Abstract
Background
Physicians often have difficulty with prognostication and identification of patients who are in need of counseling about options for care at the end of life. Consequently, the objective of this study was to describe the initial stages in development of a computerized algorithm that will identify breast and lung cancer patients most in need of counseling about care options, including advance care planning, palliative care, and hospice.
Methods
Clinical and non-clinical data were extracted from the electronic medical record of breast and lung cancer patients admitted to a large, urban hospital for the year 2010. These data were used to create an electronic (e-EOL) algorithm designed to identify advanced cancer patients who could benefit from in-depth discussion about end-of-life care options.
Results
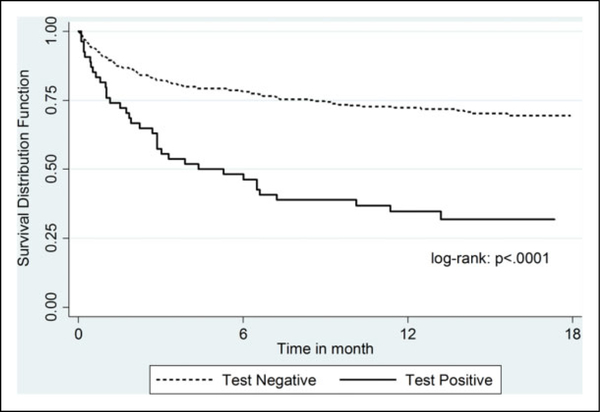
There were 369 eligible breast (42%) and lung (58%) cancer patients identified by ICD-9 code. The e-EOL algorithm identified 53 (14%) patients that met assigned criteria (presence of metastatic disease and albumin < 2.5 g/dl). The sensitivity, specificity, and positive predictive value of the first generation algorithm were 21%, 96%, and 91% when compared to physician expert chart review. Survival analysis showed that 6-month survival for algorithm positive cases was 46% versus 78% for algorithm negative cases, and 1-year survival was 32% versus 72%, respectively.
Conclusions
Initial testing of the e-EOL algorithm appears to be promising. Other markers of advanced illness will added to the algorithm to improve its test operating characteristics so it may be used to identify patients with poor prognosis in real time.
Keywords: health information technology, palliative care, end-of-life care, cancer, prognosis, electronic medical record, safety net
Introduction
Determining the prognosis for patients who are seriously or terminally ill is a challenge that many clinicians encounter. Although cancer often follows a steady decline in functional status and overall disease trajectory, it is still sometimes difficult for physicians to accurately give a prognosis to patients and their families. Prior research has shown that physicians are often inaccurate in their prognoses of the terminally ill, and they tend to be overly optimistic.1–3 Additional research has shown that in some cases, although some physicians have formulated a survival estimate for a patient, they may provide a frank estimate to the patient only 37% of the time and may provide no estimate, a conscious overestimate, or a conscious underestimate most of the time (63%)—even among patients with cancer.4 Even when physicians understand that their patients are in the last months of life, many are uncomfortable with discussing prognosis or end-of-life (EOL) care options, overstrained by the multiple challenges of discussing EOL issuesorlacktraininginhavingthesediscussions.5–9 This means that many patients with advanced cancer whose pain and symptoms may be better controlled with palliative care may not be offered this service, and patients who may qualify for hospice may only be offered this service late in their disease trajectory.
Knowledge of prognosis can have many implications for patients and their families. For instance, the Study to Understand Prognoses and Preferences for Outcomes and Risks of Treatments (SUPPORT) revealed that patients with metastatic(stage III or IV) colon and lung cancer who overestimated their chances of 6-month survival were more likely to favor life-extending therapy over comfort care compared to those who thought there was at least a 10% chance that they would not live 6 months.10 Other research has also shown that among terminally ill patients with cancer, those who accurately understood their prognosis were more likely to prefer comfort-oriented care and less likely to prefer life-prolonging treatments.11 Having knowledge of accurate prognosis gives patients and families the opportunity explore their options for care at the end of life and create an advance care plan if that is their desire.
In 2009, Congress passed the Health Information Technology for Economic and Clinical Health (HITECH) Act. One of the goals of the HITECH Act is to improve health care quality, safety, and efficiency, and in doing so, health care organizations are encouraged to implement certified electronic health record (EHR) technology to achieve significant improvements and advances in health care processes and outcomes.12,13 As a result, more and more health systems are adopting EHR technology for use in clinical practice and quality improvement initiatives. The Department of Health and Human Services and the Centers for Medicare and Medicaid Services have implemented policies to advance the “meaningful use” of HERs to make improvements in health care,12 including enhancing reporting of quality measures, provision of patient education, and documentation of advance directives.
In an effort to develop innovative, “meaningful uses” of EHRs, we have previously demonstrated the ability to use computerized algorithms to identify and stratify patients in real time with specific clinical conditions, who are at high risk of hospital readmission14–16 and predict inpatient risk of cardiopulmonary arrest.17 We hope to use this existing technology to assist physicians with difficulties in determining prognosis. The specific aims of this study were to (1) describe the initial stages in development of an electronic end-of-life (e-EOL) algorithm to identify patients hospitalized with advanced lung and breast cancer who meet criteria for an EOL care discussion; (2) evaluate the sensitivity, specificity, and predictive values of the algorithm compared to physician review; and (3) assess the construct validity of such an approach by examining overall survival rates among these patients. The ultimate goal of this study is to describe the development of a “first-generation” electronic algorithm that will lay the groundwork for a future computerized tool that may be used in real time to identify patients with advanced cancer who benefit from counseling about their options for care, including advance care planning, palliative care, and hospice if they desire it.
Methods
Study Population
The e-EOL algorithm was constructed using data from patients admitted to Parkland Hospital, a large urban, safety net hospital in Dallas, Texas, between January 1, 2010, to December 31, 2010, with the diagnosis of lung or breast cancer (with and without metastatic disease) as defined by the following International Classification of Diseases, Ninth Revision, Clinical Modification (ICD-9-CM) codes.18 The codes are as follows: for lung cancer (162, 162.0, 162.2, 162.3, 162.4, 162.5, 162.8, and 162.9), breast cancer (174, 174.0, 174.1, 174.2, 174.3, 174.4, 174.5, 174.6, 174.8, and 174.9), and metastatic disease or “secondary malignant neoplasm” (197.0, 197.1, 197.2, 197.3, 197.4, 197.5, 197.6, 197.8, 198.0, 198.1, 198.2, 198.3, 198.4, 198.6, 198.7, 198.8, and 199.0). The institutional review board at the University of Texas Southwestern Medical Center approved all the study procedures.
Data Collection and Creation of the e-EOL Algorithm
The e-EOL algorithm sought to identify patients hospitalized with lung or breast cancer, metastatic lung or breast cancer, and metastatic lung or breast cancer and an albumin of < 2.5 g/dL. We chose to include albumin level in the e-EOL algorithm because it is a marker that can be easily obtained from the EHR in a discrete field, at low levels suggests a limited prognosis,19 and is sometimes used as supportive evidence for hospice eligibility.20 For the purposes of this study, patients who were deemed eligible for in-depth discussion about EOL care options (advance care planning, palliative care, and hospice) were those who reviewers felt would be appropriate for hospice referral (reviewer “test-positive” cases). Those patients who had metastatic lung or breast cancer with an albumin of <2.5 g/dL were deemed e-EOL algorithm test-positive cases. Those who had only lung or breast cancer or metastatic lung or breast cancer with an albumin ≥2.5 g/dL were e-EOL algorithm “test-negative” cases. The presence of lung or breast cancer and metastatic disease was based on ICD-9 codes as noted previously. We also extracted from the EHR information on age, gender, race, ethnicity, marital status, insurance status, length of stay for the index hospitalization, discharge destination (ie, home, nursing home, hospice, etc) after the index hospitalization, emergency department (ED) visits, and hospitalizations in the prior 12 months. Survival status and date of death were extracted from the vital status section of the EHR, which included all deaths known to Parkland Health and Hospital System (PHHS) during and after the index admission. PHHS is an integrated delivery system, the sole safety net provider in Dallas County, and a dominant provider of palliative care to the uninsured in the region, so all or nearly all of the subsequent care and deaths in the county for these patients with advanced cancer would be expected to be recorded within the health system EHR.
Two physician reviewers (RR and SK) independently completed an implicit and explicit chart review of the most recent (index) hospitalizations for lung and breast cancer during the study period to identify eligible patients. Both physician reviewers were board certified in internal medicine and have served as attendings on the general medicine wards of 2 hospitals in the area. One physician reviewer was also board certified in hospice and palliative medicine. The physician reviewers underwent training and practice on a test set of 20 cases to create a reliable, shared understanding in their assessment of (1) the presence of advanced cancer and (2) a case meeting guideline criteria for hospice eligibility. Initial agreement for hospice eligibility determination, or interobserver reliability, was 90.5%. The physician reviewers independently reviewed all the cases without knowing the e-EOL algorithm results. They also extracted information about the hospitalization that was not electronically ascertainable including patients’ possession of an advance directive, identification of surrogate decision makers, palliative care consults, hospice referrals, do-not-resuscitate orders, and an estimate of the Karnofsky performance score (KPS). Any disagreements between reviewers were resolved by discussion and review of hospice eligibility criteria.
Statistical Analyses
We used descriptive statistics and 2-sample tests (chi-square, t test, Fisher exact test, or Wilcoxon rank sum tests, as appropriate) to characterize the baseline sociodemographic characteristics of the overall sample and compare subgroups. The physician determination of hospice eligibility was considered the gold standard for determination of reviewer test-negative and test-positive cases, and the e-EOL algorithm identified the algorithm test-positive and test negative patients. Based on this, we calculated the sensitivity, specificity, and positive and negative predictive values (and 95% confidence intervals [CIs]) for the e-EOL algorithm. As a measure of construct validity, we used Kaplan-Meier survival curves with the log-rank test to compare the overall survival of test-positive versus test-negative cases identified by the e-EOL algorithm.
Results
There were 387 patients identified as having lung or breast cancer who were hospitalized during the study period. Of those, 11 (3%) patients were excluded because they did not have definite diagnosis of lung or breast cancer on physician chart review (eg, benign lung mass, infectious lung mass, lung metastases but not primary lung cancer, necrotizing pneumonia, lung mass found to be anaplastic lymphoma, etc), and 7 patients had missing data. This left 369 patients for the analysis. More patients had lung cancer (58%) compared to breast cancer (42%). Table 1 shows the characteristics of cohort. Of the patients with lung cancer, 62% were male. All except one patient with breast cancer was female. The mean age of patients was 57.7 years. In terms of race and ethnicity, 48.2% were non-Hispanic black, 27.6% were non-Hispanic white, 3.5% were Asian, and 20.3% were Hispanic. Given the small number of Asians in the cohort, they were not included in the analyses noted in Table 1. Consistent with the sociodemographic characteristics of a safety net population, more than two-thirds (69%) of patients received county charity assistance, had Medicaid, or were uninsured. Only 6.8% had commercial insurance, and 24.2% had Medicare.
Table 1.
Baseline Characteristics of the Sample.
| Baseline characteristics | Total sample, N = 369 (%) | Physician reviewer test-positive cases, n = 230 (%) | Algorithma test-positive cases, n = 53 (%) | Algorithma test-negative cases, n = 316 (%) | P valuea |
|---|---|---|---|---|---|
| % Male | 136 (36.9) | 104 (45.2) | 28 (52.8) | 108 (34.2) | .009 |
| Mean age, years | 57.7 | 58.2 | 55.5 | 58.0 | .13 |
| Ethnicity | |||||
| Hispanic | 75 (20.3) | 43 (18.7) | 13 (24.5) | 62 (19.6) | .42 |
| Raceb | |||||
| Non-Hispanic white | 102 (36.6) | 58 (32.4) | 10 (25.6) | 92 (38.3) | .13 |
| Non-Hispanic black | 177 (63.4) | 121 (67.6) | 29 (74.4) | 148 (61.7) | |
| Marital statusb | |||||
| Married | 86 (23.9) | 54 (24.0) | 9 (17.7) | 77 (24.9) | .22 |
| Single | 139 (38.6) | 86 (38.2) | 17 (33.3) | 122 (39.5) | |
| Widowed | 48 (13.3) | 26 (11.6) | 7 (13.7) | 41 (13.3) | |
| Divorced/separated | 87 (24.2) | 59 (26.2) | 18 (35.3) | 69 (22.3) | |
| Insurance statusb | |||||
| Country program/uninsured | 132 (36.0) | 73 (32.0) | 14 (26.9) | 118 (37.5) | .30 |
| Medicare | 89 (24.2) | 59 (25.9) | 12 (23.1) | 77 (24.4) | |
| Medicaid | 121 (33.0) | 84 (36.8) | 23 (44.2) | 98 (31.1) | |
| Commercial | 25 (6.8) | 12 (5.3) | 3 (5.8) | 22 (7.0) | |
| Mean albumin | NA | 2.9 | 2.3 | 3.4 | <.001 |
| Mean number of ED visits | NA | 3.5 | 3.7 | 3.4 | .04 |
| Mean number of hospitalizations | NA | 2.5 | 2.8 | 2.4 | .08 |
| Mean LOS for index hospitalization, days | NA | 7.8 | 7.4 | 7.8 | .30 |
| KPS ≤50 | NA | 193 (83.9) | 44 (83.0) | 161 (51.0) | <.001 |
| Code status documented on admission of index hospitalization | NA | 107 (49.5) | 31 (67.4) | 76 (44.4) | .006 |
| Full code onb admission | NA | 62 (58.5) | 17 (54.8) | 45 (60.0) | .62 |
| Died during index hospitalization | NA | 59 (26.5) | 18 (34.6) | 43 (14.2) | <.001 |
Abbreviations: ED, emergency department; KPS, Karnofsky performance score; LOS, length of stay; NA, not applicable.
Chi-square, t test, Fisher exact test, or Wilcoxon rank sum test to compare test-positive and test-negative cases.
Limited to variable components with sufficient numbers for analysis.
Characteristics of the e-EOL Algorithm Test-Positive and -Negative Cases
Table 1 also shows how those flagged positive and negative by the e-EOL algorithm compared. A greater percentage of test-positive cases were men (52.8% vs 34.2%, P < .009), had a KPS of less than 50 (83.0% vs 51%, P < .001), and died during the index hospitalization (34.6% vs 14.2%, P < .001) than test-negative cases. There were no statistically significant differences by race, ethnicity, marital status, insurance status, number hospitalizations, or length of stay. Among the larger group of patients identified by the physician reviewers as eligible for EOL care, a greater percentage were men (45.2%), non-Hispanic black (54.8%), single (38.2%), or had Medicaid (36.8%). The majority (83.9%) had a KPS of 50 or less, and 26.5% died during their index hospitalization.
Performance of the e-EOL Algorithm
The e-EOL algorithm flagged 53 (14.3%) test-positive cases and 316 test-negative cases. The physician reviewers identified 230 test-positive cases (62.3%) and 139 test-negative cases. The specificity (96%; 95% CI: 93%−100%) and positive predictive value (91%; 95% CI: 83%−98%) of the e-EOL algorithm were high; however, the sensitivity (21%; 95% CI: 16%−26%) and negative predictive (42%; 95% CI: 37%−48%) value were low. The overall survival among patients flagged by the e-EOL algorithm was much worse indicating construct validity (see Figure 1). The 6-month survival rate for test-positive versus test-negative cases was 46.3% (95% CI: 32.7%−58.8%) versus 77.5% (95% CI: 72.6%−81.6%). One-year survival for test-positive versus test-negative cases was 31.8% (95% CI: 19.5%−44.8%) versus 71.9% (95% CI: 66.6%−76.4%).
Figure 1.
Survival for Algorithm Test Positive and Test Negative Cases.
End-of-Life Care Processes of Care
More than two-thirds of e-EOL algorithm test-positive cases had documentation of having a discussion about code status on admission during their index hospitalization and, of those patients, 54.8% were full code. Sixty percent of test-positive cases did not have a surrogate decision maker identified on admission; however, 57% of those did identify a surrogate decision maker within 48 hours of being admitted. Furthermore, 33% of test-positive cases were not referred to hospice during their index hospitalization.
Discussion
The use of the EHR and HIT is evolving beyond use for routine care and toward more “meaningful use” of data to improve processes and outcomes of care. In our study, we used data available in one of the most common commercially used EHRs to create an electronic algorithm to identify patients with advanced lung and breast cancer who were eligible for EOL care discussion according to national guidelines and clinical experience. The e-EOL algorithm used data on presence of metastatic disease and low albumin among patients with lung and breast cancer hospitalized at a large safety net hospital. The specificity and positive predictive value of the e-EOL algorithm were high at 96% and 91%, respectively, while the sensitivity and negative predictive value were low (21% and 42%); however, there was good construct validity with e-EOL algorithm-flagged cases having much worse survival rates.
The creation of the e-EOL algorithm and the subsequent analysis of the data yielded some very interesting results. Generation of the algorithm shows that the EHR can be used for more than just clinical practice. It is feasible to operationalize guidelines and identify patients with life-limiting illness and poor prognosis. For instance, in our study, we used discrete elements taken for the EHR to identify patients who were likely to have poorer prognosis and be most in need of discussion about EOL care options. The specificity and positive predictive value of the e-EOL algorithm were high. The test-positive cases were real cases, and there were very few false positives. Survival of the test-positive cases was much worse than the test-negative cases. In fact, only 46.3% of test-positive cases were alive at 6 months and 31.8% were alive at 1 year, further supporting evidence that creation of an electronic algorithm to assist health care providers in identifying these patients is a possibility. The sensitivity and negative predictive value, however, were not as good, which suggests that in future “generations” of the e-EOL algorithm additional variables should be added to the algorithm to make it more robust.
Studies have used the EHR to predict mortality and 30-day readmission rates of patients with common chronic medical conditions14–17,21; however, to our knowledge, this is the only study that uses electronic data in a way that will identify patients at the EOL. This first-generation algorithm was developed within the context of Parkland Hospital, the large safety net hospital system for Dallas County. Parkland services a large population of underrepresented minorities and those of low socioeconomic status—groups that historically do not participate in advance care planning, access palliative care, and utilize hospice services for a number of reasons, including lack of knowledge. The palliative care service has made inroads in those areas, however. We have found that once patients are referred to palliative care, there are no racial/ethnic differences in hospice referral or enrollment.22 Development of an algorithm to identify patients who are in need of palliative care and hospice services can counteract any “upstream barriers” to palliative care and hospice enrollment that may be encountered. The ultimate goal of development of this algorithm is to identify patients in real time who are most in need of counsel about advance care planning, palliative care, and hospice care. We then hope to develop educational interventions that will provide these patients with culturally sensitive counsel about their options for advance directive completion, palliative care and EOL care.
There are certain limitations that must be taken into account. This study was conducted using the EHR of one safety net hospital, which may hamper the generalizability of these findings to other settings. The EHR used here, however, is a commonly used system for mid-size and large medical groups, hospitals, and integrated care organizations.23 Furthermore, the data elements abstracted by the e-EOL algorithm are readily available in any EHR. This study consisted of a retrospective chart abstraction of test-positive and test-negative cases. Although the physician chart reviewers were blinded to which patients were test positive and test negative, some patients died during the course of the study, and this was documented in the medical record. This may have introduced a certain amount of selection bias in terms of the chart abstractors’ identification of patients. The goal of this algorithm will be to identify patients in real time; consequently, the selection bias identified by retrospective chart review will not be present. Despite these limitations, to our knowledge, this e-EOL algorithm is one of the first uses of EHR to identify patients with breast and lung cancer who are most in need of counsel about their options for advance care planning, palliative care, and hospice care. Furthermore, our analysis of survival among these patients suggests that most, if not all patients identified by the algorithm have a poorer prognosis, and should be informed about their options for care at the end of life.
Some would argue that all patients with metastatic cancer should be counseled about their options for EOL care. While we agree that these conversations should take place early within the disease trajectory, our goal was to identify those patients who are most in need of having discussions about advance care planning, palliative care for management of symptoms associated with their treatment or illness, and hospice for EOL care. One should note that this study was conducted in a safety net hospital system, and some patients have limited access to care. As a result, patients are often diagnosed late in the disease trajectory, and at a point where curative treatment is no longer an alternative. In reviewing the charts of test-positive patients who were hospitalized, we found that one-third did not have documentation of code status on admission, and of those who did, the majority (54.8%) wished to be full code on admission. We also found that on admission, most (60.8%) of these patients did not have a documented surrogate decision maker. These findings suggest that though conversations about goals of care should be conducted early in the disease trajectory, there is certainly opportunity for initiation of advance care planning in persons with limited life expectancy that may be getting missed.
The e-EOL algorithm test operating statistics showed that the algorithm has great specificity and positive predictive value, while the sensitivity and negative predictive value of the algorithm can still be improved upon. We plan to add additional parameters and variables to the next version of the algorithm to strengthen its sensitivity and negative predictive value. For instance, we hope to add markers of functional status and pain/symptom management needs (ie, documentation of opioid use, number of ER visits or hospitalizations for pain/symptom management related to the patient’s primary illness, markers of functional status, etc) that can be obtained in discreet EHR fields that will make the algorithm even more robust. We will also make note of the timing of albumin assessment, as low albumin may sometimes be a marker of acute rather than chronic illness. Our ultimate goal is to identify those who are at highest risk of having unmet needs at the end of life and design interventions that could assist in educating them about their options for EOL care. We feel that the e-EOL algorithm and development of culturally sensitive educational interventions could be extremely helpful to providers and certainly helpful to patients who receive care within safety net hospital systems who are historically underrepresented and underserved. Future research can and should include continued use of the EHR to identify patients with various chronic and life-limiting illnesses in efforts to provide them with the best possible palliative and EOL care.
Funding
The authors disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: This work was conducted with support from UT-STAR, NIH/NCATS Grant Number KL2TR000453 and AHRQ grant 1R24HS022418. The content is solely the responsibility of the authors and does not necessarily represent the official views of UT-STAR, UT Southwestern Medical Center and its affiliated academic and health care centers, the National Center for Advancing Translational Sciences, the National Institutes of Health, or the Agency for Healthcare Research and Quality.
Footnotes
Declaration of Conflicting Interests
The authors declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
References
- 1.Christakis NA, Lamont EB. Extent and determinants of error in doctors’ prognoses in terminally ill patients: prospective cohort study. BMJ. 2000;320(7233):469–472. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Glare P, Virik K, Jones M, et al. A systematic review of physicians’ survival predictions in terminally ill cancer patients. BMJ. 2003;327(7408):195–198.12881260 [Google Scholar]
- 3.Brandt HE, Ooms ME, Ribbe MW, van der Wal G, Deliens L. Predicted survival vs. actual survival in terminally ill noncancer patients in Dutch nursing homes. J Pain Symptom Manage. 2006;32(6):560–566. [DOI] [PubMed] [Google Scholar]
- 4.Lamont EB, Christakis NA. Prognostic disclosure to patients with cancer near the end of life. Ann Intern Med. 2001;134(12): 1096–1105. [DOI] [PubMed] [Google Scholar]
- 5.Calam B, Far S, Andrew R. Discussions of “code status” on a family practice teaching ward: what barriers do family physicians face? CMAJ. 2000;163(10):1255–1259. [PMC free article] [PubMed] [Google Scholar]
- 6.Galushko M, Romotzky V, Voltz R. Challengesin end-of-life communication. Curr Opin Support Palliat Care. 2012;6(3):355–364. [DOI] [PubMed] [Google Scholar]
- 7.Goelz T, Wuensch A, Stubenrauch S, et al. Specific training program improves oncologists’ palliative care communication skills in a randomized controlled trial. J Clin Oncol. 2011;29(25): 3402–3407. [DOI] [PubMed] [Google Scholar]
- 8.Gorman TE, Ahern SP, Wiseman J, Skrobik Y. Residents’ end-of-life decision making with adult hospitalized patients: a review of the literature. Acad Med. 2005;80(7):622–633. [DOI] [PubMed] [Google Scholar]
- 9.Rhodes RL, Tindall K, Xuan L, Paulk ME, Halm EA. Communication about advance directives and end-of-life care options among internal medicine residents. Am J Hosp Palliat Care. 2015;32(3):262–268. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Weeks JC, Cook EF, O’Day SJ, et al. Relationship between cancer patients’ predictions of prognosis and their treatment preferences. JAMA. 1998;279(21):1709–1714. [DOI] [PubMed] [Google Scholar]
- 11.Tang ST, Liu TW, Chow JM, et al. Associations between accurate prognostic understanding and end-of-life care preferences and its correlates among Taiwanese terminally ill cancer patients surveyed in 2011–2012. Psychooncology. 2014;23(7): 780–787. [DOI] [PubMed] [Google Scholar]
- 12.Blumenthal D, Tavenner M. The “meaningful use” regulation for electronic health records. N Engl J Med. 2010;363(6):501–504. [DOI] [PubMed] [Google Scholar]
- 13.The HITECH Act U.S. Department of Health & Human Services 2009; Web site. http://www.hhs.gov/ocr/privacy/hipaa/understanding/coveredentities/hitechact.pdf. Accessed June 23, 2015.
- 14.Singal AG, Rahimi RS, Clark C, et al. An automated model using electronic medical record data identifies patients with cirrhosis at high risk for readmission. Clin Gastroenterol Hepatol. 2013; 11(10):1335–1341. e1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Nijhawan AE, Clark C, Kaplan R, Moore B, Halm EA, Amarasingham R. An electronic medical record-based model to predict 30-day risk of readmission and death among HIV-infected inpatients. J Acquir Immune Defic Syndr. 2012;61(3):349–358. [DOI] [PubMed] [Google Scholar]
- 16.Amarasingham R, Moore BJ, Tabak YP, et al. An automated model to identify heart failure patients at risk for 30-day readmission or death using electronic medical record data. Med Care. 2010;48(11):981–988. [DOI] [PubMed] [Google Scholar]
- 17.Alvarez CA, Clark CA, Zhang S, et al. Predicting out of intensive care unit cardiopulmonary arrest or death using electronic medical record data. BMC Med Inform Decis Mak. 2013;13:28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Classifications of Diseases, Functioning, and Disability: International Classifications of Diseases, Ninth Revision, Clinical Modification (ICD-9-CM). Centers for Disease Control and Prevention, National Center for Health Statistics; Web site. http://www.cdc.gov/nchs/icd/icd9cm.htm. Accessed June 23, 2015. [Google Scholar]
- 19.Corti MC, Guralnik JM, Salive ME, Sorkin JD. Serum albumin level and physical disability as predictors of mortality in older persons. JAMA. 1994;272(13):1036–1042. [PubMed] [Google Scholar]
- 20.Medical Guidelines for Determining Prognosis in Selected Non-Cancer Diseases and Hospice Enrollment Criteria for End-Stage Dementia Patients. The National Hospice Organization; 1996. Web site. http://aspe.hhs.gov/daltcp/reports/impquesa.htm#appendixC. Accessed June 23, 2015. [DOI] [PubMed]
- 21.Makam AN, Nguyen OK, Moore B, Ma Y, Amarasingham R. Identifying patients with diabetes and the earliest date of diagnosis in real time: an electronic health record case-finding algorithm. BMC Med Inform Decis Mak. 2013;13:81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Rhodes RL, Xuan L, Paulk ME, Stieglitz H, Halm EA. An examination of end-of-life care in a safety net hospital system: a decade in review. J Health Care Poor Underserved. 2013;24(4): 1666–1675. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Epic Systems Corporation; 2015. Web site. http://www.epic.com/. Accessed June 23, 2015.