Abstract
Background
Great variability exists in response to stressful or traumatic events, leading to an interest in the construct of resilience as a trait and an outcome. The etiologic sources of variability across differing conceptualizations of resilience are poorly understood.
Methods
Using behavioral genetic methods in a sample of 2,056 female twins, the present study sought to a) examine the etiologic sources of a trait-based self-report measure of perceived resilience (PR), b) determine the genetic and environmental overlap with an outcome-based measure of resilience, as defined by the absence of psychiatric symptoms after stressful life events, previously used by our research team (discrepancy-based psychiatric resilience; DBPR), and c) determine the etiologic overlap of these two resilience measures with major depressive disorder (MDD).
Results
PR was modestly (11%) heritable. A moderate degree of genetic overlap (39%) and a nominal amount of environmental overlap (3%) was found between the two alternative measures of resilience. Genetic factors that influence PR accounted for 3% of MDD heritability, whereas 31% of MDD heritability was due to DBPR genetic factors.
Conclusions
Findings of a higher genetic correlation between the outcome-based resilience measure and MDD compared to the trait-based measure and MDD suggest gene-finding efforts may benefit from considering the multifaceted nature of resilience and that resilience is best understood as both a phenotypically and genetically heterogeneous construct.
Keywords: Resilience, Heritability, Twin, Genetic, MDD
Introduction
Exposure to stressful and traumatic life events has been associated with negative psychological outcomes, such as posttraumatic stress disorder (PTSD) and major depressive disorder (MDD; Overstreet, Berenz, Kendler, Dick, & Amstadter, 2017; Pietrzak, Goldstein, Southwick, & Grant, 2011), though many exposed to such events demonstrate resilience. The field has, in more recent years, shown an appreciation of the study of resilient phenotypes. However, the popularity of resilience has had a snowball effect, and the term ‘resilience’ is currently used interchangeably to describe this multifaceted construct from various perspectives (Southwick, Pietrzak, Tsai, Krystal, & Charney, 2015). As a result, prevalence rates of resilience across different samples in the literature vary, likely in part due to differing definitions of this construct. Studies have demonstrated differences within the same sample based on various approaches to modeling resilience outcomes (Infurna & Luthar, 2016) and various definitions (Sheerin, Stratton, Amstadter, Education, & McDonald, 2018). Moreover, the genetic and environmental etiologic contributions to various definitions of resilience, as well as their potential etiologic overlap, are unknown. Due to wide-ranging public health implications of better elucidating the etiologic components of resilience, refining this phenotype and comparing ways in which it has been measured is critical.
Resilience has been conceptualized in numerous ways, including as an outcome (e.g., the absence of PTSD; Bonanno, Galea, Bucciarelli, & Vlahov, 2006; Polusny et al., 2017), a process (e.g., developmental or systems perspectives; Masten, 2016; Walsh, 2016), and longitudinal trajectories of responses to stress (e.g., “resistant” and “resilient” patterns; Fink et al., 2017; Norris, Tracy, & Galea, 2009). However, arguably, the most frequently used operationalization and thus measurement of resilience in the traumatic stress literature is that of a trait (e.g., a stable, distinguishing quality or characteristic; Bensimon, 2012; Connor & Davidson, 2003). Self-report assessments, such as the Connor-Davidson Resilience Scale (CD-RISC; Connor & Davidson, 2003) or the Resilience Scale for Adults (RSA; Friborg, Hjemdal, Rosenvinge, & Martinussen, 2003) were developed to assess resilience traits and skills. Trait-based measurements assume resilience to be a multidimensional trait that the respondent believes is present or absent. In this definition, this multidimensional trait exists regardless of whether an individual experiences adversity and/or symptoms of mental illness (Luthar, Cicchetti, & Becker, 2000). Despite being a frequently used method of defining resilience, to our knowledge only one genetically-informed study has examined a trait-based measure of perceived resilience. In a recent study, Wolf et al. (2018) quantified the heritability of the CD-RISC in a sample of Vietnam-era veteran twins at 25% and found that the genetic influence on resilience fully overlapped with the genetic influence on PTSD.
Behavioral genetic methodologies have also been employed to quantify the etiologic sources (i.e., degree of genetic and environmental influence underlying the phenotype) of a quantitative measure of resilience as an outcome. A model used in children to quantitatively measure psychological resilience (Kim-Cohen, Moffitt, Caspi, & Taylor, 2004) was adapted to measure psychological resilience in adults on a continuum based on the severity of symptoms pursuant to adverse experiences (Amstadter, Myers, & Kendler, 2014). Specifically, resilience was operationalized as the difference between an individual’s actual score on a specific outcome (e.g., psychiatric distress) and the score predicted by their level of adversity (e.g., number of stressful life events or total trauma load). Resilience scores were derived from standardized residuals in a regression model. The residuals represent the variance in each individual’s outcome remaining after removal of the predictor’s effects. Amstadter et al. (2014) used this discrepancy-based model of resilience, regressing total stressor load on internalizing symptoms, and found that genetic factors constituted about 50% of the variance for this resilience definition (Amstadter et al., 2014). Additional studies identified that 60% of the heritability of resilience was explained by genetic factors shared with neuroticism (Amstadter, Moscati, Maes, Myers, & Kendler, 2016). There was also a larger genetic overlap of resilience with internalizing disorders (e.g., major depressive disorder) than with externalizing disorders (e.g., alcohol use disorder), but some unique genetic influence on resilience remained (Amstadter, Maes, Sheerin, Myers, & Kendler, 2016). Thus, resilience defined in this way is not simply the absence of psychiatric disorders. Two other twin studies using a residual-based model of resilience have demonstrated moderate to strong genetic influence on resilience (Boardman, Blalock, & Button, 2008; Kim-Cohen et al., 2004).
To our knowledge, no attempts have been made to compare patterns of genetic and environmental factors between trait-based and outcome-based resilience. Improved understanding of the etiology of different definitions of resilience can assist the field in answering important questions about the validity of the measurements used and can identify factors that lead to positive outcomes following stressful and traumatic events. The current study utilized data from a community-based twin study to evaluate the magnitude of genetic and environmental influences on a trait-based, self-report measure of perceived resilience (PR) similar to that measured with the CD-RISC. The aims of the current study were to use twin modeling to 1) quantify genetic and environmental factors of PR, 2) clarify patterns of genetic and environmental covariance between PR and discrepancy-based psychiatric resilience (referred to hereafter as DBPR), and 3) to examine the shared versus unique contributions of the two forms of resilience with major depressive disorder (MDD), a common stress-related psychiatric disorder. Consistent with previous research, we expected to find moderate heritability of PR. Moderate-to-strong genetic overlap was anticipated between PR and DBPR, given they are both definitions of resilience currently in use in the literature. Differences in measurement were expected to result in small unique genetic effects attributed to PR and DBPR. Lastly, given that previous studies suggested DBPR is not simply the absence of negative psychiatric outcomes, it was expected that there would be moderate, but not complete genetic overlap among PR, DBPR, and MDD. It was not known whether PR or DBPR would exhibit stronger genetic overlap with MDD.
Method
Sample
Participants were from the all-female first wave of the Virginia Adult Twin Studies of Psychiatric and Substance Use Disorders (VATSPSUD), a large, longitudinal twin study of Caucasian adults, described in detail elsewhere (Kendler & Prescott, 2006) with sample characteristics as shown in Table 1. The Institutional Review Board at Virginia Commonwealth University (VCU) approved this study, and all subjects provided informed consent before participating. Items used in the perceived resilience measure were only available in the all-female wave of this sample. Zygosity was determined by discriminant function analyses using standard twin questions validated against genotyping in 496 pairs (Kendler & Prescott, 1999).
Table 1.
Sample Characteristics
| Characteristic | Mean (SD) |
|---|---|
| Age (in years) | 29.3 (7.72) |
| PR | 19.78 (1.64) |
| SLE | 1.67 (1.66) |
| MDD Last Year Diagnosis | N = 217 (11%) |
| MZ twins | N = 1,178 |
| DZ twins | N = 878 |
Note. PR = Perceived Resilience, SLE = number of stressful life events in past 90 days, MDD = Major Depressive Disorder. MZ = monozygotic twin pair, DZ = dizygotic twin pair. Discrepancy-based psychiatric resilience (DBPR) was a standardized measure with mean = 0 and variance = 1.
Resilience Measures
Perceived resilience (PR)
Participants completed several questionnaires as part of VATSPSUD. All items were examined for similarity in wording with the CD-RISC 10-item scale (Campbell-Sills & Stein, 2007). An approximate match was found for seven items. These items were extracted and their factor structure analyzed via confirmatory factor analysis (CFA).
Discrepancy-based psychiatric resilience (DBPR)
VATSPSUD participants completed a shortened version of the Symptom Checklist-90, (SCL-90; Derogatis, Lipman, & Covi, 1973; Hardt & Gerbershagen, 2001) to assess past-month distress symptoms. The shortened version used a Likert scale ranging from 1 (“not at all”) to 4 (“extremely”) and contained 27 items from four of the SCL-90 subscales: depression (10 items), somatization (5 items), anxiety (7 items), and phobic anxiety (5 items). It demonstrates relatively high internal reliability (Chronbach’s α= 0.74; Hardt & Gerbershagen, 2001). A composite score was calculated for symptoms and used to create the resilience variable. Exposure to a range of stressful life events (SLEs; e.g., assault, marital problems, job loss, death of a spouse or child) over the past 90 days (to be proximal to distress ratings) was also assessed (via a 15-item checklist) and a stressor load value based on total number of SLEs was assigned. The measure of DBPR was operationalized as the residual from regressing total stressor load (SLE) on internalizing symptoms (SCL-90; Amstadter et al., 2014). For clarity in interpreting subsequent analyses, scores were reverse-coded, and the residual was used as a continuous measure of resilience, with positive, higher residuals indicating greater resilience and negative residuals representing lower resilience.
Major depressive disorder (MDD)
Last year MDD was assessed at personal interview by trained mental health professionals who were blind to the status of cotwin, using modifications of the Structured Clinical Interview for DSM-III-R Axis I Disorders (Spitzer, Williams, Gibbon, & Williams, 1995). Last year MDD status was the most relevant of available stress-related psychiatric diagnoses in our sample to assess shared etiology of PR and DBPR.
Twin Modeling
This study used a classic twin design, which leverages the differences between monozygotic (MZ) and dizygotic (DZ) twin types to decompose the phenotypic variation into additive genetic (A), common environmental (C), and unique environmental (E) factors (Neale & Cardon, 1992). Table 3 shows the cross-twin cross-trait correlations for MZ and DZ twin pairs. These correlations are the basis for the classic twin design used in this study. Due to MZ twins sharing 100% of their genes and DZ twins sharing, on average, 50% of their segregating genes, the genetic factor contributes twice as much to the MZ twin correlation compared to the DZ twin correlation. Common environmental factors are shared factors, which make twins more similar and contribute equally to the MZ and DZ twin correlations. Unique environmental factors are specific to the individual, represent experiences not shared by twins, do not contribute to either MZ or DZ twin correlation, and capture measurement error.
Table 3.
MZ and DZ Cross-twin Cross-trait Correlations
| Twin 1 | Twin 2 | ||||||
|---|---|---|---|---|---|---|---|
| PR | DBPR | MDD | PR | DBPR | MDD | ||
| Twin 1 | PR | - | .18*** | −0.14*** | 0.11* | 0.07 | −0.05 |
| DBPR | 0.32*** | - | −0.28*** | 0.07 | 0.34*** | −0.10** | |
| MDD | −0.10* | −0.29*** | - | −0.04 | −0.14*** | 0.19*** | |
| Twin 2 | PR | 0.07* | 0.02 | −0.03 | - | 0.29 *** | −0.14** |
| DBPR | 0.06 | 0.16** | −0.11* | 0.21*** | - | −0.24*** | |
| MDD | −0.04 | −0.18 | 0.07 | −0.14** | −0.27*** | - | |
Note. MZ twin pair correlations are above the diagonal and DZ twin pair correlations are below the diagonal. MZ = monozygotic twin pair, DZ = dizygotic twin pair. PR = Perceived Resilience, DBPR = Discrepancy-Based Psychiatric Resilience, MDD = Major Depressive Disorder.
p < 0.05
p < 0.01
p < 0.001
We examined three primary models that investigated 1) the etiology of PR via a univariate twin model, 2) the shared etiology of PR and DBPR via a bivariate twin model, and 3) the shared etiology of PR, DBPR, and MDD via a trivariate twin model. For each of the primary models, submodels (models II-VII in each section of Table 4) were tested by dropping parameters. By comparing the fit statistics to the full model (I) we determined the significance of each set of factors to identify the best-fitting model for the univariate, bivariate, and trivariate models. All twin analyses used a full information maximum-likelihood approach for raw data implemented in the OpenMx software (Neale, Boker, Xie, & Maes, 2003; Neale et al., 2016). A likelihood ratio χ2 test was used to determine if the constrained model fit the data significantly worse than the full models (model I in each section of Table 4). Akaike Information Criterion (AIC) is based on twice the difference in log-likelihood between higher order and submodels with a penalty for degrees of freedom. A lower AIC denoted a better balance of model fit and parsimony (Akaike, 1987; Williams & Holahan, 1994).
Table 4.
Results of Cholesky Models for Resilience and Major Depressive Disorder
| Model | Parameters | Paths Constrained | −2LL | ΔDF | Δ(−2LL) | ΔAIC | p |
|---|---|---|---|---|---|---|---|
|
Univariate Model (PR) | |||||||
| I | ACE | - | 6585.08 | - | - | - | - |
| II | AE | C | - | 1 | 0.12 | −1.88 | 0.724 |
| III | CE | A | - | 1 | 0.16 | −1.85 | 0.692 |
| IV | E | AC | - | 2 | 6.86 | −2.86 | 0.032 |
|
Bivariate Model (PR & DBPR) | |||||||
| I | ACE | - | 12336.27 | - | - | - | - |
| II | AE | All C | - | 3 | 0.01 | −5.98 | .998 |
| III | CE | All A | - | 3 | 14.46 | 8.47 | .002 |
| IV | E | All AC | - | 6 | 90.87 | 78.88 | <.001 |
| V | AE | Shared A | - | 4 | 6.32 | −1.76 | .176 |
| VI | AE | Shared E | - | 4 | 34.49 | 26.50 | <.001 |
| VII | AE | Shared AE | - | 5 | 110.23 | 100.24 | <.001 |
|
Trivariate Model (PR, DBPR & MDD) | |||||||
| I | ACE | - | 15085.78 | - | - | - | - |
| II | AE | All C | - | 6 | 1.74 | −10.23 | .939 |
| III | CE | All A | - | 6 | 19.21 | 7.21 | .003 |
| IV | E | All AC | - | 12 | 132.60 | 108.61 | <.001 |
| V | AE | Shared A | - | 9 | 43.24 | 25.25 | <.001 |
| VI | AE | Shared E | - | 9 | 45.12 | 27.12 | <.001 |
| VII | AE | Shared AE | - | 12 | 242.01 | 218.01 | <.001 |
Note. −2LL = −2 log-likelihood, ΔDF = change in degrees of freedom from full model (I), ΔAIC = change in Akaike Information Criterion from full model (I), ACE = model with additive genetic, shared environment, and unique environmental factors included, AE = model with additive genetic and unique environmental factors included, CE = model with shared and unique environmental factors included. Best fitting models are designated in bold text for each section of analyses.
Results
PR Creation
Item wording from questions in our dataset and their corresponding CD-RISC 10 wording can be found in Table 2 along with the standardized factor loadings from the CFA, and the scale from which each item was drawn. One twin from each family was used to account for the non-independence of twins in the CFA (N = 1,028). To assess if the selected items represented a unitary construct similar to the theory behind the CD-RISC-10 we used a 1-factor CFA with a diagonally weighted least squares estimator. We found the model adequately fit the data (CFI = 0.95, TLI = 0.92, RMSEA = 0.06), consistent with the unitary factor structure of the CD-RISC-10 (Campbell-Sills & Stein, 2007). Since the modeling was used to test a specific theory and not to create a new psychometric scale, no further models were fitted. The total score of these 7-items was used as the PR measure for the VATSPSUD participants.
Table 2.
CD-RISC Item Descriptors and Most Closely Matched Items
| CD-RISC Item Descriptor | Most Closely Matched Items within the VATSPSUD dataset | Original Scale | CFA Standardized Factor Loading |
|---|---|---|---|
| Able to adapt to change | There is no way I can solve some of the problems I have.a | PMS | 0.39 |
| Can deal with whatever comes | I can do just about anything I set my mind to. | PMS | 0.60 |
| See the humorous side of things | I always look on the bright side of things. | LOT | 0.74 |
| You can achieve your goals | Whatever happens to me in the future mostly depends on me. | PMS | 0.48 |
| Under pressure, focus and think clearly | In the last 30 days how much discomfort have you felt from the following symptom: Trouble concentrating a | SCL-90 | 0.35 |
| Not easily discouraged by failure | In uncertain times, I usually expect the best. | LOT | 0.57 |
| Think of self as strong person | I often feel helpless in dealing with the problems of my life.a | PMS | 0.71 |
Note. CD-RISC = Connor-Davidson Resilience Scale, VATSPSUD = Virginia Adult Twin Studies of Psychiatric and Substance Use Disorders, LOT = Life Orientation Test (Scheier & Carver, 1985), PMS = Pearlin Mastery Scale (Pearlin & Schooler, 1978), SCL-90 = the Symptom Checklist-90 (Derogatis et al., 1973).
Item scores were inversed. Both LOT and PMS questions use a 4-point Likert scale for participants to rate how strongly they agreed with each statement.
Twin Modeling
To quantify the genetic and environmental influences on both measures of resilience we fitted univariate and bivariate twin models. The Univariate Model section in Table 4 outlines the models we tested for PR. Models were compared to the full ACE model (I). Beginning with model II we tested the significance of each latent factor. A sub-model that was significantly different from the full model (compared using chi-squared of −2LL) would indicate the necessity of the dropped parameter. Our best fitting univariate model was a genetic and environmental model which found PR to be 11% heritable with the remaining variance accounted for by unique experiences (89%; model II- AE).
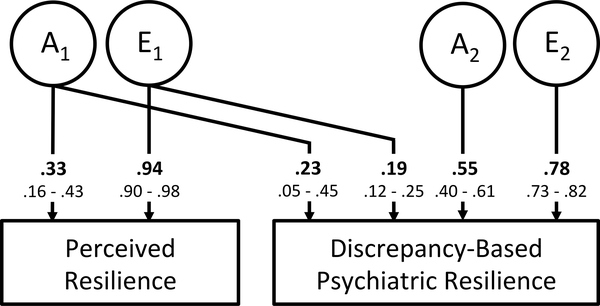
To clarify the patterns of covariance between the two measures of resilience, a series of bivariate twin models was conducted. The best fitting bivariate model was a genetic and environmental model (model II in Bivariate Model section of Table 4) and the heritability of PR was 11%, consistent with the univariate model. DBPR was found to be 35.2% heritable with 15% of the total heritability shared with PR and the remaining 85% specific to DBPR. The remaining 64.2% of DBPR’s total variance was accounted for by unique experiences with only 5% of DBPR’s unique environmental influences shared with PR and the remaining 95% specific to DBPR. These proportions were derived by squaring the path estimates of the best fitting model illustrated in Figure 1, and all sources of variance sum to 1.0.
Figure 1.
Final Bivariate Model for Trait-based Resilience and Measures Resilience. Standardized parameter estimates are bolded and standard errors are reported below. Proportions of variance are calculated by squaring these standardized path estimates.
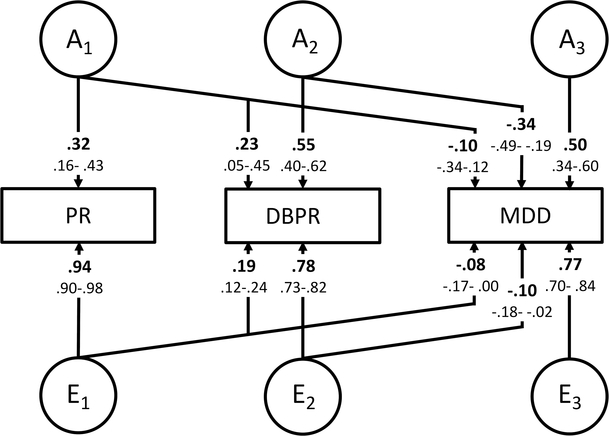
Incorporating MDD into the bivariate models above allowed for examination of the shared etiology between these two measures of resilience and MDD. The subsequent best fitting trivariate model was a genetic and environmental model (path diagram shown in Figure 2, model fit shown in Trivariate Model section of Table 4, model II). It had a similar structure to the bivariate model of PR and DBPR with slightly differing relationships to MDD (path estimates shown in Figure 2). Overall, MDD was found to be 38% heritable, with 3% of its total heritability shared with PR, 31% shared with DBPR and the remaining 66% specific to MDD. Unique environmental factors had a similar structure to the genetic factors, with specific factors explaining 62% of MDD variance and nominal overlap of unique experiences between MDD and PR (1%) and DBPR (1%). The negative path estimates onto MDD (Figure 2) denote that factors that increase scores for the resilience measures would also be protective of MDD. Despite the nominal overlap in unique environmental experience between these three measures we were unable to remove the cross-paths without a significant deterioration in fit (model fits and comparisons shown in Trivariate Section of Table 4).
Figure 2.
Final Trivariate Model for Perceived Resilience (PR), Discrepancy-Based Psychiatric Resilience (DBPR) and lifetime Major Depressive Disorder (MDD). Standardized parameter estimates are bolded and standard errors are reported below each parameter. Proportions of variance are calculated by squaring these standardized path estimates.
Discussion
The aims of this study were threefold. We first sought to construct a trait-based, self-report measure of resilience (PR) and clarify the genetic and environmental etiology of this measure. We next sought to determine the overlap, or covariance, between PR and a residual-based resilience construct (DBPR). Finally, we sought to explore the overlap between these two resilience definitions and MDD. Each will be discussed in turn.
Genetic and unique environmental (AE) models provided the best fit of all models, which was consistent with existing studies examining various measures of resilience and resilience-like traits (e.g., Amstadter, Myers, & Kendler, 2014; Boardman, Blalock, & Button, 2008). Modeling from the first aim found that PR was modestly heritable (11%). Compared to the heritability of other trait-like measures (e.g., mastery estimated at 33% (Kessler, Gilman, Thornton, & Kendler, 2004; Kiecolt, Aggen, & Kendler, 2013); optimism estimated at 36% (Mosing, Zietsch, Shekar, Wright, & Martin, 2009)), present findings suggest a smaller contribution of genetic factors to individual differences in PR, but align with findings of greater impact of environmental influences.
For the second aim, the bivariate model found the genetic overlap accounted for 30% of the phenotypic correlation of PR and DBPR, suggesting that genetic influences played a modest to moderate role in the etiologic relationship between the two constructs. The greater degree of unique genetic variance for the DBPR outcome as compared to the PR outcome aligns with previous work with alternative measures of resilience when operationalized as positive affect despite repeated exposure to stressful life events (38% for women and 52% for men; Boardman et al., 2008), as well as previous work by our group using the DBPR construct in this sample (31–50% heritability; Amstadter et al., 2014). However, for both constructs, unique environmental effects explained more of the variance. Such unique environmental events may include differences in the various trauma exposure types and other aspects in which twins may differ, all of which were unmeasured in our sample. This finding highlights the importance of a wide range of individual experiences, and environmental contexts, in addition to the moderate influence of genetic liability when evaluating the etiology of resilience. Further, the presence of a more modest degree of effects common to both constructs, as compared to effects unique to each, supports the conceptualization of resilience as a multifaceted, heterogeneous construct (Southwick, Bonanno, Masten, Panter-Brick, & Yehuda, 2014). Our findings also align with more recent discussion in the literature of separating resilience into different facets (i.e., ‘resistance to breakdown’ describing the ability to withstand a stressor without breakdown, while ‘plasticity’ describes the ability to undergo change without breakdown; Hobfoll, Stevens, & Zalta, 2015). Perhaps these facets map on to various definitions of resilience (outcomes-based, systems-based, or trait-based) and in turn evidence unique genetic etiology.
The trivariate model examining the etiological overlap across both resilience constructs and depression (aim 3) indicated greater genetic correlations of MDD with the DBPR measure (−0.56) as compared to the PR measure (−0.07). The genetic correlation between MDD and DBPR could be partially explained by construct overlap (e.g., some items of the SCL, which is used to calculate the DBPR variable, overlap with symptoms of MDD). However, our prior work with the DBPR demonstrated a unique genetic influence on DBPR that is separate from that of MDD over and above shared genetic influence of DBPR and MDD (Amstadter et al., 2016). Furthermore, the current findings suggest the majority of etiologic influences on resilience and depression are unique to each phenotype. This adds to ongoing discussion in the literature of whether resilience is the polar opposite of psychopathology (Hobfoll, 2012) or represents a qualitatively different phenotype (Hobfoll et al., 2015).
Present findings can inform future genetic investigations of resilience. Most notably, gene-finding efforts should not be focused on a unitary construct, as resilience is not likely to be best captured in this manner. As suggested by Choi et al (2019), studies should also clearly define resilience to facilitate interpretation and replication efforts. Limited work has examined candidate genes associated with a small number of resilience and related trait-based constructs (e.g., CD-RISC, optimism) and has not found significant associations (Rana et al., 2014). It is hoped that continued efforts that focus on a wider range of well-measured resilience constructs will prove fruitful. Additionally, resilience is not the same as the absence of psychopathology, as discussed above, yet many of the existing, large-powered genetic investigations continue to view resilience in the context of psychopathology (e.g., absence of PTSD; Nievergelt et al., 2015). While this work remains important, in order for continued growth in our understanding of resilience as a unique construct, there is a need to examine a wider distribution of resilient responding (Bonanno, Romero, & Klein, 2015; Choi, Stein, Dunn, Koenen, & Smoller 2019), which genetic researchers should also bear in mind. Clinically, the contribution of unique experiences to resilience, however defined, highlights the need for continued research to identify environmental and psychological factors that are modifiable and may be intervened upon to foster resilience (see review by Chmitorz et al., 2018). Furthermore, there are potential benefits of examining resilience from gene by environment interaction approaches to better understand the mechanisms of resilience (see review by Elbau, Cruceanu, & Binder, 2019).
A number of limitations are worth noting. First, the trait-based measure (PR) was not standardized and had only seven of 10 items linked with its comparison measure (CD-RISC), therefore results need to be replicated with a more standardized trait-based measure. While the DBPR measure reduces a source of error because it is not based solely on an individual’s self-perception, it is calculated using self-reported distress, which may be correlated with MDD, thus potentially inflating the strength of association. It is also noted that in contrast to PR, which is more unidimensional, DBPR, by definition as a residual, includes other unmeasured factors, such as sociodemographic factors. Thus, the measure is more multifaceted and is dependent upon the sample in which it was determined. Another limitation of the DBPR measure is that it primarily captures stressors along with a few traumas (e.g. assaults) and not lifetime trauma burden, which also plays a role in the degree of distress observed and is thus an inherent limitation of this study. Additionally, the Caucasian- and female-only sample limits generalizability, and replication is needed in more diverse samples. Finally, neither resilience measure examined here captures resilience as an ongoing process nor do they capture aspects of functioning relevant for resilience. Continued work examining a broader set of resilience conceptualizations will help inform our understanding of the genetic underpinnings of this multifaceted and important construct.
Conclusion
In summary, resilience is best viewed as a phenotypically heterogeneous construct (Infurna & Luthar, 2016; Southwick et al., 2014), and present findings suggest it is also genetically heterogeneous. Results also add further evidence to the perspective that resilience is unique from the absence of a disorder, in this case, MDD. The slightly stronger heritability estimates for DBPR as compared to PR suggest the potential benefit of future gene-finding efforts using this construct. However, our findings also suggest that future efforts aimed at understanding the etiology of resilience take into account its multifaceted nature and examine a wide range of well-measured constructs. Study findings, while supportive of common genetic factors, also highlight the relatively greater importance of unique experience; this wide range of individual experiences and circumstances (e.g., trauma exposure, social support) at play may later manifest in a wide range of resilient responding. Notably, these unique environmental experiences are additive, and understanding their impact on genetic predisposition over time is a useful avenue of further research.
Acknowledgments
This work was supported by National Institute of Health grants in part by NIH grants T32 MH020030, K02 AA023239, R01 AA020179, P20 AA10782, R37 AA011408, R37 DA18673 and R01 DA22989.
Footnotes
Data Availability
Research data are not shared.
References
- Akaike H (1987). Factor analysis and AIC. Psychometrika, 52(3), 317–332. 10.1007/BF02294359 [DOI] [Google Scholar]
- Amstadter A, Moscati A, Maes H, Myers J, & Kendler K (2016). Personality, cognitive/psychological traits and psychiatric resilience: A multivariate twin study. Personality and Individual Differences, 91, 74–79. 10.1016/j.paid.2015.11.041 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Amstadter AB, Myers JM, & Kendler KS (2014). Psychiatric resilience: longitudinal twin study. The British Journal of Psychiatry, 205(4), 275–280. 10.1192/bjp.bp.113.130906 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Amstadter AB, Maes HH, Sheerin CM, Myers JM, & Kendler KS (2016). The relationship between genetic and environmental influences on resilience and on common internalizing and externalizing psychiatric disorders. Social Psychiatry and Psychiatric Epidemiology, 51(5), 669–678. 10.1007/s00127-015-1163-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bensimon M (2012). Elaboration on the association between trauma, PTSD and posttraumatic growth: The role of trait resilience. Personality and Individual Differences, 52(7), 782–787. 10.1016/j.paid.2012.01.011 [DOI] [Google Scholar]
- Boardman JD, Blalock CL, & Button TMM (2008). Sex differences in the heritability of resilience. Twin Research and Human Genetics, 11(1), 12–27. 10.1375/twin.11.1.12 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bonanno GA, Galea S, Bucciarelli A, & Vlahov D (2006). Psychological Resilience After Disaster: New York City in the Aftermath of the September 11th Terrorist Attack. Psychological Science, 17(3), 181–186. 10.1111/j.1467-9280.2006.01682.x [DOI] [PubMed] [Google Scholar]
- Bonanno GA, Romero SA, & Klein SI (2015). The Temporal Elements of Psychological Resilience: An Integrative Framework for the Study of Individuals, Families, and Communities. Psychological Inquiry, 26(2), 139–169. 10.1080/1047840X.2015.992677 [DOI] [Google Scholar]
- Campbell-Sills L, & Stein MB (2007). Psychometric analysis and refinement of the Connor-Davidson Resilience Scale (CD-RISC): Validation of a 10-item measure of resilience. Journal of Traumatic Stress, 20(6), 1019–1028. 10.1002/jts.20271 [DOI] [PubMed] [Google Scholar]
- Chmitorz A, Kunzler A, Helmreich I, Tuscher O, Kalisch R, Kubiak T, … Lieb K (2018). Intervention studies to foster resilience - A systematic review and proposal for a resilience framework in future intervention studies. Clinical Psychology Review, 59, 78–100. 10.1016/j.cpr.2017.11.002 [DOI] [PubMed] [Google Scholar]
- Choi KW, Stein MB, Dunn EC, Koenen KC, & Smoller JW (2019). Genomics and psychological resilience: a research agenda. Molecular Psychiatry. 24, 1770–1778. 10.1038/s41380-019-0457-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Connor KM, & Davidson JRT (2003). Development of a new Resilience scale: The Connor-Davidson Resilience scale (CD-RISC). Depression and Anxiety, 18(2), 76–82. 10.1002/da.10113 [DOI] [PubMed] [Google Scholar]
- Derogatis LR, Lipman RS, & Covi L (1973). SCL-90: an outpatient psychiatric rating scale--preliminary report. Psychopharmacology Bulletin, 9(1), 13–28. [PubMed] [Google Scholar]
- Elbau IG, Cruceanu C, & Binder EB (2019). Genetics of Resilience: Gene-by-Environment Interaction Studies as a Tool to Dissect Mechanisms of Resilience. Biological Psychiatry. 10.1016/j.biopsych.2019.04.025 [DOI] [PubMed] [Google Scholar]
- Fink DS, Lowe S, Cohen GH, Sampson LA, Ursano RJ, Gifford RK, … Galea S (2017). Trajectories of posttraumatic stress symptoms after civilian or deployment traumatic event experiences. Psychological Trauma: Theory, Research, Practice, and Policy, 9(2), 138–146. 10.1037/tra0000147 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Friborg O, Hjemdal O, Rosenvinge JH, & Martinussen M (2003). A new rating scale for adult resilience: what are the central protective resources behind healthy adjustment? International Journal of Methods in Psychiatric Research, 12(2), 65–76. 10.1002/mpr.143 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hardt J, & Gerbershagen HU (2001). Cross-validation of the SCL-27: A short psychometric screening instrument for chronic pain patients. European Journal of Pain (London, England), 5(2), 187–197. 10.1053/eujp.2001.0231 [DOI] [PubMed] [Google Scholar]
- Hobfoll SE (2012). Conservation of Resources and Disaster in Cultural Context: The Caravans and Passageways for Resources. Psychiatry: Interpersonal and Biological Processes, 75(3), 227–232. 10.1521/psyc.2012.75.3.227 [DOI] [PubMed] [Google Scholar]
- Hobfoll SE, Stevens NR, & Zalta AK (2015). Expanding the Science of Resilience: Conserving Resources in the Aid of Adaptation. Psychological Inquiry, 26(2), 174–180. 10.1080/1047840X.2015.1002377 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Infurna FJ, & Luthar SS (2016). Resilience to Major Life Stressors Is Not as Common as Thought. Perspectives on Psychological Science, 11(2), 175–194. 10.1177/1745691615621271 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kendler KS, & Prescott CA (1999). A population-based twin study of lifetime major depression in men and women. Archives of General Psychiatry, 56(1), 39–44. 10.1001/archpsyc.56.1.39 [DOI] [PubMed] [Google Scholar]
- Kendler KS, & Prescott CA (2006). Genes, environment, and psychopathology: Understanding the causes of psychiatric and substance use disorders. New York: The Guilford Press. [Google Scholar]
- Kessler RC, Gilman SE, Thornton LM, & Kendler KS (2004). Health, well-being, and social responsibility in the MIDUS twin and sibling subsamples In Brim OG, Ryff CD, & Kessler RC (Eds.), How healthy are we?: A national study of well-being at midlife (pp. 124–152). Chicago: University of Chicago Press. [Google Scholar]
- Kiecolt KJ, Aggen SH, & Kendler KS (2013). Genetic and Environmental Influences on the Relationship Between Mastery and Alcohol Dependence. Alcoholism: Clinical and Experimental Research, 37(6), 905–913. 10.1111/acer.12058 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kim-Cohen J, Moffitt TE, Caspi A, & Taylor A (2004). Genetic and environmental processes in young children’s resilience and vulnerability to socioeconomic deprivation. Child Development, 75(3), 651–668. 10.1111/j.1467-8624.2004.00699.x [DOI] [PubMed] [Google Scholar]
- Luthar SS, Cicchetti D, & Becker B (2000). The construct of resilience: a critical evaluation and guidelines for future work. Child Development, 71(3), 543–562. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Masten AS (2016). Resilience in developing systems: the promise of integrated approaches. European Journal of Developmental Psychology, 13(3), 297–312. 10.1080/17405629.2016.1147344 [DOI] [Google Scholar]
- Mosing MA, Zietsch BP, Shekar SN, Wright MJ, & Martin NG (2009). Genetic and environmental influences on Optimism and its relationship to mental and self-rated health: A study of aging twins. Behavior Genetics, 39(6), 597–604. 10.1007/s10519-009-9287-7 [DOI] [PubMed] [Google Scholar]
- Neale MC, Boker SM, Xie G, & Maes HH (2003). Mx: Statistical Modelling (6th ed.). Department of Psychiatry, Virginia Institute for Psychiatric and Behavioral Genetics, Virginia Commonwealth University. [Google Scholar]
- Neale MC, Hunter MD, Pritikin JN, Zahery M, Brick TR, Kirkpatrick RM, … Boker SM (2016). OpenMx 2.0: Extended Structural Equation and Statistical Modeling. Psychometrika, 81(2), 535–549. 10.1007/s11336-014-9435-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Neale M, & Cardon L (1992). Methodology for Genetic Studies of Twins and Families. Dordrecht, Netherlands: Kluwer Academic Publishers. [Google Scholar]
- Nievergelt CM, Maihofer AX, Mustapic M, Yurgil KA, Schork NJ, Miller MW, … Baker DG (2015). Genomic predictors of combat stress vulnerability and resilience in U.S. Marines: A genome-wide association study across multiple ancestries implicates PRTFDC1 as a potential PTSD gene. Psychoneuroendocrinology, 51, 459–471. 10.1016/j.psyneuen.2014.10.017 [DOI] [PubMed] [Google Scholar]
- Norris FH, Tracy M, & Galea S (2009). Looking for resilience: understanding the longitudinal trajectories of responses to stress. Social Science & Medicine (1982), 68(12), 2190–2198. 10.1016/j.socscimed.2009.03.043 [DOI] [PubMed] [Google Scholar]
- Overstreet C, Berenz EC, Kendler KS, Dick DM, & Amstadter AB (2017). Predictors and mental health outcomes of potentially traumatic event exposure. Psychiatry Research, 247, 296–304. 10.1016/j.psychres.2016.10.047 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pearlin L, & Schooler C (1978). The Structure of Coping. Journal of Health and Social Behavior, 19(1), 2–21. [PubMed] [Google Scholar]
- Pietrzak RH, Goldstein RB, Southwick SM, & Grant BF (2011). Prevalence and Axis I comorbidity of full and partial posttraumatic stress disorder in the United States: Results from Wave 2 of the National Epidemiologic Survey on Alcohol and Related Conditions. Journal of Anxiety Disorders, 25(3), 456–465. 10.1016/j.janxdis.2010.11.010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Polusny MA, Erbes CR, Kramer MD, Thuras P, DeGarmo D, Koffel E, … Arbisi PA (2017). Resilience and Posttraumatic Stress Disorder Symptoms in National Guard Soldiers Deployed to Iraq: A Prospective Study of Latent Class Trajectories and Their Predictors. Journal of Traumatic Stress, 30(4), 351–361. 10.1002/jts.22199 [DOI] [PubMed] [Google Scholar]
- Rana BK, Darst BF, Bloss C, Shih PAB, Depp C, Nievergelt CM, … Jeste DV (2014). Candidate SNP associations of optimism and resilience in older adults: Exploratory study of 935 community-dwelling adults. American Journal of Geriatric Psychiatry, 22(10), 997–1006.e5. 10.1016/j.jagp.2014.03.009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Scheier M, & Carver C (1985). Optimism, Coping, and Health: Assessment and Implications of Generalized Outcome Expectancies. Health Psychology, 4(3), 219–247. [DOI] [PubMed] [Google Scholar]
- Sheerin CM, Stratton KJ, Amstadter AB, Education CC (MIRECC) W., The VA Mid-Atlantic Mental Illness Research, & McDonald SD (2018). Exploring resilience models in a sample of combat-exposed military service members and veterans: a comparison and commentary. European Journal of Psychotraumatology, 9(1), 1486121 10.1080/20008198.2018.1486121 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Southwick SM, Bonanno GA, Masten AS, Panter-Brick C, & Yehuda R (2014). Resilience definitions, theory, and challenges: Interdisciplinary perspectives. European Journal of Psychotraumatology, 5(1), 25338 10.3402/ejpt.v5.25338 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Southwick S, Pietrzak R, Tsai J, Krystal J, & Charney D (2015). Resilience: An Update. PTSD Research Quarterly, 25(4), 1050–1835. [Google Scholar]
- Spitzer R, Williams J, Gibbon M, & Williams JBW (1995). Structured Clinical Interview for DSM-III-R. Washington, DC: American Psychiatric Press. [Google Scholar]
- Walsh F (2016). Family resilience: a developmental systems framework. European Journal of Developmental Psychology, 13(3), 313–324. 10.1080/17405629.2016.1154035 [DOI] [Google Scholar]
- Williams L, & Holahan P (1994). Parsimony-based fit indices for multiple-indicator models: Do they work? Structural Equation Modeling: A Multidisciplinary Journal, 1(2), 161–189. [Google Scholar]
- Wolf EJ, Miller MW, Sullivan DR, Amstadter AB, Mitchell KS, Goldberg J, & Magruder KM (2018). A classical twin study of PTSD symptoms and resilience: Evidence for a single spectrum of vulnerability to traumatic stress. Depression and Anxiety, 35(2), 132–139. 10.1002/da.22712 [DOI] [PMC free article] [PubMed] [Google Scholar]