Abstract
Introduction
Radiation therapy is widely used for prostate cancer, but radiation‐induced sarcomas have been rarely reported.
Case presentation
A 77‐year‐old Japanese male was diagnosed with prostate cancer and received a combined androgen blockade and radiation therapy (total dose of 76 Gy). Five years after the radiation therapy, testicular pain and dysuria appeared. Computed tomography showed a soft tissue dense mass with invasion to the right subpubic ramus and prostate, mainly to the perineum. A needle biopsy revealed the pathological features of high‐grade sarcoma. The patient was diagnosed with radiation‐induced sarcoma based on the cancer's occurrence in the vicinity of the radiation field.
Conclusion
Although irradiation is one of the important treatments for prostate cancer, the risk of radiation‐induced malignancy should be considered.
Keywords: prostate adenocarcinoma, radiation therapy, radiation‐induced sarcoma
Abbreviations & Acronyms
- CT
computed tomography
- PET
positron emission tomography
- PSA
prostate‐specific antigen
- SIR
standardized incidence ratio
Keynote message
Radiation‐induced sarcomas, although very rare, have a poor prognosis once they occur. Radiation therapy is one of the important treatments for prostate cancer, but it is essential that physicians in clinical practice consider the risk of radiation‐induced cancer and proceed accordingly.
Introduction
Radiation therapy is one of the indispensable therapeutic approaches in the treatment of prostate cancer. A rare adverse event of this approach is radiation‐induced cancer, which may increase the frequency of bladder cancer and rectal cancer after radiation therapy.1 Radiation‐induced sarcomas after radiation therapy for prostate cancer are very rare, and few reports have been published in Japan.2, 3 Here we describe our patient's case of radiation‐induced sarcoma arising from soft tissue after irradiation for prostate cancer.
Case presentation
A 77‐year‐old Japanese male had been treated for prostatic hypertrophy and overactive bladder for 8 years. His serum PSA level was 5.49 ng/mL at periodic blood sampling. Based on the results of a needle biopsy of the prostate, he was diagnosed as having prostate cancer. His Gleason score was 3 + 4. Magnetic resonance imaging of the pelvis showed a tumor in the right marginal area of the prostate. CT showed no enlarged lymph nodes or distant metastases.
After 3 months of a combined androgen blockade, a total dose of 76 Gy was administered to the patient as intensity‐modulated radiation therapy (Fig. 1). The follow‐up after treatment showed no evidence of recurrence.
Figure 1.
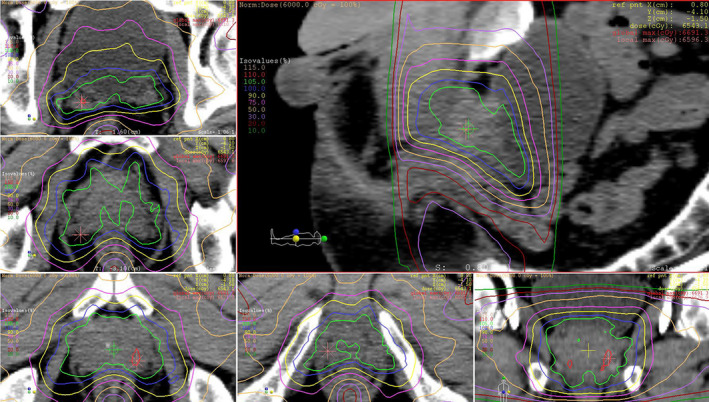
Dose distribution for prostate cancer.
Five years after the patient's radiation therapy, testicular pain and dysuria appeared. The PSA level at the time was 0.10 ng/mL. CT showed a soft tissue dense mass around the right pubic ischium and a subsequent perineal lesion. PET‐CT confirmed accumulation at the same sites (Fig. 2a–d). No enlarged lymph nodes or distant metastases were observed. A needle biopsy of the perineal lesion was performed. Microscopically, the lesion consists of atypical spindle and polygonal cells with brisk mitotic activity, atypical mitoses, and necrosis (Fig. 3a,b). Immunohistochemically, the lesion was positive for vimentin (Fig. 3c,d), and was no any pattern of protein expression that would permit more specific subclassification. A pathological diagnosis of high‐grade sarcoma was thus made.
Figure 2.

Axial CT scan. The patient's pelvis showing a mass around the right pubic ischium (a), and the subsequent perineal mass (b). PET‐CT confirmed accumulation at the same sites (c, d).
Figure 3.
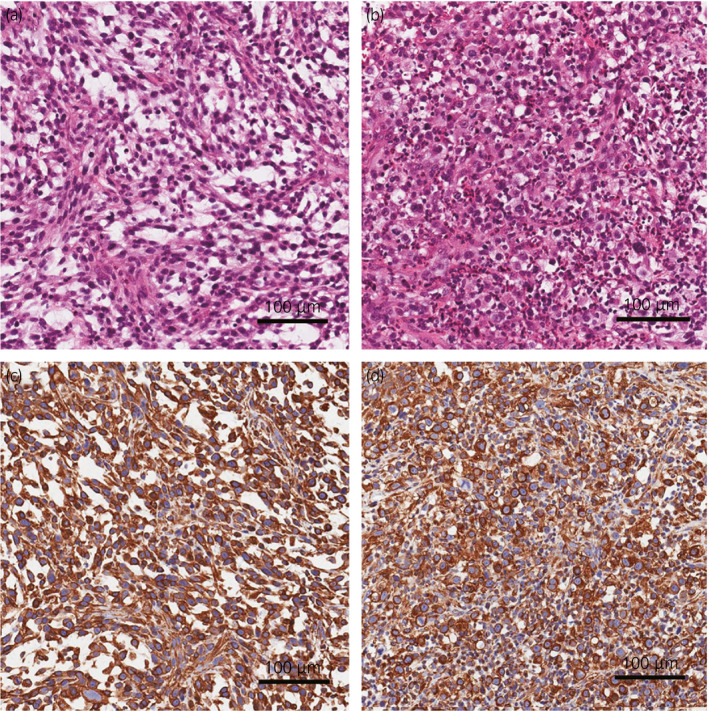
Hematoxylin and eosin staining showing spindle cells (a) and polygonal cells (b). Immunostaining by vimentin in the spindle cells (c) and polygonal cells (d).
He was treated with chemotherapy using doxorubicin. After two cycles of chemotherapy, CT revealed the growth of the original tumor without metastases, and the patient developed general malaise and anorexia. Because of these symptoms, the doxorubicin was discontinued, and he chose supportive care. He died 4 months after the start of doxorubicin treatment.
Discussion
Cahan et al. proposed a definition of radiation‐induced sarcoma that is based on the following criteria: (i) a second neoplasm occurs in the field of previous irradiation; (ii) the sarcoma of the irradiation lesion is histologically different from that of the primary cancer; and (iii) the incubation period from irradiation to sarcoma development is >5 years.4 Our patient's case fulfilled these criteria, and his tumor was diagnosed as a radiation‐induced sarcoma. Gladdy et al. reported that the median time from irradiation to the diagnosis of radiation‐induced sarcoma was 10 years (range 1.3–74 years).5 Although a shorter onset has been reported,6, 7 the criteria proposed by Cahan et al. require an incubation period of ≥5 years for the diagnosis of radiation‐induced sarcoma. A careful assessment may be necessary for the diagnosis of radiation‐induced sarcoma when the incubation period of the tumor is less than 5 years.
Radiation‐induced sarcoma has a poor prognosis. Cha et al. reported that the 1‐, 3‐, and 5‐year overall actuarial survival rates of surgically resected radiation‐induced sarcomas were 78%, 58%, and 41%, respectively.6 Patients who underwent complete resection had a 5‐year survival rate of 44%, compared with 27% for those with positive surgical margins. Kalra et al. reported that 42 patients with radiation‐induced sarcoma of bone had a 5‐year survival rate of 35% and that 30 of these patients, who were treated with the intention to cure, had a better survival rate of 41%.8 The remaining patients, who were treated palliatively, died within 2 years.
Various reports have described second malignancies after radiation therapy for prostate cancer. Pickles et al. reported an increase in bladder, testicular, and colorectal cancers, which are organs in and near the radiation field for prostate cancer.9 A meta‐analysis also indicated an increased risk of developing bladder, colorectal, and rectal cancers after radiation therapy.1 However, in a recent report by Hegemann et al., the second malignancies that occurred in patients who received radiation therapy for prostate cancer were induced by cigarette smoking and not by radiation therapy.10 The meta‐analysis by Wallis et al.1 lacks information on smoking; further studies to reduce bias are thus needed.
Sarcomas are rare, particularly after radiation therapy for prostate cancer. Brenner et al. used the results of the SEER Program Cancer Registry to investigate the frequency of second malignancies occurring after radiation therapy or surgery for prostate cancer.11 There were 38 sarcomas among the 51 584 patients who received irradiation, and the SIR of sarcomas in the treatment field was 1.80. Among the 70 539 patients who underwent surgery, the SIR was 1.02, suggesting that the risk of developing a sarcoma was significantly larger after radiation therapy compared to surgery. Pickles et al. also reported a 1.21 relative risk of sarcomas in their radiation therapy group.9
In Japan, only two cases of radiation‐induced osteosarcoma for prostate cancer have been reported.2, 3 Our present case report is, to our knowledge, the first of a soft tissue sarcoma after radiation therapy for prostate cancer in Japan.
Radiation therapy is a highly effective treatment option for prostate cancer. Regarding second malignancies after radiation therapy in this field, attention has been paid to only bladder cancer and colorectal cancer. However, radiation‐induced sarcomas, although very rare, have a poor prognosis once they occur. Physicians in clinical practice should be aware of the risk of radiation‐induced sarcoma following radiation treatment for prostate cancer.
Informed consent
Informed consent was not obtained from the patient because no identifying information is included in this article and the patient is now deceased.
Conflict of interest
The authors declare no conflict of interest.
Acknowledgment
This research was supported in part by a Health Labor Sciences Research Grant (H29‐ICT‐Ippan‐002) from the Ministry of Health, Labor and Welfare of Japan.
References
- 1. Wallis CJ, Mahar AL, Choo R et al Second malignancies after radiotherapy for prostate cancer: systematic review and meta‐analysis. BMJ 2016; 352: i851. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Nishiyama T, Ikarashi T, Terunuma M, Ishizaki S. Osteogenic sarcoma of the prostate. Int. J. Urol. 2001; 8: 199–201. [DOI] [PubMed] [Google Scholar]
- 3. Nukui F, Nagata M, Kurokawa J et al A case of osteosarcoma in pelvic bone following radiation therapy for prostate cancer. Nihon Hinyokika Gakkai Zasshi 2004; 95: 59–62. In Japanese. [DOI] [PubMed] [Google Scholar]
- 4. Cahan WG, Woodard HQ, Higinbotham NL, Stewart FW, Coley BL. Sarcoma arising in irradiated bone; Report of 11 cases. Cancer 1948; 1: 3–29. [DOI] [PubMed] [Google Scholar]
- 5. Gladdy RA, Qin LX, Moraco N et al Do radiation‐associated soft tissue sarcomas have the same prognosis as sporadic soft tissue sarcomas? J. Clin. Oncol. 2010; 28: 2064–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Cha C, Antonescu CR, Quan ML, Maru S, Brennan MF. Long‐term results with resection of radiation‐induced soft tissue sarcomas. Ann. Surg. 2004; 239: 903–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Dang ND, Teh BS, Paulino AC. Rhabdomyosarcoma arising in a previously irradiated field: an analysis of 43 patients. Int. J. Radiat. Oncol. Biol. Phys. 2013; 85: 598–603. [DOI] [PubMed] [Google Scholar]
- 8. Kalra S, Grimer RJ, Spooner D, Carter SR, Tillman RM, Abudu A. Radiation‐induced sarcomas of bone: factors that affect outcome. J. Bone Joint Surg. Br. 2007; 89: 808–13. [DOI] [PubMed] [Google Scholar]
- 9. Pickles T, Phillips N. The risk of second malignancy in men with prostate cancer treated with or without radiation in British Columbia, 1984–2000. Radiother. Oncol. 2002; 65: 145–51. [DOI] [PubMed] [Google Scholar]
- 10. Hegemann NS, Schlesinger‐Raab A, Ganswindt U et al Risk of second cancer following radiotherapy for prostate cancer: a population‐based analysis. Radiat. Oncol. 2017; 12: 2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Brenner DJ, Curtis RE, Hall EJ, Ron E. Second malignancies in prostate carcinoma patients after radiotherapy compared with surgery. Cancer 2000; 88: 398–406. [DOI] [PubMed] [Google Scholar]


