Abstract
Background
School-based injuries represent a sizeable portion of child injuries. This study investigated the rates of school-based injuries in Lebanon, examining injury mechanisms, outcomes and associated risk factors.
Methods
Data were prospectively collected by intern school nurses at 11 private schools for the 2018–2019 academic year. Descriptive and inferential analyses were performed. Chi-square comparisons were conducted to determine the significance of any differences in injury rates between boys and girls for each category of school.
Results
4,619 injury cases were collected. The yearly rate for school injuries was 419.1 per 1,000 children for the year 2018–2019. Boys demonstrated a significantly higher injury rate for all mechanisms of injuries, with the exception of being injured while walking, injured in the gym/sports areas, and other areas outside the playground and classroom. Elementary school children had the highest rate of injuries, nearly 2.4 times higher than kindergarten, 2.8 times higher than middle school, and 14.5 times higher than high school. Injuries to the face, upper extremities, and lower extremities were nearly 3 times more common than injuries to other areas of the body. Bumps/hits and bruises were most common—almost 3 times more likely than all other injury types. Injuries were mainly minor or moderate in severity—severe injuries were about 10 times less likely. Most injuries were unintentional, with rates nearly 5 times higher than those with unclear intent and 12 times higher than intentional injuries.
Conclusions
School injuries represent a relatively common problem. Compliance with playground safety standards coupled with the implementation of injury prevention strategies and active supervision at schools can curtail child injuries and ensure a safe and injury-free school environment.
Background
Injury accounts for a large share of the global burden of disease [1]. Child injury, in particular, is a substantial public health problem that claims more children’s lives than any major diseases combined [1]. Play- and sport-related injury is one of the leading causes of child injury worldwide [2–4]. Most of these injuries occur at school premises where children spend a considerable number of days per year. School-related injury is a major contributor to paediatric-related emergency department visits and hospital admissions; where the majority of the reported injuries were bruises, sprain/strains, and open wounds to the upper extremities, lower extremities and head, overwhelmingly sustained by boys, and mostly occurring during organized sports and recreational activities [5–10]. Injury studies conducted in the United States and Canada confirmed that school injuries accounted for almost 10 to 20% of the overall burden of child injury, costing billions of dollars in hospitalizations and other estimated health care expenditures [3, 6, 9, 10, 11].
An injury refers to the bodily harm sustained as the by-product of an external force and transfer of energy beyond an individual’s physiological tolerance resulting from an unsafe environment, conditions or behaviors [12]. Injuries can happen unintentionally, such as fall, drowning and burn, or intentionally, such as a purposeful assault by one individual upon another. In addition to the inflicted physical and psychological harms, child injuries impose financial repercussions on injured children and their families incurred due to healthcare expenditures, particularly in low- and middle-income countries where universal health coverage is most often lacking.
Limited research has explored child injuries in the Eastern Mediterranean Region, and few have examined the nature, extent and risk factors of school-based injuries in particular [13–22]. Among regional studies, the most commonly reported school injury type was a fracture, with the most prevalent injury cause being fall, sustained mainly by boys of younger age. Bullying, fights and physical attacks were also experienced by school children regionally [13–22]. In Lebanon, school-based injuries have received less attention in the injury research literature. A limited number of studies have focused on examining ‘bullying’ among school children and its impact on the child’s health and academic performance, while other studies reported physical, emotional and verbal abuse inflicted by teachers upon school children [23–25].
The education system in Lebanon follows the American or French system and includes grades 1 to 12 for children 5 to 18 years of age. Kindergarten years, not compulsory, begin before grade 1 and accommodate children ages 3 to 5 years, while elementary school encompasses grade 1 to grade 5, middle school grade 6 to grade 9, and high school grade 10 to grade 12. A typical academic year begins in mid-September or early October and ends in mid-June, for an average of 8.5 months of schooling per academic year. There are approximately 1,500 schools in Lebanon (58% public and 42% private), with a school attendance level of nearly 95 percent [26]. Private schools require payment of tuition fees, while public schools are free of charge, and are supported mainly by government funds and attended by less privileged families.
To the best of our knowledge, no previous studies have estimated injuries occurring at school premises in Lebanon. This underscores the importance of exploring physical injuries sustained by school children, and understanding their mechanisms, extent, and more importantly, their outcomes. The primary objective of this study was to assess the incidence of school-based physical injuries, to identify their characteristics, associated child behaviors, injury severity and potential contributing risk factors, based on analyzing school nurse reported incidents. Understanding the etiology of child school injuries is critical to help inform the design and development of school safety protocols and child injury prevention strategies and awareness programs at schools.
Methods
Participants
This cross-sectional prospective study collected injury data on school-based injuries throughout Lebanon. Within the context of this study, we focused on physical injuries, both intentional and unintentional, sustained by all school-age children and occurring within the premises of participating private schools.
In Lebanon, only private schools have sufficient resources to retain intern nurses who were available to complete injury incident report forms and collect data for this study. Therefore, only private schools with a nurse were invited to participate. Public schools and schools without an intern school nurse were excluded. A list of 74 private schools with nurses across various governorates in Lebanon was prepared. Each school was contacted, invited to participate and provided with an official letter of invitation directed to the school administration, explaining the objective and requirements of the study. Eleven schools agreed, representing a convenience sample of 14.8% of the total 74 schools. Across the 11 schools, a total of 74 school months of child injury data was gathered.
Instrument
A school injury surveillance tool was adapted from a validated Canadian school incident reporting system and was used to capture data at the participating schools. The surveillance tool was reviewed and contextualized with the assistance of school nurses from the Order of Nurses in Lebanon. To ensure validity and reliability, the tool was pilot-tested for one-year at 3 private schools located in the capital city, Beirut, during the academic year of September 2017 to June 2018. Lessons learned were documented and further refinement and modification were integrated into the tool. The final version was adopted in the current study, which was carried out during the academic year of September 2018 to June 2019.
Procedure
Once finalized, the incident data form—originally in English—was translated into French and Arabic to reflect the official language policy at each school, and to facilitate a rapid and efficient data collection process. The injury surveillance tool captured detailed information related to child school injuries, namely injury type, injury date, injury time and location, body part injured, injury intent, activity at the time of injury, contributing factors and injury severity (classified as minor, moderate or severe). The tool also collected child demographic information including child age, sex and grade level.
A soft copy of the injury surveillance tool was shared with each participating school nurse. Subsequent one-on-one training and monthly follow-up were carried out with school nurses to ensure a robust and efficient data collection process. All injuries that occurred at school premises were documented at the time the injury occurred. Collected data were reviewed to eliminate the possibility of any duplicate records. Cases of injury at home were excluded, and child identity information and personal details were concealed.
Human subjects approval statement
The study was approved by the American University of Beirut–Institutional Review Board (SBS-2018-0569). The study was also approved by each participating school administration.
Data analysis
Data collected from all schools were translated into one unified language (English), cleaned and compiled into one database. Data were analyzed using STATA, and used to assess injury incidence and to examine injury characteristics, identify keys trends and at-risk populations. Rates were calculated as the number of injuries per 1,000 students per month, to account for some schools having shorter academic years than others. Rates, with 95% confidence intervals, were calculated for boys and girls, for school grade, nature of the injury, intentionality, injury mechanism, injury severity, injury location, and injury type. Chi-square comparisons were conducted to determine the significance of any differences in injury rates between boys and girls for each grade. Due to the number of comparisons conducted, differences in injury rates were considered significant if p < 0.001.
Results
A total of 11 schools participated in this study, with a cumulative total of 4,619 school-based injuries reported during the study period. Across all schools, the incidence rate of injuries was 49.3 injuries per 1,000 students per month, which equates to 419.1 for an average 8.5-month academic year. An overwhelming number of boys reported a high injury rate of 61.4 per 1,000 students per month (95% CI 52.6, 70.2) compared to girls with a rate of 37.1 per 1,000 students per month (95% CI 28.3, 46.0), regardless of their ages. The study revealed that the injury rate was highest among elementary students (94.1 per 1,000 students per month, 95% CI 85.5, 102.7) and lowest among high school students (6.2 per 1,000 students per month, 95% CI 4.8, 7.5) Table 1.
Table 1. Characteristics of school injuries: Distribution of rates of injury intention, severity and location between gender, 2018–2019.
| Frequency (%) | Rate (per 1,000 students per month) (95% CI) | Gender Comparison | |||||
|---|---|---|---|---|---|---|---|
| Variable | Boys | Girls | Total | Boys | Girls | Overall | p-value |
| Overall | 2866 (62.0) | 1753 (38.0) | 4619 (100.0) | 61.4 (52.6, 70.2) | 37.1 (28.3, 46.0) | 49.3 (43.1, 55.5) | <0.0001 |
| School (Grade) | |||||||
| Kindergarten (KG 1–3) | 492 (60.4) | 322 (39.6) | 814 (17.6) | 48.1 (40.1, 56.1) | 31.5 (25.0, 38.0) | 39.8 (32.5, 47.1) | <0.0001 |
| Elementary (Grade 1–5) | 1899 (61.8) | 1173 (38.2) | 3072 (66.5) | 116.9 (107.4, 126.4) | 71.5 (63.9, 79.1) | 94.1 (85.5, 102.7) | <0.0001 |
| Middle (Grade 6–9) | 386 (64.8) | 210 (35.2) | 596 (12.9) | 41.2 (33.6, 48.8) | 20.4 (15.0, 25.8) | 30.3 (23.8, 36.8) | <0.0001 |
| High (Grade 10–12) | 85 (65.9) | 44 (34.1) | 129 (2.8) | 7.9 (6.4, 9.5) | 4.3 (3.2, 5.5) | 6.2 (4.8, 7.5) | <0.0001 |
| Unknown/Missing | 8 (0.2) | 0.1 (0.0, 0.2) | |||||
| Injury Location | |||||||
| Playground | 2041 (63.9) | 1151 (36.1) | 3192 (69.1) | 43.8 (40.2, 47.4) | 24.4 (21.8, 27.1) | 34.1 (30.9, 37.2) | <0.0001 |
| Classroom | 279 (62.3) | 169 (37.3) | 448 (9.7) | 6.0 (4.6, 7.3) | 3.6 (2.5, 4.6) | 4.8 (3.6, 6.0) | <0.0001 |
| Gym/Sports area | 119 (49.2) | 123 (50.8) | 242 (5.2) | 2.6 (1.7, 3.4) | 2.6 (1.7, 3.5) | 2.6 (1.9, 3.3) | 0.8694 |
| Other | 80 (50.3) | 79 (49.7) | 159 (3.4) | 1.7 (1.0, 2.4) | 1.7 (1.0, 2.4) | 1.7 (1.2, 2.2) | 0.8795 |
| Unknown/Missing | 578 (12.5) | 6.2 (4.8, 7.5) | |||||
| Intention | |||||||
| Unintentional | 1612 (62.5) | 966 (37.5) | 2578 (55.8) | 34.6 (31.4, 37.8) | 20.5 (18.0, 23.0) | 27.5 (24.7, 30.4) | <0.0001 |
| Intentional | 131 (72.8) | 49 (27.2) | 180 (3.9) | 2.8 (1.9, 3.7) | 1.0 (0.5, 1.6) | 1.9 (1.2, 2.7) | <0.0001 |
| Unclear | 327 (63.9) | 185 (36.1) | 512 (11.1) | 7.0 (5.6, 8.5) | 3.9 (2.8, 5.0) | 5.5 (4.2, 6.7) | <0.0001 |
| Unknown/Missing | 1349 (29.2) | 14.4 (12.3, 16.5) | |||||
School-related injuries were mostly unintentional with a rate of 27.5 (95% CI 24.7, 30.4), while 1.9 (95% CI 1.2, 2.7) were intentional, and 5.4 (95% CI 4.2, 6.7) had no clear intent. The rates of unintentional injuries were about 5 times higher than unclear intent and 14 times higher than intentional injuries. Further analysis showed an association between child sex and injury intent. Boys were responsible for significantly more intentional injuries than girls (p<0.0001) with injury rates of 2.8 (95% CI 1.9, 3.7) and 1.0 (95% CI 0.5, 1.6) respectively, and reported being involved in physical aggression and fights more often than their female counterparts.
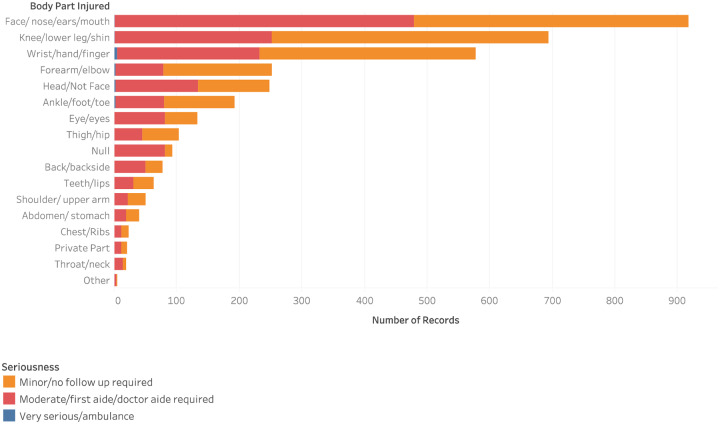
The most common nature of injury involved lower extremity injuries (14.2, 95% CI 12.2, 16.4), face (14.2, 95% CI 12.2, 16.3), and upper extremities (12.5, 95% CI 10.6, 14.4). Head injuries (4.4, 95% CI 3.2, 5.5) were the fourth most prevalent injury among school children (n = 409), of which 132 were moderate injuries and 3 were severe. Compared to girls, boys were significantly more likely to sustain injuries to all areas of the body (p<0.0001).
Various locations within schools contributed to different types and rates of injuries. The most commonplace for occurring injuries was the playground with a rate of 34.1 per 1,000 students per month (95% CI 30.9, 37.2), followed by classrooms with a rate of 4.8 (95% CI 3.6, 6.0). For these two locations, boys had significantly higher injury rates than girls (p<0.0001), but for all other locations, there were no significant differences in injury rates between the genders.
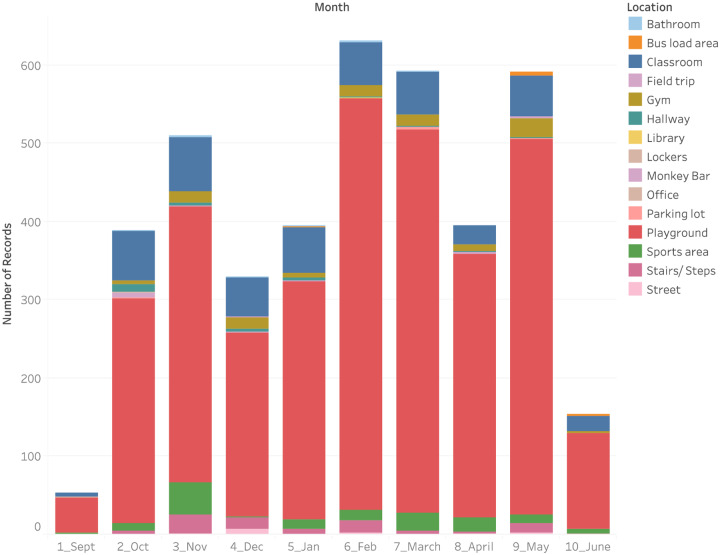
Seasonality was a predictor of injury. The analysis revealed a positive association between the injury nature and the warm season. The highest proportion of injuries occurred during February (12.8%), March (15.3%) and May (16.7%)—the month of April coincides with school closure during the Easter vacation (Fig 1).
Fig 1. Seasonal distribution of injuries by school location (Sept-June).
Playing, running, and walking were the most common mechanism of injury, with injury rates of 24.2 (95% CI 21.5, 26.9), 9.9 (95% CI 8.2, 11.6), and 2.7 (95% CI 1.8, 3.6) per 1,000 students per month, respectively. Boys had higher rates of injury while playing and running when compared with girls (p<0.0001), however, there were no significant differences between boys and girls for injuries sustained while walking.
Most school children reported mild to moderate injuries. The rate of minor injuries was 20.1 (95% CI 17.7, 22.5) as compared to moderate injuries (17.2, 95% CI 15.0, 19.5), which required basic first aid 45.9% of the time. Twelve cases of injury were severe (0.2, 95% CI 0.0, 0.4), necessitating medical attention at local hospitals Emergency Departments. Compared with girls, boys had a significantly higher injury rate for all three levels of injury severity (p<0.0001).
The response following the incident mainly depended on the seriousness of the injury. The most common response provided by the school nurse was to administer on-site care, which included the application of a ‘band-aide/bandage/ice’ in 64.6% of the cases, and ‘cleaned/washed/isolated wound/area’ in 26.9% of the cases (Fig 2).
Fig 2. Body parts affected by injuries and corresponding severity.
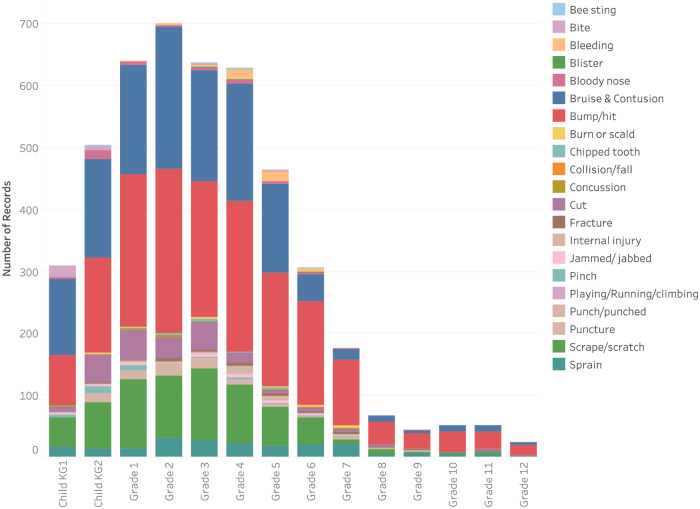
The injury types with the highest rate were bumps/hits (19.3, 95% CI 16.9, 21.7), bruises (13.6, 95% CI 11.6, 15.6), scrapes (7.2, 95% CI 5.8, 8.7), cuts (2.4, 95% CI1.6, 3.3) and sprains (2.4, 95% CI 1.4, 3.1). Boys had significantly higher rates for all common injury types (p<0.0001) except for sprains. A small number of injuries resulted in fractures (n = 39). Eye injuries (n = 184) and concussions (n = 14) were less common, though when they occurred, they were treated as major injuries with the potential for repercussions on the child’s cognitive capabilities and school performance Table 2 (Fig 3).
Table 2. The distribution of rates of injury mechanism, nature and types between gender.
| Frequency (%) | Rate (per 1,000 students per month) (95% CI) | Gender Comparison | |||||
|---|---|---|---|---|---|---|---|
| Variable | Boys | Girls | Total | Boys | Girls | Overall | p-value |
| Injury Mechanism | |||||||
| Playing | 1393 (61.5) | 872 (38.5) | 2265 (49.0) | 29.9 (26.9, 32.9) | 18.5 (16.2, 20.9) | 24.2 (21.5, 26.9) | <0.0001 |
| Running | 584 (62.9) | 344 (37.1) | 928 (20.1) | 12.5 (10.6, 14.5) | 7.3 (5.8, 8.8) | 9.9 (8.2, 11.6) | <0.0001 |
| Walking | 137 (54.6) | 114 (45.4) | 251 (5.4) | 2.9 (2.0, 3.9) | 2.4 (1.6, 3.3) | 2.7 (1.8, 3.6) | 0.1248 |
| Other | 340 (64.5) | 187 (35.5) | 527 (11.4) | 7.3 (5.8, 8.8) | 4.0 (2.8, 5.1) | 5.6 (4.3, 6.9) | <0.0001 |
| Unknown/Missing | 648 (14.0) | 6.9 (5.5, 8.4) | |||||
| Intention | |||||||
| Unintentional | 1612 (62.5) | 966 (37.5) | 2578 (55.8) | 34.6 (31.4, 37.8) | 20.5 (18.0, 23.0) | 27.5 (24.7, 30.4) | <0.0001 |
| Intentional | 131 (72.8) | 49 (27.2) | 180 (3.9) | 2.8 (1.9, 3.7) | 1.0 (0.5, 1.6) | 1.9 (1.2, 2.7) | <0.0001 |
| Unclear | 327 (63.9) | 185 (36.1) | 512 (11.1) | 7.0 (5.6, 8.5) | 3.9 (2.8, 5.0) | 5.5 (4.2, 6.7) | <0.0001 |
| Unknown/Missing | 1349 (29.2) | 14.4 (12.3, 16.5) | |||||
| Injury Nature | |||||||
| Upper Extremities | 730 (62.3) | 441 (37.7) | 1171 (25.4) | 15.7 (13.5, 17.8) | 9.4 (7.7, 11.0) | 12.5 (10.6, 14.4) | <0.0001 |
| Lower Extremities | 779 (58.2) | 560 (41.8) | 1339 (29.0) | 16.7 (14.5, 19.0) | 11.9 (10.0, 13.8) | 14.3 (12.2, 16.4) | <0.0001 |
| Face | 831 (62.3) | 502 (37.7) | 1333 (28.9) | 17.8 (15.5, 20.1) | 10.7 (8.9, 12.4) | 14.2 (12.2, 16.3) | <0.0001 |
| Head | 273 (66.7) | 136 (33.3) | 409 (8.9) | 5.9 (4.5, 7.2) | 2.9 (2.0, 3.8) | 4.4 (3.2, 5.5) | <0.0001 |
| Other | 190 (69.6) | 83 (30.4) | 273 (5.9) | 4.1 (3.0, 5.2) | 1.8 (1.0, 2.5) | 2.9 (2.0, 3.9) | <0.0001 |
| Unknown/Missing | 94 (2.0) | 1.0 (0.5, 1.6) | |||||
| Injury Type | |||||||
| Bump/Hit | 1133 (62.7) | 673 (37.3) | 1806 (39.1) | 24.3 (21.6, 27.0) | 14.3 (12.2, 16.4) | 19.3 (16.9, 21.7) | <0.0001 |
| Bruise | 785 (61.7) | 487 (38.3) | 1272 (27.5) | 16.9 (14.6, 19.1) | 10.3 (8.6, 12.1) | 13.6 (11.6, 15.6) | <0.0001 |
| Scrape/Scratch | 418 (61.7) | 260 (38.3) | 678 (14.7) | 9.0 (7.3, 10.6) | 5.5 (4.2, 6.8) | 7.2 (5.8, 8.7) | <0.0001 |
| Cut | 151 (66.5) | 76 (33.5) | 227 (4.9) | 3.2 (2.3, 4.2) | 1.6 (0.9, 2.3) | 2.4 (1.6, 3.3) | <0.0001 |
| Sprain | 115 (54.8) | 95 (45.2) | 210 (4.5) | 2.5 (1.6, 3.3) | 2.0 (1.2, 2.8) | 2.2 (1.4, 3.1) | 0.1455 |
| Other | 263 (62.5) | 158 (37.5) | 421 (9.1) | 5.7 (4.3, 7.0) | 3.4 (2.3, 4.4) | 4.5 (3.3, 5.7) | <0.0001 |
| Unknown/Missing | 5 (0.1) | 0.1 (0.0, 0.2) | |||||
| Injury Severity | |||||||
| Minor | 1130 (60.0) | 753 (40.0) | 1883 (40.8) | 24.3 (21.6, 26.9) | 16.0 (13.8, 18.2) | 20.1 (17.7, 22.5) | <0.0001 |
| Moderate | 1063 (65.9) | 551 (34.1) | 1614 (34.9) | 22.8 (20.2, 25.4) | 11.7 (9.8, 13.6) | 17.2 (15.0, 19.5) | <0.0001 |
| Severe | 12 (85.7) | 2 (14.3) | 14 (0.3) | 0.3 (0.0, 0.5) | 0.0 (0.0, 0.2) | 0.2 (0.0, 0.4) | <0.0001 |
| Unknown/Missing | 1108 (24.0) | 11.8 (9.9, 13.7) | |||||
Fig 3. Distribution of school injury by injury type across grade levels.
Discussion
This prospective study highlights the relevance of school injuries as a common public health problem affecting the health and well-being of school-aged children in Lebanon. Key findings from this study provide a novel and relatively comprehensive understanding of the characteristics, the extent and the rates of child school injuries occurring at private schools in Lebanon. Such important knowledge is necessary to design effective school injury prevention policies and programs going forward.
Relative to other regional studies, this study estimated a school injury rate of 419/1000, which is comparable to rates suggested by Eastern Mediterranean countries, including Jordan (437/1000), Egypt (385/1000), Oman (263/1000), and UAE (307/1000) [13–21], retrieved from the Global School-Based Students Health Survey (GSBHS). Findings from this study are consistent with similar school injury studies in the region namely, that ‘Fall’ injuries are the most common mechanism, particularly among boys of a young age [13–22].
The study findings align with international literature and suggest that boys sustain more school injuries than girls of similar age groups [9,11,15]. Boys have a significantly higher injury rate for all mechanisms of injury with the exception of injuries sustained while walking, and injuries occurring in sports areas. Increased rates of injuries among boys may be explained by the fact that boys are more active than girls of the same age; they tend to display greater risk-taking behavior while underestimating potential hazards and dangers associated with their activities [27].
This study confirms that the rate and severity of injuries decrease as children age. The injury rate for elementary school children was nearly 2.4 higher than kindergarten; 2.8 higher than middle school; and, 14.5 times higher than high school. Consequently, school injury prevention measures and safety strategies should target elementary school children as ‘populations at-risk’ for effective reduction of school-based injuries.
Most injuries were unintentional, with rates about 5 times higher than ‘unclear intention’ and 12 times higher than ‘intentional injuries’. Being a male student represents a predictor of incidents of intentional injuries exhibited mainly by aggressive behavior, physical assaults, fighting, and roughness. Accordingly, there is a need to address aggressive behaviour among school children and to consider the implementation of zero-tolerance policies towards bullying and fighting that frequently result in injuries among students.
This study agrees with previous research and shows the increased risk of various types of injuries (e.g. fractures, contusions and laceration) associated with informal recreational activities and unstructured play involving playgrounds [9,11, 28–30]. Playing was the most prevalent mechanism for injury, with rates 2.5 times higher than injuries sustained while running and over 4 times higher than all other causes of injuries. The majority of the reported school-based injuries occurred during recreational hours and were linked to playground activities, predominantly during the warmer season when children were able to play outdoors. Playground injuries were common among school children; they were associated with multiple hazards and were mainly due to poor design and lack of compliance with international playground and equipment safety standards (e.g. playground slide dimension, swing height, climbing elevation, impact-absorbent ground, protective surface, equipment spacing, etc.) [31,32]. An ample number of studies have shown the strong association between the height of playground equipment and the increased risk of head- and arm-related injuries due to falls, especially with the absence of impact-absorbent playground surfacing [33–35]. Compliance with playground safety standards effectively curtails the occurrence of playground injuries and reduces risks for serious injuries, particularly among young children. Unfortunately, a limited number of schools in Lebanon have a school safety protocol in place. Hence, establishing injury prevention protocols and introducing playground safety awareness programs to educate school children about the risk of injuries are essential to the prevention of school injuries [35–37]. Moreover, the lack of active supervision during recreational hours may be associated with increased rates of injuries. Bumps/hits and bruises were almost 3 times more likely to happen compared to all other injury types. Several studies have linked adult direct supervision and active observation of children to reduced occurrences of playground injuries [38–40]. Supervisors’ presence around children can help to enforce safe behavior and allow for timely intervention in case of aggressiveness and intentionally inflicted injuries among students.
Contrary to existing literature, our study reported a low rate of sports-related injuries compared to unstructured play activities [41–43]. This may be explained by a relatively limited organized sports activity at schools in Lebanon, related to their associated setting and facility costs. Previous research has encouraged schools to invest in expanding sports curriculum and engaging students in multiple sports and outdoor activities in an effort to reduce obesity and promote an active and healthy lifestyle [44]. Organized sports and structured outdoor activities should be encouraged and adopted by schools while ensuring a safe and injury-free environment by integrating evidence-based policies and safety protocols.
This study showed that the majority of reported injuries were mainly minor or moderate in severity; severe injuries were nearly 10 times less likely to occur. Nevertheless, injuries to the face, upper extremities, and lower extremities were reported to be the most common nature of injury, approximately 3 times higher than injuries to other parts of the body. The discrepancy between the number of reported concussion cases in this study vis-a-vis the number of moderate head and face injuries raises concern, especially that the latter are not documented as serious injuries or diagnosed as mild or moderate Traumatic Brain Injury (TBI). Concussions were judged and classified as mild to moderate injury, not serious enough to warrant medical attention and follow up. This misclassification may signal a lack of adequate knowledge among school nurses on the accurate assessment of the severity of head injuries sustained, especially concussions. Specific training in the early recognition and management of concussion is encouraged, as the consequences of untreated concussion can have a significant impact on the child’s health and well-being [45,46]. Additionally, these types of child injuries should be assessed by a certified professional or specialized physician prior to the child’s return to school and play.
Limitations
The study has some limitations to be acknowledged. The data collection was limited to private schools due to the fact that only private schools have nurses on-site to collect data and report child school injury incidents. This may affect the generalizability of the findings to the Lebanese school population as a whole. Further, given that only eleven of 74 private schools agreed to participate, there may be some limitation in generalizing the results to all private schools in Lebanon, though we have no reason to indicate that other private schools would be different from our study’s participating schools. Including only private schools in this study might also influence the reported rate of injuries as presumably private schools are relatively well-maintained with fewer overcrowded classrooms; students typically belonging to higher socioeconomic status families and more highly educated parents. In short, students in this study may be associated with multiple contributing factors linked to reduced injury morbidity and mortality rates [47–49]. Future communication with the Ministry of Health will be established to include public schools and compare findings from both private and public schools. A second limitation is related to the injury classification tool used by school nurses. Fractures and concussions were not classified as ‘severe injuries’, with the exception of a small number of cases. This may have impacted the rate and severity of the reported injuries at schools. Thirdly, not all variables were completely filled out, resulting in missing data. Most notable was that 29% of injury intent was missing, which would result in an underestimation of the injury intent rate. And lastly, this study documented child school injuries with no follow up to determine the effects of the sustained injuries in the longer term. For instance, the impact of the injury on children missing days of schools or any short or long-term consequences on students’ physical and/or academic performance.
Conclusions
This is a first-time study in Lebanon that quantifies child school injury rates, investigates injury types and mechanisms, and highlights their direct associated risk factors. Examining school-based injuries and their associated behavior and risk factors is crucial to designing and adopting effective injury prevention measures and strategies at schools in the future.
As part of growing older, children’s risky behavior varies, resulting in various types of injuries associated with children’s age, sex and their surrounding environment. In an attempt to curtail child injuries, there is a need to identify the mechanisms and underlying factors associated with these injuries. By recognizing, changing and controlling these factors, most children’s injuries can be prevented. Further study is needed to investigate the repercussion of moderate to severe injuries on a child’s health and academic performance.
Implications for school health
Findings from this study will be shared with the Ministry of Education and will call for the development and implementation of school safety protocols and strategies that align with international safety standards, mainly playground equipment safety. Promoting a safe and injury-free school environment is critical for the physical, emotional, and cognitive development and well-being of children. School administrators, teachers and nurses should mobilize the efforts to ensure child safety and reduce school-based injuries.
Moreover, this study calls for the implementation of a school-based injury surveillance tool and system that will serve as a platform to provide the evidence needed to design effective and strategic injury prevention programs and interventions at schools.
The study evidence will be utilized to design and develop educational training courses that will be offered to school nurses, administrators and coaches to impart necessary skills and adequate training on the latest injury prevention theories and best practices to effectively diagnose and manage severe school injuries, particularly traumatic brain injuries (concussions).
Supporting information
(XLSX)
Acknowledgments
The authors would like to greatly acknowledge participating schools. A special gratitude to all school nurses whose contribution was substantial in collecting injury data and completing this study.
Data Availability
All relevant data are within the manuscript and Supporting Information files.
Funding Statement
The author(s) received no specific funding for this work.
References
- 1.GBD 2017 Causes of Death Collaborators. Global, regional, and national age-sex-specific mortality for 282 causes of death in 195 countries and territories, 1980–2017: a systematic analysis for the Global Burden of Disease Study 2017. The Lancet. 8 November 2018;392:1736–88. 10.1016/S0140-6736(18)32203-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Hirschhorn RM, Kerr ZY, Wasserman EB, Kay MC, Clifton DR, Dompier TP, et al. Epidemiology of injuries requiring emergency transport among collegiate and high school student-athletes. Journal of athletic training. 2018. September;53(9):906–14. 10.4085/1062-6050-340-17 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Johnson BK, Comstock RD. Epidemiology of chest, rib, thoracic spine, and abdomen injuries among United States high school athletes, 2005/06 to 2013/14. Clinical journal of sport medicine. 2017. July 1;27(4):388–93. 10.1097/JSM.0000000000000351 [DOI] [PubMed] [Google Scholar]
- 4.Schneuer FJ, Bell JC, Adams SE, Brown J, Finch C, Nassar N. The burden of hospitalized sports-related injuries in children: an Australian population-based study, 2005–2013. Injury epidemiology. 2018. December;5(1):45 10.1186/s40621-018-0175-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Amanullah S, Heneghan JA, Steele DW, Mello MJ, Linakis JG. Emergency department visits resulting from intentional injury in and out of school. Pediatrics. 2014. February 1;133(2):254–61. 10.1542/peds.2013-2155 [DOI] [PubMed] [Google Scholar]
- 6.Aubertin P, Tanenbaum B, Fleet R. Don’t take down the monkey bars: Rapid systematic review of playground-related injuries. Canadian family physician. 2019. March 1;65(3):e121–8. [PMC free article] [PubMed] [Google Scholar]
- 7.Roach R, Maffulli N. Childhood injuries in sport. Physical Therapy in sport. 2003. May 1;4(2):58–66. [Google Scholar]
- 8.Limbos MA, Peek-Asa C. Comparing unintentional and intentional injuries in a school setting. Journal of school health. 2003. March;73(3):101–6. 10.1111/j.1746-1561.2003.tb03582.x [DOI] [PubMed] [Google Scholar]
- 9.Zagel AL, Cutler GJ, Linabery AM, Spaulding AB, Kharbanda AB. Unintentional Injuries in Primary and Secondary Schools in the United States, 2001‐2013. Journal of School Health. 2019. January;89(1):38–47. 10.1111/josh.12711 [DOI] [PubMed] [Google Scholar]
- 10.Bergeron N, Bergeron C, Lapointe L, Kriellaars D, Giannotti M, Al-Sahab B, et al. Epidemiology of acute soccer injuries in Canadian children and youth. Pediatric emergency care. 2011. February 1;27(2):81–5. 10.1097/PEC.0b013e3182094340 [DOI] [PubMed] [Google Scholar]
- 11.Josse JM, MacKay M, Osmond MH, MacPherson AK. School injury among ottawa‐area children: a population‐based study. Journal of school health. 2009. February;79(2):45–50. 10.1111/j.1746-1561.2008.00375.x [DOI] [PubMed] [Google Scholar]
- 12.Haddon W Jr. Advances in the epidemiology of injuries as a basis for public policy. Public health reports. 1980. September;95(5):411 [PMC free article] [PubMed] [Google Scholar]
- 13.Al-Hajj S, El Bcheraoui C, Daoud F, Khalil I, Moradi-Lakeh M, Abu-Raddad LJ, et al. Child and adolescent injury burden in the eastern Mediterranean region: findings from the Global Burden of Disease 1990–2017. BMC public health. 2020. December;20(1):1–0. 10.1186/s12889-019-7969-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Peyton RP, Ranasinghe S, Jacobsen KH. Injuries, violence, and bullying among middle school students in Oman. Oman medical journal. 2017. March;32(2):98 10.5001/omj.2017.19 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Altheeb A, Hussein H, Al Faisal W, AlBehandy N, Alshareef N, Wasfy A. Incidence and determinants of severity of unintentional injuries among students of private schools in Dubai: a cross-sectional study. Eastern Mediterranean health journal. 2017. January 1;23(1). [DOI] [PubMed] [Google Scholar]
- 16.Wahdan MM, Sayed AM, Elaziz KM, El-Hoseiny MM, Al-Gwaily MM. Prevalence of injuries among high school students in Eastern and Western parts of Cairo, Egypt. Injury. 2016. December 1;47(12):2650–4. https://www.cpsc.gov/s3fs-public/325.pdf [DOI] [PubMed] [Google Scholar]
- 17.Hesham ES, Fatma H, Suzan G. Cross-sectional study of injuries among school children in Ismailia governorate, Egypt. Injury prevention. 2012. October 1;18(Suppl 1):A117-. [Google Scholar]
- 18.Ozkan O. Incidence and outcomes of school‐based injuries during four academic years in Kocaeli, Turkey. Pediatrics international. 2016. August;58(8):732–9. 10.1111/ped.12909 [DOI] [PubMed] [Google Scholar]
- 19.Sirhan NA. Non-intentional injuries in adolescents and youth: facts and figures. Bahrain medical bulletin. 2012;34(1):37-. [Google Scholar]
- 20.Lithander J, Kindi HA, Tönjum AM. Loss of visual acuity due to eye injuries among 6292 school children in the Sultanate of Oman. Acta Ophthalmologica Scandinavica. 1999. December;77(6):697–9. 10.1034/j.1600-0420.1999.770619.x [DOI] [PubMed] [Google Scholar]
- 21.Jildeh C, Abdeen Z, Al Sabbah H, Philalithis A. Unintentional injuries among school-aged children in Palestine: findings from the National Study of Palestinian Schoolchildren (HBSC-WBG2006). International Journal of Population Research. 2013;2013 10.1155/2013/624245 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Livny A, Sgan‐Cohen HD, Junadi S, Marcenes W. Traumatic dental injuries and related factors among sixth grade schoolchildren in four Palestinian towns. Dental traumatology. 2010. October;26(5):422–6. 10.1111/j.1600-9657.2010.00922.x [DOI] [PubMed] [Google Scholar]
- 23.Al-Hajj S, Pawliuk C, Smith J, Zheng A and Pike I. History of injury in a developing country: a scoping review of injury literature in Lebanon. Journal of Public Health. 2020. [DOI] [PubMed] [Google Scholar]
- 24.El Bcheraoui C, Kouriye H, Adib SM. Physical and verbal/emotional abuse of schoolchildren, Lebanon, 2009. Eastern Mediterranean Health Journal. 2012;18(10):1011–1020. 10.26719/2012.18.10.1011 [DOI] [PubMed] [Google Scholar]
- 25.Khamis V. Bullying among school-age children in the greater Beirut area: risk and protective factors. Child Abuse Negl. 2015;39:137–146. 10.1016/j.chiabu.2014.08.005 [DOI] [PubMed] [Google Scholar]
- 26.Lebanon Education System Overview (2019). Retrieved online January 2020: https://education.stateuniversity.com/pages/827/Lebanon-EDUCATIONAL-SYSTEM-OVERVIEW.html
- 27.Morrongiello BA, McArthur BA, Spence JR. Understanding gender differences in childhood injuries: Examining longitudinal relations between parental reactions and boys’ versus girls’ injury-risk behaviors. Health psychology. 2016. June;35(6):523 10.1037/hea0000275 [DOI] [PubMed] [Google Scholar]
- 28.Petridou E, Sibert J, Dedoukou X, Skalkidis I, Trichopoulos D. Injuries in public and private playgrounds: the relative contribution of structural, equipment and human factors. Acta paediatrica. 2002. June;91(6):691–7. 10.1080/080352502760069133 [DOI] [PubMed] [Google Scholar]
- 29.Vollman D, Witsaman R, Comstock RD, Smith GA. Epidemiology of playground equipment-related injuries to children in the United States, 1996–2005. Clinical pediatrics. 2009. January;48(1):66–71. 10.1177/0009922808321898 [DOI] [PubMed] [Google Scholar]
- 30.Adelson SL, Chounthirath T, Hodges NL, Collins CL, Smith GA. Pediatric playground-related injuries treated in hospital emergency departments in the United States. Clinical pediatrics. 2018. May;57(5):584–92. 10.1177/0009922817732144 [DOI] [PubMed] [Google Scholar]
- 31.Canadian Standard Organization 2019. Children Playground and Equipment. Retrieved online November 2, 2019: https://www.cpsionline.ca/index.php?action=cms.trainCpsiResources
- 32.US Consumer Product Safety Commission. 2015. Public Playground Safety Handbook. 2019. Retrieved online November 2, 2019
- 33.Altmann A, Ashby K, Stathakis V. Childhood injuries from playground equipment. Hazard. 1996. December;29:1–2. [Google Scholar]
- 34.Howard AW, Macarthur C, Rothman L, Willan A, Macpherson AK. School playground surfacing and arm fractures in children: a cluster randomized trial comparing sand to wood chip surfaces. PLoS medicine. 2009. December 15;6(12):e1000195 10.1371/journal.pmed.1000195 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Laforest S, Robitaille Y, Lesage D, Dorval D. Surface characteristics, equipment height, and the occurrence and severity of playground injuries. Injury Prevention. 2001. March 1;7(1):35–40. 10.1136/ip.7.1.35 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Orton E, Whitehead J, Mhizha‐Murira J, Clarkson M, Watson MC, Mulvaney CA, et al. School‐based education programmes for the prevention of unintentional injuries in children and young people. Cochrane database of systematic reviews. 2016(12). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Göpfert A, Van Hove M, Emond A, Mytton J. Prevention of sports injuries in children at school: a systematic review of policies. BMJ open sport & exercise medicine. 2018. June 1;4(1):e000346. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Landen MG, Bauer U, Kohn M. Inadequate supervision as a cause of injury deaths among young children in Alaska and Louisiana. Pediatrics. 2003. February 1;111(2):328–31. 10.1542/peds.111.2.328 [DOI] [PubMed] [Google Scholar]
- 39.Morrongiello BA, Schell SL. Child injury: The role of supervision in prevention. American journal of lifestyle medicine. 2010. January;4(1):65–74. [Google Scholar]
- 40.Guilfoyle SM, Karazsia BT, Langkamp DL, Wildman BG. Supervision to prevent childhood unintentional injury: Developmental knowledge and self-efficacy count. Journal of child health care. 2012. June;16(2):141–52. 10.1177/1367493511423855 [DOI] [PubMed] [Google Scholar]
- 41.Räisänen AM, Kokko S, Pasanen K, Leppänen M, Rimpelä A, Villberg J, et al. Prevalence of adolescent physical activity-related injuries in sports, leisure time, and school: the National Physical Activity Behaviour Study for children and Adolescents. BMC musculoskeletal disorders. 2018. December;19(1):58 10.1186/s12891-018-1969-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Burchard R, Stolpp A, Kratz T, Efe T, Soost C, Forreiter C, et al. School sport-associated injuries in adolescents: A single center experience. Technology and health care. 2017. January 1;25(6):1053–9. 10.3233/THC-170931 [DOI] [PubMed] [Google Scholar]
- 43.Welton KL, Kraeutler MJ, Pierpoint LA, Bartley JH, McCarty EC, Comstock RD. Injury recurrence among high school athletes in the United States: A decade of patterns and trends, 2005–2006 through 2015–2016. Orthopaedic journal of sports medicine. 2018. January 2;6(1):2325967117745788 10.1177/2325967117745788 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Foster C, Moore JB, Singletary CR, Skelton JA. Physical activity and family‐based obesity treatment: a review of expert recommendations on physical activity in youth. Clinical obesity. 2018. February;8(1):68–79. 10.1111/cob.12230 [DOI] [PubMed] [Google Scholar]
- 45.Concussion Awareness Training Tool (CATT) (2019). Concussion Resources for School Professionals. Retrieved online January 2020 from: https://cattonline.com/wp-content/uploads/2018/08/Concussion-Resources-for-School-Professionals-CATT-V2-Sep-2019.pdf
- 46.Centre for Disese Control (2019). HEADS UP. Retrieved online January 2020 from: https://www.cdc.gov/headsup/index.html
- 47.Hong J, Lee B, Ha EH, Park H. Parental socioeconomic status and unintentional injury deaths in early childhood: consideration of injury mechanisms, age at death, and gender. Accident Analysis & Prevention. 2010. January 1;42(1):313–9. [DOI] [PubMed] [Google Scholar]
- 48.Birken CS, MacArthur C. Socioeconomic status and injury risk in children. Paediatrics & child health. 2004. May 1;9(5):323–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Potter BK, Speechley KN, Koval JJ, Gutmanis IA, Campbell MK, Manuel D. Socioeconomic status and non-fatal injuries among Canadian adolescents: variations across SES and injury measures. BMC public health. 2005. December;5(1):132. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
(XLSX)
Data Availability Statement
All relevant data are within the manuscript and Supporting Information files.