The need for coordination of health care is a global issue, driven by increasing fragmentation across the health care system. Countries such as Australia, the United Kingdom, and New Zealand have all implemented strategies to improve coordination of care and address system fragmentation.1,2 In Canada, fragmentation exists across multiple sectors of care, notably primary care, which has been touted as the foundation for system improvement.3–6 In a survey of Commonwealth countries, Canada consistently lacked in health care coordination.7,8 Weak coordination negatively affects patients’ quality of care, access to care, and quality of life.6,7,9,10 Health care providers (HCPs) are also affected by system fragmentation owing to duplication of services, conflicting information from providers, and costs incurred by delays in care.10–12 The landscape of primary health care in Canada has been changing, with an increase in the different types of independent primary HCPs (eg, nurse practitioners, pharmacists).5 While this increase in available practitioners can support access to primary care, it can also result in a potential increase in fragmentation of care more broadly.
In Canada, the term siloization is often used to describe this fragmentation across sectors of care. Siloization refers to the lack of flow of information and resources between different sectors of care; this results in each sector of care operating in a manner isolated from the others within the same system. Siloization of health care in Canada is well documented.13,14 Within primary care, siloization limits the efficiency and effectiveness of care provision, and contributes to both fragmentation and reduced quality of care.15
Care coordination
Care coordination is “the deliberate organization of patient care activities … to facilitate the appropriate delivery of health care services.”11 Care coordination requires communication, trust, and collaboration; additionally, it requires practical channels through which HCPs can effectively coordinate care.11,13,16–19 Literature has demonstrated the functional and systematic benefits of a formalized care coordinator role, where coordinators manage and communicate patient information and needs across clinics and sectors. Coordinators are often responsible for in-person consultation with patients in their homes,20,21 and a care coordinator can facilitate the connection between a patient and the long-term care sector by connecting the patient to necessary services, resources, and support.20 While the effective use of coordinators for improving care and patient flow has been common in hospitals for decades,22 there remains a lack of consensus on a standard definition of care coordinator. The care coordination role has been successful at supporting transitions in care and managing continuity of care, most often from acute to subacute settings.6,23 Continuity of care is an essential element across high-performing health systems, and improvements to primary care coordination are a critical component of improving health system quality.24 Studies have shown that improvements in care coordination support a reduction in hospital admissions among patients with chronic conditions (except for those with mental illness) and reduced emergency department (ED) visits among older patients.10,19,25
Care coordination in primary care is a newer concept.26 While little to no evidence exists on the effectiveness of care coordination in primary care in Canada, a study in the United States showed no net savings for care coordination programs serving fee-for-service Medicare patients with chronic disease.27 More research is needed in this area.
Care coordination interventions can exist as communication and support for HCPs and patients28 or as structural arrangements to support the system.1 Interventions should be specific to the needs of patients and adaptable to various settings.16,29 Successful care coordination requires a culture of strong communication, support, trust, and collaboration, in addition to practical channels through which care practitioners can funnel that motivation to coordinate patients’ care.16,17
Comprehensive interventions to improve care coordination use multiple strategies and experience greater success in patient health and satisfaction. Strategies can be categorized into 2 groups: communication and support for HCPs and patients, and structural arrangements.16
Primary care is an essential focus of care coordination because the sector is a gateway to other health care services, and as such primary care is well suited to coordinate care for complex cases.30–32 In Ontario, family health teams (FHTs) were introduced as an intervention to facilitate coordinated care33 and to unite physician care with allied health providers in an interprofessional, team-based approach. However, many FHTs continue to experience a lack of care coordination.34
This commentary describes an innovative primary care coordination intervention called Primary Care Connections (PCC). We are highlighting the PCC intervention based on an availability (or convenience) approach28 (author D.R.D. works in the clinic where PCC was implemented). This does not serve as a formal evaluation of the intervention; our goal is to share the story of PCC and the lessons learned from its implementation to date.
Primary Care Connections
In 2016, an FHT in southwestern Ontario piloted the PCC care coordination quality improvement intervention. The PCC was grounded in recommendations for and enablers of coordination found in the literature.35 During the implementation of PCC, within the whole clinic, staff were encouraged to engage in smaller quality improvement interventions, focused on specific areas of care (such as diabetes or opioid use). Simultaneously, PCC used existing resources and streamlined existing structures to improve care provision for all patients.
Context
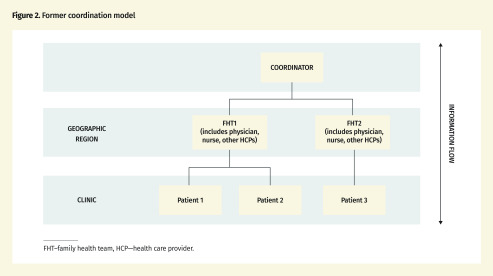
At the time of PCC’s implementation, the geographic region was organized under the South West Local Health Integration Network (LHIN). The South West LHIN served a population of nearly 1 million; approximately 30% lived rurally, 3% identified as Aboriginal, and 30% lived below the provincial low-income cutoff.36 The region experienced gaps in primary care including geographic inaccessibility, inaccessibility to culturally competent care, and a lack of after-hours care.37,38 Gaps were compounded by a lack of coordination. There were 19 FHTs within the South West LHIN. The clinic that implemented PCC is located in a suburban part of the larger city of London, Ont, and serves more than 100 000 patients and hosts more than 500 000 patient visits annually. The clinic is part of a large FHT with more than 115 providers operating across multiple sites within the region. From 2006 to 2016, community care access centres (CCACs) coordinated home, community, and long-term care in the province.39 In 2016, CCACs were subsumed under the LHINs, where care coordinators were assigned to a geographic region.39 The PCC brought care coordination into the clinic, closer to patients and care providers.
Actors
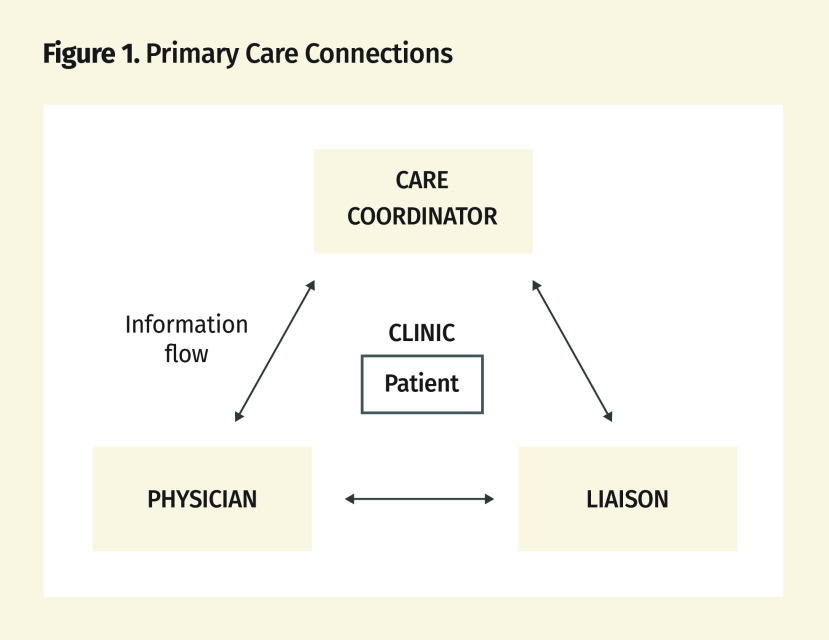
Within PCC, 3 roles were critical to patient coordination: the care coordination liaison, the care coordinator, and the physician (Figures 1 and 2).
Figure 1.
Primary Care Connections
Figure 2.
Former coordination model
FHT–family health team, HCP—health care provider.
Care coordinator.
When PCC was first implemented, there was 1 coordinator assigned to the clinic. This was later increased to 2 coordinators providing 1.5 full-time equivalents. This clinic-based care coordinator ensured patients received appropriate and efficient care. Under PCC, the clinic-based care coordinator caseload was limited to patients of the clinic (N = 17 000 to 18 000).
Under PCC, physician referrals for coordination of care were sent directly to the clinic-based care coordinator. This was more efficient than sending referrals to regional coordinators. The clinic-based care coordinators had access to patient health information through both the Client Health and Related Information System (CHRIS) and the clinic’s electronic medical record (EMR). The clinic-based care coordinators did not require any additional training to facilitate the implementation of PCC. They had extensive experience providing both primary and acute care within their current roles and related previous roles.
Care coordination liaison.
The care coordination liaison mediated communication between physicians, clinic-based care coordinators, and patients. The liaison required a robust skill set in disease management and system navigation, including a comprehensive knowledge of the system and available services. These skills and this knowledge allowed the liaison to be effective at supporting care coordination for patients within the clinic. The liaison worked at the clinic as an HCP in addition to the role for PCC; the liaison had access to the clinic’s CHRIS (through the coordinator) and the EMR.
To effectively support the coordinator and facilitate continuity of care, the liaison required extensive working knowledge of primary and acute care. Within the specific case presented, the liaison was a registered nurse, with relevant knowledge and experience working in primary and acute care; no additional training was required for this nurse. The liaison provided the coordinator with administrative support to facilitate the flow of information and resources between the coordinator and clinic.
Physician.
Within the clinic, the physician addressed patients’ care needs by providing diagnoses and managing treatment. While the physician is traditionally focused on the clinical aspects of care, the increasing emphasis on team-based care required that the physician provide additional support to facilitate the provision of coordinated care, including identifying patients requiring home care, monitoring patients’ health status, supporting home care providers, and supporting care transitions.
Successes and challenges
The PCC’s implementation included several successes and challenges that provide insight into its potential effectiveness in coordinating care.
Successes
Improved relationship between HCPs and patients: Experiential information suggests that PCC improved relationships between HCPs and patients. Clinic-based assignment of coordinators fostered trust between patients and the liaison and coordinators with their existing physicians and clinic. This association combated misconceptions of coordinators being outsiders with access to patients’ private information. Under PCC, patients came to view coordinators as a reliable resource.
Improved communication: The PCC streamlined information flow within the clinic and between the clinic and patients. Before PCC, the clinic would contact the CCACs to access information (through CHRIS). Under PCC, the clinic’s liaison could access this information through CHRIS and the EMR. This increased access to information enabled HCPs to more effectively address patient concerns and questions. This improved communication between the clinic and patients.
Improved quality of care: Knowledge of the system, clinic history, protocols, communication lines, and caseload positioned the liaison to more quickly and nimbly address patients’ needs. This ensured that patients received the most appropriate care when needed and supported more preventive care for patients.
Challenges
Relationship dynamics: The PCC’s success depended heavily on supportive working relationships. Unfortunately, the demanding nature of the coordinators’ role contributed to a high turnover rate. This often meant the coordinators’ tacit knowledge, which contributed to the success of the working relationships, was lost when there was transition. This also meant relationships with coordinators took time to build and might not have reached their full potential.
Procedure and culture: Implementation of PCC required reassignment of patient cases that were the responsibility of multiple coordinators, to 2 coordinators. The workload associated with organizing and monitoring the increased caseload, in addition to daily coordination activities, was demanding. Consequently, there was a need for forming procedures to support the coordinators. This also required a substantial culture change within the clinic. Often, navigational knowledge is tacit and experiential.40 The implementation process demonstrated that a lack of knowledge and skills negatively affects working relationships and PCC’s overall success. Early in PCC’s implementation, the coordinator lacked sufficient navigational skills and systems knowledge to manage the needs of the clinic; consequently, the implementation stagnated. When the coordinator was changed to an individual with a more robust skill set and knowledge base, the perceived effectiveness of PCC improved.
It took approximately 2 years to shift the culture and establish the liaison as the authority on care coordination.
Evaluation metrics: It was challenging to determine evaluation metrics for PCC. Most information pertaining to PCC’s effectiveness and efficiency came from staff and patient experiences. This tacit information coupled with the small patient population served (relative to the catchment) made it challenging to use traditional metrics (eg, ED visits, ED admissions) to prove the effectiveness of the intervention.
The next steps for PCC might include embedding formal evaluation metrics to better understand the effects on provider and patient experiences and determine the benefits associated with the intervention. However, there remains a lack of agreement in the literature on the best way to do these complex evaluations.41 As a main goal of care coordination is to meet patients’ needs and preferences in the delivery of high-quality, high-value health care, evaluation should be done using a mixed-method approach. The approach should consider both qualitative factors (such as patient and provider experiences) as well as quantitative elements (such as cost effectiveness and health outcomes). Further, evaluation should be done using an integrated knowledge translation approach that involves all stakeholders (from providers to patients and family) in the evaluation planning.42 While an evaluation of this nature was beyond the scope of this commentary, the lessons learned from our description of the PCC implementation can help support the current transformations in our health care system.
Lessons learned
The liaison and coordinators’ considerable workload and limited time required robust time management and communication skills. Strong communication is linked to improved collaboration, quality of care, and patient outcomes.43 Compartmentalization as a time management strategy allowed the liaison and coordinators to prepare for common issues and reduced disruption to daily activities. Additionally, 1 to 2 hours every week were allocated for in-person meetings; this structure acted as a scaffold for all communication, both structured and unanticipated.
Under PCC, the liaison and coordinators shared databases. Before PCC, the clinic contacted CCACs with queries about patients’ care; this process was time-consuming, resource intensive, and an example of the inefficiencies and siloization in health care. The PCC initiative streamlined communication, which facilitated timely access to patient information and improved quality of care. Bridging health care silos through communication pathways, collaboration, and knowledge of the health care system was both necessary to implement PCC and vital to its success.
Conclusion
While PCC was piloted in a specific clinic of an FHT in Ontario, the intervention could be adapted by other clinics and organizations as part of the ongoing efforts to improve primary care and care coordination. Other clinics (within this FHT) and other organizations (outside of the FHT and even outside of the region or province) could learn from this example of a care coordination intervention. It is important to note that there remain challenges in knowing how best to objectively measure the success of interventions like PCC (either current or future). It is further concerning that there are few useful measures provided in the literature (for example visit counts and measures of costs and resources are insufficient). In the program example presented in this commentary, having a lead physician involved made the process of implementation more comprehensive and effective. We believe there might be value in looking to relationship measures (such as the patient relationship with a caregiver and between providers). We encourage future research to capture these types of measures both before and after implementation. Given the challenges associated with evaluation metrics, PCC has not yet been subject to rigorous evaluation, and this commentary did not include a formal evaluation. While there is a need for additional research on the appropriate outcome metrics, PCC can act as a resource for other clinics and organizations pursuing similar quality improvement initiatives. This commentary aims to present PCC as a concrete example of a care coordination intervention and provide insight into the practical implications associated with its implementation. There is no “one-size-fits-all” approach; if PCC were to be adopted by other clinics, it would also be necessary to adapt the model to address the needs unique to the population. The recent and proposed changes to Ontario’s health care system mandate moving toward increased coordination and integration under constrained budgets.44 It is imperative that existing resources and infrastructure be used to improve coordination improvement efforts. The PCC intervention demonstrates that coordination can be improved by facilitating communication within and across sectors, using existing resources, and streamlining existing organ izationalstructures.
Footnotes
Competing interests
None declared
The opinions expressed in commentaries are those of the authors. Publication does not imply endorsement by the College of Family Physicians of Canada.
This article has been peer reviewed.
La traduction en français de cet article se trouve à www.cfp.ca dans la table des matières du numéro de juin 2020 à la page e165.
References
- 1.Powell Davies G, Williams AM, Larsen K, Perkins D, Roland M, Harris MF. Coordinating primary health care: an analysis of the outcomes of a systematic review. Med J Aust. 2008;188(S8):S65–8. doi: 10.5694/j.1326-5377.2008.tb01748.x. [DOI] [PubMed] [Google Scholar]
- 2.The Commonwealth Fund. International health care system profiles: what is being done to promote delivery system integration and care coordination? New York, NY: The Commonwealth Fund; 2019. Available from: https://international.commonwealthfund.org/features/integration. Accessed 2018 Nov 1. [Google Scholar]
- 3.Blendon RJ, Schoen C, DesRoches C, Osborn R, Zapert K. Common concerns amid diverse systems: health care experiences in five countries. Health Aff (Millwood) 2003;22(3):106–21. doi: 10.1377/hlthaff.22.3.106. [DOI] [PubMed] [Google Scholar]
- 4.Health Council of Canada. Health care renewal in Canada: accelerating change. Toronto, ON: Health Council of Canada; 2005. Available from: https://healthcouncilcanada.ca/files/2.48-Accelerating_Change_HCC_2005.pdf. Accessed 2018 Nov 3. [Google Scholar]
- 5.Hutchison B, Levesque JF, Strumpf E, Coyle N. Primary health care in Canada: systems in motion. Milbank Q. 2011;89(2):256–88. doi: 10.1111/j.1468-0009.2011.00628.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Peterson K, Anderson J, Bourne D, Charns M, Gorrin SS, Hynes D, et al. Healthcare coordination theoretical frameworks: a systematic scoping review to increase their understanding and use in practice. J Gen Intern Med. 2019;34(Suppl 1):90–8. doi: 10.1007/s11606-019-04966-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Health Quality Ontario. Connecting the dots for patients: family doctors’ views on coordinating patient care in Ontario’s healthcare system. Toronto, ON: Health Quality Ontario; 2016. Available from: https://www.hqontario.ca/Portals/0/documents/system-performance/connecting-the-dots-report-en.pdf. Accessed 2018 Nov 3. [Google Scholar]
- 8.Schoen C, Osborn R, Squires D, Doty M, Pierson R, Applebaum S. New 2011 survey of patients with complex care needs in eleven countries finds that care is often poorly coordinated. Health Aff (Millwood) 2011;30(12):2437–48. doi: 10.1377/hlthaff.2011.0923. Epub 2011 Nov 9. [DOI] [PubMed] [Google Scholar]
- 9.McKesson Canada. Patient-centered care: a framework for care coordination. Saint-Laurent, QC: McKesson Canada; 2013. Available from: http://healthcareathome.ca/mh/en/Documents/RelayHealth_-_White_Paper[1].pdf. Accessed 2018 Dec 18. [Google Scholar]
- 10.Tricco AC, Antony J, Ivers NM, Ashoor HM, Khan PA, Blondal E, et al. Effectiveness of quality improvement strategies for coordination of care to reduce use of health care services: a systematic review and meta-analysis. CMAJ. 2014;186(15):E568–78. doi: 10.1503/cmaj.140289. Epub 2014 Sep 15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.McDonald KM, Sundaram V, Bravata DM, Lewis R, Lin N, Kraft SA, et al. Closing the quality gap: a critical analysis of quality improvement strategies (vol. 7: care coordination) Rockville, MD: Agency for Healthcare Research and Quality; 2007. [PubMed] [Google Scholar]
- 12.Katz EB, Carrier ER, Umscheid CA, Pines JM. Comparative effectiveness of care coordination interventions in the emergency department: a systematic review. Ann Emerg Med. 2012;60(1):12–23.e1. doi: 10.1016/j.annemergmed.2012.02.025. Epub 2012 Apr 27. [DOI] [PubMed] [Google Scholar]
- 13.Guerriere M. Connecting healthcare silos to improve patient outcomes. Vancouver, BC: Telus Health; 2019. [Google Scholar]
- 14.4 Steps for hospitals to reduce their “siloization.”. Chicago, IL: Becker’s Hospital Review; 2012. Available from: https://www.beckershospitalreview.com/patient-flow/4-steps-for-hospitals-to-reduce-their-qsilo-izationq.html. Accessed 2019 Sep 10. [Google Scholar]
- 15.Dykes PC, Carroll DL, Hurley AC, Benoit A, Middleton B. Why do patients in acute care hospitals fall? Can falls be prevented? J Nurs Adm. 2009;39(6):299–304. doi: 10.1097/NNA.0b013e3181a7788a. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Ontario Primary Care Council. Position statement: care coordination in primary care. Ontario Primary Care Council; 2016. Available from: https://www.allianceon.org/sites/default/files/documents/Position%20statement_care%20coordinaton%20in%20primary%20care.pdf. Accessed 2019 Jan 1. [Google Scholar]
- 17.Jones CD, Jones J, Richard A, Bowles K, Lahoff D, Boxer RS, et al. “Connecting the dots”: a qualitative study of home health nurse perspectives on coordinating care for recently discharged patients. J Gen Intern Med. 2017;32(10):1114–21. doi: 10.1007/s11606-017-4104-0. Epub 2017 Jul 13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Central Community Care Access Centre. Your home and community partner: 2014–2015 annual report to the community. Markham, ON: Central Community Care Access Centre; 2016. Available from: http://healthcareathome.ca/central/en/performance/Documents/2014-15AnnualReportEnglish.pdf. Accessed 2019 Jan 15. [Google Scholar]
- 19.Weaver JS, Che XX, Peterson LA, Hysong SJ. Unpacking care coordination through a multiteam system lens: a conceptual framework and systemic review. Med Care. 2018;58(3):247–59. doi: 10.1097/MLR.0000000000000874. [DOI] [PubMed] [Google Scholar]
- 20.Mississauga-Halton Community Care Access Centre. Role of community care providers. Etobicoke, ON: Mississauga-Halton Community Care Access Centre; 2015. Available from: http://healthcareathome.ca/mh/en/care/patient/Documents/5%20-%20Role%20of%20community%20care%20providers_Final.pdf. Accessed 2019 Jan 2. [Google Scholar]
- 21.Cheyne A. Care Coordination Program of Work guidebook. Mississauga, ON: Mississauga Halton Local Health Integration Network; 2018. Available from: http://healthcareathome.ca/mh/en/Documents/Guidebook-CareCoordinationProgramOfWork-FINAL.pdf. Accessed 2019 Jan 18. [Google Scholar]
- 22.Gabutti I, Mascia D, Cicchetti A. Exploring “patient-centered” hospitals: a systematic review to understand change. BMC Health Serv Res. 2017;17(1):364. doi: 10.1186/s12913-017-2306-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Meijboom B, Schmidt-Bakx S, Westert G. Supply chain management practices for improving patient-oriented care. Supply Chain Manag. 2011;16(3):166–75. [Google Scholar]
- 24.Ministry of Health and Long-Term Care. Bill 41. c. 30. S.O. An Act to amend various Acts in the interests of patient-centred care. Toronto, ON: Legislative Assembly of Ontario; 2019. Available from: https://www.ola.org/sites/default/files/node-files/bill/document/pdf/2016/2016-12/bill---text-41-2-en-b041ra.pdf. Accessed 2020 May 2. [Google Scholar]
- 25.Althaus F, Paroz S, Hugli O, Ghali WA, Daeppen JB, Peytremann-Bridevaux I, et al. Effectiveness of interventions targeting frequent users of emergency departments: a systematic review. Ann Emerg Med. 2011;58(1):41–52. doi: 10.1016/j.annemergmed.2011.03.007. [DOI] [PubMed] [Google Scholar]
- 26.Manderson B, McMurray J, Piraino E, Stolee P. Navigation roles support chronically ill older adults through healthcare transitions: a systematic review of the literature. Health Soc Care Community. 2012;20(2):113–27. doi: 10.1111/j.1365-2524.2011.01032.x. Epub 2011 Oct 13. [DOI] [PubMed] [Google Scholar]
- 27.Peikes D, Chen A, Schore J, Brown R. Effects of care coordination on hospitalization, quality of care, and health care expenditures among Medicare beneficiaries: 15 randomized trials. JAMA. 2009;301(6):03–18. doi: 10.1001/jama.2009.126. [DOI] [PubMed] [Google Scholar]
- 28.Andrew S, Halcomb EJ, editors. Mixed methods research for nursing and the health sciences. Oxford, UK: Blackwell Publishing Ltd; 2009. [Google Scholar]
- 29.Joosten EA, DeFuentes-Merillas L, de Weert GH, Sensky T, van Der Staak CP, de Jong CA. Systematic review of the effects of shared decision-making on patient satisfaction, treatment adherence and health status. Psychother Psychosom. 2008;77(4):219–26. doi: 10.1159/000126073. Epub 2008 Apr 16. [DOI] [PubMed] [Google Scholar]
- 30.Carroll JC, Talbot Y, Permaul J, Tobin A, Moineddin R, Blaine S, et al. Academic family health teams. Part 1: patient perceptions of core primary care domains. Can Fam Physician. 2016;62:e23–30. Available from: www.cfp.ca/content/cfp/62/1/e23.full.pdf. Accessed 2020 May 2. [PMC free article] [PubMed] [Google Scholar]
- 31.Lerberghe WV. The World Health Report 2008. Primary health care. Now more than ever. Geneva, Switz: World Health Organization; 2008. Available from: https://www.who.int/whr/2008/whr08_en.pdf. Accessed 2019 Jan 2. [Google Scholar]
- 32.Agarwal R, Jain P, Ghosh MS, Parihar KS. Importance of primary health care in the society. Int J Health Sci. 2017;1(1):6–11. [Google Scholar]
- 33.McKenzie B. Improving patient outcomes through care coordination and population health management. Frisco, TX: Conifer Health Solutions; 2018. Available from: https://www.coniferhealth.com/knowledge-center/improving-patient-outcomes-through-care-coordination-and-population-health-management. Accessed 2019 Jan 2. [Google Scholar]
- 34.Sibbald SL, Selkirk K, Cherla A, Misra V. An opportunity for quality: the need for better evaluation of family health teams in Ontario. Healthc Q. 2019;21(4):28–31. doi: 10.12927/hcq.2019.25744. [DOI] [PubMed] [Google Scholar]
- 35.Maruthappu M, Hasan A, Zeltner T. Enablers and barriers in implementing integrated care. Health Syst Reform. 2015;1(4):250–6. doi: 10.1080/23288604.2015.1077301. [DOI] [PubMed] [Google Scholar]
- 36.South West Local Health Integration Network. Understanding health inequities and access to primary care in the South West LHIN. London, ON: Human Environments Analysis Laboratory; 2016. Available from: http://southwestlhin.on.ca/∼/media/sites/sw/PDF/Physicians/SWLHIN_PrimaryHealthCareCapacity_ReportFINAL.pdf?la=en. Accessed 2019 Jan 2. [Google Scholar]
- 37.Shah TI, Clark AF, Seabrook JA, Sibbald S, Gilliland JA. Geographic accessibility to primary care providers: comparing rural and urban areas in southwestern Ontario. Can Geogr. 2020;64(1):65–78. Epub 2019 Aug 8. [Google Scholar]
- 38.Sibbald SL, Clark AF, Seabrook JA, Gilliland J. Without compromising integrity: research and planning around the primary healthcare landscape in southwestern Ontario. Healthc Q. 2018;21(1):46–53. doi: 10.12927/hcq.2018.25528. [DOI] [PubMed] [Google Scholar]
- 39.Community Legal Education Ontario [website]. What is a CCAC? How does it work? Community Legal Education Ontario; 2019. Available from: https://www.cleo.on.ca/en/publications/homecare/what-ccac-how-does-it-work. Accessed 2019 Jan 2. [Google Scholar]
- 40.Kothari A, Hovanec N, Hastie R, Sibbald S. Lessons from the business sector for successful knowledge management in health care: a systematic review. BMC Health Serv Res. 2011;11(1):173. doi: 10.1186/1472-6963-11-173. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Hays RD, Martino S, Brown JA, Cui M, Cleary P, Gaillot S, et al. Evaluation of a care coordination measure for the Consumer Assessment of Healthcare Providers and Systems (CAHPS) Medicare survey. Med Care Res Rev. 2014;71(2):192–202. doi: 10.1177/1077558713508205. Epub 2013 Nov 13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Gagliardi AR, Berta W, Kothari A, Boyko J, Urquhart R. Integrated knowledge translation (IKT) in health care: a scoping review. Implement Sci. 2015;11(1):38. doi: 10.1186/s13012-016-0399-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Szafran O, Torti JMI, Kennett SL, Bell NR. Family physicians’ perspectives on interprofessional teamwork: findings from a qualitative study. J Interprof Care. 2018;32(2):169–77. doi: 10.1080/13561820.2017.1395828. Epub 2017 Nov 8. [DOI] [PubMed] [Google Scholar]
- 44.Ministry of Health and Long-Term Care. Bill 74. c. 5. S.O. An Act concerning the provision of health care, continuing Ontario Health and making consequential and related amendments and appeals. Toronto, ON: Legislative Assembly of Ontario; 2019. Available from: https://www.ola.org/sites/default/files/node-files/bill/document/pdf/2019/2019-04/b074ra_e.pdf. Accessed 2020 Jan 21. [Google Scholar]