsibilities of caregiving, and rudimentary caregiving skills. Most adults are able to imagine becoming a caregiver, but few see themselves as care recipients (Schulz & Tompkins 2010). We need to break through these perceptual barriers to adequately prepare adults for these inevitable life experiences.
Caregiving is a central feature of the health care landscape and will become even more prominent in the decades ahead. The demand and need for care will increase dramatically over the next three decades as a result of the aging of the population, infant and childhood survival, health behaviors that increase disabling health conditions such as obesity, and returning war veterans suffering from polytrauma. This will happen in a context where the availability of informal support is declining because of lower fertility and higher rates of childlessness, divorce, and people never marrying, as well as increased labor force participation of women, who will continue to be the primary caregivers. The costs of formal care and support are already too high and unsustainable, and there is a growing shortfall of health care professionals with relevant expertise. Resolving this supply–demand dilemma will require new models of integrated informal and formal care that achieve greater efficiencies than current practice. The alternative is a world where negative stereotypes about aging become a reality.
Acknowledgments
DISCLOSURE STATEMENT
Preparation of the manuscript was in part supported by the National Institutes of Health and the Health Resources and Services Administration. The authors are not aware of any affiliations, memberships, funding, or financial holdings that might be perceived as affecting the objectivity of this review.
LITERATURE CITED
- Acierno R, Hernandez MA, Amstadter AB, Resnick HS, Steve K, et al. 2010. Prevalence and correlates of emotional, physical, sexual, and financial abuse and potential neglect in the United States: the National Elder Mistreatment Study. Am. J. Public Health 100:292–97 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Allen AP, Curran EA, Duggan Á, Cryan JF, Chorcoráin AN, et al. 2017A systematic review of the psychobiological burden of informal caregiving for patients with dementia: focus on cognitive and biological markers of chronic stress. Neurosci. Biobehav. Rev. 73:123–64 [DOI] [PubMed] [Google Scholar]
- Amirkhanyan AA, Wolf DA. 2006. Parent care and the stress process: findings from panel data. J. Gerontol. B 61:S248–55 [DOI] [PubMed] [Google Scholar]
- Aneshensel CS, Pearlin LI, Mullan JT, Zarit SH, Whitlatch CJ. 1995. Profiles in Caregiving: The Unexpected Career. Cambridge, MA: Academic [Google Scholar]
- Ascher EA, Sturm VE, Seider BH, Holley SR, Miller BL, Levenson RW. 2010. Relationship satisfaction and emotional language in frontotemporal dementia and Alzheimer’s disease patients and spousal caregivers. Alzheimer Dis. Assoc. Disord. 24:49–55 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Backhouse A, Ukoumunne OC, Richards DA, McCabe R, Watkins R, Dickens C. 2017. The effectiveness of community-based coordinating interventions in dementia care: a meta-analysis and subgroup analysis of intervention components. BMC Health Serv. Res. 17:717. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ballard C, Lowery K, Powell I, O’Brien J, James I. 2000. Impact of behavioral and psychological symptoms of dementia on caregivers. Int. Psychogeriatr. 12:93–105 [Google Scholar]
- Beach SR, Schulz R. 2017. Family caregiver factors associated with unmet needs for care of older adults. J. Am. Geriatr. Soc. 65:560–66 [DOI] [PubMed] [Google Scholar]
- Beach SR, Schulz S, Friedman EM, Rodakowski J, Martsolf RG, James AE. 2019. Adverse consequences of unmet needs for care in high-need/high-cost older adults. J. Gerontol. B. In press. 10.1093/geronb/gby021 [DOI] [PubMed] [Google Scholar]
- Beach SR, Schulz R, Williamson GM, Miller LS, Weiner MF, Lance CE. 2005. Risk factors for potentially harmful informal caregiver behavior. J. Am. Geriatr. Soc. 53:255–61 [DOI] [PubMed] [Google Scholar]
- Beach SR, Schulz R, Yee JL, Jackson S. 2000. Negative and positive health effects of caring for a disabled spouse: longitudinal findings from the Caregiver Health Effects Study. Psychol. Aging 15:259–71 [DOI] [PubMed] [Google Scholar]
- Belle SH, Burgio L, Burns R, Coon D, Czaja SJ, et al. 2006. Enhancing the quality of life of dementia caregivers from different ethnic or racial groups: a randomized, controlled trial. Ann. Intern. Med. 145:727–38 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bittman M, Hill T, Thomson C. 2007. The impact of caring on informal carers’ employment, income and earnings: a longitudinal approach. AJSI 42:255–72 [Google Scholar]
- Bolin K, Lindgren B, Lundborg P. 2008. Your next of kin or your own career? Caring and working among the 50+ of Europe. J. Health Econ. 27:718–38 [DOI] [PubMed] [Google Scholar]
- Bookwala J 2009. The impact of parent care on marital quality and well-being in adult daughters and sons. J. Gerontol. B 64B:339–47 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brodaty H, Green A, Koschera A. 2003. Meta-analysis of psychosocial interventions for caregivers of people with dementia. J. Am. Geriatr. Soc. 51:657–64 [DOI] [PubMed] [Google Scholar]
- Brown RM, Brown SL. 2014. Informal caregiving: a reappraisal of effects on caregivers. Soc. Issues Policy Rev. 8:74–102 [Google Scholar]
- Burgio LD, Collins IB, Schmid B, Wharton T, McCallum D, DeCoster J. 2009. Translating the REACH caregiver intervention for use by area agency on aging personnel: the REACH OUT program. Gerontologist 49:103–16 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cameron JI, Elliott TR. 2015. Studying long-term caregiver health outcomes with methodologic rigor. Neurology 84:1292–93 [DOI] [PubMed] [Google Scholar]
- Capistrant BD. 2016. Caregiving for older adults and the caregivers’ health: an epidemiologic review. Curr. Epidemiol. Rep. 3:72–80 [Google Scholar]
- Carmichael F, Charles S. 2003. The opportunity costs of informal care: Does gender matter? J. Health Econ. 22:781–803 [DOI] [PubMed] [Google Scholar]
- Chien LY, Chu H, Guo JL, Liao YM, Chang LI, et al. 2011. Caregiver support groups in patients with dementia: a meta-analysis. Int. J. Geriatr. Psychiatry 26:1089–98 [DOI] [PubMed] [Google Scholar]
- Clarkson P, Hughes J, Xie C, Larbey M, Roe B, et al. 2017. Overview of systematic reviews: effective home support in dementia care, components and impacts—Stage 1, psychosocial interventions for dementia. J. Adv. Nurs. 73:2845–63 [DOI] [PubMed] [Google Scholar]
- Cohen S, Kessler RC, Gordon LU, eds. 1995. Measuring Stress: A Guide for Health and Social Scientists. Oxford, UK: Oxford Univ. Press [Google Scholar]
- Collins RN, Gilligan LJ, Poz R. 2018. The evaluation of a compassion-focused therapy group for couples experiencing a dementia diagnosis. Clin. Gerontol. 41:474–86 [DOI] [PubMed] [Google Scholar]
- Collins RN, Kishita N. 2019. The effectiveness of mindfulness- and acceptance-based interventions for informal caregivers of people with dementia: a meta-analysis. Gerontologist 59:e363–79 [DOI] [PubMed] [Google Scholar]
- Corry M, While A, Neenan K, Smith V. 2015. A systematic review of systematic reviews on interventions for caregivers of people with chronic conditions. J. Adv. Nurs. 71:718–34 [DOI] [PubMed] [Google Scholar]
- Cuijpers P 2005. Depressive disorders in caregivers of dementia patients: a systematic review. Aging Mental Health 9:325–30 [DOI] [PubMed] [Google Scholar]
- Cuthbert CA, King-Shier K, Ruether D, Tapp DM, Culos-Reed SN. 2017. What is the state of the science on physical activity interventions for family caregivers? A systematic review and RE-AIM evaluation. J. Phys. Act. Health 14:578–95 [DOI] [PubMed] [Google Scholar]
- Czaja SJ, Lee CC, Perdomo D, Loewenstein D, Bravo M, et al. 2018. Community REACH: a community implementation of an evidence-based caregiver program. Gerontologist 58:e130–37 [DOI] [PubMed] [Google Scholar]
- Czaja SJ, Loewenstein D, Schulz R, Nair SN, Perdomo D. 2013. A videophone psychosocial intervention for dementia caregivers. Am.J. Geriatr Psychiatry 21:1071–81 [DOI] [PubMed] [Google Scholar]
- Czaja SJ, Schulz R, Lee CC, Belle SH. 2003. A methodology for describing and decomposing complex psychosocial and behavioral interventions. Psychol. Aging 18:385–95 [DOI] [PubMed] [Google Scholar]
- Damjanovic AK, Yang Y, Glaser R, Kiecolt-Glaser JK, Nguyen H, et al. 2007. Accelerated telomere erosion is associated with a declining immune function of caregivers of Alzheimer’s disease patients. J. Immunol. 179:4249–54 [DOI] [PMC free article] [PubMed] [Google Scholar]
- De Vugt ME, Stevens F, Aalten P, Lousberg R, Jaspers N, et al. 2003. Behavioural disturbances in dementia patients and quality of the marital relationship. Int. J. Geriatr. Psychiatry 18:149–54 [DOI] [PubMed] [Google Scholar]
- Dharmawardene M, Givens J, Wachholtz A, Makowski S, Tjia J. 2016. A systematic review and meta-analysis of meditative interventions for informal caregivers and health professionals. BMJ Support. Palliat. Care 6:160–69 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dickinson C, Dow J, Gibson G, Hayes L. 2017. Psychosocial intervention for carers of people with dementia: What components are most effective and when? A systematic review of systematic reviews. Int. Psychogeriatr. 29:31–43 [DOI] [PubMed] [Google Scholar]
- Dunkle RE, Feld S, Lehning AJ, Kim H, Shen HW, Kim MH. 2014. Does becoming an ADL spousal caregiver increase the caregiver’s depressive symptoms? Res. Aging 36:655–82 [DOI] [PubMed] [Google Scholar]
- Egan KJ, Pinto-Bruno AC, Bighelli I, Berg-Weger M, van Straten A, et al. 2018. Online training and support programs designed to improve mental health and reduce burden among caregivers of people with dementia: a systematic review. J. Am. Med. Dir Assoc. 19:200–6 [DOI] [PubMed] [Google Scholar]
- Freedman VA, Kasper JD, Cornman JC, Agree EM, Bandeen-Roche K, et al. 2011. Validation of new measures of disability and functioning in the National Health and Aging Trends Study. J. Gerontol. A 66:1013–21 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gaugler J, Jutkowitz E, Shippee TP, Brasure M. 2017. Consistency of dementia caregiver intervention classification: an evidence-based synthesis. Int. Psychogeriatr. 29:19–30 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gilhooly KJ, Gilhooly ML, Sullivan MP, McIntyre A, Wilson L, et al. 2016. A meta-review of stress, coping and interventions in dementia and dementia caregiving. BMC Geriatr. 16:106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Giovannetti ER, Wolff JL. 2010. Cross-survey differences in national estimates of numbers of caregivers of disabled older adults. Milbank Q. 88:310–49 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gitlin LN, Kales HC, Lyketsos CG. 2012. Nonpharmacologic management of behavioral symptoms in dementia. JAMA 308:2020–29 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goodwin KM, Mills WL, Anderson JA, Kunik ME. 2013. Technology-driven interventions for caregivers of persons with dementia: a systematic review. Am. J. Alzheimers Dis. Other Demen 28:216–22 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grady PA, Rosenbaum LM. 2015. The science of caregiver health. J. Nurs. Scholarsh. 47:197–99 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grossman A, D’Augelli A, Dragowski E. 2007. Caregiving and care receiving among older lesbian, gay, and bisexual adults. J. Gay Lesbian Soc. Serv. 18:15–38 [Google Scholar]
- Gwyther LP, Matchar BG. 2015. The Duke employee elder care consultation: meeting employees where they are. Generations 39:105–8 [Google Scholar]
- Haley WE, Roth DL, Howard G, Safford MM. 2010. Caregiving strain and estimated risk for stroke and coronary heart disease among spouse caregivers: differential effects by race and sex. Stroke 41:331–36 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Heitmueller A, Inglis K. 2007. The earnings of informal carers: wage differentials and opportunity costs. J. Health Econ. 26:821–41 [DOI] [PubMed] [Google Scholar]
- Hirst M 2005. Carer distress: a prospective, population-based study. Soc. Sci. Med. 61:697–708 [DOI] [PubMed] [Google Scholar]
- Hughes M, Kentlyn S. 2011. Older LGBT people’s care networks and communities of practice: a brief note. Int. Soc. Work 54:436–44 [Google Scholar]
- Jaffray L, Bridgman H, Stephens M, Skinner T. 2016. Evaluating the effects of mindfulness-based interventions for informal palliative caregivers: a systematic literature review. Palliat. Med. 30:117–31 [DOI] [PubMed] [Google Scholar]
- Kazdin AE. 1999. The meanings and measurement of clinical significance. J. Consult. Clin. Psychol. 67:332–39 [DOI] [PubMed] [Google Scholar]
- Kendall PC, Marrs-Garcia A, Nath SR, Shedrick RC. 1999. Normative comparisons for the evaluation of clinical significance. J. Consult. Clin. Psychol. 67:285–99 [DOI] [PubMed] [Google Scholar]
- Kiecolt-Glaser JK, Preacher KJ, MacCallum RC, Atkinson C, Malarkey WB, Glaser R. 2003. Chronic stress and age-related increases in the proinflammatory cytokine IL-6. PNAS 100:9090–95 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kong J, Moorman SM. 2015. Caring for my abuser: childhood maltreatment and caregiver depression. Gerontologist 55:656–66 [DOI] [PubMed] [Google Scholar]
- Kotsadam A 2011. Does informal eldercare impede women’s employment? The case of European welfare states. Fem. Econ. 17:121–44 [Google Scholar]
- Kurtz ME, Kurtz JC, Given CW, Given B. 1995. Relationship of caregiver reactions and depression to cancer patients’ symptoms, functional states and depression—a longitudinal view. Soc. Sci. Med 40:837–46 [DOI] [PubMed] [Google Scholar]
- Kwon OY, Ahn HS, Kim HJ, Park KW. 2017. Effectiveness of cognitive behavioral therapy for caregivers of people with dementia: a systematic review and meta-analysis. J. Clin. Neurol. 13:394–404 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lachs M, Berman J. 2011. Under the radar: New York State Elder Abuse Prevalence Study. Rep., Lifesp. Great. Rochester Inc./Weill Cornell Med. Cent. Cornell Univ./New York City Dep. Aging, New York [Google Scholar]
- Lafferty A, Fealy G, Downes C, Drennan J. 2016. The prevalence of potentially abusive behaviours in family caregiving: findings from a national survey of family carers of older people. Age Ageing 45:703–7 [DOI] [PubMed] [Google Scholar]
- Lambert SD, Duncan LR, Kapellas S, Bruson AM, Myrand M, et al. 2016. A descriptive systematic review of physical activity interventions for caregivers: effects on caregivers’ and care recipients’ psychosocial outcomes, physical activity levels, and physical health. Ann. Behav. Med. 50:907–19 [DOI] [PubMed] [Google Scholar]
- Laumann EO, Leitsch SA, Waite LJ. 2008. Elder mistreatment in the United States: prevalence estimates from a nationally representative study. J. Gerontol. B 63:S248–54 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lilly MB, Laporte A, Coyte PC. 2007. Labor market work and home care’s unpaid caregivers: a systematic review of labor force participation rates, predictors of labor market withdrawal, and hours of work. Milbank Q. 85:641–90 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lilly MB, Laporte A, Coyte PC. 2010. Do they care too much to work? The influence of caregiving intensity on the labour force participation of unpaid caregivers in Canada. J. Health Econ. 29:895–903 [DOI] [PubMed] [Google Scholar]
- Loi SM, Dow B, Ames D, Moore K, Hill K, et al. 2014. Physical activity in caregivers: What are the psychological benefits? Arch. Gerontol. Geriatr. 59:204–10 [DOI] [PubMed] [Google Scholar]
- Lopez-Hartmann M, Wens J, Verhoeven V, Remmen R. 2012. The effect of caregiver support interventions for informal caregivers of community-dwelling frail elderly: a systematic review. Int. J. Integr. Care 12:e133. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marim CM, Silva V, Taminato M, Barbosa DA. 2013. Effectiveness of educational programs on reducing the burden of caregivers of elderly individuals with dementia: a systematic review. Rev. Lat. Am. Enfermagem. 21:267–75 [DOI] [PubMed] [Google Scholar]
- Martire LM, Schulz R. 2007. Involving family in psychosocial interventions for chronic illness. Curr. Dir. Psychol. Sci. 16:90–94 [Google Scholar]
- Mason A, Weatherly H, Spilsbury K, Arksey H, Golder S, et al. 2007. A systematic review of the effectiveness and cost-effectiveness of different models of community-based respite care for frail older people and their carers. Health Technol. Assess. 11:1–157 [DOI] [PubMed] [Google Scholar]
- Mausbach BT, Patterson TL, Rabinowitz YG, Grant I, Schulz R. 2007. Depression and distress predict time to cardiovascular disease in dementia caregivers. Health Psychol. 26:539–44 [DOI] [PubMed] [Google Scholar]
- Mausbach BT, Roepke SK, Depp CA, Moore R, Patterson TL, Grant I.2011. Integration of the pleasant events and activity restriction models: development and validation of a “PEAR” model of negative outcomes in Alzheimer’s caregivers. Behav. Ther 42:78–88 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Meng A 2013. Informal home care and labor-force participation of household members. Empir. Econ. 44:959–79 [Google Scholar]
- Monin JK, Levy B, Doyle M, Schulz R, Kershaw T. 2019. The impact of both spousal caregivers’ and care recipients’ health on relationship satisfaction in the Caregiver Health Effects Study. J. Health Psychol. 24:1744–55 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Monin JK, Schulz R. 2009. Interpersonal effects of suffering in older adult caregiving relationships. Psychol. Aging 24:681–95 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Natl. Alliance Caregiv. AARP Public Policy Inst. 1997. Family caregiving in the U.S.: findings from a national survey. Rep, Natl. Alliance Caregiv./AARP Public Policy Inst, Washington, DC [Google Scholar]
- Natl. Alliance Caregiv. AARP Public Policy Inst. 2004. Caregiving in the U.S.: 2004 report. Rep, Natl. Alliance Caregiv./AARP Public Policy Inst., Washington, DC [Google Scholar]
- Natl. Alliance Caregiv. AARP Public Policy Inst. 2009. Caregiving in the U.S.: 2009 report. Rep, Natl. Alliance Caregiv./AARP Public Policy Inst., Washington, DC [Google Scholar]
- Natl. Alliance Caregiv. AARP Public Policy Inst. 2015. Caregiving in the U.S.: 2015 report. Rep, Natl. Alliance Caregiv./AARP Public Policy Inst., Washington, DC [Google Scholar]
- Nichols LO, Martindale-Adams J, Burns R, Zuber J, Graney MJ. 2016. REACH VA: moving from translation to system implementation. Gerontologist 56:135–44 [DOI] [PubMed] [Google Scholar]
- O’Reilly D, Rosato M, Maguire A. 2015. Caregiving reduces mortality risk for most caregivers: a census-based record linkage study. Int. J. Epidemiol. 44:1959–69 [DOI] [PubMed] [Google Scholar]
- Orgeta V, Miranda-Castillo C. 2014. Does physical activity reduce burden in carers of people with dementia? A literature review. Int. J. Geriatr. Psychiatry 29:771–83 [DOI] [PubMed] [Google Scholar]
- O’Toole MS, Zachariae R, Renna ME, Mennin DS, Applebaum A. 2017. Cognitive behavioral therapies for informal caregivers of patients with cancer and cancer survivors: a systematic review and meta-analysis. Psychooncology 26:428–37 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pearlin LI, Mullan JT, Semple SJ, Skaff MM. 1990. Caregiving and the stress process: an overview of concepts and their measures. Gerontologist 30:583–94 [DOI] [PubMed] [Google Scholar]
- Penrod JD, Kane RA, Kane RL, Finch MD. 1995. Who cares? The size, scope and composition of the caregiver support system. Gerontologist 35:489–97 [DOI] [PubMed] [Google Scholar]
- Pinquart M, Sörensen S. 2003. Associations of stressors and uplifts of caregiving with caregiver burden and depressive mood: a meta-analysis. J. Gerontol. B 58:P112–28 [DOI] [PubMed] [Google Scholar]
- Pinquart M, Sörensen S. 2006. Gender differences in caregiver stressors, social resources and health: updated meta-analysis. J. Gerontol. B 61:P33–45 [DOI] [PubMed] [Google Scholar]
- Pusey H, Richards D. 2001. A systematic review of the effectiveness of psychosocial interventions for carers of people with dementia. Aging Mental Health 5:107–19 [DOI] [PubMed] [Google Scholar]
- Reiner M, Niermann C, Jekauc D, Woll A. 2013. Long-term health benefits of physical activity—a systematic review of longitudinal studies. BMC Public Health 13:813. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Reinhard S, Feinberg L. 2015. The escalating complexity of family caregiving: meeting the challenge In Family Caregiving in the New Normal, ed. Gaugler JE, Kane RL, pp. 291–304. Cambridge, MA: Academic [Google Scholar]
- Reinhard SC, Levine C, Samis S. 2012. Home alone: family caregivers providing complex chronic care. Rep., United Hosp. Fund/AARP Public Policy Inst., Washington, DC [Google Scholar]
- Robison J, Fortinsky R, Kleppinger A, Shugrue N, Porter M. 2009. A broader view of family caregiving: effects of caregiving and caregiver conditions on depressive symptoms, health, work, and social isolation. J. Gerontol. B 64:788–98 [DOI] [PubMed] [Google Scholar]
- Roth DL, Fredman L, Haley WE. 2015. Informal caregiving and its impact on health: a reappraisal from population-based studies. Gerontologist 55:309–19 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Savovic J, Turner RM, Mawdsley D, Jones HE, Beynon R, et al. 2018. Association between risk-of-bias assessments and results of randomized trials in Cochrane reviews: the ROBES meta-epidemiologic study. Am. J. Epidemiol. 187:1113–22 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schoenmakers B, Buntinx F, Delepeleire J. 2010. Factors determining the impact of care-giving on caregivers of elderly patients with dementia: a systematic literature review. Maturitas 66:191–200 [DOI] [PubMed] [Google Scholar]
- Schulz R 2019. The intersection of family caregiving and work: labor force participation, productivity, and caregiver well-being. In Current and Emerging Trends in Aging and Work, ed. Czaja S, Sharit J, James J, Grosch J. Berlin: Springer; In press [Google Scholar]
- Schulz R, ed. 2000. Handbook on Dementia Caregiving: Evidence-Based Interventions for Family Caregivers. Berlin: Springer [Google Scholar]
- Schulz R, Beach SR, Cook TB, Martire LM, Tomlinson JM, Monin JK. 2012. Predictors and consequences of perceived lack of choice in becoming an informal caregiver. Aging Mental Health 16:712–21 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schulz R, Beach SR, Friedman EM, Martsolf GR, Rodakowski J, James AE. 2018. Changing structures and processes to support family caregivers of seriously ill patients. J. Palliat. Med. 21:S36–42 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schulz R, Czaja SJ, Lustig A, Zdaniuk B, Martire LM, Perdomo D. 2009. Improving the quality of life of caregivers of persons with spinal cord injury: a randomized controlled trial. Rehab. Psychol. 54:1–15 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schulz R, Czaja SJ, McKay JR, Ory MG, Belle SH. 2010. Intervention taxonomy (ITAX): describing essential features of interventions. Am. J. Health Behav. 34:811–21 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schulz R, Eden J, eds. 2016. Families Caring for an Aging America. Washington, DC: Natl. Acad. Press; [PubMed] [Google Scholar]
- Schulz R, Hebert RS, Dew MA, Brown SL, Scheier MF, et al. 2007. Patient suffering and caregiver compassion: new opportunities for research, practice, and policy. Gerontologist 47:4–13 [DOI] [PubMed] [Google Scholar]
- Schulz R, Mendelsohn AB, Haley WE, Mahoney D, Allen RS, et al. 2003. End-of-life care and the effects of bereavement on family caregivers of persons with dementia. N. Engl. J. Med. 349:1936–42 [DOI] [PubMed] [Google Scholar]
- Schulz R, O’Brien AT, Bookwala J, Fleissner K. 1995. Psychiatric and physical morbidity effects of Alzheimer’s disease caregiving: prevalence, correlates, and causes. Gerontologist 35:771–91 [DOI] [PubMed] [Google Scholar]
- Schulz R, Sherwood P. 2008. Physical and mental health effects of family caregiving. Am. J. Nurs. 108:23–27 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schulz R, Tompkins CA. 2010. Informal caregivers in the United States: prevalence, caregiver characteristics, and ability to provide care In The Role of Human Factors in Home Health Care, Workshop Summary, pp. 117–43. Washington, DC: Natl. Acad. Press [Google Scholar]
- Schulz R, Wahl H, Matthews JT, De Vito Dabbs A, Beach SR, Czaja SJ. 2015. Advancing the aging and technology agenda in gerontology. Gerontologist 55:724–34 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Scott JL, Dawkins S, Quinn MG, Sanderson K, Elliott KE, et al. 2016. Caring for the carer: a systematic review of pure technology-based cognitive behavioral therapy (TB-CBT) interventions for dementia carers. Aging Mental Health 20:793–803 [DOI] [PubMed] [Google Scholar]
- Shaw C, McNamara R, Abrams K, Cannings-John R, Hood K, et al. 2009. Systematic review of respite care in the frail elderly. Health Technol. Assess. 13:1–224 [DOI] [PubMed] [Google Scholar]
- Simonelli C, Tripodi F, Rossi R, Fabrizi A, Lembo D, et al. 2008. The influence of caregiver burden on sexual intimacy and marital satisfaction in couples with an Alzheimer spouse. Int. J. Clin. Pract. 62:47–52 [DOI] [PubMed] [Google Scholar]
- Spillman BC, Pezzin LE. 2000. Potential and active family caregivers: changing networks and the “sandwich generation.” Milbank Q. 78:347–74 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Strawbridge WJ, Wallhagen MI. 1991Impact of family conflict on adult child caregivers. Gerontologist 31:770–77 [DOI] [PubMed] [Google Scholar]
- Torti FM, Gwyther LP, Reed SD, Friedman JY, Schulman KA. 2004. A multinational review of recent trends and reports in dementia caregiver burden. Alzheimer Dis. Assoc. Disord. 18:99–109 [DOI] [PubMed] [Google Scholar]
- van der Lee J, Bakker TJ, Duivenvoordenc HJ, Droes RM. 2014. Multivariate models of subjective caregiver burden in dementia: a systematic review. Ageing Res. Rev. 15:76–93 [DOI] [PubMed] [Google Scholar]
- Van Houtven CH, Coe NB, Skira MM. 2013. The effect of informal care on work and wages. J. Health Econ. 32:240–52 [DOI] [PubMed] [Google Scholar]
- Vandepitte S, Van Den Noortgate N, Putman K, Verhaeghe S, Verdonck C, Annemans L. 2016. Effectiveness of respite care in supporting informal caregivers of persons with dementia: a systematic review. Int. J. Geriatr. Psychiatry 31:1277–88 [DOI] [PubMed] [Google Scholar]
- Vazeou Nieuwenhuis A, Beach SR, Schulz R. 2018. Care recipient concerns about being a burden and unmet needs for care. Innov. Aging 2:igy026 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vitaliano PP, Zhang JP, Scanlan JM. 2003. Is caregiving hazardous to one’s physical health? A meta-analysis. Psychol. Bull. 129:946–72 [DOI] [PubMed] [Google Scholar]
- von Känel R, Mausbach BT, Patterson TL, Dimsdale JE, Aschbacher K, et al. 2008. Increased Framingham Coronary Heart Disease Risk Score in dementia caregivers relative to non-caregiving controls. Gerontology 54:131–37 [DOI] [PubMed] [Google Scholar]
- Warburton DER, Nicol CW, Bredin SSD. 2006. Health benefits of physical activity: the evidence. CMAJ 174:801–9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wasilewski MB, Stinson JN, Cameron JI. 2017. Web-based health interventions for family caregivers of elderly individuals: a scoping review. Int. J. Med. Inform. 103:109–38 [DOI] [PubMed] [Google Scholar]
- Wendler D, Rid A. 2011. Systematic review: the effect on surrogates of making treatment decisions for others. Ann. Intern. Med. 154:336–46 [DOI] [PubMed] [Google Scholar]
- Wolff JL, Kasper JD. 2006. Caregivers of frail elders: updating a national profile. Gerontologist 46:344–56 [DOI] [PubMed] [Google Scholar]
- Wolff JL, Spillman BC, Freedman VA, Kasper JD. 2016. A national profile of family and unpaid caregivers who assist older adults with health care activities. JAMA Intern. Med. 176:372–79 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yee J, Schulz R. 2000. Gender differences in psychiatric morbidity among family caregivers: a review and analysis. Gerontologist 40:147–64 [DOI] [PubMed] [Google Scholar]
- Zarit SH, Bangerter LR, Liu Y, Rovine MJ. 2017. Exploring the benefits of respite services to family caregivers: methodological issues and current findings. Aging Mental Health 21:224–31 [DOI] [PMC free article] [PubMed] [Google Scholar]