The relationship between disease severity, immunosuppression, and outcome
The immunological response in sepsis patients is complex, comprising concurrent pro- and anti-inflammatory responses. It has become increasingly clear that most sepsis patients do not succumb to an early, overwhelming pro-inflammatory response, but rather to complications related to immunosuppression occurring later on in their disease trajectory [1, 2]. This severely suppressed state of the immune system renders patients unable to clear their primary infection and increases susceptibility toward secondary infections, often with opportunistic pathogens [3, 4]. Recently, a seminal observational study questioned the contribution of secondary infections to sepsis mortality [5]. This study linked disease severity in sepsis patients to increased susceptibility toward secondary infections and higher mortality. Analysis of the transcriptome of circulating leukocytes revealed distinct hallmarks of immune suppression at the onset of secondary infections, consistent with an important role for sepsis-induced immunosuppression as a causative factor. However, after adjustment for age and, crucially, disease severity the attributable mortality from secondary infections was low (2%) [5]. This may appear to indicate that sepsis-induced immunosuppression is of limited importance for outcome, and that interventions aimed to mitigate or reverse it will therefore have little impact. We believe this is not the case, because immunosuppression is an intermediary factor in sepsis patients. Disease severity drives immunosuppression, eventually leading to mortality related to secondary infections. It is therefore not surprising that correcting for disease severity abolishes the contribution of secondary infections to mortality. This does, however, not mean that therapeutic interventions aimed at an intermediary factor, in this case immunosuppression, may not affect outcome. We would like to illustrate this using diabetes as an example. In diabetic patients, poor glycemic control (indicated by increased HbA1c) induces vascular damage, resulting in an increased rate of myocardial infarctions. In this example, HbA1c reflects disease severity, vascular damage the intermediary factor, and myocardial infarction the outcome. If the attributable myocardial infarctions of vascular damage would be corrected for HbA1c in diabetic patients, the effect would be modest as well. However, it is widely accepted that vascular damage is causative for myocardial infarctions. More importantly, interventions targeting vascular damage (e.g., percutaneous coronary intervention) are highly effective, also in patients with diabetes. Analogously, strategies aimed at mitigating sepsis-induced immunosuppression should not be written off.
Noradrenaline as an intermediate factor linking disease severity to immunosuppression
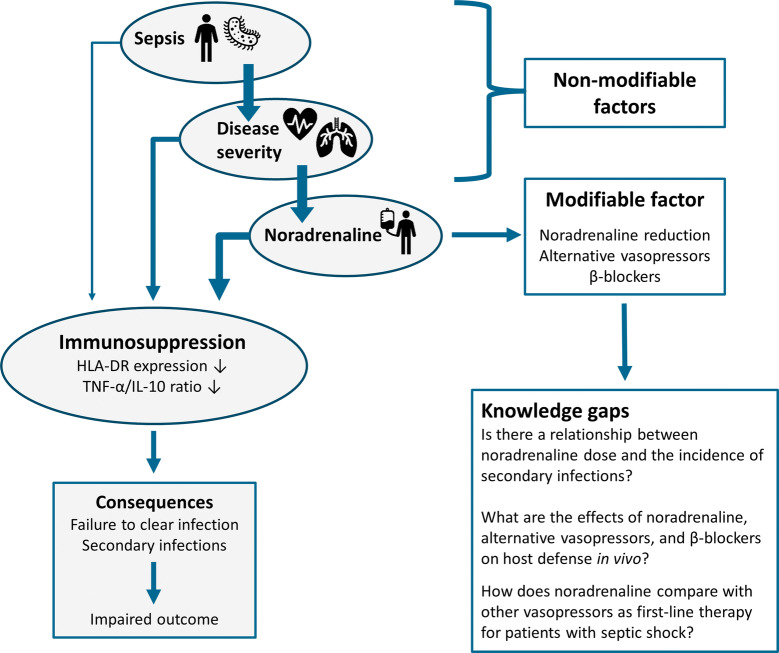
Although new therapies to reconstitute immune function in sepsis patients are being developed, current standard of care practices should also be reevaluated in light of sepsis-induced immunosuppression, as some interventions may significantly dysregulate the immune response. In sepsis patients, the use of noradrenaline reflects disease severity and we hypothesize that this cornerstone vasopressor treatment is an important driver of sepsis-induced immunosuppression. In this capacity, it acts as an intermediate factor as well, linking disease severity to immunosuppression and impaired outcome, as outlined below and in Fig. 1.
Fig. 1.
Conceptual framework showing that, in sepsis patients, both disease severity and noradrenaline administration are important drivers of sepsis-induced immunosuppression. The development of immunosuppression is an intermediary factor, linking disease severity to adverse clinical outcomes. Several features of sepsis-induced immunosuppression are listed, as well as the consequences of immunosuppression, ultimately leading to impaired clinical outcome. As more severely ill sepsis patients are more likely to suffer from hemodynamic instability, anti-inflammatory effects of noradrenaline, mediated through the β-adrenoceptor, link disease severity to the development of immunosuppression. Therefore, noradrenaline represents an intermediary factor as well. This is of clinical relevance, because noradrenaline is a modifiable factor, which can be exploited for the prevention or treatment of sepsis-induced immunosuppression. Different approaches can be pursued, such as use of alternative vasopressors or concurrent administration of β-blockers. The current knowledge gaps that need to be bridged to explore this new concept are highlighted
There are several arguments for this. First, disease severity and circulating noradrenaline levels are highly intertwined, as more severely ill septic patients generally require more vasopressor support. These phenomena are also correlated by default, as blood pressure and/or vasopressor requirement is commonly part of the disease severity scores used in sepsis. Second, noradrenaline exerts profound anti-inflammatory effects, predominantly mediated via the β-adrenergic receptor [6]. For instance, it attenuates production of pro-inflammatory mediators tumor necrosis factor (TNF)-α and interleukin (IL)-6, while enhancing the release of the anti-inflammatory cytokine IL-10 by lipopolysaccharide-stimulated leukocytes [7]. Furthermore, noradrenaline was shown to inhibit natural killer cell cytotoxicity [8] and, conversely, destruction of noradrenergic nerve endings increased bacterial resistance in mice [9]. To date, clinical evidence is circumstantial. In the aforementioned ‘attributable mortality study,’ the prevalence of shock (defined as noradrenaline requirement in a dose > 0.1 µg/kg/min) was significantly higher in patients who developed a secondary infection compared with those who did not [5]. Furthermore, improved outcomes using a catecholamine-sparing ‘permissive hypotension’ strategy [10] or the use of a beta-blocker [11] in septic shock patients have been reported. Finally, previous studies have linked a higher vasopressor (i.e., noradrenaline) load to increased mortality [12], although none has assessed its relationship with secondary infections. This remains an important aspect for future studies.
Breaking the link: alternative vasopressors
Next to the use of β-blockers, alternative non-catecholaminergic vasopressors with less or no untoward immunological effects might be instrumental to break the putative link between disease severity and sepsis-induced immunosuppression, thereby improving outcome. Several clinical trials have compared noradrenaline with vasopressin (analogues). In the most recent, the selective V1-receptor agonist selepressin conferred no clear clinical advantage over noradrenaline [13], although development of secondary infections was not assessed. Angiotensin II is another vasopressor with no reported immunosuppressive effects that significantly reduces noradrenaline requirements [14]. Importantly, in all previous trials investigating alternative vasopressors, the new vasopressor was used as add-on therapy to noradrenaline instead of as first-line vasopressor. Therefore, patients were treated with noradrenaline for hours already, which could have masked any immunological benefits of alternative vasopressors. To allow a beneficial immunological effect of an alternative vasopressor to emerge, they should be investigated as initial monotherapy against noradrenaline and development of secondary infections should be a predefined endpoint.
Conclusion
We argue that immunosuppression is an intermediary factor linking disease severity to adverse outcome in sepsis patients. Therefore, the contribution of immunosuppression to outcome will be severely underestimated when it is corrected for disease severity, while interventions aimed at restoring immunocompetence may still have a significant impact on outcome. Furthermore, we identify noradrenaline as an important driver of immunosuppression in sepsis, as it exerts profound immunosuppressive effects in preclinical studies. Because the need for noradrenaline is related to disease severity, this vasopressor may represent a crucial intermediary factor between disease severity and immunosuppression. Nevertheless, use of more clinically relevant models of inflammation and sepsis as well as translation to the human setting is highly warranted to properly assess the consequences of noradrenaline therapy for host defense. Furthermore, unlike disease severity, noradrenaline represents a modifiable intermediary factor. Therefore, the use of alternative vasopressors as first-line therapy should be further explored.
Authors contribution
RFS, MK, and PP drafted and critically revised the article. All authors read and approved the final article and provided consent for publication in Intensive Care Medicine.
Funding
The work in this article was supported by a Radboudumc-Rijnstate Ph.D grant (Grant no. 160721-6).
Compliance with ethical standards
Conflicts of interest
The authors declare they have no competing interests.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
The authors M. Kox and P. Pickkers have contributed equally.
References
- 1.Hotchkiss RS, Monneret G, Payen D. Sepsis-induced immunosuppression: from cellular dysfunctions to immunotherapy. Nat Rev Immunol. 2013;13(12):862–874. doi: 10.1038/nri3552. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Boomer JS, et al. Immunosuppression in patients who die of sepsis and multiple organ failure. JAMA. 2011;306(23):2594–2605. doi: 10.1001/jama.2011.1829. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Otto GP, et al. The late phase of sepsis is characterized by an increased microbiological burden and death rate. Crit Care. 2011;15(4):R183. doi: 10.1186/cc10332. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Torgersen C, et al. Macroscopic postmortem findings in 235 surgical intensive care patients with sepsis. Anesth Analg. 2009;108(6):1841–1847. doi: 10.1213/ane.0b013e318195e11d. [DOI] [PubMed] [Google Scholar]
- 5.van Vught LA, et al. Incidence, risk factors, and attributable mortality of secondary infections in the intensive care unit after admission for sepsis. JAMA. 2016;315(14):1469–1479. doi: 10.1001/jama.2016.2691. [DOI] [PubMed] [Google Scholar]
- 6.Stolk RF, et al. Potentially inadvertent immunomodulation: norepinephrine use in sepsis. Am J Respir Crit Care Med. 2016;194(5):550–558. doi: 10.1164/rccm.201604-0862CP. [DOI] [PubMed] [Google Scholar]
- 7.van der Poll T, et al. Noradrenaline inhibits lipopolysaccharide-induced tumor necrosis factor and interleukin 6 production in human whole blood. Infect Immun. 1994;62(5):2046–2050. doi: 10.1128/IAI.62.5.2046-2050.1994. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Takamoto T, et al. Norepinephrine inhibits human natural killer cell activity in vitro. Int J Neurosci. 1991;58(1–2):127–131. doi: 10.3109/00207459108987189. [DOI] [PubMed] [Google Scholar]
- 9.Rice PA, et al. Chemical sympathectomy increases the innate immune response and decreases the specific immune response in the spleen to infection with Listeria monocytogenes. J Neuroimmunol. 2001;114(1–2):19–27. doi: 10.1016/S0165-5728(00)00421-5. [DOI] [PubMed] [Google Scholar]
- 10.Lamontagne F, et al. Effect of reduced exposure to vasopressors on 90-day mortality in older critically ill patients with vasodilatory hypotension: a randomized clinical trial. JAMA. 2020;323:938–949. doi: 10.1001/jama.2020.0930. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Morelli A, et al. Effect of heart rate control with esmolol on hemodynamic and clinical outcomes in patients with septic shock: a randomized clinical trial. JAMA. 2013;310(16):1683–1691. doi: 10.1001/jama.2013.278477. [DOI] [PubMed] [Google Scholar]
- 12.Dunser MW, et al. Association of arterial blood pressure and vasopressor load with septic shock mortality: a post hoc analysis of a multicenter trial. Crit Care. 2009;13(6):R181. doi: 10.1186/cc8167. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Laterre PF, et al. Effect of selepressin vs placebo on ventilator- and vasopressor-free days in patients with septic shock: the SEPSIS-ACT randomized clinical trial. JAMA. 2019;322:1476–1485. doi: 10.1001/jama.2019.14607. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Khanna A, et al. Angiotensin II for the treatment of vasodilatory shock. N Engl J Med. 2017;377(5):419–430. doi: 10.1056/NEJMoa1704154. [DOI] [PubMed] [Google Scholar]