Background:
Revision anterior cruciate ligament (ACL) reconstruction has been documented to have worse outcomes than primary ACL reconstruction. The reasons remain varied and not completely understood.
Methods:
Patients undergoing revision ACL reconstruction were prospectively enrolled. Data collected included baseline demographics, surgical technique and pathological condition, prescribed rehabilitation instructions, and a series of validated patient-reported outcome instruments. Patients were followed for 2 years and asked to complete a set of outcome instruments identical to those completed at baseline. Subsequent surgical procedures on the ipsilateral knee were recorded. Regression analysis was used to control for age, sex, activity level, baseline outcome scores, and the above-mentioned rehabilitation-related variables in order to assess the factors affecting clinical outcomes 2 years after revision ACL reconstruction.
Results:
A total of 843 patients met the inclusion criteria and were successfully enrolled, and 82% (695) were followed for 2 years. Two rehabilitation-related factors were found to influence outcome. First, patients who were prescribed an ACL brace for their return to sports had a significantly better Knee injury and Osteoarthritis Outcome Score (KOOS) for sports and recreational activities at 2 years (odds ratio [OR] =1.50, 95% confidence interval [CI] = 1.07 to 2.11; p = 0.019). Second, patients prescribed an ACL brace for the postoperative rehabilitation period were 2.3 times more likely to have subsequent surgery by 2 years (OR = 2.26, 95% CI = 1.11 to 4.60; p = 0.024). The odds of a graft rerupture were not affected by any type of brace wear.
Conclusions:
Rehabilitation-related factors that the physician can control at the time of an ACL reconstruction have the ability to influence clinical outcomes at 2 years. Weight-bearing and motion can be initiated immediately postoperatively. Bracing during the early postoperative period is not helpful. Use of a functional brace early in the postoperative period was associated with an increased risk of a reoperation. Use of a functional brace for a return to sports improved the KOOS on the sports/recreation subscale.
Level of Evidence:
Prognostic Level I. See Instructions for Authors for a complete description of levels of evidence.
There is lack of consensus regarding the optimal postoperative rehabilitation elements that orthopaedic surgeons should prescribe following anterior cruciate ligament (ACL) reconstruction. In 2016, Budny et al. surveyed key professional groups of orthopaedic surgeons who performed ACL reconstructions (members of the American Orthopaedic Society for Sports Medicine and the Arthroscopy Association of North America) to better understand their preferences and trends1. When asked about postoperative rehabilitation factors, 69% (566) of 824 respondents stated that they preferred their patients to be fully weight-bearing immediately after surgery, 55% chose to use a range-of-motion brace locked in extension, 13% chose to use a rigid knee immobilizer, and 15% chose no immobilization for their postoperative care. In addition, functional bracing was preferred by 48% of the respondents, and 54% of those who used it preferred to have it in place for 6 to 12 months in the majority of the cases whereas 34% preferred a period of 1 to 2 years. Interestingly, these postoperative preferences did not change drastically from those in similar surveys performed in 19992 and 20063.
The literature on rehabilitation practices following primary ACL reconstruction is robust, with numerous Level-I and II studies evaluating and establishing appropriate approaches for postoperative rehabilitation protocols4-28. Unfortunately, the outcomes of revision ACL reconstruction are significantly worse than those of primary procedures, and many factors and variables may contribute to these disappointing results1,4-6. To our knowledge, rehabilitation practices after revision ACL reconstruction have not yet been evaluated. While some previous series of ACL reconstructions may have included some revisions, the studies typically have not delineated between primary and revision ACL reconstructions or excluded revision ACL reconstructions as part of the study design. We are not aware of any previously published studies of rehabilitation solely after revision ACL reconstructions.
The purpose of this study was to determine whether rehabilitation-related factors prescribed at the time of revision ACL reconstruction significantly influence 2-year outcomes as well as the prevalence of subsequent reoperations. Our hypothesis was that an immediate rather than a restricted passive/active range of motion and weight-bearing would result in improved outcomes without subsequent surgery. We also hypothesized that use of postoperative and functional return-to-sports braces would not improve sports-related function.
Materials and Methods
Study Design
The Multicenter ACL Revision Study (MARS) Group was formed to address the inferior outcomes typically seen following revision ACL reconstruction and to try to determine modifiable predictors of these worse outcomes29-31. The group was supported by the American Orthopaedic Society for Sports Medicine at both a board and a research committee level. Participation was offered to all members, and all of those who accepted participated in educational and study design meetings prior to patient enrollment. As previously described, the consortium is a group of 83 fellowship-trained sports surgeons working at 52 unique sites32,33, which are a mix of 29 private-practice sites (56%) and 23 sites employing academic surgeons (44%). To be included in the study, a surgeon had to review and understand the surgeon questionnaire, obtain and maintain institutional review board approval, and complete a training session that included assessment of the surgeons’ ability to agree on the type and severity of articular cartilage and meniscal injuries and input and review of the study design and patient inclusion criteria. Surgeons were allowed to perform the revision reconstruction as they desired. Allografts had to be obtained from a designated company (Musculoskeletal Transplant Foundation).
Study Population
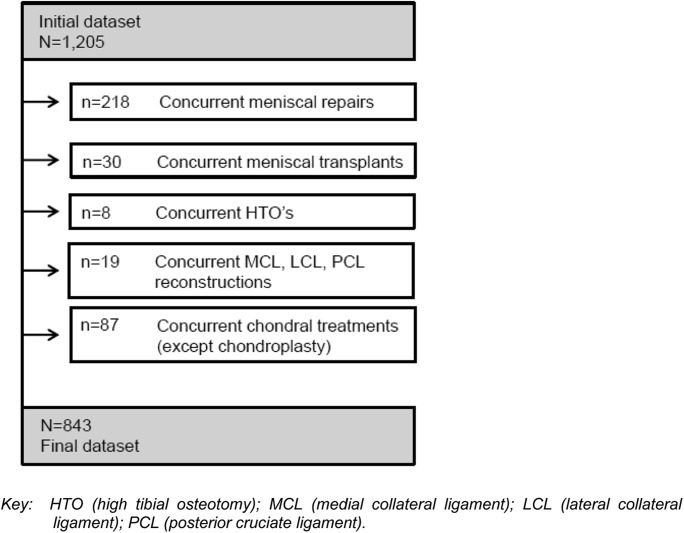
After institutional review board approval from each site, 1,205 patients scheduled to undergo revision ACL reconstruction surgery following failure of an ACL reconstruction graft qualified for and agreed to participate in this study. The multicenter group began patient enrollment in 2006 and ended it in 2011. All patients between 12 and 65 years of age who were scheduled to be treated with a revision ACL reconstruction to address ACL deficiency by a participating MARS surgeon at a MARS site were eligible for inclusion. Participants needed to have a known ACL reconstruction graft failure as defined by a KT-1000 (MedMetric) arthrometer showing >5 mm of laxity, a positive Lachman and/or pivot-shift test, or magnetic resonance imaging (MRI) demonstrating graft failure. Exclusion criteria were a previous ACL reconstruction or knee infection, arthrofibrosis, or complex regional pain syndrome. Screening logs were not kept at all sites, so it was not possible to determine an accurate enrollment percentage. For this particular study, we excluded enrolled patients from the data analysis who underwent, at the time of the revision surgery, concomitant procedures that would affect rehabilitation. These additional procedures included concurrent meniscal repairs, meniscal transplants, high tibial osteotomies, ligamentous reconstructions (of the medial collateral ligament, lateral collateral ligament, and/or posterior cruciate ligament), and certain chondral treatments (e.g., microfracture, abrasion arthroplasty, mosaicplasty, osteochondral autograft/allograft transplantation [OATS], and autologous chondrocyte implantation [ACI]). Figure 1 provides the study’s enrollment flow diagram.
Fig. 1.
Flow diagram of study cohort.
Data Sources and Measurement
Following informed consent, each patient filled out a 13-page questionnaire eliciting information about demographic characteristics, sports participation, mechanism of knee injury, and comorbidities. This questionnaire included a series of validated general and knee-specific outcome instruments: the Knee injury and Osteoarthritis Outcome Score (KOOS)34, the International Knee Documentation Committee (IKDC) Subjective Knee Form35,36, and the Marx activity rating scale37. MARS surgeons filled out a questionnaire on their impression of the etiology of the failure of the previous ACL reconstruction, the physical examination findings, the surgical technique utilized, and the meniscal and articular cartilage findings and their surgical management of these findings. Chondral damage was described using the modified Outerbridge system38, with grade II or higher defined as a “worse grade” in this study. Meniscal injuries were classified by location and whether they were partial or complete tears. We recorded treatment as none, repair, resection, or other, which included trephination and transplants. At the time of surgery, the physicians answered “yes” or “no” to questions regarding their prescription of postoperative rehabilitation and brace use: i.e., whether they planned to restrict passive range of motion postoperatively, restrict active range of motion postoperatively, restrict postoperative full weight-bearing, prescribe a motion control brace (i.e., a knee immobilizer) postoperatively, prescribe an ACL derotation brace to be used in the postoperative rehabilitation period, and prescribe an ACL derotation brace to be used when the patient returned to sports. If any of these were answered “yes,” the surgeon was instructed to fill in the number of days for which each prescription was to be followed (see Appendix).
Patient Follow-up
The questionnaire used at baseline was also completed at 2 years postoperatively. Patients were asked, by mail or telephone, whether they had undergone surgery subsequent to the revision reconstruction, and operative reports of all subsequent surgical procedures were obtained. Subsequent graft failure was verified by MRI report and/or arthroscopic confirmation.
Statistical Analysis
Continuous variables expressed as percentiles (i.e., 25th, 50th, and 75th) and categorical variables expressed as numbers and percentages were used to categorize our patient cohort. Independent predictors of outcome variables were identified via multivariable regression analyses. The primary outcome variables of interest were the 2-year outcome scores of the KOOS subscales and the IKDC, the Marx activity level, and the prevalence of subsequent surgery on the ipsilateral knee. The KOOS, IKDC, and Marx activity scores were all treated as continuous variables, whereas the prevalence of subsequent surgery was treated as binomial (yes/no). For the ordinal outcome variables (KOOS, IKDC, and Marx scores), a multivariable proportional odds model was fit because the data were not linear. A parametric model (e.g., linear regression) makes a linear assumption about the shape of the data that can lead to a model that does not reflect the true shape of the data. Hence, a proportional odds model fit the KOOS, IKDC, and Marx data more accurately. For the binary outcome variable (subsequent surgery), a multivariable logistic model was fit to the data. The covariates that we controlled for were age, sex, baseline activity level, baseline outcome scores, and the surgeon’s rehabilitation prescription—i.e., restriction of postoperative passive range of motion (yes/no), active range of motion (yes/no), and full weight-bearing (yes/no) and prescription of a motion control brace (i.e., knee immobilizer) postoperatively (yes/no), an ACL derotation brace in the postoperative rehabilitation period (yes/no), and an ACL derotation brace for return to sports (yes/no). According to the number of levels, categorical variables were fit according to their degrees of freedom (i.e., n − 1). To stay within the allowable degrees of freedom, each continuous variable was tested for a nonlinear relationship, with a p value of <0.05 indicating significance. Statistical analysis was performed using open-source R statistical software (www.r-project.org; version 3.0.3).
Results
Patient Population
A total of 843 patients met the inclusion criteria and were successfully enrolled. Fifty-seven percent (482) were male, and the median age in the entire cohort was 27 years. Baseline characteristics of the cohort are summarized in Table I.
TABLE I.
Baseline Cohort Characteristics
| Percentage (No.)* | Days†, If Yes | |
| Sex | ||
| Male | 57% (482) | |
| Female | 43% (361) | |
| Age† (yr) | 27 (20, 36) | |
| Baseline Marx activity level (range, 0-16)† | 11 (4, 16) | |
| Restriction of passive range of motion | ||
| No | 88% (745) | |
| Yes | 11% (94) | 14 (5, 28) |
| Blank | <1% (4) | |
| Restriction of active range of motion | ||
| No | 86% (722) | |
| Yes | 14% (115) | 16 (7, 30) |
| Blank | <1% (6) | |
| Restriction of postoperative full weight-bearing (without support) | ||
| No | 60% (507) | |
| Yes | 39% (332) | 21 (14, 28) |
| Blank | <1% (4) | |
| Prescription of motion control brace (i.e., knee immobilizer) postoperatively | ||
| No | 45% (380) | |
| Yes | 55% (458) | 24 (14, 42) |
| Blank | <1% (5) | |
| Prescription of ACL derotation brace for postoperative rehabilitation | ||
| No | 85% (715) | |
| Yes | 15% (124) | 180 (90, 365) |
| Blank | <1% (4) | |
| Prescription of ACL derotation brace for return to sports | ||
| No | 68% (573) | |
| Yes | 30% (253) | 365 (300, 365) |
| Blank | 2% (17) |
Except as indicated.
The values are given as the median (25th, 75th percentiles).
Two-Year Follow-up
At 2 years, the follow-up questionnaire was returned by 82% (695) of the 843 patients, and an answer to whether the patient had undergone any subsequent surgery was attained for 93% (782) of the 843 patients. Table II provides a comparison of demographic, surgical, and rehabilitation characteristics as well as baseline outcome measures between the patients who provided outcomes at 2 years and those who were lost to follow-up. We found a higher percentage of males in the group that did not return their 2-year follow-up questionnaires (70%) than in the cohort that did (55%). Body mass index (BMI) was also slightly higher in the group that was lost to follow-up. All other variables were fairly similar between groups.
TABLE II.
Comparison of Demographic, Surgical, and Rehabilitation Characteristics As Well As Baseline Patient-Reported Outcome Measures Between Patients with Follow-up and Those Lost to Follow-up
| Patients with Follow-up* (N = 695) | Patients Lost to Follow-up* (N = 148) | |
| Demographics | ||
| Sex | ||
| Male | 379 (55%) | 103 (70%) |
| Female | 316 (45%) | 45 (30%) |
| Age† (yr) | 28.9 ± 10.5, 27 (20, 36) | 28.0 ± 10, 25 (20, 34) |
| BMI† (kg/m2) | 25.9 ± 4.6, 25.1 (22.5, 28.3) | 26.9 ± 4.9, 26.5 (23.1, 30.5) |
| Smoking status | ||
| Never | 537 (77%) | 107 (72%) |
| Quit | 85 (12%) | 24 (16%) |
| Current | 63 (9%) | 13 (9%) |
| Blank | 10 (1%) | 4 (3%) |
| Education level† (yr of school) | 14.7 ± 2.9, 15 (12, 17) | 14.3 ± 3.0, 14 (12, 16) |
| Surgical | ||
| Time from last ACL reconstruction† (yr) | 6.2 ± 6.0, 4.0 (1.5, 10.0) | 4.5 ± 4.4, 3.0 (1.3, 6.5) |
| Graft type for revision | ||
| Autograft | 345 (50%) | 78 (53%) |
| Allograft | 329 (47%) | 64 (43%) |
| Both | 21 (3%) | 6 (4%) |
| Graft source for revision | ||
| Bone-patellar tendon-bone | 354 (51%) | 82 (55%) |
| Soft tissue | 333 (48%) | 63 (43%) |
| Other | 8 (1%) | 3 (2%) |
| Rehabilitation | ||
| Restriction of passive range of motion | ||
| No | 612 (88%) | 133 (90%) |
| Yes | 79 (11%) | 15 (10%) |
| Blank | 4 (<1%) | 0 |
| Restriction of active range of motion | ||
| No | 597 (86%) | 125 (84%) |
| Yes | 93 (13%) | 22 (15%) |
| Blank | 5 (<1%) | 1 (<1%) |
| Restriction of postoperative full weight-bearing (without support) | ||
| No | 417 (60%) | 90 (61%) |
| Yes | 275 (40%) | 57 (39%) |
| Blank | 3 (<1%) | 1 (<1%) |
| Prescription of motion control brace (i.e., knee immobilizer) postoperatively | ||
| No | 320 (46%) | 60 (41%) |
| Yes | 371 (53%) | 87 (59%) |
| Blank | 4 (<1%) | 1 (<1%) |
| Prescription of ACL derotation brace for postoperative rehabilitation | ||
| No | 595 (86%) | 120 (81%) |
| Yes | 96 (14%) | 28 (19%) |
| Blank | 4 (<1%) | 0 |
| Prescription of ACL derotation brace for return to sports | ||
| No | 482 (69%) | 91 (62%) |
| Yes | 197 (28%) | 56 (38%) |
| Blank | 16 (2%) | 1 (<1%) |
| Baseline patient reported outcomes† | ||
| IKDC | 52 ± 18, 52 (40, 63) | 50 ± 19, 51 (32, 65) |
| KOOS | ||
| Symptoms | 67 ± 20, 68 (54, 82) | 64 ± 21, 68 (50, 82) |
| Pain | 72 ± 19, 75 (61, 86) | 70 ± 22, 75 (56, 89) |
| Activities of daily living | 81 ± 18, 87 (69, 96) | 78 ± 22, 85 (68, 96) |
| Sports/recreation | 47 ± 28, 45 (25, 65) | 45 ± 27, 43 (25, 60) |
| Quality of life | 34 ± 20, 31 (19, 44) | 31 ± 22, 31 (13, 44) |
| Marx activity level | 9 ± 6, 11 (4, 16) | 9 ± 6, 10 (2, 14) |
The variables are reported as the number (percentage) except as indicated.
The variables are reported as the mean ± standard deviation, median (25th, 75th percentiles).
IKDC and KOOS subscale outcomes all significantly improved (p < 0.05) by 2 years as compared with baseline (Table III). Conversely, the Marx activity levels were significantly lower at 2 years. Eleven percent (88) of the 782 patients reported at least 1 subsequent surgical procedure on the ipsilateral knee within the 2-year follow-up period.
TABLE III.
Patient-Reported Outcomes and Prevalence of Subsequent Ipsilateral Knee Surgery at 2 Years
| Baseline | 2-Year Follow-up | |
| IKDC* | 52 (39, 64) | 78 (61, 87) |
| KOOS* | ||
| Symptoms | 68 (54, 82) | 79 (68, 89) |
| Pain | 75 (58, 86) | 89 (75, 97) |
| Activities of daily living | 87 (69, 96) | 97 (88, 100) |
| Sports/recreation | 45 (25, 65) | 75 (55, 90) |
| Quality of life | 31 (19, 44) | 62 (44, 75) |
| Marx activity level (range, 0-16)* | 11 (4, 16) | 7 (2, 12) |
| Subsequent ipsilateral knee surgery† | ||
| No | 82% (694) | |
| Yes | 10% (88) | |
| Unknown (unable to contact patient) | 7% (61) |
The variables are reported as the median (25th, 75th percentiles).
Revision ACL reconstruction, arthroscopic procedure for meniscal and/or chondral pathology, implant removal, etc.). The variable is reported as the percentage (number).
Rehabilitation Predictors of 2-Year Outcomes
Two rehabilitation-related factors were found to influence 2-year outcomes. First, patients who were prescribed an ACL derotation brace for their return to sports had significantly better KOOS sports/recreation scores at 2 years (odds ratio [OR] = 1.50, 95% confidence interval [CI] = 1.07 to 2.11; p = 0.019) compared with patients who were not prescribed an ACL brace. In other words, the odds of having a higher KOOS sports/recreation score increased by 50% in patients who were prescribed a functional brace for sports (versus patients who were not prescribed one). Second, patients who were prescribed an ACL derotation brace to be used in the postoperative rehabilitation period were 2.3 times more likely to have subsequent surgery by 2 years (OR = 2.26, 95% CI = 1.11 to 4.60; p = 0.024). Lower baseline outcome scores and a lower baseline Marx activity rating significantly increased the odds of reporting worse clinical outcomes on the IKDC, all KOOS subscales, and the Marx activity rating) at 2 years. Conversely, whether or not a physician restricted a patient’s passive or active range of motion postoperatively, restricted full weight-bearing without support, or prescribed a motion control brace postoperatively were all found to not be influential risk factors for 2-year outcomes in this revision cohort. In addition, 2-year activity levels were not influenced by whether a patient wore a brace.
Prevalence of Graft Failures with Brace Use
There were 25 confirmed graft failures over the 2-year follow-up period, for an overall graft failure rate of 3.2% (25 of 782). Of these 25 failures, 80% (20) occurred in subjects who had not been prescribed an ACL derotation brace for return to sports whereas 20% (5) occurred in subjects who had been prescribed an ACL derotation brace (intent-to-treat basis). As shown in Table I, 68% (573) of the 843 patients in the overall cohort were not prescribed an ACL functional brace for their return to sports, whereas 30% (253 of 843) were. As such, the expected frequency of graft failures among patients who were prescribed an ACL derotation brace for return to sports should have been 30%. However, although patients who were prescribed an ACL functional brace for their return to sports had a lower-than-expected frequency of graft failure (20% versus 30%), this difference was not significant (p = 0.23; chi-square = 1.414). Therefore, there was no difference between groups.
Discussion
As all sports surgeons know, postoperative rehabilitation can influence whether ACL reconstruction is a success or failure for the patient2,3,7,8,39. The best surgical procedure will fail if the rehabilitation is poorly or inappropriately performed. The protocol needs to protect the graft while regaining range of motion, strength, and proprioception. This needs to be accomplished in the most patient-friendly manner available to aid patient compliance. Many principles have been established as safe and improving outcomes in the primary ACL reconstruction setting. Whether or not these principles can be extended to the revision ACL reconstruction setting has not been established. A cohort study is way to analyze multiple variables given the challenge of accumulating a sufficient number of patients quickly enough to perform a randomized controlled study of revision ACL reconstruction.
This study enabled us to ask about and analyze a small number of important rehabilitation-related issues in the revision ACL reconstruction setting, including early versus delayed active and passive range of motion, immediate versus delayed weight-bearing, and rehabilitative and functional bracing. Range of motion has been analyzed in previous studies of primary ACL reconstructions7,40. Early initiation of extension and flexion has not been noted to be deleterious for the graft and may aid in obtaining a full range of motion. In this study, we confirmed that an early active and passive range of motion did not negatively impact outcome and can be allowed in the revision ACL reconstruction setting.
Early weight-bearing has been demonstrated to be safe and in fact decreases the risk of patellofemoral pain as evidenced by Level-I and II studies of primary ACL reconstruction25,41. In the current study, immediate weight-bearing did not have any negative impact on either reoperation rates or patient-reported outcomes.
At least 15 studies have analyzed rehabilitative bracing and motion control braces for rehabilitation after primary ACL reconstruction8-10,12-14,16,20-22,24,27,39,42,43. In aggregate, these studies did not support the use of these devices in the primary setting. In the current study, we analyzed this variable in the revision ACL reconstruction setting and found that use of these braces did not improve outcome. This allows surgeons to avoid their use in the absence of other surgical procedures that the surgeon believes require utilization of a motion control brace (meniscal repair and collateral ligament repair or reconstruction), which can decrease cost and improve patient satisfaction. Some surgeons prescribe an ACL derotation device (or “ACL functional brace”) during the postoperative rehabilitation period. There is little evidence regarding such utilization in any ACL reconstruction setting. Interestingly, in the current study, patients who were prescribed an ACL derotation brace in the rehabilitative phase were 2.3 times more likely to have subsequent surgery in the first 2 years of postoperative follow-up. It is not known why this may have occurred. Does the derotation brace have an inherent detrimental effect in this setting or does this finding reflect selection bias, confounding variables, or comorbidities? It appears counterintuitive to most clinicians. Two proposed mechanisms are (1) wearing a brace gave patients increased confidence and encouraged higher-level activity at an inappropriate time in their recovery and (2) these patients represented a cohort for which their surgeons thought the surgical reconstruction had not been as successful and needed additional protection and thus they were at a higher risk for outcomes requiring additional surgery.
Use of a functional ACL derotation brace for return to sports has been a controversial topic. Despite subjective hope that it might prevent future injury, evidence of a decreased likelihood of graft rupture or improved performance with their use has not been strong5,18. In the present study, prescribed use of a derotation brace for the return to sports was associated with a significant improvement in the score on the patient-reported KOOS sports/recreation subscale (OR = 1.50; p = 0.019) but had no effect on activity level or graft failure rates.
Strengths of this study include the fact that, to our knowledge, we analyzed the largest prospective cohort of revision ACL reconstructions ever reported. Its mix of private-practice and academic surgeons makes the results generalizable to the sports community. Our high rate of follow-up prevented attrition bias. Weaknesses include the lack of on-site follow-up. Not including graft choice in the model may be another important limitation. Also, as is a problem with rehabilitation studies in general, compliance with weight-bearing and brace wear during rehabilitation and return to sports was not known and could not be assessed in our study design. Individual prescribing practices and the indications used by the individual surgeons were not known. Some surgeons may only prescribe braces for patients who are absolutely committed to returning to sports.
Conclusions
There are rehabilitation-related factors that the physician can control at the time of an ACL revision that may have the ability to modify clinical outcomes at 2 years. Specifically, patients who were prescribed an ACL brace for return to sports had significantly better KOOS sports/recreation scores at 2 years and those who were prescribed an ACL brace for the postoperative rehabilitation period were 2.3 times more likely to have subsequent ipsilateral knee surgery by 2 years, independent of age and time of reinjury.
Appendix
Supporting material provided by the authors is posted with the online version of this article as a data supplement at jbjs.org (http://links.lww.com/JBJS/F235).
Acknowledgments
Note: The MARS group expresses its appreciation to the late Barton Mann, PhD (American Orthopaedic Society for Sports Medicine, Rosemont, Illinois), Timothy M. Hosea, MD (University Orthopaedic Associates LLC, Princeton, New Jersey), and Allen F. Anderson, MD (Tennessee Orthopaedic Alliance, Nashville, Tennessee), whose contributions to this work were of great importance.
Footnotes
Members of the MARS (Multicenter ACL Revision Study) Group include Rick W. Wright, MD; Laura J. Huston, MS; Samuel K. Nwosu, MS; Christina R. Allen, MD; Allen F. Anderson, MD; Daniel E. Cooper, MD; Thomas M. DeBerardino, MD; Warren R. Dunn, MD, MPH; Amanda K. Haas, MA; Brett (Brick) A. Lantz, MD; Barton Mann, PhD; Kurt P. Spindler, MD; Michael J. Stuart, MD; John P. Albright, MD; Annunziato (Ned) Amendola, MD; Jack T. Andrish, MD; Christopher C. Annunziata, MD; Robert A. Arciero, MD; Bernard R. Bach Jr., MD; Champ L. Baker III, MD; Arthur R. Bartolozzi, MD; Keith M. Baumgarten, MD; Jeffery R. Bechler, MD; Jeffrey H. Berg, MD; Geoffrey A. Bernas, MD; Stephen F. Brockmeier, MD; Robert H. Brophy, MD; Charles A. Bush-Joseph, MD; J. Brad Butler V, MD; John D. Campbell, MD; James L. Carey, MD, MPH; James E. Carpenter, MD; Brian J. Cole, MD; Jonathan M. Cooper, DO; Charles L. Cox, MD, MPH; R. Alexander Creighton, MD; Diane L. Dahm, MD; Tal S. David, MD; David C. Flanigan, MD; Robert W. Frederick, MD; Theodore J. Ganley, MD; Elizabeth A. Garofoli; Charles J. Gatt Jr., MD; Steven R. Gecha, MD; James Robert Giffin, MD; Sharon L. Hame, MD; Jo A. Hannafin, MD, PhD; Christopher D. Harner, MD; Norman Lindsay Harris Jr., MD; Keith S. Hechtman, MD; Elliott B. Hershman, MD; Rudolf G. Hoellrich, MD; Timothy M. Hosea, MD; David C. Johnson, MD; Timothy S. Johnson, MD; Morgan H. Jones, MD; Christopher C. Kaeding, MD; Ganesh V. Kamath, MD; Thomas E. Klootwyk, MD; Bruce A. Levy, MD; C. Benjamin Ma, MD; G. Peter Maiers II, MD; Robert G. Marx, MD; Matthew J. Matava, MD; Gregory M. Mathien, MD; David R. McAllister, MD; Eric C. McCarty, MD; Robert G. McCormack, MD; Bruce S. Miller, MD, MS; Carl W. Nissen, MD; Daniel F. O’Neill, MD, EdD; Brett D. Owens, MD; Richard D. Parker, MD; Mark L. Purnell, MD; Arun J. Ramappa, MD; Michael A. Rauh, MD; Arthur C. Rettig, MD; Jon K. Sekiya, MD; Kevin G. Shea, MD; Orrin H. Sherman, MD; James R. Slauterbeck, MD; Matthew V. Smith, MD; Jeffrey T. Spang, MD; Steven J. Svoboda, MD; Timothy N. Taft, MD; Joachim J. Tenuta, MD; Edwin M. Tingstad, MD; Armando F. Vidal, MD; Darius G. Viskontas, MD; Richard A. White, MD; James S. Williams Jr., MD; Michelle L. Wolcott, MD; Brian R. Wolf, MD; and James J. York, MD.
A commentary by Elizabeth Matzkin, MD, is linked to the online version of this article at jbjs.org.
Investigation performed at the Department of Orthopaedics, Washington University, St. Louis, Missouri, and the Department of Orthopaedic Surgery and Rehabilitation, Vanderbilt University, Nashville, Tennessee
Disclosure: This project was partially funded by Grant 5R01-AR060846 from the National Institutes of Health/National Institute of Arthritis and Musculoskeletal and Skin Diseases. On the Disclosure of Potential Conflicts of Interest forms, which are provided with the online version of the article, one or more of the authors checked “yes” to indicate that the author had a relevant financial relationship in the biomedical arena outside the submitted work (http://links.lww.com/JBJS/F234).
References
- 1.Budny J, Fox J, Rauh M, Fineberg M. Emerging trends in anterior cruciate ligament reconstruction. J Knee Surg. 2017. January;30(1):63-9. Epub 2016 Mar 28. [DOI] [PubMed] [Google Scholar]
- 2.Delay BS, Smolinski RJ, Wind WM, Bowman DS. Current practices and opinions in ACL reconstruction and rehabilitation: results of a survey of the American Orthopaedic Society for Sports Medicine. Am J Knee Surg. 2001. Spring;14(2):85-91. [PubMed] [Google Scholar]
- 3.Duquin TR, Wind WM, Fineberg MS, Smolinski RJ, Buyea CM. Current trends in anterior cruciate ligament reconstruction. J Knee Surg. 2009. January;22(1):7-12. [DOI] [PubMed] [Google Scholar]
- 4.Beynnon BD, Uh BS, Johnson RJ, Abate JA, Nichols CE, Fleming BC, Poole AR, Roos H. Rehabilitation after anterior cruciate ligament reconstruction: a prospective, randomized, double-blind comparison of programs administered over 2 different time intervals. Am J Sports Med. 2005. March;33(3):347-59. [DOI] [PubMed] [Google Scholar]
- 5.Birmingham TB, Bryant DM, Giffin JR, Litchfield RB, Kramer JF, Donner A, Fowler PJ. A randomized controlled trial comparing the effectiveness of functional knee brace and neoprene sleeve use after anterior cruciate ligament reconstruction. Am J Sports Med. 2008. April;36(4):648-55. Epub 2008 Jan 11. [DOI] [PubMed] [Google Scholar]
- 6.Christensen JC, Goldfine LR, West HS. The effects of early aggressive rehabilitation on outcomes after anterior cruciate ligament reconstruction using autologous hamstring tendon: a randomized clinical trial. J Sport Rehabil. 2013. August;22(3):191-201. Epub 2013 Apr 9. [DOI] [PubMed] [Google Scholar]
- 7.Fukuda TY, Fingerhut D, Moreira VC, Camarini PM, Scodeller NF, Duarte A, Jr, Martinelli M, Bryk FF. Open kinetic chain exercises in a restricted range of motion after anterior cruciate ligament reconstruction: a randomized controlled clinical trial. Am J Sports Med. 2013. April;41(4):788-94. Epub 2013 Feb 19. [DOI] [PubMed] [Google Scholar]
- 8.Grant JA. Updating recommendations for rehabilitation after ACL reconstruction: a review. Clin J Sport Med. 2013. November;23(6):501-2. [DOI] [PubMed] [Google Scholar]
- 9.Harilainen A, Sandelin J. Post-operative use of knee brace in bone-tendon-bone patellar tendon anterior cruciate ligament reconstruction: 5-year follow-up results of a randomized prospective study. Scand J Med Sci Sports. 2006. February;16(1):14-8. [DOI] [PubMed] [Google Scholar]
- 10.Harilainen A, Sandelin J, Vanhanen I, Kivinen A. Knee brace after bone-tendon-bone anterior cruciate ligament reconstruction. Randomized, prospective study with 2-year follow-up. Knee Surg Sports Traumatol Arthrosc. 1997;5(1):10-3. [DOI] [PubMed] [Google Scholar]
- 11.Henriksson M, Rockborn P, Good L. Range of motion training in brace vs. plaster immobilization after anterior cruciate ligament reconstruction: a prospective randomized comparison with a 2-year follow-up. Scand J Med Sci Sports. 2002. April;12(2):73-80. [DOI] [PubMed] [Google Scholar]
- 12.Hiemstra LA, Heard SM, Sasyniuk TM, Buchko GL, Reed JG, Monteleone BJ. Knee immobilization for pain control after a hamstring tendon anterior cruciate ligament reconstruction: a randomized clinical trial. Am J Sports Med. 2009. January;37(1):56-64. Epub 2008 Sep 18. [DOI] [PubMed] [Google Scholar]
- 13.Ito Y, Deie M, Adachi N, Kobayashi K, Kanaya A, Miyamoto A, Nakasa T, Ochi M. A prospective study of 3-day versus 2-week immobilization period after anterior cruciate ligament reconstruction. Knee. 2007. January;14(1):34-8. Epub 2006 Nov 28. [DOI] [PubMed] [Google Scholar]
- 14.Kartus J, Stener S, Köhler K, Sernert N, Eriksson BI, Karlsson J. Is bracing after anterior cruciate ligament reconstruction necessary? A 2-year follow-up of 78 consecutive patients rehabilitated with or without a brace. Knee Surg Sports Traumatol Arthrosc. 1997;5(3):157-61. [DOI] [PubMed] [Google Scholar]
- 15.Kruse LM, Gray B, Wright RW. Rehabilitation after anterior cruciate ligament reconstruction: a systematic review. J Bone Joint Surg Am. 2012. October 3;94(19):1737-48. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Lindström M, Wredmark T, Wretling ML, Henriksson M, Felländer-Tsai L. Post-operative bracing after ACL reconstruction has no effect on knee joint effusion. A prospective, randomized study. Knee. 2015. December;22(6):559-64. Epub 2015 Jun 6. [DOI] [PubMed] [Google Scholar]
- 17.Lobb R, Tumilty S, Claydon LS. A review of systematic reviews on anterior cruciate ligament reconstruction rehabilitation. Phys Ther Sport. 2012. November;13(4):270-8. Epub 2012 Jun 7. [DOI] [PubMed] [Google Scholar]
- 18.McDevitt ER, Taylor DC, Miller MD, Gerber JP, Ziemke G, Hinkin D, Uhorchak JM, Arciero RA, Pierre PS. Functional bracing after anterior cruciate ligament reconstruction: a prospective, randomized, multicenter study. Am J Sports Med. 2004. December;32(8):1887-92. [DOI] [PubMed] [Google Scholar]
- 19.Melegati G, Tornese D, Bandi M, Volpi P, Schonhuber H, Denti M. The role of the rehabilitation brace in restoring knee extension after anterior cruciate ligament reconstruction: a prospective controlled study. Knee Surg Sports Traumatol Arthrosc. 2003. September;11(5):322-6. Epub 2003 Jul 16. [DOI] [PubMed] [Google Scholar]
- 20.Mikkelsen C, Cerulli G, Lorenzini M, Bergstrand G, Werner S. Can a post-operative brace in slight hyperextension prevent extension deficit after anterior cruciate ligament reconstruction? A prospective randomised study. Knee Surg Sports Traumatol Arthrosc. 2003. September;11(5):318-21. Epub 2003 Jul 26. [DOI] [PubMed] [Google Scholar]
- 21.Möller E, Forssblad M, Hansson L, Wange P, Weidenhielm L. Bracing versus nonbracing in rehabilitation after anterior cruciate ligament reconstruction: a randomized prospective study with 2-year follow-up. Knee Surg Sports Traumatol Arthrosc. 2001;9(2):102-8. [DOI] [PubMed] [Google Scholar]
- 22.Muellner T, Alacamlioglu Y, Nikolic A, Schabus R. No benefit of bracing on the early outcome after anterior cruciate ligament reconstruction. Knee Surg Sports Traumatol Arthrosc. 1998;6(2):88-92. [DOI] [PubMed] [Google Scholar]
- 23.Noyes FR, Mangine RE, Barber S. Early knee motion after open and arthroscopic anterior cruciate ligament reconstruction. Am J Sports Med. 1987. Mar-Apr;15(2):149-60. [DOI] [PubMed] [Google Scholar]
- 24.Risberg MA, Holm I, Steen H, Eriksson J, Ekeland A. The effect of knee bracing after anterior cruciate ligament reconstruction. A prospective, randomized study with two years’ follow-up. Am J Sports Med. 1999. Jan-Feb;27(1):76-83. [DOI] [PubMed] [Google Scholar]
- 25.Tyler TF, McHugh MP, Gleim GW, Nicholas SJ. The effect of immediate weightbearing after anterior cruciate ligament reconstruction. Clin Orthop Relat Res. 1998. December;(357):141-8. [DOI] [PubMed] [Google Scholar]
- 26.van Grinsven S, van Cingel RE, Holla CJ, van Loon CJ. Evidence-based rehabilitation following anterior cruciate ligament reconstruction. Knee Surg Sports Traumatol Arthrosc. 2010. August;18(8):1128-44. Epub 2010 Jan 13. [DOI] [PubMed] [Google Scholar]
- 27.Wright RW, Fetzer GB. Bracing after ACL reconstruction: a systematic review. Clin Orthop Relat Res. 2007. February;455(455):162-8. [DOI] [PubMed] [Google Scholar]
- 28.Wright RW, Haas AK, Anderson J, Calabrese G, Cavanaugh J, Hewett TE, Lorring D, McKenzie C, Preston E, Williams G; MOON Group. Anterior cruciate ligament reconstruction rehabilitation: MOON guidelines. Sports Health. 2015. May;7(3):239-43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.MARS Group; MARS Group. Effect of graft choice on the outcome of revision anterior cruciate ligament reconstruction in the Multicenter ACL Revision Study (MARS) Cohort. Am J Sports Med. 2014. October;42(10):2301-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Group M. Factors influencing graft choice in revision anterior cruciate ligament reconstruction in the MARS Group. J Knee Surg. 2016. August;29(6):458-63. Epub 2015 Nov 20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Wright RW, Huston LJ, Spindler KP, Dunn WR, Haas AK, Allen CR, Cooper DE, DeBerardino TM, Lantz BB, Mann BJ, Stuart MJ; MARS Group. Descriptive epidemiology of the Multicenter ACL Revision Study (MARS) cohort. Am J Sports Med. 2010. October;38(10):1979-86. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Mars Group. The Development and Early to Midterm Findings of the Multicenter Revision Anterior Cruciate Ligament Study. J Knee Surg. 2016. October;29(7):528-32. Epub 2016 Jul 25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.MARS Group. Meniscal and articular cartilage predictors of clinical outcome after revision anterior cruciate ligament reconstruction. Am J Sports Med. 2016. July;44(7):1671-9. Epub 2016 May 9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Roos EM, Roos HP, Lohmander LS, Ekdahl C, Beynnon BD. Knee Injury and Osteoarthritis Outcome Score (KOOS)—development of a self-administered outcome measure. J Orthop Sports Phys Ther. 1998. August;28(2):88-96. [DOI] [PubMed] [Google Scholar]
- 35.Irrgang JJ, Anderson AF, Boland AL, Harner CD, Kurosaka M, Neyret P, Richmond JC, Shelborne KD. Development and validation of the international knee documentation committee subjective knee form. Am J Sports Med. 2001 Sep-Oct;29(5):600-13. [DOI] [PubMed] [Google Scholar]
- 36.Irrgang JJ, Anderson AF, Boland AL, Harner CD, Neyret P, Richmond JC, Shelbourne KD; International Knee Documentation Committee. Responsiveness of the International Knee Documentation Committee Subjective Knee Form. Am J Sports Med. 2006. October;34(10):1567-73. Epub 2006 Jul 26. [DOI] [PubMed] [Google Scholar]
- 37.Marx RG, Stump TJ, Jones EC, Wickiewicz TL, Warren RF. Development and evaluation of an activity rating scale for disorders of the knee. Am J Sports Med. 2001. Mar-Apr;29(2):213-8. [DOI] [PubMed] [Google Scholar]
- 38.Curl WW, Krome J, Gordon ES, Rushing J, Smith BP, Poehling GG. Cartilage injuries: a review of 31,516 knee arthroscopies. Arthroscopy. 1997. August;13(4):456-60. [DOI] [PubMed] [Google Scholar]
- 39.Elmqvist LG, Lorentzon R, Långström M, Fugl-Meyer AR. Reconstruction of the anterior cruciate ligament. Long-term effects of different knee angles at primary immobilization and different modes of early training. Am J Sports Med. 1988. Sep-Oct;16(5):455-62. [DOI] [PubMed] [Google Scholar]
- 40.Isberg J, Faxén E, Brandsson S, Eriksson BI, Kärrholm J, Karlsson J. Early active extension after anterior cruciate ligament reconstruction does not result in increased laxity of the knee. Knee Surg Sports Traumatol Arthrosc. 2006. November;14(11):1108-15. Epub 2006 Sep 6. [DOI] [PubMed] [Google Scholar]
- 41.Kruse LM, Gray BL, Wright RW. Anterior cruciate ligament reconstruction rehabilitation in the pediatric population. Clin Sports Med. 2011. October;30(4):817-24. Epub 2011 Aug 5. [DOI] [PubMed] [Google Scholar]
- 42.Hiemstra LA, Veale K, Sasyniuk T. Knee immobilization in the immediate post-operative period following ACL reconstruction: a survey of practice patterns of Canadian orthopedic surgeons. Clin J Sport Med. 2006. May;16(3):199-202. [DOI] [PubMed] [Google Scholar]
- 43.Villa FD, Ricci M, Perdisa F, Filardo G, Gamberini J, Caminati D, Villa SD. Anterior cruciate ligament reconstruction and rehabilitation: predictors of functional outcome. Joints. 2016. January 31;3(4):179-85. [DOI] [PMC free article] [PubMed] [Google Scholar]