Abstract
The impact of changes to posttraumatic stress disorder (PTSD) diagnostic criteria from Diagnostic and Statistical Manual of Mental Disorders (4th ed.; DSM-IV) to Diagnostic and Statistical Manual of Mental Disorders (5th ed.; DSM-5) within diverse communities is unclear. Young adult sexual minority women are at high risk for interpersonal violence and other forms of trauma exposure compared with heterosexual populations and sexual minority men. They are also at heightened risk of PTSD. As a result, young adult sexual minority women are a key population of interest when examining the impact of diagnostic criteria changes. The goal of the current study was to evaluate the impact of changes to PTSD diagnostic criteria in sexual minority women. Using an online survey, we administered both the original PTSD Symptom Checklist-S (based on DSM-IV criteria) and a version adapted to assess DSM-5 criteria to a national, nonclinical sample of young adult sexual minority women (N = 767). The DSM-5 symptom criteria fit the data well in confirmatory factor analysis. Current PTSD prevalence was higher under the DSM-5 diagnostic algorithm compared with DSM-IV (18.6% vs. 22.9%; d = 0.15). Compared with DSM-IV, associations between PTSD and depression were stronger using DSM-5 criteria, whereas associations between PTSD and high-risk drinking were reduced. Findings suggest that changes to PTSD diagnostic criteria do not have a major impact on prevalence of PTSD among sexual minority women but may have some impact on observed comorbidities.
Keywords: posttraumatic stress disorder, minority stress, diagnosis, lesbian, bisexual
Comparing PTSD in DSM-5 Versus DSM-IV in a National Sample of Sexual Minority Women
The release of the Diagnostic and Statistical Manual of Mental Disorders (5th ed.; DSM-5; American Psychiatric Association, 2013) included significant changes to posttraumatic stress disorder (PTSD) criteria (see Friedman et al., 2011). Because diagnostic criteria may not perform equally well across diverse groups, evaluation of these changes within minority populations, particularly those with elevated risk, is needed (Elhai & Palmieri, 2011). However, no research to our knowledge has examined the performance of DSM-5 PTSD symptom structure within specific U.S. minority groups. Sexual minority women (SMW), including but not limited to cisgender and transgender women who identify as lesbian or bisexual, are a key population to study in this regard, as large population-based studies have found higher prevalence of interpersonal violence and other trauma exposure and PTSD as defined by the Diagnostic and Statistical Manual of Mental Disorders (4th ed., text rev.; DSM-IV-TR; American Psychiatric Association, 2000) among SMW as compared with heterosexual women and gay men (Gilman et al., 2001; Roberts et al., 2010). In addition, some data suggest that young adult SMW experience especially high risk of interpersonal violence (Roberts et al., 2010). Thus, the purpose of this article is to examine the impact of changes in PTSD criteria from DSM-IV to DSM-5 among a young adult, nonclinical SMW sample.
Changes to PTSD Diagnostic Criteria in DSM-5
The updated DSM-5 PTSD criteria involved two significant changes: changes to the definition of a traumatic event and changes to the symptoms themselves. Next, we review the nature of these changes and evidence of their impact in general population samples.
The first major change in DSM-5 PTSD criteria involved alteration in the definition of a traumatic event. DSM-IV required a subjective reaction (i.e., reports of fear, horror, or helplessness; Criterion A2) to a qualifying traumatic event (Criterion A1). Due to concerns that DSM-IV definition of a traumatic event was too vague, particularly around indirect exposure to traumatic events such as witnessing or learning about traumatic experiences happening to others (e.g., Zoellner et al., 2013), Criterion A1 was narrowed in DSM-5 to be more restrictive in specifying who was directly exposed (i.e., a family member or close friend) and the nature of the event to which they were exposed (i.e., violent or accidental actual or threatened death). Criterion A2 was removed in light of evidence that it has limited diagnostic utility (Bedard-Gilligan & Zoellner, 2008; Karam et al., 2010). Removing Criterion A2 appears to have little influence on prevalence estimates of DSM-IV PTSD (e.g., Bedard-Gilligan & Zoellner, 2008; Kilpatrick et al., 2009), and results in slightly increased prevalence of DSM-5 PTSD (Elhai et al., 2012; Kilpatrick et al., 2013), although more research, particularly in diverse samples, is needed to confirm this finding.
The second major change in DSM-5 PTSD criteria involved changes in the number of symptom clusters and the nature of symptoms. DSM-IV included three clusters: reexperiencing, avoidance/numbing, and arousal. Due in part to problems with model fit of the three-cluster model (for reviews, see Armour et al., 2016; Elhai & Palmieri, 2011), DSM-5 used a four-cluster model that has demonstrated improved fit in factor analyses (Armour et al., 2016; Elhai et al., 2012; Forbes et al., 2015; Miller et al., 2013). Criterion B (reexperiencing/intrusions) had only minor changes from the DSM-IV (e.g., removing rumination, clarifying that nightmare content should be trauma-related). Avoidance of internal reminders (e.g., thoughts, feelings) and external reminders (e.g., people, places) were retained with minor wording changes and together now comprise effortful avoidance (Criterion C), and the remaining emotional numbing symptoms were moved to a new cluster focused on negative changes in mood and cognitions (Criterion D). In addition to minor changes to symptoms, the new Criterion D includes three symptoms not captured in DSM-IV: exaggerated negative expectations about oneself, others, or the world; cognitive distortions regarding trauma-related blame; and pervasive negative emotional state. Foreshortened future, formerly considered avoidance, was removed altogether. Finally, the five hyperarousal symptoms of DSM-IV were retained as DSM-5 Criterion E (arousal/reactivity), a self-destructive or reckless behavior symptom was added, and minor changes were made to several symptoms (e.g., the irritability symptom was modified to include aggressive behavior). On the whole, these DSM-5 changes to Criteria B to E appear to somewhat reduce lifetime PTSD prevalence estimates (from 10.6% to 9.4%) but have no significant impact on past-6-month diagnoses (Miller et al., 2013). Requiring at least one symptom of effortful avoidance to meet diagnostic criteria leads some individuals to meet criteria under DSM-IV but not DSM-5, and the expanded mood and hyperarousal symptoms leads some to meet criteria under DSM-5 but not DSM-IV (Kilpatrick et al., 2013).
Sexual Minority Women and PTSD in DSM-5
It is important to test the assumption that changes to diagnostic criteria perform well in minority groups, especially when those groups are disproportionately diagnosed with or affected by a given condition (Asnaani et al., 2010; Elhai & Palmieri, 2011; Pole et al., 2008). Symptoms may have different meanings and may not cluster together in the same ways across different groups. In the case of PTSD, diverse groups may experience unique forms of stressors (e.g., identity-based harassment, discrimination, and trauma) that could affect symptom expression (Elhai & Palmieri, 2011).
Several studies have used confirmatory factor analysis to compare the DSM-IV and DSM-5 factor structures in diverse populations. The DSM-5 four-factor model outperformed the DSM-IV three-factor model in a sample of earthquake survivors in Armenia (Demirchyan et al., 2015) and sexual violence survivors in the Democratic Republic of Congo (Michalopoulos et al., 2015). Both models performed comparably well among Sri Lankans (Kuowei et al., 2018) and refugees in Switzerland (Schnyder et al., 2015), and neither performed adequately in Iraqis (Michalopoulos et al., 2015). This demonstrates that the superior fit of the DSM-5 symptom structure is an assumption that requires testing across diverse groups.
SMW are a key group to examine in regard to PTSD diagnostic changes because they experience high risk for both trauma (especially interpersonal violence) and PTSD (Gilman et al., 2001; Roberts et al., 2010), and this risk may occur through unique mechanisms relative to heterosexual populations. From a minority stress perspective, SMW experience chronic bias-related social stressors, such as microaggressions, explicit discrimination, harassment, and violent assault targeted to SMW because of their identity (Hatzenbuehler, 2009; Meyer, 2003). The chronic stressors experienced by SMW may, themselves, be traumatic events—as in the case of bias-based violence—or may increase vulnerability to PTSD after non–bias-based events, to which they are also highly vulnerable relative to heterosexuals (Balsam et al., 2005; Dworkin et al., 2018; Katz-Wise & Hyde, 2012). These chronic minority stressors are thought to increase risk for emotion dysregulation, interpersonal dysfunction, and cognitive shifts (Hatzenbuehler, 2009; Meyer, 2003) which, in turn, increase the prevalence of both PTSD and comorbid disorders (e.g., anxiety, depression, alcohol use disorders) (King et al., 2008; Steele et al., 2009).
Thus, from a minority stress perspective, SMW’s exposure to chronic social stress could impact endorsement of the new DSM-5 PTSD symptoms and therefore increase prevalence of DSM-5 PTSD as well as comorbid conditions. For example, SMW may experience cognitive shifts, such as the internalization of heterosexism, which could manifest as persistent and exaggerated negative beliefs (D2) related to a trauma (Alessi et al., 2013; Dworkin et al., 2018; Szymanski & Balsam, 2011). SMW experiencing emotional dysregulation may also be more likely to endorse risky behavior (E2) based on evidence of higher risk of substance abuse, suicidality, and other related behaviors in sexual minority samples (Conron et al., 2010; McCabe et al., 2009).
The Present Study
Because young SMW are disproportionately affected by both trauma (especially interpersonal violence) and PTSD, it is important to test the assumption that PTSD diagnostic criteria perform well within this population specifically. This study thus evaluated the potential impact of changes from DSM-IV to DSM-5 PTSD diagnostic criteria on factor structure model fit, prevalence estimates, and comorbidity in a national sample of young SMW. We hypothesized that (a) both the DSM-IV and DSM-5 factor structures would evidence acceptable model fit, (b) the removal of Criterion A2 would result in slight increases in past-month PTSD prevalence, (c) the symptom criterion changes would not alter past-month PTSD prevalence, and (d) there would be increased likelihood of comorbidity with anxiety, depression, and alcohol misuse when using DSM-5 compared with DSM-IV criteria.
Method
Participants and Procedures
Paid online advertisements were placed on Facebook and Craigslist to recruit a national sample of self-identified lesbian and bisexual women aged 18 to 25 for a larger longitudinal study (Kaysen et al., 2014; Litt et al., 2015). Interested participants completed an online consent form and web-based screening. Eligibility criteria included women who: (a) lived in the United States, (b) had a valid email address, (c) were between the ages of 18 to 25, (d) self-identified as lesbian or bisexual at the time of the assessment, and (e) were assigned female sex at birth and currently identified as women (as a result of the focus of the larger study on sex-dependent alcohol consumption variables).1 For the larger longitudinal study, 1,057 women provided consent and were enrolled. Data for this study were from the 12-month follow-up assessment, in which both DSM-IV sand DSM-5 PTSD symptoms were assessed. Of the 1,057 women enrolled, 203 did not complete the 12-month follow-up assessment. An additional 87 participants were missing data on measures of PTSD and trauma exposure, leaving 767 (72.5%) who were included in this study. There were no statistically significant differences between those who were and were not included in these analyses according to various baseline characteristics including age, χ2(7) = 5.57; p = .591, DSM-IV PTSD diagnosis, χ2(1) = 1.13; p = .288, and elevated anxiety, χ2(1) = .54; p = .463. However, those with elevated compared with nonelevated depression at baseline were less likely to be in the analysis sample, χ2(1) = 4.01, p = .045. Participants were paid US$25 for completing the baseline and US$30 for completing the follow-up assessments. All study procedures were approved by the University of Washington IRB and a federal Certificate of Confidentiality was obtained from the National Institutes of Health. The sample included 41.8% lesbian women and 58.2% bisexual women. Ethnic composition included 70.5% Caucasian, 8.8% African American, 2.4% Asian, 15.6% multiracial, and 2.7% “other.” The mean age was 20.88 years old (SD = 2.11).
Measures
The following measures were completed online.
Generalized anxiety.
The Generalized Anxiety Disorder-7 (GAD-7; Spitzer et al., 2006; Swinson, 2006) was used to assess past-month anxiety symptoms. The GAD-7 has acceptable internal consistency and construct validity in the general population (Löwe et al., 2008); internal consistency was 0.92 in a past study of SMW (Lehavot & Simoni, 2011). Internal consistency was high in this sample (α = .89). Scores of 10 or higher indicated clinically elevated anxiety (Swinson, 2006).
Depressive symptoms.
The Center for Epidemiologic Studies Depression (CES-D) Scale (Radloff, 1977) is a 20-item self-report scale modified to measure past-month depressive symptoms. Internal consistency reliability, test–retest reliability, and validity are acceptable in the general population (Radloff, 1977); prior studies of SMW reported internal consistency of 0.86 to 0.93 (Herek et al., 1997; Lehavot & Simoni, 2011). The CES-D had strong internal consistency in this sample (α = .80). Scores of 16 or higher indicated clinically elevated depression (Radloff, 1977).
Alcohol use.
Alcohol use was assessed with a modified version of the Daily Drinking Questionnaire (DDQ; Collins et al., 1985). This measure has previously been found to have good reliability and construct validity (Kivlahan et al., 1990). Participants were asked to report the number of standard drinks consumed each day on a typical week in the last 12 months. A binary variable for low risk alcohol use was created according to NIAAA guidelines (low risk use = 3 or less drinks during a typical day and <7 drinks during a typical week).
Trauma exposure.
The Traumatic Life Experiences Questionnaire (TLEQ; Kubany et al., 2000) was used to assess the number of lifetime traumatic events participants had experienced. The TLEQ includes a comprehensive list of 22 potentially traumatic life events and assesses DSM-IV-TR PTSD Criterion A2 with a follow-up question regarding whether the person experienced fear, helplessness, or horror. The temporal stability of this scale has been demonstrated in prior work (Kubany et al., 2000). Participants who endorsed sexual traumas were asked to indicate whether they believed that the event occurred because they are lesbian/bisexual.
PTSD symptoms.
The PTSD Checklist (PCL; Weathers et al., 1991) was adapted to assess both past-month DSM-IV and DSM-5 PTSD symptoms at the 12-month assessment. As this study was conducted prior to publication of the PCL-5 (Weathers et al., 2013), we made the following modifications to capture the proposed DSM-5 symptom changes (APA, DSM-5 Development, 2010), as summarized in Table 4: four new items assessed the new DSM-5 symptoms (three in Criterion D and one in Criterion E), six items included wording changes in symptom descriptions (three in Criterion B, one in Criterion C, one in Criterion D, and one in Criterion E), and the foreshortened future item was removed. The new and modified items were administered in addition to the original 17, for a total of 27 questions paralleling both DSM-IV and DSM-5 diagnostic criteria. Participants were prompted to choose a “most distressing” traumatic event from their TLEQ responses and answer the PCL questions regarding that event. This scale has acceptable internal consistency and validity (Weathers et al., 1994), and internal consistency has been reported at 0.94 among SMW specifically (Szymanski & Balsam, 2011). The 17-item DSM-IV PCL had strong internal consistency in this sample (α = .93) as did the 20-item DSM-5 PCL (α = .94). All items used the PCL for DSM-IV 5-point Likert-type scale. For analysis, we treated responses of 3 to 5 (moderately, quite a bit, and extremely) as symptomatic and responses of 1 to 2 (not at all and a little bit) as nonsymptomatic (Weathers et al., 1991) due to data sparseness. We then used diagnostic algorithms matching DSM-IV and DSM-5 symptom endorsement requirements to determine whether diagnostic criteria were met.
Table 4.
Prevalence and Prevalence Ratios for Clinically Elevated Depression, Anxiety, and High-Risk Alcohol Use According to DSM-IV and DSM-5 Diagnostic Criteria.
| DSM-IV PTSD Criteria | DSM-5 PTSD Criteria | |||||
|---|---|---|---|---|---|---|
|
|
||||||
| Outcome | % of Those Meeting DSM-IV Criteria With Outcome | % of Those NOT Meeting DSM-IV Criteria With Outcome | PR [95% CI] | % of Those Meeting DSM-5 Criteria With Outcome | % of Those NOT Meeting DSM-5 Criteria With Outcome | PR [95% CI] |
| Depression | 85.1 | 54.0 | 1.58 [1.43, 1.74] | 87.9 | 51.5 | 1.71 [1.55, 1.88] |
| Anxiety | 91.6 | 63.5 | 1.44 [1.33, 1.56] | 89.8 | 62.5 | 1.44 [1.33, 1.56] |
| High-risk drinking | 39.4 | 31.6 | 1.25 [0.99, 1.58] | 33.1 | 33.0 | 1.00 [0.79, 1.28] |
Note. DSM-IV = Diagnostic and Statistical Manual of Mental Disorders (4th ed.); DSM-5 = Diagnostic and Statistical Manual of Mental Disorders (5th ed.); PTSD = posttraumatic stress disorder; PR = prevalence ratio.
Data Analytic Plan
Descriptive analyses estimated the prevalence and associated 95% confidence interval of trauma exposure and PTSD using DSM-IV and DSM-5 criteria. To test whether the prevalence of PTSD was different between the two criteria, we used McNemar’s test to account for the nonindependence of observations within a participant. These analyses included all 767 women.
Confirmatory factor analysis (CFA) was used to assess criteria factor structure fit using the lavaan package (version 0.5–10) in R 2.15.1 software. One-hundred thirty-two (15.9%) participants who did not indicate a worst traumatic event were excluded from analyses, leaving a total of 635 participants. PCL items were treated as categorical using the tetrachoric covariance matrix (Flora & Curran, 2004; Wirth & Edwards, 2007). Diagonally weighted least squares (DWLS) estimation was used to estimate the model parameters, but the full weight matrix was used to compute the robust standard errors with a mean- and variance-adjusted test statistic (WLSMV). Fit indices reported for the models include the chi-square statistic, root mean square error of approximation (RMSEA), the comparative fit index (CFI), and the Tucker–Lewis index (TLI). A RMSEA value of less than 0.06 and a CFI and TLI value of 0.95 or greater were chosen as indicators of good fit for the data (Hu & Bentler, 1999).
To examine cross-sectional associations between PTSD diagnoses and comorbidity, we used modified Poisson regression with robust standard errors to estimate prevalence ratios (PRs) associated with concurrent PTSD diagnosis (Spiegelman & Hertzmark, 2005). Sample sizes for analysis of each outcome were 754 (98.3%) for depression, 765 (99.7%) for anxiety, and 760 (99.1%) for high-risk drinking. Descriptive and Poisson regression analyses were performed using Stata 14.1 software (Stata Corporation, College Station, TX).
Results
Table 1 summarizes hypotheses and results. Of the 767 women in this analysis, 635 (82.8%) reported a Criterion A trauma, and 605 (78.9%) reported a trauma that additionally met DSM-IV Criterion A2 (i.e., 30 women reported traumas that did not meet DSM-IV criteria due to the absence of peritraumatic fear, horror, or helplessness). The most commonly reported index traumas were sudden death of a friend or loved one (16.0%) and unwanted sexual contact as a child (5.3%), adolescent (7.2%), or adult (6.6%). Of the index traumas, 3.8% involved unwanted sexual contact attributed by the participant to their sexual orientation. Using DSM-IV criteria, 18.6% of participants met criteria for past-month PTSD. A statistically significant higher prevalence of 22.9% was observed when DSM-5 criteria were used, McNemar’s χ2(1) = 11.97; p < .001. Generally, there was a high level of agreement between the two diagnostic criteria sets (Table 2).
Table 1.
Summary of Changes in PTSD Diagnostic Criteria From DSM-IV to DSM-5 and Corresponding Study Results.
| Change | Hypothesized Impact | Result |
|---|---|---|
| Narrowing of Criterion A1 | Not tested | Not tested |
| Removal of Criterion A2 | Small prevalence increase | Small prevalence increase |
| Changes to specific symptoms | No prevalence increase | No prevalence increase |
| Symptoms organized into four clusters | Improved model fit | Improved model fit |
Note. PTSD = posttraumatic stress disorder; DSM-IV = Diagnostic and Statistical Manual of Mental Disorders (4th ed.); DSM-5 = Diagnostic and Statistical Manual of Mental Disorders (5th ed.).
Table 2.
Distribution of Participants Meeting DSM-IV and/or DSM-5 PTSD Criteria.
| DSM-IV | DSM-5 | Total | |
|---|---|---|---|
|
| |||
| Yes | No | ||
|
|
|||
|
n (Row %) (Column %) |
n (Row %) (Column %) |
||
| Yes, n (%) | 114 (79.7) (64.8) |
29 (20.3) (4.9) |
143 |
| No, n (%) | 62 (9.9) (35.2) |
562 (90.1) (95.1) |
624 |
| Total | 176 | 591 | 767 |
Note. PTSD = posttraumatic stress disorder; DSM-IV = Diagnostic and Statistical Manual of Mental Disorders (4th ed.); DSM-5 = Diagnostic and Statistical Manual of Mental Disorders (5th ed.).
Table 3 shows PTSD prevalence with and without the inclusion of Criterion A2. If Criterion A2 were applied similarly across DSM-IV and DSM-5, the proportion meeting PTSD criteria would be lower according to DSM-5 compared with DSM-IV. This difference was significant when A2 was applied and not significant when A2 was not applied.
Table 3.
Endorsement of Overall PTSD Diagnosis and Specific Symptoms.
| DSM-IV PTSD Symptoms | n (%) | DSM-5 PTSD Symptoms Assessed in Study | n (%) |
|---|---|---|---|
| Overall diagnosis | Overall diagnosis | ||
| With Criterion A2 | 143 (18.6) | With Criterion A2 | 129 (16.8) |
| Without Criterion A2 | 192 (25.0) | Without Criterion A2 | 176 (22.9) |
| Criterion B: Intrusive symptoms | |||
| Repeated, disturbing memories/thoughts/images | 264 (34.4) | Repeated, disturbing memories | 177 (23.1) |
| Repeated, disturbing dreams | 183 (23.9) | Retained in measure | — |
| Acting/feeling like stressful experience happening | 179 (23.3) | Acting/feeling like stressful experience actually happening | 109 (14.2) |
| Upset when reminded | 362 (47.2) | Retained in measure | — |
| Physical reactions | 253 (33.0) | Strong physical reactions | 189 (24.6) |
| Criterion C: Avoidance | |||
| Avoiding thinking/talking about experience | 255 (33.3) | Retained in measure | — |
| Avoiding activities/situations | 274 (35.7) | Avoiding external reminders | 232 (30.3) |
| Criterion D: Cognition/mood symptoms | |||
| Trouble remembering parts of experience | 199 (26.0) | Retained in measure | — |
| Feeling future will be cut short | 187 (24.4) | Removed in measure | — |
| — | — | Blaming oneself or someone else | 199 (26.0) |
| — | — | Strong negative feelings | 233 (30.4) |
| Loss of interest | 149 (19.4) | Retained in measure | — |
| Feeling distant or cut off | 247 (32.2) | Retained in measure | — |
| Feeling emotionally numb | 183 (23.9) | Trouble experiencing positive feelings | 174 (22.7) |
| — | — | Strong negative beliefs | 235 (30.6) |
| Criterion E: Hyperarousal | |||
| Feeling irritated or having outbursts | 225 (29.3) | Feeling irritable or acting aggressively | 202 (26.3) |
| Hypervigilance | 204 (26.6) | Retained in measure | — |
| Feeling jumpy | 180 (23.5) | Retained in measure | — |
| Difficulty concentrating | 234 (30.5) | Retained in measure | — |
| Trouble sleeping | 270 (35.2) | Retained in measure | — |
| — | — | Risk taking | 104 (13.6) |
Note. PTSD = posttraumatic stress disorder; DSM-IV = Diagnostic and Statistical Manual of Mental Disorders (4th ed.); DSM-5 = Diagnostic and Statistical Manual of Mental Disorders (5th ed.).
Table 3 also shows the number and percentage of women who endorsed specific DSM-IV and DSM-5 PTSD symptoms. Figures 1 and 2 show factor structure and loadings from CFA analyses for DSM-IV and DSM-5 models, respectively. CFA analyses indicated that acceptability of the DSM-IV 17-item three-factor model fit was not consistent across fit indices, with CFI and TLI suggesting acceptable fit and RMSEA indicating less than acceptable fit, χ2(116) = 619.04, p < .001; CFI = .961; TLI = .955; RMSEA = .083. In contrast, model fit was acceptable for the DSM-5 20-item four-factor model across all three fit indices, χ2(164) = 475.10, p < .001; CFI = .981; TLI = .978; RMSEA = .055.
Figure 1.
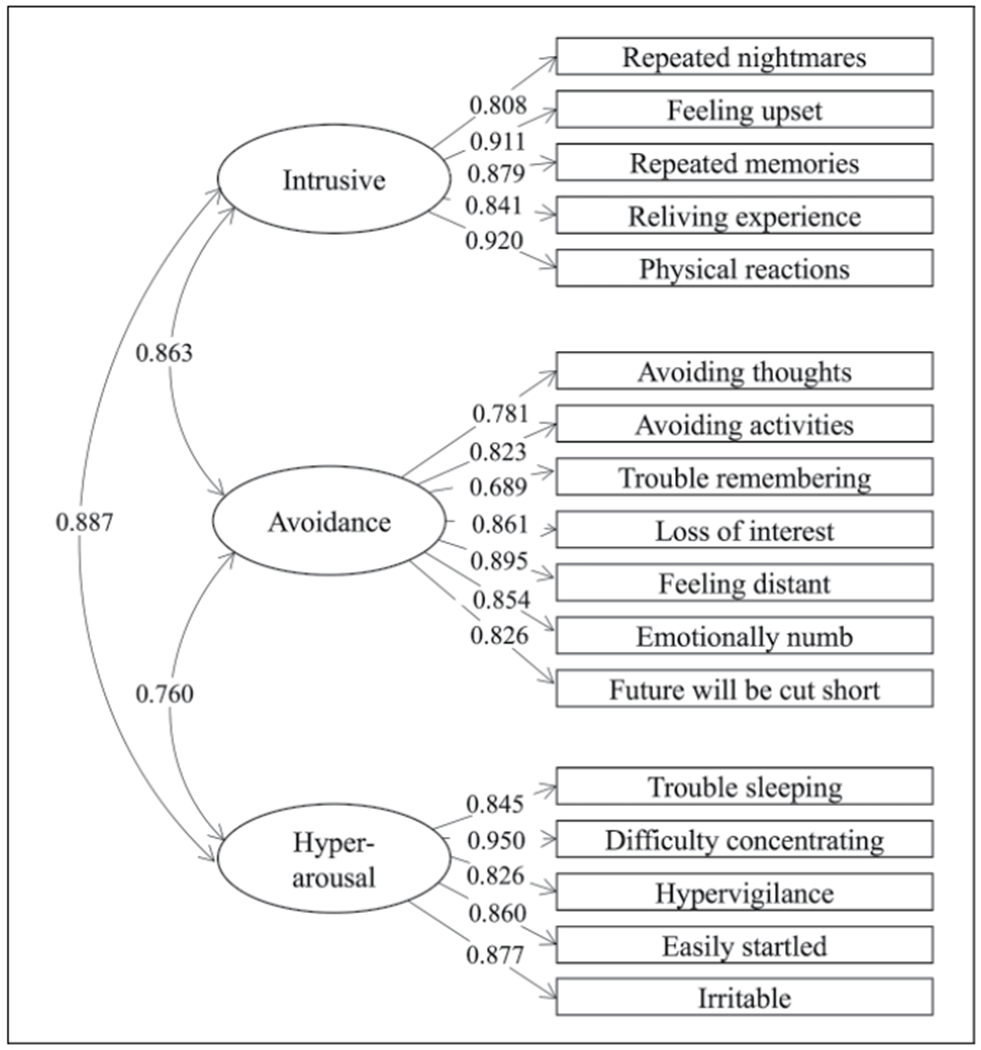
Factor loadings for the DSM-IV PTSD three-factor model.
Note. DSM-IV = Diagnostic and Statistical Manual of Mental Disorders (4th ed.); PTSD = posttraumatic stress disorder.
Figure 2.
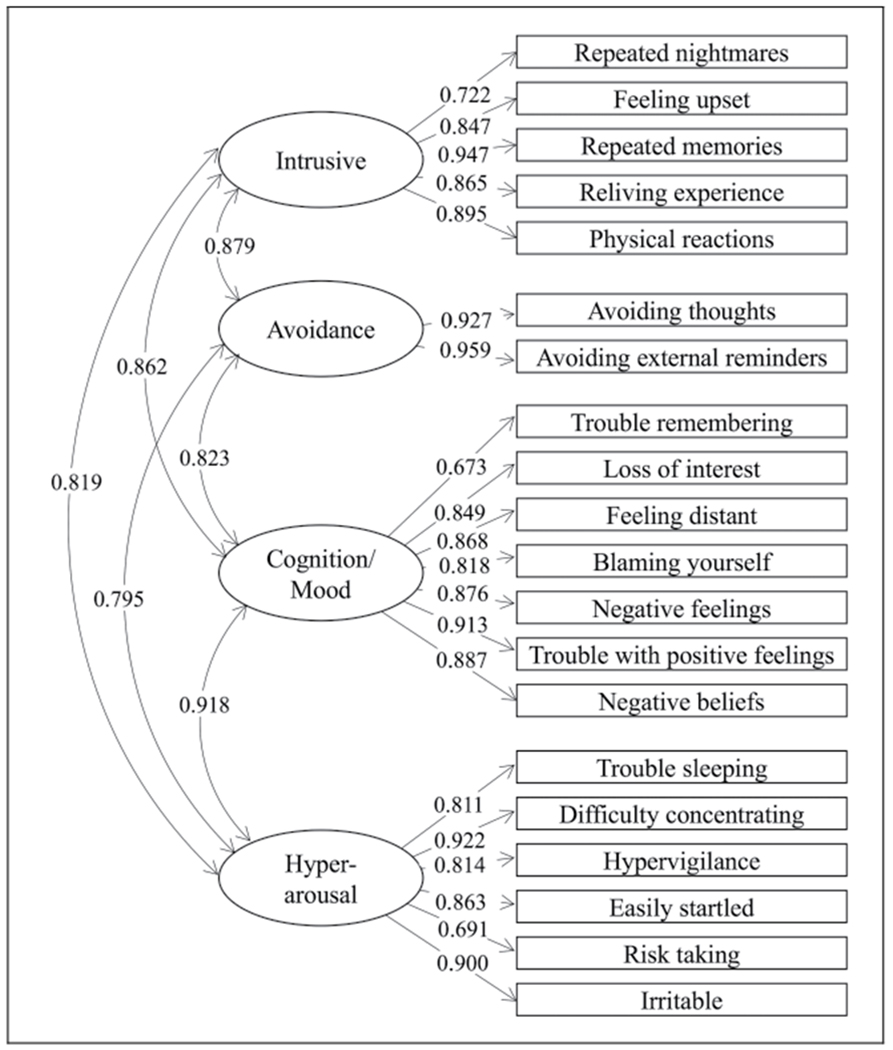
Factor loadings for the DSM-5 PTSD four-factor model.
Note. DSM-5 = Diagnostic and Statistical Manual of Mental Disorders (5th ed.); PTSD = posttraumatic stress disorder.
Table 4 shows associations between DSM-IV and DSM-5 PTSD with comorbid disorders. There was a high prevalence of depression (59.8%) and anxiety (68.8%) in this sample. The prevalence of high-risk drinking was 33.0%. There was a statistically significant association between both depressive and anxiety symptoms with DSM-IV and DSM-5 PTSD criteria. The association with depression was stronger for DSM-5 compared with DSM-IV. No such difference was found for anxiety or high-risk drinking.
Discussion
Although changes to diagnostic criteria are rigorously tested in general population samples, their applicability to specific populations is often an untested assumption; indeed, no research to our knowledge has evaluated the DSM-5 PTSD diagnostic criteria changes among U.S. minority groups. We found that, among a young, large, nationally recruited sample of SMW, DSM-5 symptom criteria evidenced adequate fit for the symptoms of PTSD experienced by SMW, whereas the DSM-IV criteria did not. However, the DSM-5 criteria were associated with a slight prevalence increase that appeared to be driven by the removal of Criterion A2, as well as some changes to patterns of comorbidity. Collectively, these findings suggest that the new symptoms and criteria structure (e.g., changes to symptom clusters) have general applicability to SMW and appear to be appropriate for use in research and clinical practice.
We tested whether DSM-IV and DSM-5 PTSD latent symptom structures fit the symptom presentations of the young SMW in our sample. The four-cluster model in DSM-5 performed well in confirmatory factor analyses, whereas the three-factor model in DSM-IV had more mixed support, consistent with existing studies of samples unselected for sexual orientation (Elhai et al., 2012; Forbes et al., 2015; Miller et al., 2013) and some studies of other diverse populations (Demirchyan et al., 2015; Michalopoulos et al., 2015; cf. Kuowei et al., 2018; Schnyder et al., 2015). Importantly, it is not possible to directly compare DSM-IV and DSM-5 latent structures using confirmatory factor analysis given differences in the number of items from each, and the finding that the DSM-5 structure performed adequately across all fit indices, whereas the DSM-IV structure did not could be attributable to the larger number of factors in the DSM-5 structure. Nevertheless, it appears that the DSM-5 changes, such as creating an effortful avoidance cluster of symptoms and restructuring to include a wider variety of changes in mood and cognition, are a good fit with the symptoms experienced by SMW after trauma.
As expected, the prevalence of PTSD with DSM-5 symptoms and without A2 was higher than the prevalence of PTSD with DSM-IV symptoms and A2 included. This appeared to be primarily driven by the removal of A2 more so than by symptom criterion changes, as the prevalence of PTSD increased when A2 was excluded with either DSM-IV or DSM-5 symptom criteria, but decreased somewhat when comparing DSM-5 versus DSM-IV symptom criteria (this decrease was significant when A2 was applied and was not significant when A2 was not applied). This is consistent with past studies, in which removing Criterion A2 led to increases in prevalence (Elhai et al., 2012; Kilpatrick et al., 2013), and no change in prevalence when assessed in relation to recent symptoms (Kilpatrick et al., 2013). However, the increase in prevalence associated with A2 was larger in this study than in past studies (Elhai et al., 2012; Kilpatrick et al., 2013). Peritraumatic reactions, like those assessed by A2 (i.e., fear, horror, helplessness), are sometimes theorized as integral to the definition of PTSD and may be especially important among SMW (Bovin & Marx, 2011), perhaps as a result of chronic exposure to minority stress. Future studies should investigate the degree to which accounting for other peritraumatic reactions, like disgust, anger, shame, numbing, and sadness, improve diagnostic accuracy in SMW.
It should be noted that we did not examine changes to A1. DSM-5 sought to narrow the objective definition of a traumatic stressor (A1), which might be expected to decrease prevalence estimates, and this possibility should be tested in future research on SMW. In addition, whether this lower prevalence evidences increased specificity, as suggested by Elhai and colleagues (2009) and Forbes and colleagues (2011), or a failure to account for the experiences of certain affected trauma survivors, is an avenue for future research. It is possible that, in an atmosphere of chronic discrimination, the latter explanation could disproportionately impact SMW, and clinicians should be conscious of this possibility when conducting assessments.
We found high agreement (88%) between DSM-IV (using A2) and DSM-5 (with symptom changes and without A2), with 15% meeting PTSD criteria and 73% not meeting criteria using both algorithms. When there was disagreement, it was more common that a case would be PTSD positive using DSM-5 and negative with DSM-IV. We found an increase of 4.3% moving to DSM-5, which is higher than that noted by other studies (Elhai et al., 2012). One possible explanation for this is that we were unable to distinguish between experiencing the sudden natural versus unnatural death of a loved one to account for the stricter A1 definition in DSM-5, as this change has been identified as a primary explanation for meeting DSM-IV but not DSM-5 criteria (Kilpatrick et al., 2013). Alternatively, it is possible that DSM-5 symptoms may function differently for SMW. Research investigating aspects of SMW’s experiences of trauma that make them more likely to endorse symptoms included in the DSM-5 and/or whether there is assessment bias affecting DSM-5 diagnoses among SMW is critical.
One DSM-5 goal was to increase PTSD specificity and differentiation from other disorders (Forbes et al., 2011; Friedman, 2013). However, DSM-5 PTSD has been criticized for its overlap with depression symptoms (Frueh et al., 2010; McNally, 2009). Although other studies with different subject populations have not supported this concern (Elhai et al., 2012; Hoge et al., 2014), we found higher comorbidity between PTSD and depression with DSM-5 criteria as compared with DSM-IV (33.7% vs. 26.6%). It is possible that the sequelae of minority stress for SMW manifest in the types of cognitive dysfunction captured by additions to the DSM-5 criteria (i.e., depressive rather than anxious). Indeed, about 30% of SMW endorsed negative beliefs about oneself, others, and the world, while the risk-taking item was endorsed by only 13.6% of our sample. Cognitive theories of PTSD posit that exposure to traumatic events can strengthen existing negative beliefs about oneself and the world (Dunmore et al., 2001; Elwood et al., 2009; Nishith et al., 2000), and SMW-specific stressors such as heterosexism and internalized SMW-related stigma may increase the likelihood of developing depressive distorted cognitions after trauma. Such cognitions may be an especially important target for clinical intervention.
This study had several limitations. Our sample was not a representative or random sample of SMW; participants were primarily White and represented a narrow age range. However, demographic characteristics of the sample match national representative samples of SMW (Chandra et al., 2011), increasing confidence in external validity. Online sampling could lead to participant misrepresentation, although past research on a similar topic found that potentially invalid responses were a small minority (2%-7.5%) (Ramo et al., 2010; Ramo & Prochaska, 2012). Although web-based assessments of trauma and PTSD are also subject to concerns about participant honesty, and are additionally limited in that they preclude querying about symptoms or conducting true diagnostic assessments, research supports the reliability and validity of online assessments of these topics (Fortson et al., 2006; Read et al., 2009). In addition, although the PCL for DSM-IV is strongly correlated with interviewer measures (Blanchard et al., 1996), we do not know whether that extends to our DSM-5 items. We did not evaluate functional impairment, and the TLEQ was not adjusted for the restricted A1 trauma criterion in DSM-5. Consequently, we might have categorized individuals as meeting PTSD criteria who technically would not, which could have lessened the observed increase in individuals meeting criteria from DSM-IV to DSM-5.
Nonetheless, this study is an important step in examining the impact of changes to the diagnostic criteria of PTSD on a subgroup that is at high risk for trauma exposure and PTSD. Changes from DSM-IV to DSM-5 suggest slight increases in PTSD prevalence estimates and adequate performance in terms of the factor structure of PTSD symptom criteria among SMW. This indicates that it is likely appropriate for clinicians assessing PTSD in SMW to use DSM-5 criteria. Further research regarding how our diagnostic criteria perform in diverse populations should be a goal of evaluating our conceptualizations of mental disorders.
Acknowledgments
Funding
The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: Data collection and manuscript preparation for this article was supported by National Institute on Alcohol Abuse and Alcoholism Grant R01AA018292 (PI: Kaysen). Manuscript preparation was also supported in part through National Institute of Alcohol Abuse and Alcoholism Grants T32AA007455 (PI: Larimer), T32AA007459 (PI: Monti), and K99AA026317 (PI: Dworkin). The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institute on Alcohol Abuse and Alcoholism, the National Institutes of Health, or the University of Washington.
Biographies
Author Biographies
Debra Kaysen is a clinical psychologist, and a professor in the Department of Psychiatry & Behavioral Sciences at Stanford University. Her area of specialty both in research and clinical work is in the care of those who have experienced traumatic events including treatment of PTSD and comorbid disorders. Her body of research is notable for the inclusion of underserved populations such as research with Native Americans, sexual minorities, and individuals in low- and middle-income countries.
Isaac C. Rhew is a psychiatric epidemiologist and research associate professor in the Department of Psychiatry and Behavioral Sciences at the University of Washington. He also holds an adjunct appointment in the Department of Epidemiology. His research focuses on the etiology and prevention of substance use and common psychiatric conditions and the application of innovative epidemiological and statistical methods toward the study of these problems.
Joyce Bittinger received her PhD from the University of Washington in 2012 and she completed a postdoctoral fellowship in 2014 at the University of Washington Department of Psychiatry and Behavioral Sciences. Her research focused on PTSD and memory processes and she was dedicated to training and mentoring students in clinical psychology. She passed away in 2018 after a long illness. She is greatly missed.
Michele Bedard-Gilligan is a licensed clinical psychologist and an associate professor at the University of Washington in the Department of Psychiatry and Behavioral Sciences. She received her PhD in clinical psychology from the University of Washington in 2009. Her research interests focus on recovery processes following trauma exposure with a specific interest in the treatment of PTSD and the impact of co-occurring substance use on symptoms and recovery.
Lisa A. Garberson is a research scientist in the Department of Family Medicine at the University of Washington. She received her PhD in educational psychology (Research, Evaluation, Measurement, and Statistics) from the University of Georgia. Her research interests include secondary data analysis and Medicare administrative data.
Kimberley A. Hodge received her bachelor’s degree in psychology from the University of Washington and has worked as a research coordinator on multiple projects. She has particular interests in research on lesbian and bisexual women and addictive behaviors.
Amanda J. Nguyen received her PhD in public mental health from the Johns Hopkins Bloomberg School of Public Health in 2016. She is currently a research assistant professor at the University of Virginia, where she is affiliated with the Youth-Nex Center to Promote Effective Youth Development. Her research focuses on prevention of mental health problems and promotion of well-being among youth who have experienced adversity.
Diane E. Logan earned her PhD in clinical psychology from the University of Washington. She is a behavioral health psychologist and coordinates substance use services at a rural community health center. She has published numerous peer-reviewed articles and provides clinical trainings across the country on substance use disorder interventions.
Emily R. Dworkin received her PhD in clinical-community psychology from the University of Illinois Urbana–Champaign. She is an acting assistant professor in the Department of Psychiatry & Behavioral Sciences at the University of Washington. The central goal of her program of research is to mitigate the development of psychopathology after sexual assault and other forms of trauma by targeting the social, community, and cultural contexts in which recovery unfolds.
Kristen P. Lindgren received her PhD in clinical psychology from the University of Washington in 2006. She is currently an associate professor in the Department of Psychiatry & Behavioral Sciences at the University of Washington. Her research focuses on cognitive factors that may underlie substance use and trauma-related problems.
Footnotes
Declaration of Conflicting Interests
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Due to this sampling strategy, we use the term “women” when discussing this sample to refer to individuals who had been assigned female sex at birth and identified as women at the time that they responded to study advertisements. As a result, some women (e.g., transgender women) are not reflected in this sample, which is a notable limitation of this study. Some participants may have primarily identified with a gender identity term (e.g., genderqueer, nonbinary) other than “woman,” and others who identified as women at the time of enrollment may have changed their gender identity during study participation.
References
- Alessi EJ, Martin JI, Gyamerah A, & Meyer IH (2013). Prejudice events and traumatic stress among heterosexuals and lesbians, gay men, and bisexuals. Journal of Aggression, Maltreatment & Trauma, 22(5), 510–526. [PMC free article] [PubMed] [Google Scholar]
- American Psychiatric Association. (1994). Diagnostic and statistical manual of mental disorders (4th ed.). Washington, DC: Author. [Google Scholar]
- American Psychiatric Association. (2000). Diagnostic and statistical manual of mental disorders (4th ed., text rev.). Washington, DC: Author. [Google Scholar]
- American Psychiatric Association. (2010). DSM-5 development: Proposed draft revisions to DSM disorders and criteria. http://www.dsm5.org/ProposedRevesions/
- American Psychiatric Association. (2013). Diagnostic and statistical manual of mental disorders (5th ed.). Arlington, VA: American Psychiatric Publishing. [Google Scholar]
- Armour C, Műllerová J, & Elhai JD (2016). A systematic literature review of PTSD’s latent structure in the diagnostic and statistical manual of mental disorders: DSM-IV to DSM-5. Clinical Psychology Review, 44, 60–74. [DOI] [PubMed] [Google Scholar]
- Asnaani A, Richey JA, Dimaite R, Hinton DE, & Hofmann SG (2010). A cross-ethnic comparison of lifetime prevalence rates of anxiety disorders. The Journal of Nervous and Mental Disease, 198(8), 551–555. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Balsam KF, Rothblum ED, & Beauchaine TP (2005). Victimization over the life span: A comparison of lesbian, gay, bisexual, and heterosexual siblings. Journal of Consulting and Clinical Psychology, 73(3), 477–487. [DOI] [PubMed] [Google Scholar]
- Bedard-Gilligan M, & Zoellner LA (2008). The utility of the A1 and A2 criteria in the diagnosis of PTSD. Behaviour Research and Therapy, 46(9), 1062–1069. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Blanchard EB, Jones-Alexander J, Buckley TC, & Forneris CA (1996). Psychometric properties of the PTSD Checklist (PCL). Behaviour Research and Therapy, 34, 669–673. [DOI] [PubMed] [Google Scholar]
- Bovin MJ, & Marx BP (2011). The importance of the peritraumatic experience in defining traumatic stress. Psychological Bulletin, 137(1), 47–87. [DOI] [PubMed] [Google Scholar]
- Chandra A, Mosher WD, & Copen C (2011). Sexual behavior, sexual attraction, and sexual identity in the United States: Data from the 2006–2008 National Survey of Family Growth. National Health Statistics Reports, 36, 1–36 [PubMed] [Google Scholar]
- Collins RL, Parks GA, & Marlatt GA (1985). Social determinants of alcohol consumption: The effects of social interaction and model status on the self-administration of alcohol. Journal of Consulting and Clinical Psychology, 53(2), 189–200. [DOI] [PubMed] [Google Scholar]
- Conron KJ, Mimiaga MJ, & Landers SJ (2010). A population-based study of sexual orientation identity and gender differences in adult health. American Journal of Public Health, 100(10), 1953–1960. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Demirchyan A, Goenjian AK, & Khachadourian V (2015). Factor structure and psychometric properties of the Posttraumatic Stress Disorder (PTSD) checklist and DSM-5 PTSD symptom set in a long-term postearthquake cohort in Armenia. Assessment, 22(5), 594–606. [DOI] [PubMed] [Google Scholar]
- Dunmore E, Clark DM, & Ehlers A (2001). A prospective investigation of the role of cognitive factors in persistent Posttraumatic Stress Disorder (PTSD) after physical or sexual assault. Behaviour Research and Therapy, 39(9), 1063–1084. [DOI] [PubMed] [Google Scholar]
- Dworkin ER, Bedard-Gilligan M, Gilmore A, Lehavot K, Guttmannova K, & Kaysen D (2018). Predicting PTSD severity from experiences of trauma and heterosexism in lesbian and bisexual women: A longitudinal study of cognitive mediators. Journal of Counseling Psychology, 65, 324–333. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Elhai JD, Ford JD, Ruggiero KJ, & Frueh CB (2009). Diagnostic alterations for post-traumatic stress disorder: Examining data from the National Comorbidity Survey Replication and National Survey of Adolescents. Psychological Medicine, 39, 1957–1966. [DOI] [PubMed] [Google Scholar]
- Elhai JD, Miller ME, Ford JD, Biehn TL, Palmieri PA, & Frueh BC (2012). Posttraumatic stress disorder in DSM-5: Estimates of prevalence and symptom structure in a nonclinical sample of college students. Journal of Anxiety Disorders, 26(1), 58–64. [DOI] [PubMed] [Google Scholar]
- Elhai JD, & Palmieri PA (2011). The factor structure of posttraumatic stress disorder: A literature update, critique of methodology, and agenda for future research. Journal of Anxiety Disorders, 25(6), 849–854. [DOI] [PubMed] [Google Scholar]
- Elwood LS, Hahn KS, Olatunji BO, & Williams NL (2009). Cognitive vulnerabilities to the development of PTSD: A review of four vulnerabilities and the proposal of an integrative vulnerability model. Clinical Psychology Review, 29(1), 87–100. [DOI] [PubMed] [Google Scholar]
- Flora DB, & Curran PJ (2004). An empirical evaluation of alternative methods of estimation for confirmatory factor analysis with ordinal data. Psychological Methods, 9(4), 466–491. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Forbes D, Fletcher S, Lockwood E, O’Donnell M, Creamer M, Bryant RA, … Silove D (2011). Requiring both avoidance and emotional numbing in DSM-V PTSD: Will it help? Journal of Affective Disorders, 130(3), 483–486. [DOI] [PubMed] [Google Scholar]
- Forbes D, Lockwood E, Elhai JD, Creamer M, Bryant R, McFarlane A, … O’Donnell M (2015). An evaluation of the DSM-5 factor structure for posttraumatic stress disorder in survivors of traumatic injury. Journal of Anxiety Disorders, 29, 43–51. [DOI] [PubMed] [Google Scholar]
- Fortson BL, Scotti JR, Ben KSD, & Chen YC (2006). Reliability and validity of an Internet traumatic stress survey with a college student sample. Journal of Traumatic Stress: Official Publication of the International Society for Traumatic Stress Studies, 19(5), 709–720. [DOI] [PubMed] [Google Scholar]
- Friedman MJ (2013). Finalizing PTSD in DSM-5: Getting here from there and where to go next. Journal of Traumatic Stress, 26(5), 548–556. [DOI] [PubMed] [Google Scholar]
- Friedman MJ, Resick PA, Bryant RA, & Brewin CR (2011). Considering PTSD for DSM-5. Depression & Anxiety, 28(9), 750–769. [DOI] [PubMed] [Google Scholar]
- Frueh BC, Elhai JD, & Acierno R (2010). The future of posttraumatic stress disorder in the DSM. Psychological Injury and Law, 3(4), 260–270. [Google Scholar]
- Gilman SE, Cochran SD, Mays VM, Hughes M, Ostrow D, & Kessler RC (2001). Risk of psychiatric disorders among individuals reporting same-sex sexual partners in the National Comorbidity Survey. American Journal of Public Health, 91(6), 933–939. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hatzenbuehler ML (2009). How does sexual minority stigma “get under the skin”? A psychological mediation framework. Psychological Bulletin, 135(5), 707–730. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Herek GM, Gillis JR, Cogan JC, & Glunt EK (1997). Hate crime victimization among lesbian, gay, and bisexual adults: Prevalence, psychological correlates, and methodological issues. Journal of Interpersonal Violence, 12(2), 195–215. [Google Scholar]
- Hoge CW, Riviere LA, Wilk JE, Herrell RK, & Weathers FW (2014). The prevalence of post-traumatic stress disorder (PTSD) in US combat soldiers: a head-to-head comparison of DSM-5 versus DSM-IV-TR symptom criteria with the PTSD checklist. The Lancet Psychiatry, 1(4), 269–277. [DOI] [PubMed] [Google Scholar]
- Hu L, & Bentler PM (1999). Cutoff criteria for fit indexes in covariance structure analysis: Conventional criteria versus new alternatives. Structural Equation Modeling, 6(1), 1–55. [Google Scholar]
- Karam EG, Andrews G, Bromet E, Petukhova M, Ruscio AM, Salamoun M, & Kessler RC (2010). The role of criterion A2 in the DSM-IV diagnosis of posttraumatic stress disorder. Biological Psychiatry, 68, 465–473. 10.1016/j.biopsych.2010.04.032 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Katz-Wise SL, & Hyde JS (2012). Victimization experiences of lesbian, gay, and bisexual individuals: A meta-analysis. Journal of Sex Research, 49(2-3), 142–167. [DOI] [PubMed] [Google Scholar]
- Kaysen DL, Kulesza M, Balsam KF, Rhew IC, Blayney JA, Lehavot K, & Hughes TL (2014). Coping as a mediator of internalized homophobia and psychological distress among young adult sexual minority women. Psychology of Sexual Orientation and Gender Diversity, 1(3), 225–233. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kilpatrick DG, Resnick HS, & Acierno R (2009). Should PTSD criterion A be retained? Journal of Traumatic Stress, 22(5), 374–383. [DOI] [PubMed] [Google Scholar]
- Kilpatrick DG, Resnick HS, Milanak ME, Miller MW, Keyes KM, & Friedman MJ (2013). National estimates of exposure to traumatic events and PTSD prevalence using DSM-IV and DSM-5 criteria. Journal of Traumatic Stress, 26(5), 537–547. [DOI] [PMC free article] [PubMed] [Google Scholar]
- King M, Semlyen J, Tai SS, Killaspy H, Osborn D, Popelyuk D, & Nazareth I (2008). A systematic review of mental disorder, suicide, and deliberate self harm in lesbian, gay and bisexual people. BMC Psychiatry, 8(1), 70–86. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kivlahan DR, Marlatt GA, Fromme K, Coppel DB, & Williams E (1990). Secondary prevention with college drinkers: Evaluation of an alcohol skills training program. Journal of Consulting and Clinical Psychology, 58(6), 805–810. [DOI] [PubMed] [Google Scholar]
- Kubany ES, Leisen MB, Kaplan AS, Watson SB, Haynes SN, Owens JA, & Burns K (2000). Development and preliminary validation of a brief broad-spectrum measure of trauma exposure: The Traumatic Life Events Questionnaire. Psychological Assessment, 12(2), 210–224. [DOI] [PubMed] [Google Scholar]
- Kuowei A, Jayasuriya R, Jayasuriya D, & Silove D (2018). Assessing the factorial structure and measurement invariance of PTSD by gender and ethnic groups in Sri Lanka: An analysis of the modified Harvard Trauma Questionnaire (HTQ). Journal of Anxiety Disorders, 47, 45–53. [DOI] [PubMed] [Google Scholar]
- Lehavot K, & Simoni JM (2011). The impact of minority stress on mental health and substance use among sexual minority women. Journal of Consulting and Clinical Psychology, 79(2), 159–170. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Litt DM, Lewis MA, Rhew IC, Hodge KA, & Kaysen DL (2015). Reciprocal relationships over time between descriptive norms and alcohol use in young adult sexual minority women. Psychology of Addictive Behaviors, 29(4), 885–893. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lockwood E, & Forbes D (2014). Posttraumatic stress disorder and comorbidity: Untangling the Gordian knot. Psychological Injury and Law, 7(2), 108–121. [Google Scholar]
- Löwe B, Decker O, Müller S, Brähler E, Schellberg D, Herzog W, & Herzberg PY (2008). Validation and standardization of the Generalized Anxiety Disorder Screener (GAD-7) in the general population. Medical Care, 46(3), 266–274. [DOI] [PubMed] [Google Scholar]
- McCabe SE, Hughes TL, Bostwick WB, West BT, & Boyd CJ (2009). Sexual orientation, substance use behaviors and substance dependence in the United States. Addiction, 104(8), 1333–1345. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McNally RJ (2009). Can we fix PTSD in DSM-V? Depression & Anxiety, 26(7), 597–600. [DOI] [PubMed] [Google Scholar]
- Meyer IH (2003). Prejudice, social stress, and mental health in lesbian, gay, and bisexual populations: Conceptual issues and research evidence. Psychological Bulletin, 129, 674–697. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Michalopoulos LM, Unick GJ, Haroz EE, Bass J, Murray LK, & Bolton PA (2015). Exploring the fit of Western PTSD models across three non-Western low- and middle-income countries. Traumatology, 21, 55–63. [Google Scholar]
- Miller MW, Wolf EJ, Kilpatrick D, Resnick H, Marx BP, Holowka DW, & Friedman MJ (2013). The prevalence and latent structure of proposed DSM-5 posttraumatic stress disorder symptoms in U.S. national and veteran samples. Psychological Trauma: Theory, Research, Practice, and Policy, 5(6), 501–512. [Google Scholar]
- Nishith P, Mechanic MB, & Resick PA (2000). Prior interpersonal trauma: The contribution to current PTSD symptoms in female rape victims. Journal of Abnormal Psychology, 109(1), 20–25. [PMC free article] [PubMed] [Google Scholar]
- Pole N, Gone JP, & Kulkarni M (2008). Posttraumatic stress disorder among ethnoracial minorities in the United States. Clinical Psychology: Science and Practice, 15(1), 35–61. [Google Scholar]
- Radloff LS (1977). The CES-D scale: A self report depression scale for research in the general population. Applied Psychological Measurement, 1(3), 385–401. [Google Scholar]
- Ramo DE, Hall SM, & Prochaska JJ (2010). Reaching young adult smokers through the internet: Comparison of three recruitment mechanisms. Nicotine & Tobacco Research, 12(7), 768–775. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ramo DE, & Prochaska JJ (2012). Broad reach and targeted recruitment using Facebook for an online survey of young adult substance use. Journal of Medical Internet Research, 14(1), Article e28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Read JP, Farrow SM, Jaanimägi U, & Ouimette P (2009). Assessing trauma and traumatic stress via the Internet: Measurement equivalence and participant reactions. Traumatology, 15(1), 94–102. [Google Scholar]
- Roberts AL, Austin SB, Corliss HL, Vandermorris AK, & Koenen KC (2010). Pervasive trauma exposure among US sexual orientation minority adults and risk of posttraumatic stress disorder. American Journal of Public Health, 100(12), 2433–2441. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schnyder U, Müller J, Morina N, Schick M, Bryant RA, & Nickerson A (2015). A comparison of DSM-5 and DSM-IV diagnostic criteria for posttraumatic stress disorder in traumatized refugees. Journal of Traumatic Stress, 28, 267–274. [DOI] [PubMed] [Google Scholar]
- Spiegelman D, & Hertzmark E (2005). Easy SAS calculations for risk or prevalence ratios and differences. American Journal of Epidemiology, 162(3), 199–205. [DOI] [PubMed] [Google Scholar]
- Spitzer RL, Kroenke K, & Williams JB (2006). A brief measure for assessing generalized anxiety disorder: The GAD-7. Achieves of Internal Medicine, 166(10), 1092–1097. [DOI] [PubMed] [Google Scholar]
- Steele LS, Ross LE, Dobinson C, Veldhuizen S, & Tinmouth JM (2009). Women’s sexual orientation and health: Results from a Canadian population-based survey. Women & Health, 49(5), 353–367. [DOI] [PubMed] [Google Scholar]
- Swinson RP (2006). The GAD-7 scale was accurate for diagnosing generalized anxiety disorder. Evidence Based Medicine, 11(6), 184. [DOI] [PubMed] [Google Scholar]
- Szymanski DM, & Balsam KF (2011). Insidious trauma: Examining the relationship between heterosexism and lesbians’ PTSD symptoms. Traumatology, 17(2), 4–13. [Google Scholar]
- Thomsen CJ, Stander VA, McWhorter SK, Rabenhorst MM, & Milner JS (2011). Effects of combat deployment on risky and self-destructive behavior among active duty military personnel. Journal of Psychiatric Research, 45(10), 1321–1331. [DOI] [PubMed] [Google Scholar]
- Weathers F, Huska J, & Keane T (1991). The PTSD checklist military version (PCL-M). National Center for PTSD. [Google Scholar]
- Weathers FW, Litz BT, Herman DS, Huska JA, & Keane TM (1994). The PTSD Checklist (PCL): Reliability, validity, and diagnostic utility. In The annual meeting of the International Society for Traumatic Stress Studies. San Antonio, TX. [Google Scholar]
- Weathers FW, Litz BT, Keane TM, Palmieri PA, Marx BP, & Schnurr PP (2013). The PTSD checklist for DSM-5 (PCL-5). https://www.ptsd.va.gov/.
- Wirth RJ, & Edwards MC (2007). Item factor analysis: Current approaches and future directions. Psychological Methods, 12(1), 58–79. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zoellner LA, Bedard-Gilligan MA, Jun JJ, Marks LH, & Garcia NM (2013). The evolving construct of Posttraumatic Stress Disorder (PTSD): DSM-5 criteria changes and legal implications. Psychological Injury and Law, 6(4), 277–289. [DOI] [PMC free article] [PubMed] [Google Scholar]


